When is organogenesis complete?
12 weeks
When is the GB seen?
20 weeks
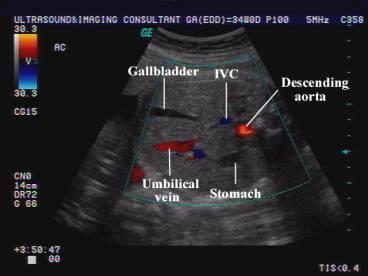
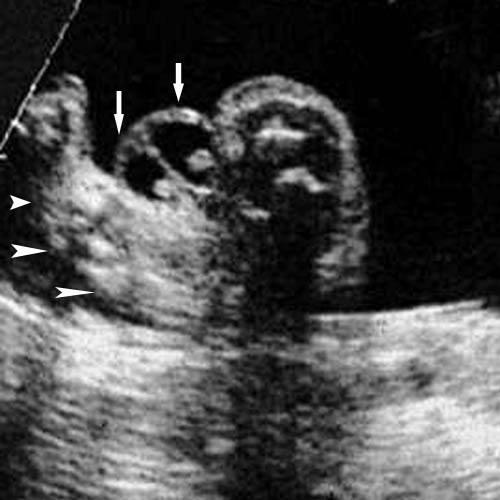
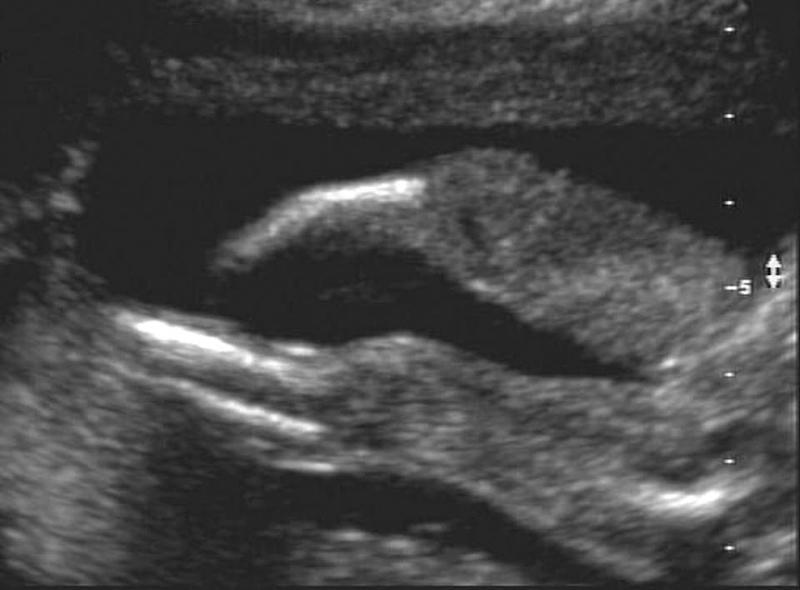
Fetal GB
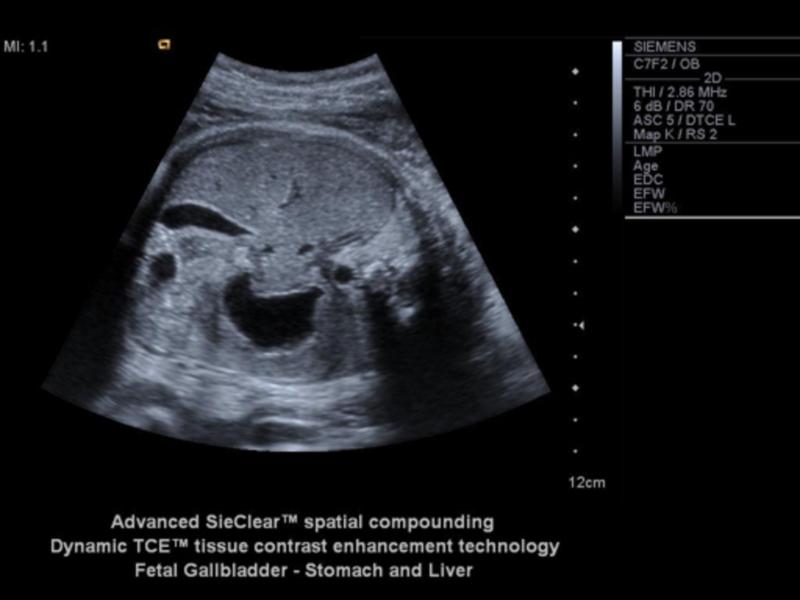
Fetal GB

Fetal GB
What is suspected when the spleen is enlarged in a fetus?
Rh immunoIncompatibility
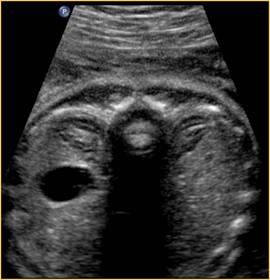
When can the stomach be seen?
14 weeks
If the stomach is not seen by 16 weeks, what could be the problem?
esophageal atresia
What is the stomach a landmark for?
AC
What does the intestines act as in utero?
resevor for meconium
Why does the the fetus not poo in utero
peristalisis does not occur until birth
anal sphincter is closed
*unless in distress
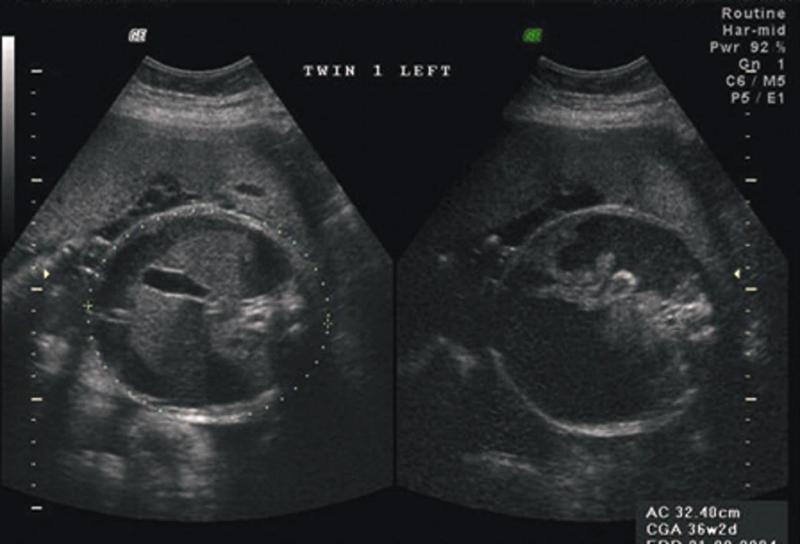
kidney / testis crisscross
...
what is meconium made of
amniotic fluid + fetal cells
bacteria and enzymes added

spleenomegaly
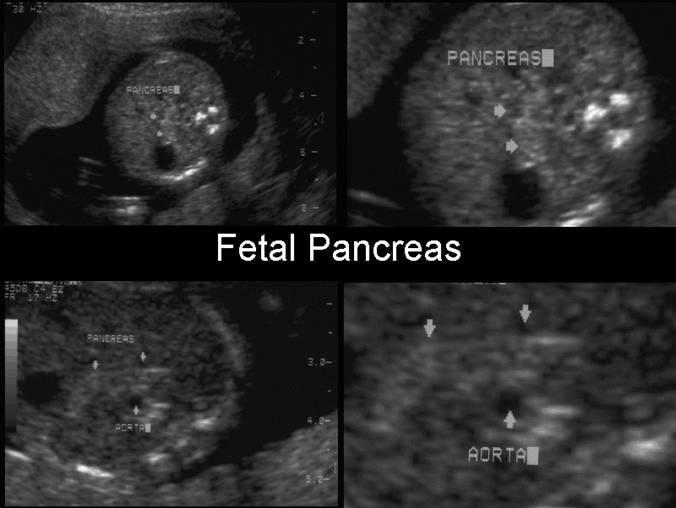
Pancreas
What is the size of the adrenals in a fetus?
20x larger in fetus than adults
can mimic kidneys
adrenal

adrenal
______________ is directly proportional to AC.
liver size
What is hypoxic?
pertaining to low oxygen
What does the umbilical arteries become after birth?
hypogastric ligament
What does the umbilical vein become after birth?
ligament venosum
What measurements do we take involving the abdomen?
AC
renal length
What is the AC landmarks?
trans spine - 3 oss center
J - portal vein
stomach & GB
What is esophageal atresia?
congenital atresia of the esophagus
What causes esophageal atresia?
failure of recanalization of the GIT
a blind end tube is result
What is present in most cases of esophageal atresia?
tracheo-esophageal fistula
What percent of esophageal atresia have a tracheo-esophageal fistula present?
90%
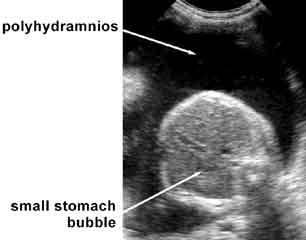
What is the sonographic appearance of esophageal atresia?
polyhydramnios
stomach usually not identified
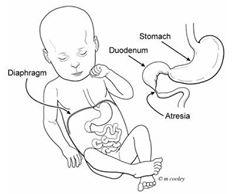
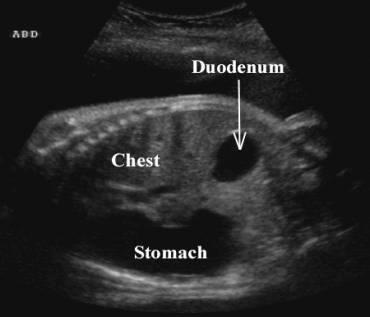
Duodenal atresia
What is duodenal atresia usually associated with?
Downs syndrome
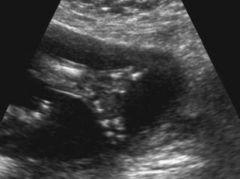
What is the sonographic appearance of duodenal atresia?
Double bubble
polyhydramnios
Duodenal atresia

Double bubble
When can duodenal atresia be seen?
24 weeks
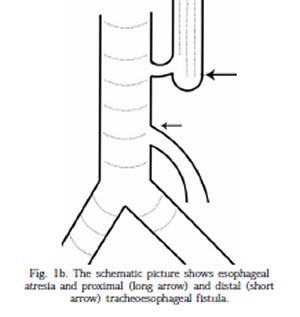
tracheo-esophageal fistula
What causes a double bubble?
duodenal atresia
duodenal stenosis
annular pancreas
jejunal atresia
What is an annular pancreas?
extension of pancreas tissue around duodenal
forming a ring
What problems does annular pancreas cause in infants?
feeding problems
reflux and vomiting
What is the sonographic appearance of jejunal atresia?
bowel proximal to the blockage dilated
What is the first sign of cystic fibrosis?
meconium ileus
echogenic bowel

meconium ileus

meconium ileus
What is a meconium ileus?
small bowel disorder, presense of thick meconium in the distal ileum
impaction of abnormal thick sticky mecomium
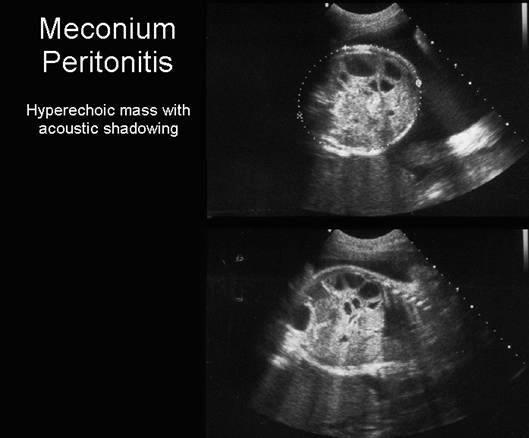
Meconium Peritonitis

Meconium Peritonitis
Meconium Peritonitis
What can obstructed bowel cause?
perforation and infection
What is the sonographic appearance of meconium ileus?
echogenic small bowel
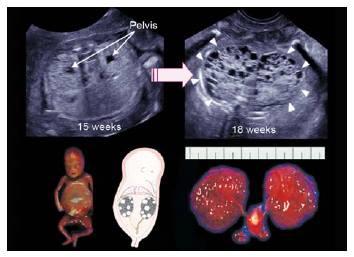
When is the migration of the kidney to the abdomen complete?
9 weeks
What causes pelvic kidneys?
can be physical or hormonal
What are horseshoe kidneys?
inferior portion fuses early on
When should the kidneys and the bladder be seen?
15 weeks

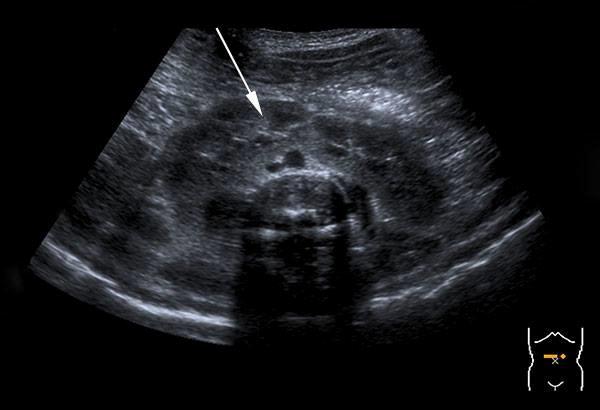
bubble sign
When should the renal cortex and medulla be differentiated?
25 weeks

bubble sign
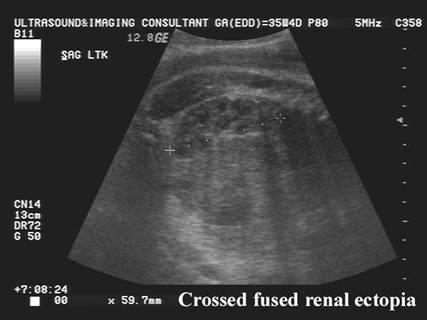
Cross-over fusion kidneys
What happens with bilateral renal agenesis?
olighydramnios usuually resulting in miscarriage - always fatal
What is Potter's type 2?
multicystic dysplastic kidneys
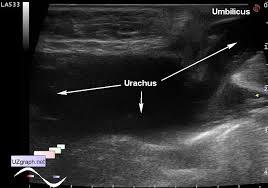
Urachal fistula
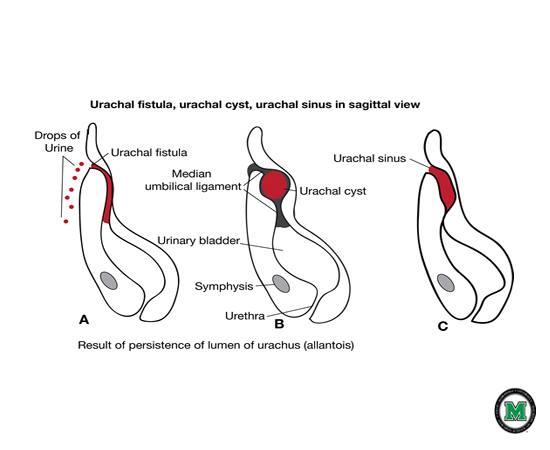
Urachal fistula
What is a urichal fistula?
Urachus doesn't close and belly button leaks urin

Urachal cyst
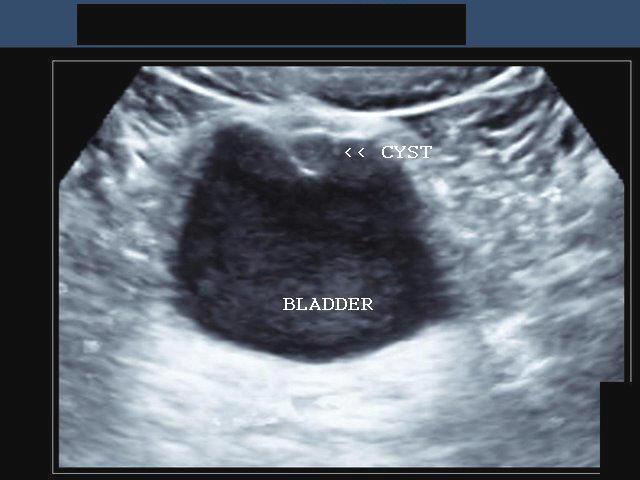
Urachal cyst

Unilateral renal agenesis
Mesoblastic Nephroma AKA: fetal renal harmatoma & congenital Wilm's tumor

Mesoblastic Nephroma AKA: fetal renal harmatoma & congenital Wilm's tumor

Wilm's Tumor AKA: Nephroblastoma
What is mesoblastic nephroma?
Congenital Wilms' tumors
big benign mass usually expresses its self by 3 months
most common neonatal solid tumor
mostly in boys
What is Nephroblastoma?
wilms tumor
What is the most common malignant tumor of childhood?
Wilms tumor
At what age does wilms tumor usually occur?
commonly occurs at 3 yrs
what is a Urachus?
a fibrous cord that extends from the umbilicus to the bladder.
What is the sonographic appearance of Potter's type 2?
Severe oligohydramnios
Absent kidneys
Nondistended bladder
What is IPKD?
disorder associated with multiple bilateral cysts

Infantile Polycystic Kidney Disease
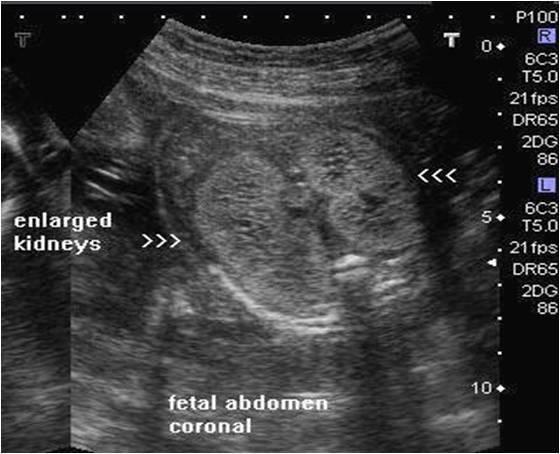
Infantile Polycystic Kidney Disease
What is another name for IPKD?
Potter Type 1
Urachal cyst
Is IPKD recessive of dominant?
recessive
What are the 4 groups of IPKD?
Perinatal – renal failure in utero
Neonatal
Infantile
juvenile
When does neonatal IPKD occur?
within 1st month after birth
When does infantile IPKD occur?
3 - 6 months
When does juvenile IPKD occur?
1 - 5 years
What is the sonographic appearance of IPKD?
enlarged
hyperechoic
homogeneous hyoerechoic large kidneys
increased kidney AC
small bladder
loss of corticomedullary differentiation
What is Meckyl-Gruber syndrome?
- polucystic kidneys
- posterior encephalocoele/holoprosencephaly
- polydactyly
What is adult polycystic kidney disease?
large
echogenic
What age does APKD usually occur?
age 30 with hypertension
If one person has APKD what is the chance of passing it on to children?
50%
What is polycystic kidney disease?
auto dominant
family history
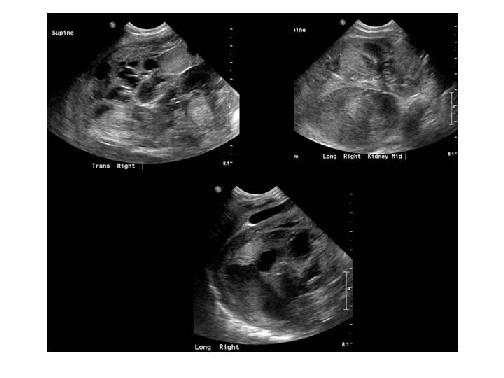
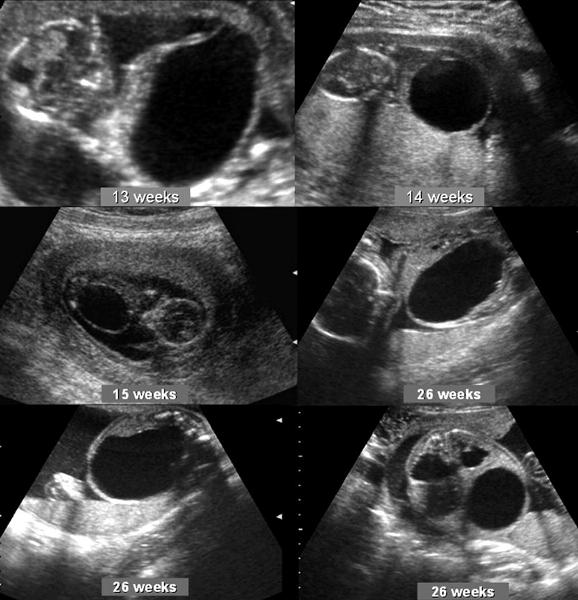
What is multicystic dysplastic kidneys?
disorder associated with unilateral cystic lesions
correspond to dilated collecting tubules
Enlarged
unilateral
nonfunctioning
Bilateral multicystic dysplastic kidney disease

unilateral multicystic dysplastic kidney disease

unilateral multicystic dysplastic kidney disease
What happens to the contralateral kidney with MDK?
enlarges to compensate
What is the sonographic appearance of bilateral MDK?
multiple, round
various sizes
bladder not seen
olighydramnios
Poor Prognosis
What is the sonographic appearance of unilateral MDK?
multiple, round
various sizes
bladder seen
hydronephrosis
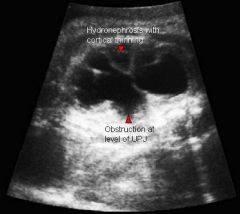
What is UPJ?
uritopelvis junction
What is UVJ?
uritovesicilar junction

Hydronephrosis
Where is a double collecting system most likely to have hydro?
the superior collecting system
What is the most common fetal anomaly?
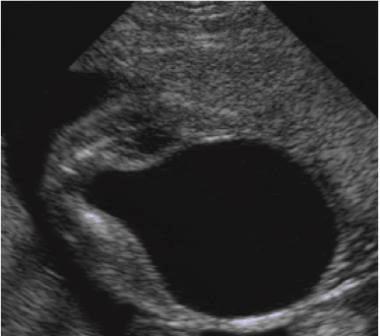
hydronephrosis
What is hydronephrosis usually caused by?
UPJ or UVJ obstruction
What is a UPJ obstruction caused by?
bend or kink in ureter
What is a UVJ obstruction caused by?
bad valves at trigone region
What do normal ureters measure?
1 mm
Prune belly syndrome usually occurs in _____________
boys
What is hydronephrosis?
Dilation of the renal pelvis due to blockage
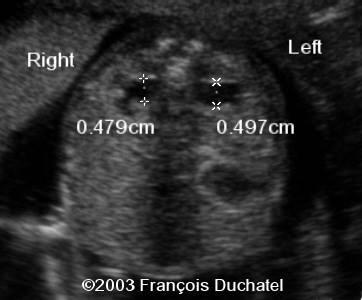
Pyelectasis
What is pyelectasis?
abnormal collection of urine within the renal pelvis 5-9 mm

Caliectasis
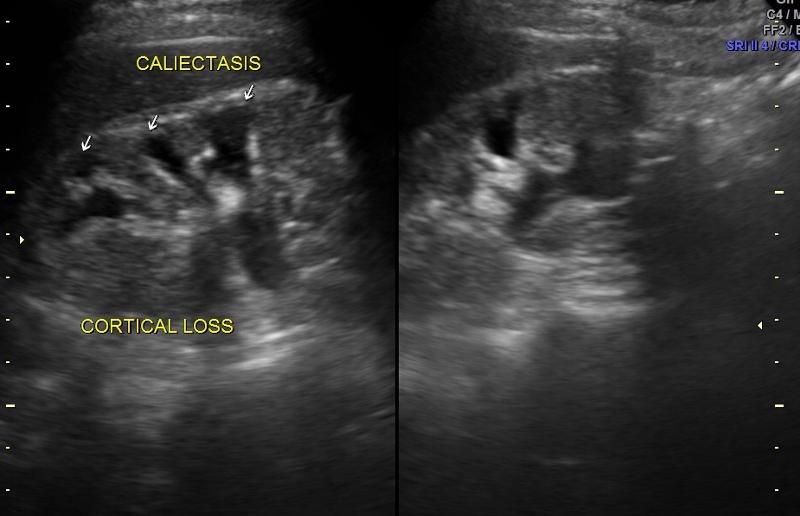
Caliectasis
What is calyectasis?
rounded calyces with renal pelvis dilatation
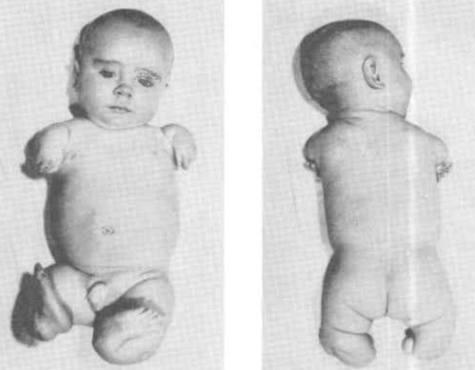
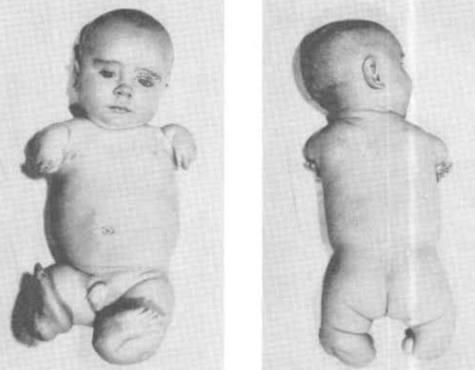
What is Prune Belly Syndrome?
Rare congenital abnormality. A partial or complete lack of abdominal wall muscles w/ renal abnormalities. Usually in males.
anterior abdominal wall defect
urinary tract obstruction
cryptorchidism
hypoplastic abdominal wall muscles
massive distention of bladder
wrinkling
urethral obstruction
bladder enlarges
mega ureter
hydronephrosis
abdomen enlarges
abdominal muscles becomes abnormal
Babies are delived c-section

Prune Belly
Prune Belly
What is another name for prune belly syndrome?
Eagle Barrett syndrome
What is the sonographic appearance of prune belly syndrome
hydronephrosis with echogenic renal parenchyma
oligohydramnios
urinary ascites
a dystrophic bladder
peritoneal calcifications
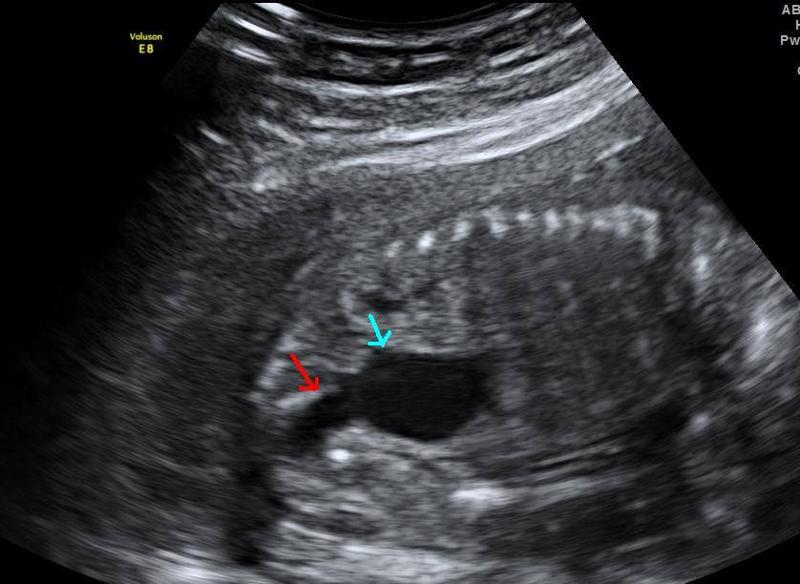
What is ureteropelvic junction obstruction?
Obstruction of the urinary outflow. Can be acquired or congenital.
obstruction at the confluence of the kidney and the ureter
Sporadic
What is the most common cause of hydronephrosis in neonates?
UPJ obstruction
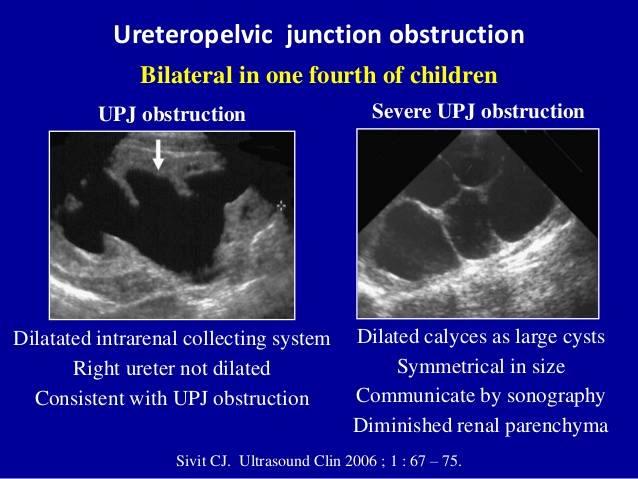
UPJ obstruction
UPJ obstruction
What is the sonographic appearance of ureteropelvic junction obstruction?
will often show a dilated renal pelvis
Doppler: Kidney w/higher resistive indices
hyperechoic kidneys
What is Ureterovesicle junction obstruction?
Obstruction of the uretrovesical junction causing urine to back up into the ureters and kidneys.
results from stenotic ureteral valve or fibrosis
What is the sonographic appearance of Ureterovesicle junction obstruction?
megaureter
hydronephrosis

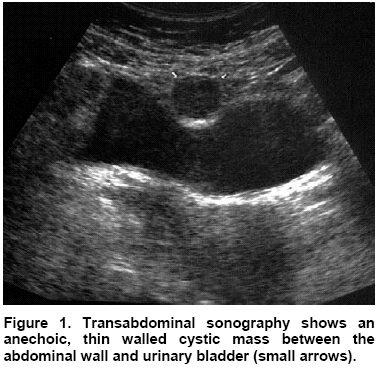
Ectopic ureterocele
What is a Ectopic ureterocele?
the distal ureter does not insert into the urinary bladder
Congenital cystic dilatations of the terminal submucosal ureter
surgical repair or can lead to loss of function
bad insertion of ureter into trigone region
What is the sonographic appearance of a Ectopic ureterocele?
Echogenic thin-walled cyst-like structures within the bladder
What is ectopic ureterocele usually associated with?
UVJ obstruction
Posterior urethral valve
What is Posterior urethral valves?
most common congenital obstructive lesion of the urethra
congenital folds act of male urethra act as valves to obstruct excretion
What is the sonographic appearance of Posterior urethral valves?
marked distention bladder
hydronephrosis
hydroureter
oligohydramnios
keyhole sign
Posterior urethral valve
What is a keyhole sign?
...
What is the major concern for babies with posterior urethral valves?
baby can't urinate
leading to
olighydramnios
pulmonary hyperplasia
risk of bladder rupture causing urinary ascites
What is the most common cause of death for fetus with posterior urethral valves?
pulmonary hyperplasia
What is cloaca?
The cloaca is a structure in the development of the urinary and reproductive organs.
plays a developmental role in
genitals
bladder
rectum

Bladder exstrophy
What is the most severe form of bladder exstrophy?
cloacal extrophy
colon is affected

Testicular hydrocele
Testicular hydrocele
What causes a testicular hydrocele?
process vaginalis does not close completely causing abdominal secretions in scrotal sac.
Many testicular hydroceles _____________ within ____________.
Many testicular hydroceles heal themselves within 24 months.
What week do the testicles descend?
28 weeks
What is Bladder exostrophy?
congenital anomaly, protrusion of the urinary bladder through a defect in the abdominal wall.
WHat is the sonographic appearance of Bladder exostrophy?
soft-tissue mass protruding through abdomen
absence of urinary bladder
separation of pubic bone
What is a differential diagnosis of bladder exostrophy?
gastroschisis or omphalocele
What is a Testicular Hydrocele?
fluid-filled sac surrounding a testicle
usually benign
What is the sonographic appearance of Testicular Hydrocele?
simple fluid collection surrounding the testis.
What is Osteochondrodysplasia?
general term for a disorder of the development of bone and cartilage
hard to identify prenatally
* filler in multiple choice...usually missed by U/S
Explain the TC of a fetus with Osteochondrodysplasia?
measure small
What should you do if the femur measures small?
red flag
marker for trisomy 21
measure humerus
What is the key bone measurement?
femur length
When do the long bones begin to ossification?
end of embryonic period
week 12
What is TC?
thoracic circomuference
What are the first bones to ossify?
mandible & clavicle
Week 8
what usually occurs with musculoskeletal abnormalities?
polyhydramnios
fetal structural anomalies
family history of recurrent syndrome
Why are the most lethal musculoskeletal anomolies easier to identify?
they have severe presentations
What bones can be Acromelia?
carpal
metacarpal
tarsels
metatarsels
phalanges
Acromelia

Acromelia
What is Acromelia?
Bone abnormality shortening of distal limb segment.
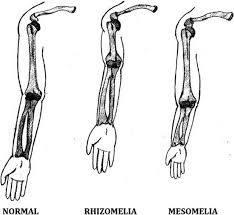
Acromelia

Mesomelia
What is Mesomelia?
shortening of middle limb segment.
What bones can be Mesomelic ?
tibia
fibula
ulnar
radius
What is Rhizomelic shortening?
Shortening of proximal limb segment

Rhizomelia
Rhizomelia
What bones can be Rhizomelic ?
femur
humerus
What is Micromelia shortening?
Shortening of proximal and distal limb segment
dwarfism
What is Extactyly?
Absence of fingers or toes
Hemimelia
What is Hemimelia?
Absence of below elbow or knee

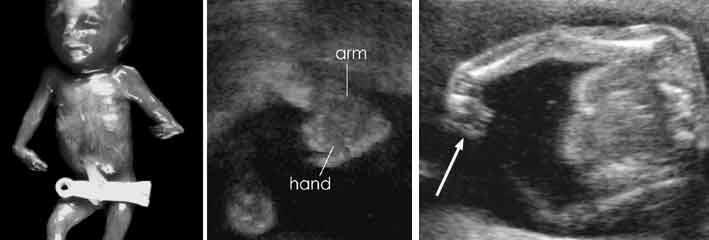
Phocomelia
Phocomelia
Phocomelia
What is Phocomelia?
Absence of middle segment
foot and hand would be attached to femur and humerus
What is Sirenomelia?
fusion of legs
mermaid syndrome

Sirenomelia
Sirenomelia
Sirenomelia
What is Dystoes?
Absence or malformation of individual bones
What is Arthrogryposis?
rigid extremities
What is the possible cause of Arthrogryposis?
olighydramnios
What is the sonographic appearance of Arthrogryposis?
joint contractures and rigidity.
head was severely hyperextended
fixed extremities
flexed arms
clubbed feet
clenched hands
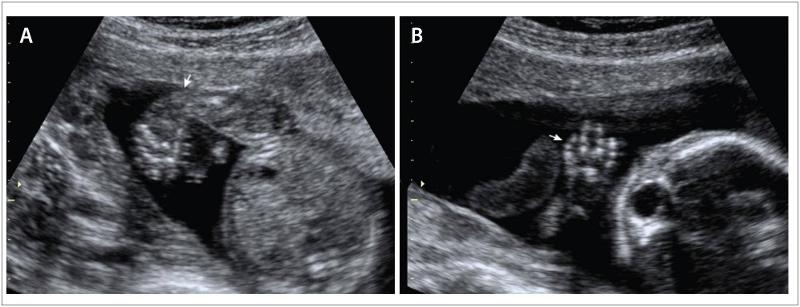
What is Polydactyly?
extra fingers or toes.
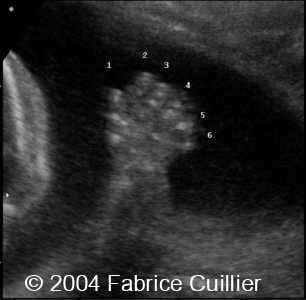
Polydactyly
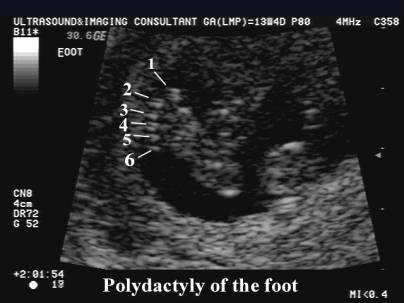
Polydactyly
Clinodactyly & club foot

Clinodactyly
What is Clinodactyly?
curvature of a digit
What is Pterygium?
webbing across joints
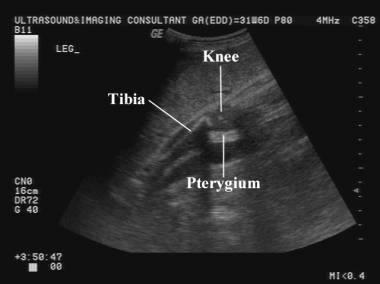
Pterygium
webbing across joints

Talipes equinovarus
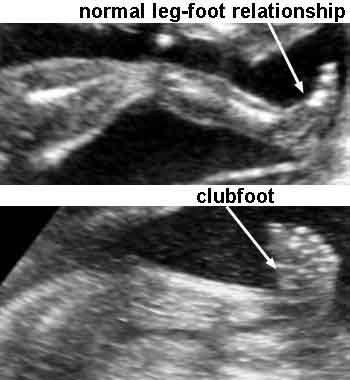
Talipes equinovarus

Ectrodactyly

Ectrodactyly
What is Talipes?
AKA Club foot.
front half of the foot turns inwards and downwards
What is Rocker-bottom feet?
prominent calcaneus and a convex rounded bottom to the foot. The foot resembles the bottom of a rocking chair.
marker for trisomy 18

Rockerbottom feet

Thanatophoric dysplasia
What are the lethal forms of Skeletal dysplasia?
Thanatophoric dysplasia
achondrogenesis
camptomelic dysplasia
osteogenesis imperfectal - Type II
Sirenomelia
What is the most common non-lethal bone dysplasia?
achondroplasia
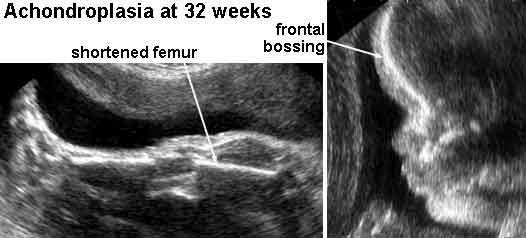
Achondroplasia
When can rhyzomelia be diagnosed in utero?
by femur length
27 - 30 weeks
measurement of femur length starts dropping off
What are the Non-lethal forms of Skeletal dysplasia?
achondroplasia
osteogenesis imperfecta Type IV
What is Thanatophporic Dysplasia?
severe skeletal disorder characterized by extremely short limbs and folds of extra skin on the arms and legs.
rhizomelia
bowed long bones
narrow thorax
large head
What is the most common form of lethal dwarfism?
Thanatophporic Dysplasia
causes severe micromelia
What is the sonographic appearance of Thanatophporic Dysplasia?
clover leaf skull
narrow chest
short ribs
underdeveloped lungs
enlarged head
large forehead and
prominent, wide-spaced eyes.

Kleeblattshadels
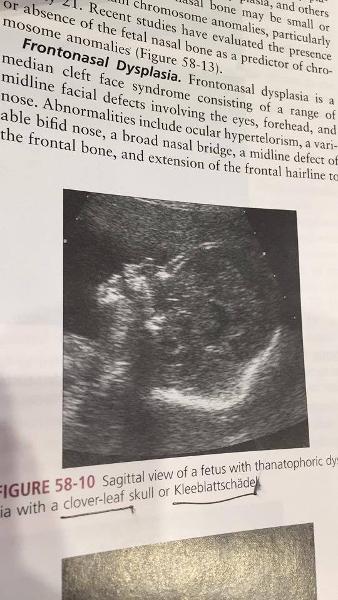
Kleeblattshadels
What is another name for cloverleaf skull?
kleeblattschädel
horseshoe
What are associated anomolies of Thanatophporic Dysplasia?
cloverleaf skull
horseshoe kidneys
ASD
imperforate anus
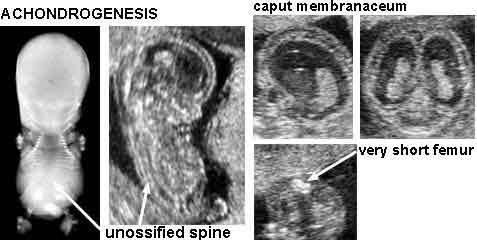
Achondrogenesis
What is the second most common form of lethal dwarfism?
Achondrogenesis
What is Achondrogenesis?
rare lethal form of short limbed dyplasia
severe malformation of bones and cartilage. Babies usually still born or die shortly
What are the two types of Achondrogenesis?
...
What is the sonographic appearance of Achondrogenesis?
demonstration of the triad
severely shortened limbs
lack of vertebral ossification
large head with slightly decreased ossification
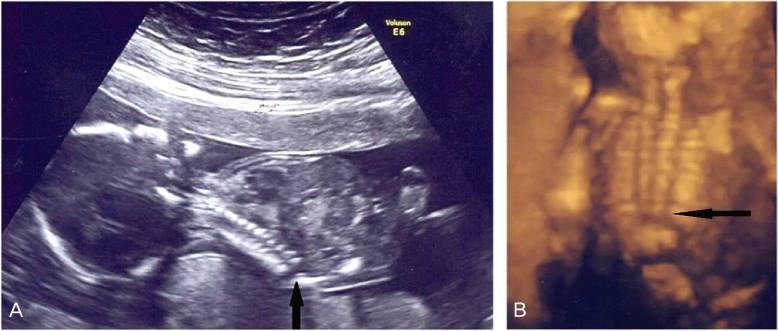
What is Camptomelic Dysplasia?
Camptomelic Dysplasia: bowing of the long bones
What are the most common bones affected by Camptomelic Dysplasia?
tibia
femur
What is the sonographic appearance of Camptomelic Dysplasia?
bowing of long bones
hydrocephalus
hydronephrosis
What are the anomolies associated with Camptomelic Dysplasia?
heart disease
hydrocephalus
hydronephrosis
What is caudal regression syndrome caused by?
early disruption of caudal portion of the neural tube
(sacral anomolies)
includes a range of anomolies
What is caudal regression syndrome?
fusion of the lower extremities
male prevalence 3:1
What is a mild case of caudal regression syndrome?
sacral anomalies
What is the most severe form of caudal regression syndrome?
Sirenomelia
Caudal regression syndrome
What are the associated anomalies of caudal regression syndrome?
diabetes
monozygotic twins
Sirenomelia
AKA Mermaid Syndrome, very rare congenital deformityin which the legs are fused together
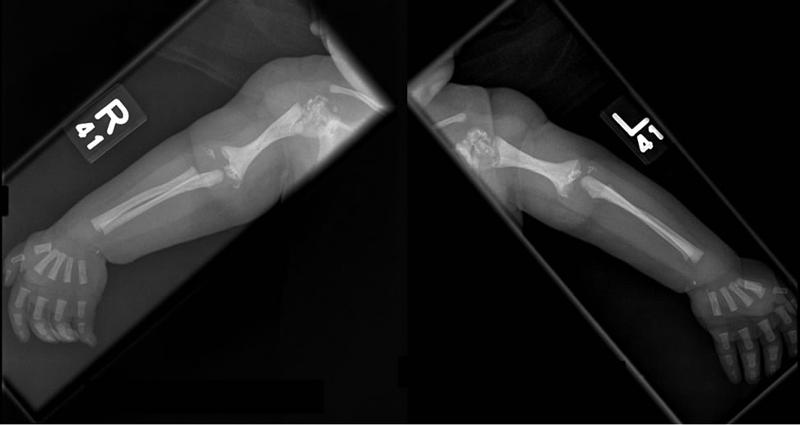
What is Osteogenesis Imperfecta Type II?
disorder of production, secretion or function of collagen
most severe form
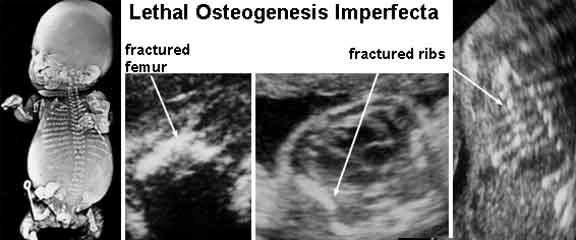
Osteogenesis Imperfecta type 2
What is Osteogenesis Imperfecta Type II characterized by?
bone fragility caused by hypominerization
What can delivery trauma lead to with Osteogenesis Imperfecta Type II?
intracranial hemorrhage
stillbirth
What is Osteogenesis Imperfecta Type IV?
AKA Brittle bone
fractured or bowed
demineralization of bone
Whe does Osteogenesis Imperfecta Type IV occur?
can occur in 3rd trimester
usually does not present until after birth
What is the sonographic appearance of Osteogenesis Imperfecta Type IV?
decreased echogenicity
fractures
cortical bone thinning
excessive trabecular bone transparency
What is Achondroplasia?
very short limbs and sometimes a face that is small in relation to the skull
What is VACTERL?
Vertebral defects
Anal atresia
Cardiac defects
TracheoEsophageal atresia
Renal anomalies
Limb anomolies
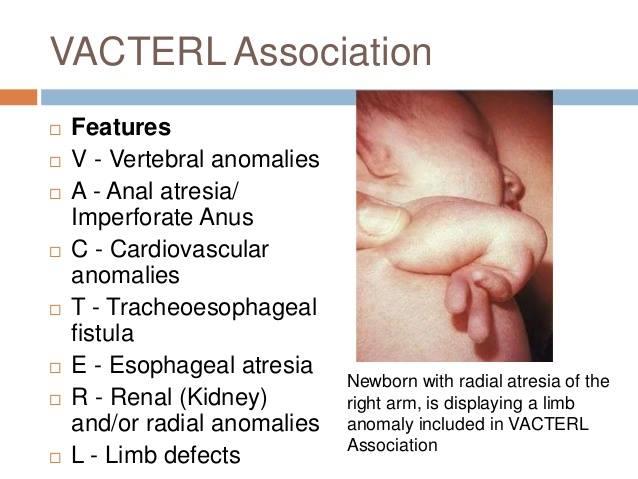
vacterl
Esophageal atresia
How many anomalies need to be present to be considered VACTERL?
3