blood vessels
the delivery system of dynamic structures that begins and ends at the heart
ateries
carry blood away from the heart - the blood is oxygenated except for pulmonary circulation and umbilical vessels of a fetus
capillaries
contact tissue cells and directly serve cellular needs - endothelium with sparse lamina
veins
carry blood towards the heart
venous system
heart - large veins (capacitance vessels) - small veins (capacitance vessels) - postcapillary venule - thoroughfare channel - capillaries
arterial system
- elastic arteries (conducting vessles) - muscular arteries (distributing vessels)-
layers of the blood vessel wall are in order from the inside out
lumen
layer one -tunica intima: endothelium - subendothelial layer -internal elastic lamina
layer two - tunica media: smooth muscle and elastic fibers - external elastic lamina
layer three- tunica externa; collagen fibers
lumen
central blood containing space, which is surrounded by three distinct layers or tunics.
tunica intima
the innermost tunic - it is in intimate contact with the blood in the lumen
simple squamous endothelium lines the lumen of all vessels, in vessels larger than 1 mm a subendothelial connective tissue basement membrane is present
tunica media
smooth muscle and sheets of elastin, sympathetic vasometer nerve fibers control vasoconstriction and vasodialation of vessels
vasoconsctriction
reduction in lumen diameter as the smooth muscle contracts
vasodialation
increase in lumen diameter as the snooth muscle relaxes
tunica externa (also known as tunica adventitia)
collagen fibers protect and reinforce, large vessels contain vasa vasorum to nourish the external layer
vasa vasorum
a system of tiny blood vessels theat nourish the more external tissues of the blood vessel wall -its own blood supply
Arteries:
•Arteries have three layers: a smooth inner layer, a muscular layer, and a thin outer layer.
•Arteries, with the exception of the pulmonary artery, carry oxygenated blood from the heart to the body.
•Arteries are of greater size, thickness and elasticity than veins.
•Blood in arteries is under significant pressure.
•Arteries do not contain valves; valves would be unnecessary considering the force that is already applied to the blood in arteries.
Veins:
•Veins, like arteries, have three layers: a smooth inner layer, a muscular layer, and a thin outer layer.
•Veins, with the exception of the pulmonary vein, carry deoxygenated blood that has been used by body tissue back to the heart. Veins, as well as carrying deoxygenated blood, carry waste products.
•Veins are smaller, thinner and much less elastic than arteries.
•Blood in veins does not experience as much pressure as blood in arteries.
•Veins contain valves to prevent back flow of blood.
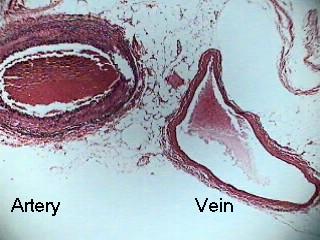
atery and vein
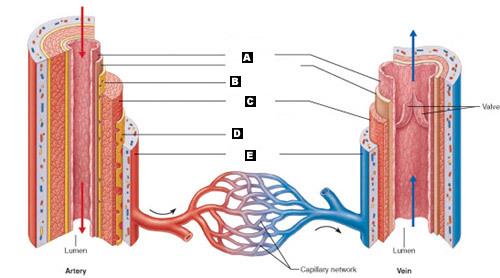
label
A. Tunica intima
C. Tunica media
D. External elastic lamina
E. Tunica externa
B. Internal elastic lamina
elastic ateries
large thick walled arteries with elastin in all three tunics, near the heart the aorta and its major branches, large lumen offers low resistance sometimes referred to as conducting arteries, act as pressure resevoirs - expand and recoil as blood is ejected from the heart
average lumen diameter 1.5 cm
average wall thickness 1.0 mm
lumen
central blood containing space
capillaries
endothelium with sparse basal lamina
tunica intima
simple squamous endothelium, lines the lumen of all vessels in vessels larger than 1 mm a subendothelial connective tissue basement membrane is present
tunica media
smooth muscle and sheets of elastin, sympathetic vasomotor nerve fibers control vasoconstriction and vasodialation of vessels
tunica externa (tunica adventitia)
collagen fibers protect and reinforce, larger vessels contain vasa vasorum to nourish the external layer
elastic conducting ateries
large thick walled arteries with elastin in all three tunics, the aorta and its major branches, large lumen offers low resistance, acts as pressure reservoirs - expand and recoil as blood is ejected from the heart
lumen
internak hollow space
muscular(distributing) arteries and arterioles
distal to elastic arteries, deliver blood to body organs, have a thick tunica media with more smotth muscle, active in vasocontriction, controls blood flow through tissues
arterioles
smallest arteries, lead to capillary beds, control flow into capillary beds via vasodialation and vasoconstriction
vasodialation
relaxation of the smooth muscles of the blood vessels, producing dialation
vasoconstriction
narrowing of blood vessels
capillaries
microscopic blood vessels, walls of thin tunica intima, one cell thick, pericytes help stablize their walls and control permeability, size allows only a single RBC to pass at a time, inall tissues except for cartilage, epithelia, cornea and lens of eye.
capillaries - function
exchange gases, nutrients, wastes, hormones, etc.
the three structural types of capillaries
continuous capillaries
fenestrated capillaries
sinusoidal capillaries (sinusoids)
continuous capillaries are abundant where
in the skin and muscles
held together by tight junctions connect endothelial cells and intercellular clefts allow the passage of fluids and small solutes
continuous capillaries of the brain - junctions
tight junctions are complete, forming the *blood brain barrier*
fenestrated capillaries
some endothelial cells contain pores (fenestrations) more permeable then continuous capillaries - function in absorption or filtrate formation (small intestines, endocrine glands, and kidneys)
sinusoidal capillaries
fewer tight junctions, larger intercellular clefts, large lumen, usually fenestrated, allow large molecules and blood cells to pass between the blood abd surrounding tissues
where are sinusoidal capillaries found
in the liver, bone marrow and spleen
where do the clefts sit
in between the cells
capillary beds
are interwoven networks of capillaries form the microcirculation between arterioles and venules
capillary beds consist of two types of vessels what are they
1. vascular shunt (metarteroile - thoroughfare channel) directly connects the terminal arteriole and a postcapillary venule
2. true capillaries - 10 - 100 exchange vessels per capillary bed - they branch off the metarteriole or terminal arteriole
precapillary sphincters do what
regulate blood flow into true capillaries; regulated by local chemical conditions and vasomotor nerves
when are venules formed
when capillary beds unite, they are very porous and allow fluids and WBC's into tissues - post capillary venules consist of endothelium and a few pericytes, larger venules have on or two layers of smooth muscle cells
which are bigger veins or capillaries
veins
When are veins formed
when venules converge, have thinner walls, larger lumens compared with corresponding arteries, blood pressure is lower than in arteries, thin tunica media and a thick externa consisting of collagen fibers and elastic networks - called capacitance vessels (blood reservoirs) contain up to 65% of the blood supply, are adaptations that ensure return of blood to the heart
pericyte
adventitial cell or mural cell, is a connective tissue cell that occurs about small blood vessels.[
what purpose do large diameter lumens offer in the veins
they offer little resistance
what purpose do valves offer in the veins
prevent the backflow of blood - most abundant in veins of the limbs
what are venous sinuses
they are flattened veins with extremely thin walls (coronary sinus of the heart and dural sinuses of the brain)
vascular anastomoses are
interconnections of blood vessels - arterial anastomoses provide alternate pathways (collateral channels) to a given body region - they are common at joints, in abdominal organs, brain and heart
vascular shunts of capillaries are example of arteriovenous anastomoses - venous anastomoses are common
blood flow -
volume of blood flowing through a vessel, an organ, or the entire circulation in a given period
- it is measured in ml/min
- equivilant to cardiac output (CO) for entire vascular system - it is relatively constant when at rest, varies widely through individual organs, based on needs
blood pressure
force per unit area exerted on the wall of a blood vessel by the blood, expressed in mm Hg
measured as systemic arterial BP in large arteries near the heart -
the pressure gradient provides the driving force that keeps blood moving from higher to lower pressure areas
resistance (peripheral resistance)
opposition of flow
measure of the amount of friction blood encounters
generally encountered in the peripheral systemic circulation
three important sources of resistance are
blood viscosity - thickness of the blood
total blood vessel length
blood vessel diameter
factors that remain relatively constant in regards to resistance are
blood viscosity - the stickiness of the blood due to formed elements and plasma proteins
and
blood vessel length - the longer the vessel the greater the resistance encountered
frequent changes that alter peripheral resistance are
blood vessel diameter - it is always changing
small diameter arterioles are the major determinants of peripheral resistance
abrupt changes in diameter or fatty plaques form atherosclerosis dramatically increase resistance * distrupt laminar flow and cause terbulance
blood flow (F) is directly proportional to what
the blood (hydrostatic) pressure gradient (delta P) if the pressure gradient increases then the blood flow speeds up
blood flow is inversely proportional to what
peripheral resistance (R)
if the resitance increases blood flow decreases
flow =
pressure gradient divided by peripheral resistance
peripheral resitance is more important in influencing local blood flow because of what
it is easily changed by altering blood vessel diameter
what generates blood flow
the pumping action of the heart
pressure results when what
when flow is opposed by resistance
systemic pressure is
highest in the aorta
declines throughout the pathway
is 0 mm Hg in the right atrium
the steepest drop occurs where
in the arterioles
arterial blood pressure reflects what
two factors of the arteries close to the heart - elasticity (compliance or distensibility) volume of blood forced into them at any time
30
pulse near the heart is what
pulsatle
systolic pressure
pressure exerted during ventricular contraction
diastolic pressure
lowest level of arterial pressure
pulse pressure
difference between systolic and diastolic pressure
mean arterial pressure
pressure that propels the blood to the tissues
MAP =
diastolic pressure = 1/3 pilse pressure
when do pulse pressure and MAP both decline
with increasing distance from the heart
what is the range of capillary blood pressure
ranges from 15 to 35 mm Hg, low capillary pressure is desirable - high blood pressure would rupture fragile, thin- walled capillaries, most are very permemable, so low pressure forces filtrate into interstitial spaces
when pressure is low how does the blood move
more slowly
does venous pressure change during the cardiac cycle
very little
small pressure gradian, about 15 mm Hg
low pressure due to cumulative effects of peripheral resistance
one of the factors aiding venous return is the respiratory pump - explain
pressure changes created during breathing move blood toward the heart by squeezing abdominal veins as thoracic veins expand
one of the factors aiding venous return is the muscular pump - explain
contraction of skeletal muscles "milk" blood toward the heart and valves prevent backflow
one of the factors aiding venous return is the vasoconstriction - explain
vasoconstiction of veins under sympathetic control - because of the smooth muscle
maintaining blood pressure requires what
cooperation of the heart blood vessels and kidneys
supervision of the brain
what are the main factors influencing blood pressure
cardiac output (CO)
peripheral resistance (PR)
blood volume
•F = P/PR and CO = P/PR
Blood pressure =
= CO x PR (and CO depends on blood volume)
•Blood pressure varies directly with CO, PR, and blood volume
•Changes in one variable are quickly compensated for by changes in the other variables
how is the cardiac output determined
by venous return and neural and hormonal controls
resting heartrate is maintinaed by what
the cardioinhibitory center via the parasympathetic vagus nerve
stroke volume is controled by what
venous return (EDV)
during stress the heart cardioaccelertory center increases heart rate and stroke volum via what
sympathetic stimulation
if the ESV decreases what happens to MAP
it increases
what are the short term controls of blood pressure
neural and hormonal controls
they counteract fluctuations in blood pressure by altering peripheral resistance
what are the long term controls of blood pressure
long term renal regulation
conteracts fluctuations in blood pressure by altering the blood volume
neural controls of peripheral resistance do what
maintain MAP by altering blood vessel diameter
alter blood distribution in response to specific demands
neural controls operate via reflex arcs tha tinvolve what
baroreceptors
vasomotor centers and vasomotor fibers
vacular smooth muscle
the vasomotor center is what
a cluster of sympathetic neurons in the medula that oversee changes in blood vessel diameter
part of the cardiovascular center along with the cardiac center
the vasomotor center does what
maintains vasomotor tone (moderate constriction of the arterioles)
receives inputs from baroreceptors, chemoreceptors, and higher brain centers
where are barorecptors located
in carotid sinuses, aortic arch, walls of large arteries of the neck and thorax
what happens to the baroreceptors when blood pressure increases
increased blood pressure stimulates the baroreceptors to increase input to the vasomotor center
inhibits the vasomotor center, causing arteriole dialation and venodialation
stimulates the cardioinhibitory center
what protects the blood supply to the brain
Baroreceptors taking part in the carotid sinus reflex protect the blood supply to the brain
what helps maintain adequate blood pressure in the systemic circuit
Baroreceptors taking part in the aortic reflex help maintain adequate blood pressure in the systemic circuit
what happens if the blood pressure rises above a normal range
1. blood pressure (arterial blood pressure rises above normal range)
2. baroreceptors in carotid sinuses and aortic arch are stimulated
3. impulses from baroreceptors stimalte cardioinhibitory center (and inhibit cardioacceleratory center) and inhibit vasomotor center
4a sympathetic impulses to the heart cause a decrease in HR, a decrease in contractility and a decrease in cardiac output
4b decrease rate of vasomotor impulses allows vasodialation causing a decrease in peripheral resistance
what happens if the blood pressure drops below a normal range
1. blood pressure decreases (arterial blood pressure falls below a normal range)
2.baroreceptors on carotid sinus and aortic arch are inhibited
3. impulses from baroreceptors stimulate cardioacceleratory center (and inhibit cardioinhibitory center) and stimulate vasomotor center
4a an increase of sympathetic impulses to the heart cause an increase in heart rate an increase in contractility and an increase in cardiac output
4b vasomotor fibers stimulate vasoconstriction causing an increase in preipheral resistance
Short-Term Mechanisms: Chemoreceptor-Initiated Reflexes where are the Chemoreceptors located
in the Carotid sinus, aortic arch, large arteries of the neck
same location as the baroreceptors
what do the chemoreceptor sin the carotid sinus respond to
to rise in CO2, drop in pH or O2
Increase blood pressure via the vasomotor center and the cardioacceleratory center
Are more important in the regulationof respiratory rate
where are the relexes that regulate blood pressure integrated from
the medulla
higher brain centers (cortex and hypothalamus) can modify BP via relays to medullary centers
which hormone causes blood pressure to decline
ANP atrial natriuretic peptide
causes blood volume and blood pressure to decline, causes generalized vasodialation
influence of selected hormones on variables affecting blood pressure: epinepherine and norepinephrine
cause generalized vasoconstriction and increase cardiac output
influence of selected hormones on variables affecting blood pressure: angiotensin II
generated by kidney release of renin causes vasoconstriction
influence of selected hormones on variables affecting blood pressure: ADH (antidiurectic hormone - vasopressin)
causes intense vasoconstriction in cases of extremely low BP
influence of selected hormones on variables affecting blood pressure: aldosterone
increase in blood volume, decrease in water loss - occurs in the kidneys
influence of selected hormones on variables affecting blood pressure: cortisol
increase in blood volume, decrease in water loss - occurs in the kidneys
kidneys act directly to regulate arterial blood pressure by doing what
direct renal mechanism
alters bllod volume independantly of hormones
*increased blood pressure or blood volume causes the kidneys to eliminate more urine, thus reducing blood pressure
*decreased blood pressure or blood volume causes the kidneys to conserve water and blood pressure rises
kidneys act indirectly to regulate arterial blood pressure by doing what
indirect renal (renin- angiotensin) mechanism
a decrease in arterial blood pressure releases renin which produces angiotensinII which is a potent vasoconstrictor - angiotensin then leads to aldosterone secretion , which causes renal absorption of sodium and decreases urine formation
Angitensin II stimultes the release of what
ADH
what are vital signs
pulse and blood pressure along with rsepiratory rate and body temperature
pulse
pressure wave caused by the expansion and recoil of ateries - rarial pulse Taken at the wrist) routinely used
how do you measure blood pressure
with a sphygmomanometer
*pressure is increase in the cuff until it exceeds systolic pressure in the brachial artery
*pressure is then slowly release and the examiner listens for sounds of KORTIKOFF with a stehoscope
* sound first occcur as blood starts to spurt through the artery (systolic pressure) (normally 110-140 mmHg)
*sounds disappear when the artery is no longer constricted and blood is flowing freely (diastolic pressure) (normally 70-80 mmHg)
what are some variations in blood pressure
blood pressure cuclye over a 24 hour period
blood presure peaks in the mornig due to levels of hormones
age, sex, weight, race, mood, and posture may vary BP
hypotension
low blood pressure
systolic pressur ebelow 100 mm Hg
often associated with long life and lack of cardiovascular illness
orthostatic hypotension
temporary low blood pressure and dizziness when suddenly rising from a sitting or reclining position
chronic hypotension
hint of poor nutrition and warning signs for addisons disease (hyposecretion of aldosterone) or hypothyroidism
acute hypotension
important sign of circulatory shock
hypertension
high blood pressure
Sustained elevated arterial pressure of 140/90 or higher
May be transient adaptations during fever, physical exertion, and emotional upset
Often persistent in obese people
Prolonged hypertension is a major cause of heart failure, vascular disease, renal failure, and stroke
Primary or essential hypertension
90% of hypertensive conditions (no underlying cause), Due to several risk factors including heredity, diet, obesity, age, stress, diabetes mellitus, and smoking
Secondary hypertension
less common
Due to identifiable disorders, including kidney disease, arteriosclerosis, and endocrine disorders such as hyperthyroidism and Cushing’s syndrome (hypersecretion of glucocorticoids)
how many pulse points are there and where are they
nine
1. superficial temporal artery
2. facial artery
3. common carotid artery
4. brachial artey
5. radial artery
6. femoral artery
7. popliteal artery
8. posterior tibial artery
9. dorsalis pedis artery
blood flow tissue perfusion is involved in what
delivery of oxygen and nutrients to and removal of wastes from tissue cells
gas exchange in the lungs
absorption of nutrients in the digestive tract
urine formation in the kidneys
** the rate of flow is precisely yhe right amount to provide for proper function
properties of the velocity of blood flow
changes as it travels through the systemic circulation
is inversely related to the total cross sectional area
is fastest in teh aorta, slowest in the capillaries and increases again in the veins
what does slow capillary flow allow for
allows for adequate time for exchange between blood and tissues
autoregulation
automatic adjustment of blood flow to each tissue in proportion to its requirements at any given point in time
how is autoregulation controlled
intrinsically by modifying the diameter of local arterioles feeding the capillaries i ti is independant of MAP , which is controlled as needed to maintain constant pressure
what are the two types of autoregulation
1. metabolic
2. myogenic
describe metabolic autoregulation
•Vasodilation of arterioles and relaxation of precapillary sphincters occur in response to
•Declining tissue O2
•Substances from metabolically active tissues (H+, K+, adenosine, and prostaglandins) and inflammatory chemicals
•Effects
•Relaxation of vascular smooth muscle
•Release of NO from vascular endothelial cells
•NO is the major factor causing vasodilation
•Vasoconstriction is due to sympathetic stimulation and endothelins
describe myogenic autoregulation
•Myogenic responses of vascular smooth muscle keep tissue perfusion constant despite most fluctuations in systemic pressure
what is passive stretch
(increased intravascular pressure) promotes increased tone and vasoconstriction
what is reduced stretch
promotes vasodilation and increases blood flow to the tissue
Intrinsic mechanisms (autoregulation)
Distribute blood flow to individual organs and tissues as needed
what are the Metabolic controls involved in Intrinsic mechanisms (autoregulation)
decrease amounts of: pH and oxygen
increase
potassium
carbondioxide
Prostaglandins
Adenosine
Nitric oxide
Endothelins (constriction)
what are the Myogenic controls (muscular responses) involved in Intrinsic mechanisms (autoregulation)
Stretch
Extrinsic mechanisms
Maintain mean arterial pressure (MAP) Redistribute blood during exercise and thermoregulation
nerves involved in extrinsic control of anterior smooth muscle in the systemic circulation
sympathetic (constriction)
hormones involved in extrinsic control of anterior smooth muscle in the systemic circulation
epinephrine and norepinephrine (alpha receptors - constrict) (beta receptors - dilate)
angiotensin II constricts
antidiuretic hormone ADH - constricts
atrial natriuretic peptide (ANP) dilates
angiogenesis
occurs when short term autoregulation cannot meet tissue nutrient requirements
the number of vessels to a region increases and existing vessels enlarge
when does angiogenesis occur
common in the heart when a coronary vessel is occluded, or throughout the body in people in high aaltitude areas
what happens to blood flow to the skeletal muscles during rest
at rest myogenic and general neural mechanisms predominate
what happens with blood flow to muscles during activity
Blood flow increases in direct proportion to the metabolic activity (active or exercise hyperemia)
Local controls override sympathetic vasoconstriction
Muscle blood flow can increase 10 or more during physical activity
blood flow to the brain
Blood flow to the brain is constant, as neurons are intolerant of ischemia
what are the metabolic controls involved in blood flow to the brain
Declines in pH, and increased carbon dioxide cause marked vasodilation
what are the Myogenic controls involved in blood flow to the brain
Decreases in MAP cause cerebral vessels to dilate
Increases in MAP cause cerebral vessels to constrict
The brain is vulnerable under extreme systemic pressure changes
•MAP below 60 mm Hg can cause syncope (fainting)
•MAP above 160 can result in cerebral edema
syncope
fainting
cerebral edema
an excess accumulation of water in the intracellular and/or extracellular spaces of the brain.
blood flow to the skin does what (through the skin)
Blood flow through the skin
Supplies nutrients to cells (autoregulation in response to O2 need)
Helps maintain body temperature (neurally controlled)
Provides a blood reservoir (neurally controlled)
blood flow to the skin does what (below the skin surface)
Blood flow to venous plexuses below the skin surface
Varies from 50 ml/min to 2500 ml/min, depending on body temperature
Is controlled by sympathetic nervous system reflexes initiated by temperature receptors and the central nervous system
as temperature rises what occurs
(heat expossure, fever, vigorous exercise)
Hypothalamic signals reduce vasomotor stimulation of the skin vessels thus producing vasodilation
Heat radiates from the skin
Sweat also causes vasodilation via bradykinin in perspiration
Bradykinin stimulates the release of NO
Bradykinin
Bradykinin is a peptide that causes blood vessels to dilate (enlarge), and therefore causes blood pressure to lower
NO
nitric oxide
as temperature decreases what occurs
As temperature decreases, blood is shunted to deeper, more vital organs
blood flow to the lungs
Pulmonary circuit is unusual in that
The pathway is short
Arteries/arterioles are more like veins/venules (thin walled, with large lumens)
Arterial resistance and pressure are low (24/8 mm Hg)
Autoregulatory mechanism is opposite of that in most tissues
Low O2 levels cause vasoconstriction; high levels promote vasodilation
Allows for proper O2 loading in the lungs
blood flow to the heart - during ventricular systole
Coronary vessels are compressed
Myocardial blood flow ceases
Stored myoglobin supplies sufficient oxygen
blood flow to the heart - during ventricular diastole
At rest, control is probably myogenic
blood flow to the heart during the strenuous exercise
Coronary vessels dilate in response to local accumulation of vasodilators
Blood flow may increase three to four times
blood flow through the capillaries vasomotion
slow and intermittent flow
reflects the on/off openining and closing of precapillary sphincters
capillary exchange of respiratory gases and nutrients
Diffusion of
O2 and nutrients from the blood to tissues
CO2 and metabolic wastes from tissues to the blood
Lipid-soluble molecules diffuse directly through endothelial membranes
Water-soluble solutes pass through clefts and fenestrations
Larger molecules, such as proteins, are actively transported in pinocytotic vesicles or caveolae
what are the four possible pathways or routes of transport across the endothelial cell wall of a fenestrated capillary
1 Diffusion through membrane (lipid-soluble substances)
2 Movement through intercellular clefts (water-soluble substances
3 Movement through fenestrations (water-soluble substances)
4 Transport via vesicles or caveolae (large substances)
Fluid Movements: Bulk Flow
•Extremely important in determining relative fluid volumes in the blood and interstitial space
•Direction and amount of fluid flow depends on two opposing forces: hydrostatic and colloid osmotic pressures
•Capillary hydrostatic pressure (HPc) (capillary blood pressure)
•Tends to force fluids through the capillary walls
•Is greater at the arterial end (35 mm Hg) of a bed than at the venule end (17 mm Hg)
•Capillary colloid osmotic pressure (OPc)
•Created by nondiffusible plasma proteins, which draw water toward themselves (~26 mm Hg)
Net Filtration Pressure (NFP)
•NFP—comprises all the forces acting on a capillary bed
•NFP = hydrostatic pressure – osmotic pressure
•At the arterial end of a bed, hydrostatic forces dominate
•At the venous end, osmotic forces dominate
•Excess fluid is returned to the blood via the lymphatic system
Circulatory Shock
Any condition in which Blood vessels are inadequately filled, Blood cannot circulate normally and Results in inadequate blood flow to meet tissue needs
Hypovolemic shock:
results from large-scale blood loss
Vascular shock:
results from extreme vasodilation and decreased peripheral resistance
Cardiogenic shock
results when an inefficient heart cannot sustain adequate circulation
artery side (arteriole)
fluid goes out - pushes out
vein side (venule)
fluid goes in - pulls in