The body contains two kinds of glands, what are they?
Exocrine and Endocrine
Secrete their products through ducts into body cavities or onto body surfaces. (sudoriferous, sebaceous, and digestive)
Exocrine glands
Secrete their products (hormones) into the extracellular spaces around the secretary cells, rather than into ducts. The secretion then diffuses into capillaries and is carried away by the blood.
Endocrine glands
The endocrine system consists of endocrine glands and several organs that contain endocrine tissue. True or False
True
In contrast, the endocrine system releases its messenger molecules, called _________, into the bloodstream
Hormones
The nervous system controls homeostasis through _________ conducted along axons of neurons.
Nerve impulses (action potentials)
Is the following true?
Certain parts of the nervous system stimulate or inhibit the release of hormones. Hormones, in turn, may not promote or inhibit the generation of nerve impulses. True or False
False
The nervous system causes muscles to contract and glands to secrete; the endocrine system affects virtually all body tissues, what does this system affect??
Altering metabolic activities, Regulating growth and development, and Guiding reproductive processes.
Nerve impulses are generally much more what?
Rapid, but brief when compared to those of the endocrine system.
Hormones regulate the what?
Internal environment, Metabolism, and Energy balance
Hormones also helps regulate what?
Smooth and cardiac muscular contraction, glandular secretion, and certain immune responses.
Hormones DO NOT play a role in the integration of growth and development, and in the maintenance of homeostasis despite emergency environmental disruptions, and contribute to the basic processes of reproduction. True or False
False
Hormones only affect specific________ that have _________ to recognize a given hormone.
Target cells and Receptors
Receptors, like other cellular proteins, are constantly synthesized and broken down. True or False
True
When a hormone (or neurotransmitter) is present in excess, the number of receptors may decrease __________, thereby decreasing the responsiveness of target cells to the hormone.
(Down-regulation)
When a hormone (or neurotransmitter) is deficient, the number of receptors may increase __________, making the target tissue more sensitive to the stimulating effect of the hormone.
(Up-regulation)
Hormones that pass into the blood to act on distant target cells are called what?
Circulating hormones or endocrines
Hormones that act on target cells close to their site of release are called what?
Local hormones (paracrines or autocrines).
Chemically, hormones are classified as what?
Steroids, Biogenic amines, Proteins and Peptides, and Eicosanoids (including prostaglandins and leukotrienes).
Water-soluble hormones circulate in free form in the blood; lipid-soluble steroid and thyroid hormones are carried attached to what?
Transport proteins
The response to a hormone depends on what?
Both the hormone and the target cell; various target cells respond differently to the same hormone.
Hormones bind to and activate their specific receptors in two quite different ways. True or False
True
These 2 hormones affect cell function by binding to and activating an intracellular receptor (usually in the nucleus), consequently altering gene expression. What are they?
Steroid hormones and Thyroid hormones
Altered by cell function by activating plasma membrane receptors, which initiate a cascade of events inside the cell. What is this called?
Water-soluble hormones
After a water-soluble hormone is release from an endocrine gland, it circulates in the blood, reaches a target cell, and brings a specific message to that cell; since such a hormone can deliver its message only to the plasma membrane, it is called the what?
First messenger
A _____________ is needed to relay the message inside the cell where hormone-stimulated responses can take place; the best known second messenger is cyclic AMP (cAMP) but other substances are known second messengers.
Second messenger
What is the best known second messenger?
Cyclic AMP (cAMP)
G-proteins are a common feature of most second messenger systems; the symptoms of cholera are a direct result of the cholera toxin on G-proteins in the intestinal lining. True or False
True
Cyclic AMP does not directly produce a particular physiological response, but instead activates one or more enzymes known as what?
Protein kinases
The responsiveness of a target cell to a hormone depends on the hormone’s concentration and the number of receptors. The manner in which hormones interact with other hormones is also important: three hormonal interactions are the? (Hint: Remember the 3 effects)
Permissive effect, Synergistic effect, and Antagonistic effect.
Is the following true?
- Most hormones are released in short bursts, with little or no release between bursts. Regulation of hormone secretion normally maintains homeostasis and prevents overproduction or underproduction of a particular hormone; when these regulating mechanisms do not operate properly, disorders result, many of which are discussed below.
- Hormone secretion is controlled by signals from the nervous system, by chemical changes in the blood, and by other hormones.
- Most often, negative feedback systems regulate hormonal secretions.
Yes they are all true facts.
What is the major integrating link between the nervous and endocrine systems?
Hypothalamus
The hypothalamus and the pituitary gland (hypophysis) do not regulate virtually all aspects of growth, development, metabolism, and homeostasis. True or False
False
Where is the pituitary gland is located???
Sell turcica of the sphenoid bone
Hormones of the adenohypophysis are controlled by releasing or inhibiting hormones produced by the what?
Hypothalamus
The blood supply to the anterior pituitary is from the superior hypophyseal arteries. It carries releasing and inhibiting hormones to the anterior pituitary. True or False
True
Histologically, the anterior pituitary consists of five principal types of glandular cells. What are they?
Hint: Sarah loves to cry to guys.
- Somatotrophs
- Lactotrophs
- Corticotrophs
- Thyrotrophs
- Gonadotrophs
Somatotrophs produce what hormone?
Human Grown Hormone (hGH)
hGH is produced by who?
Somatotrophs
Lactotrophs produce what hormone?
Prolactin (PRL)
Prolactin is produced by who?
Lactotrophs
Corticotrophs secrete what hormones?
Adrenocorticotropic hormone (ACTH) and Melanocyte-stimulating hormone (MSH)
Adrenocorticotropic hormone (ACTH) and melanocyte-stimulating hormone (MSH) are secreted by who?
Corticotrophs
Thyrotrophs secrete what hormone?
Thyroid-stimulating hormone (TSH).
Thyroid-stimulating hormone (TSH) are secreted by who?
Thyrotrophs
Gonadotrophs secrete what hormones?
Follicle-stimulating hormone (FSH) and Luteinizing hormone (LH)
Follicle-stimulating hormone (FSH) and Luteinizing hormone (LH) are secreted by who?
Gonadotrophs
Negative feedback systems will decrease the secretory activity of corticotrophs, thyrotrophs, and gonadotrophs if levels of their target gland hormones rise. True or False
True
Human growth hormone (hGH, GH, or somatotropin) does what?
Stimulates body growth through somatomedins and is controlled by GHIH (growth hormone inhibiting hormone, or somatostatin) and GHRH (growth hormone releasing hormone, or somatocrinin).
Disorders associated with improper levels of hGH are what?
Pituitary dwarfism, Giantism, and Acromegaly.
Thyroid-stimulating hormone (TSH or thyrotropin) does what?
Regulates thyroid gland activities and is controlled by TRH (thyrotropin release hormone).
Follicle-stimulating hormone (FSH) does what?
Regulates the activities of the ovaries and testes and is controlled by GnRH (gonadotropin releasing hormone).
Luteinizing hormone (LH) does what?
Regulates the activities of the ovaries and testes and is controlled by GnRH.
Prolactin (PRL or lactogenic hormone) does what?
Helps initiate milk secretion and is controlled by PIH (prolactin inhibiting hormone) and PRH (prolactin releasing hormone) from the hypothalamus.
Melanocyte-stimulating hormone (MSH) does what?
Increases skin pigmentation and is controlled by MRH (melanocyte-releasing hormone) and MIH (melanocyte-inhibiting hormone).
Adrenocorticotropic hormone (ACTH) does what?
Regulates the activities of the adrenal cortex and is controlled by CRH (corticotropin releasing hormone).
hGH stands for?
Human Growth Hormone
What does TSH stand for?
Thyroid-stimulating hormone
What does FSH mean?
Follicle-stimulating hormone
What does LH stand for?
Luteinizing hormone
What does PRL stand for?
Prolactin
What does MSH stand for?
Melanocyte-stimulating hormone
What does ACTH stand for?
Adrenocorticotropic hormone
Hormones made by the hypothalamus and stored in the posterior pituitary, what are they called?
Oxytocin (OT) and Antidiuretic hormone (ADH).
OT stands for?
Oxytocin
What does ADH stand for?
Antidiuretic hormone
Stimulates contraction of the uterus and ejection (let-down) of milk from the breasts; during labor and delivery, OT is released in large quantities.
Oxytocin (OT)
Stimulates water reabsorption by the kidneys and arteriolar constriction.
Antidiuretic hormone (ADH)
OT secretion is not controlled by uterine distention and nursing. True or False
False
Synthetic OT (Pitocin) is often given to induce labor or to increase uterine tone and control hemorrhage just after giving birth. True or False
True
The effect of ADH is to decrease urine volume and conserve body water. True or False
True
ADH is controlled primarily by osmotic pressure of the blood. True or False
True
The thyroid gland is located just below the _________ and has right and left lateral lobes.
Larynx
Histologically, the thyroid consists of thyroid follicles composed of follicular cells, which secrete the thyroid hormones called what?
thyroxine (T4) and triiodothyronine (T3) and calcitonin (CT)
IMPORTANT:
Thyroid hormones are synthesized from iodine and tyrosine within a large glycoprotein molecule called thyroglobulin (TGB) and are transported in the blood by plasma proteins, mostly thyroxine-binding globulin (TBG).
IMPORTANT:
(Watch out for confusion here since the order of the letters in these acronyms is easily reversed).
Thyroid hormones regulate the what?
Rate of metabolism, growth and development, and the reactivity of the nervous system. Secretion is controlled by the level of iodine in the thyroid gland and by negative feedback systems involving both the hypothalamus and the anterior pituitary. TRH (thyrotropin releasing hormone) and TSH (thyroid stimulating hormone) are responsible for initiating thyroid activity.
Disorders associated with the thyroid gland are what?
Cretinism, myxedema, Graves’ disease, and goiter
Calcitonin (CT) lowers the blood level of calcium. Secretion is controlled by calcium levels in the blood. True or False
True
The parathyroid glands are embedded where?
Posterior surfaces of the lateral lobes of the thyroid.
The parathyroids consist of what?
principal (chief) and oxyphil cells, which secrete parathyroid hormone (PTH), or parathormone.
Parathyroid hormone (PTH), or parathormone, regulates what?
The homeostasis of calcium and phosphate by increasing blood calcium level and decreasing blood phosphate level. Secretion is controlled by calcium level in the blood.
Disorders associated with parathyroid glands, what are they?
Tetany and Osteitis fibrosa cystica
Tetany results from what?
From a deficiency of calcium caused by hypoparathyroidism.
Osteitis fibrosa cystica is characterized by what?
Emineralized, weakened, and deformed bones, resulting from the condition of hyperparathyroidism.
The adrenal glands are located where?
Superior to the kidneys; they consist of an outer cortex and inner medulla.
Histologically, the cortex is divided into 3 zones what are they?
zona glomerulosa
zona fasciculata
zona reticularis
Increase sodium and water reabsorption and decrease potassium reabsorption, helping to regulate sodium and potassium levels in the body. What is this called?
Mineralocorticoids (e.g., aldosterone)
A dysfunction related to aldosterone hypersecretion is what?
Aldosteronism
Secretion is not controlled by the renin-angiotension pathway and the blood level of potassium. True or False
False
Promote normal organic metabolism, help resist stress, and serve as anti-inflammatory substances. What is this called?
Glucocorticoids (e.g., cortisol)
Secretion is controlled by CRH (corticotropin releasing hormone) and ACTH (adrenocorticotropic hormone) from the anterior pituitary. True or False
True
Disorders associated with glucocorticoid secretion are what?
Addison’s disease and Cushing’s syndrome
Secreted by the adrenal cortex usually have minimal effects. What is this called?
Gonadocorticoids (sex hormones) (e.g., estrogens and androgens)
Excessive production occurs in congenital adrenal hyperplasia (CAH), resulting in virilism (masculinization). True or False
True
Virilism or gynecomastia (excessive growth of male mammary glands) may also result from tumors of the adrenal gland. True or False
True
- The adrenal medulla consists of hormone-producing cells, called __________ , which surround large blood-filled sinuses.
Chromaffin cells
Medullary secretions are epinephrine and norepinephrine (NE), which produce effects similar to ___________.
They are released under stress by direct innervation from the autonomic nervous system. Like the glucocorticoids of the adrenal cortex, these hormones help the body resist stress. However, unlike the cortical hormones, the medullary hormones are not essential for life.
Sympathetic responses
Tumors of the chromaffin cells, called _______. These cause hypersecretion of epinephrine and norepinephrine. Since these hormones create the same effect as sympathetic nervous stimulation, hypersecretion puts the individual into a prolonged state of fight-or-flight response, ultimately causing generalized fatigue and weakness.
Pheochromocytomas
The pancreas is a flattened organ located where?
Posterior and slightly inferior to the stomach and can be classified as both an endocrine and an exocrine gland.
What organ can be classified as both as a endocrine and an exocrine gland?
Pancreas
Histologically, the pancreas consists of pancreatic islets or islets of Langerhans and clusters of cells (acini) (enzyme-producing exocrine cells). Four types of hormone-secreting cells compose the pancreatic islets. True or False
True
Secrete the hormone glucagon
Alpha cells
Alpha cells secrete what hormone?
Glucagon
Alpha cells secretion is stimulated by what?
Low blood glucose level.
Glucagon increases blood glucose levels. True or False
True
Beta cells secrete what hormone?
Insulin
Insulin is secreted from where?
Beta Cells
Insulin decreases blood glucose levels. True or False
True
Insulin secretion is stimulated by what?
High blood glucose levels
Disorders associated with insulin production are what?
diabetes mellitus and hyperinsulinism
These are located in the pelvic cavity and produce sex hormones (estrogens and progesterone) related to development and maintenance of female sexual characteristics, reproductive cycle, pregnancy, lactation, and normal reproductive functions. These also produce inhibin and relaxin.
Ovaries
Ovaries produce what hormone?
Estrogen
Progesterone
Inhibin
Relaxin
Lies inside the scrotum and produce sex hormones (primarily testosterone) related to the development and maintenance of male sexual characteristics and normal reproductive functions. The testes also produce inhibin.
Testes
Testes produce what hormones?
Testosterone
Inhibin
Testes and ovaries both produce this hormone, what is it?
Inhibin
Is attached to the roof of the third ventricle, inside the brain. What is it?
Pineal gland (epiphysis cerebri)
Histologically, pineal gland consists of secretory parenchymal cells called parenchymal cells called pinealocytes, neuroglial cells, and scattered postganglionic sympathetic fibers. True or False
True
The pineal secretes melatonin in a diurnal rhythm linked to the dark-light cycle. That helps you to fall asleep. True or False
True
A type of depression that arises during the winter months when day length is short, is thought to be due, in part, to over-production of melatonin. Bright light therapy, repeated doses of several hours of exposure to artificial light as bright as sunlight, may provide relief for this disorder and for jet lag.
Seasonal affective disorder (SAD)
Secretes several hormones related to immunity, this is called?
Thymus gland
The thymus produces what hormones?
Thymosin,
Thymic humoral factor (THF),
Thymic factor (TF),
Thymopoietin
What do the hormones of the Thymus gland do???
Promote the proliferation and maturation of T cells, a type of white blood cell involved in immunity.
Prostaglandins (PGs) and leukotrienes (LTs) do not act as paracrines and autocrines in most body tissues by altering the production of second messengers, such as cyclic AMP. True or False
False
Prostaglandins have a wide range of biological activity in normal physiology and pathology. True or False
True
Aspirin and related nonsteroidal anti-inflammatory drugs (NSAIDS), such as ibuprofen and acetaminophen, inhibit a key enzyme in prostaglandin synthesis and are used to treat a wide variety of inflammatory disorders. True or False
True
___________ are hormones that stimulate cell growth and division.
Growth factors
Examples include epidermal growth factor (EGF), platelet-derived growth factor (PDGF), fibroblast growth factor (FGF), nerve growth factor (NGF), tumor angiogenesis factors (TAFs), insulin-like growth factor (IGF), and cytokines. True or False
True
____________ is initiated by nerve impulses from the hypothalamus to the sympathetic division of the autonomic nervous system and adrenal medulla.
Responses are the immediate and brief fight-or-flight reactions that increase circulation promote catabolism for energy production, and decrease nonessential activities.
Alarm reaction
____________ is initiated by regulating hormones secreted by the hypothalamus.
The regulating hormones are CRH (corticotrophin releasing hormone), GHRH (growth hormone releasing hormone), and TRH (thyrotropin releasing hormone).
CRH stimulates the adenohypophysis (anterior pituitary) to increase its secretion of ACTH (adrenocorticotropic hormone), which in turn stimulates the adrenal cortex to secrete hormones.
Resistance reactions are long-term and accelerate catabolism to provide energy to counteract stress.
Glucocorticoids are produced in high concentrations during stress. They create many distinct physiological effects.
Resistance reaction
____________ results from dramatic changes during alarm and resistance reactions.
Exhaustion is caused mainly by loss of potassium, depletion of adrenal glucocorticoids, and weakened organs. If stress is too great, it may lead to death.
Stage of exhaustion
- It appears that stress can lead to certain diseases.
- Among stress-related conditions are gastritis, ulcerative colitis, irritable bowel syndrome, peptic ulcers, hypertension, asthma, rheumatoid arthritis (RA), migraine headaches, anxiety, and depression.
- It has also been shown that people under stress are at a greater risk of developing chronic disease or of dying prematurely.
- A very important link between stress and immunity is interleukin-1 (IL-1) produced by macrophages; it stimulates secretion of ACTH.
True or False
End of chapter 18
True
Blood inside blood vessels, interstitial fluid around body cells, and lymph inside lymph vessels constitute one’s what?
Internal environment.
The blood, heart, and blood vessels together make up the cardiovascular system. True or False
True
The lymph, lymphatic vessels that transport lymph, and structures and organs containing lymphatic tissue (large clusters of white blood cells called lymphocytes) make up the what???
Lymphatic system.
The branch of science concerned with the study of blood, blood-forming tissues, and the disorders associated with them is called?
Hematology.
FUNCTIONS OF THE BLOOD ARE WHAT?
- Blood transports oxygen, carbon dioxide, nutrients, heat, wastes, and hormones.
- It helps regulate pH, body temperature, and water content of cells.
- It prevents blood loss through clotting and combats toxins and microbes through certain phagocytic white blood cells or specialized plasma proteins.
Physical characteristics of blood include a viscosity greater than that of water; temperature, 38°C (100.4°F); and a pH of 7.35 to 7.45. True or False
True
The pH of blood is what?
7.35 to 7.45
Blood constitutes about ________ of body weight; volume ranges from 4 to 6 liters.
8%
Blood samples for laboratory testing may be obtained by?
Venipuncture, Finger-stick, or A rterial stick.
Blood consists of 55% plasma and 45% formed elements.
Blood consists of 55% plasma and 45% formed elements.
Plasma consists of 91.5% and 8.5% solutes.
Plasma consists of 91.5% and 8.5% solutes.
Principal solutes include proteins (albumins, globulins, fibrinogen), nutrients, enzymes, hormones, respiratory gases, electrolytes, and waste products. True or False
True
- The __________ in blood include erythrocytes (red blood cells), leukocytes (white blood cells), and thrombocytes (platelets).
Formed elements
Formed elements come from where?
Erythrocytes (red blood cells)
Leukocytes (white blood cells)
Thrombocytes (platelets).
Blood cells are formed from pluripotent hematopoietic stem cells called?
Hemocytoblasts
Hemopoiesis (or hematopoiesis) is stimulated by several hematopoietic growth factors. These hematopoietic growth factors stimulate differentiation and proliferation of the various blood cells. True or False
True
Red bone marrow (myeloid tissue) is responsible for producing red blood cells, granular leukocytes, and platelets; lymphoid tissue and myeloid tissue produce agranular leukocytes. True or False
True
Are biconcave discs without nuclei that contain what?
Hemoglobin
Erythrocytes are known as?
Red blood cells or RBC"s
Hemoglobin molecules are specialized components of the red blood cell plasma membrane which combine with oxygen (as oxyhemoglobin) or with carbon dioxide (as carbaminohemoglobin) in this transport process. True or False
True
A serious disorder called sickle-cell anemia (SCA) is due to what?
A genetic defect in the structure of hemoglobin in affected individuals.
Has been used by some athletes in an attempt to boost the oxygen-carrying capacity of their blood before an athletic event. Although evidence suggests that there may be performance benefits related to the procedure, the potential risks from higher blood viscosity are unknown and the practice is considered dishonest by the International Olympics Committee. What is this called?
Induced erythrocytemia (blood doping)
Red blood cells live for how long?
90-120 days
A healthy male has how many red blood cells?
5.4 million RBCs/mm3
A healthy female has how many red blood cells?
4.8 million/mm3
After phagocytosis of worn-out RBCs by macrophages, hemoglobin is ________. The globin portion is split from the heme with the amino acids being reused for protein synthesis. The iron in the heme portion is reclaimed with the rest of the heme molecule; the rest becomes a component of bile in the digestive process.
Recycled
Erythrocyte formation is called what?
Erythropoiesis
Occurs in adult red bone marrow of certain bones. It is stimulated by hypoxia, which stimulates release of ____________ by the kidneys.
Erythropoietin .
A reticulocyte count (average 0.5%-1.5% of all RBCs) is a diagnostic test that indicates the rate of erythropoiesis, useful in diagnosing and treating anemia. True or False
True
Measures the percentage of red blood cells in whole blood.
Hematocrit (Hct)
An average male has a hematocrit range of?
47% (range of 40-54%)
Females have a hematocrit range of?
42% (range of 38-46%)
Leukocytes (white blood cells, or WBCs) are nucleated cells and do not contain hemoglobin. True or False
True
Are nucleated cells and do not contain hemoglobin, what is this called?
Leukocytes (white blood cells, or WBCs)
Neutrophils, Eosinophils, Basophils are what? G ranular or Agranular
Granular
Lymphocytes and Monocytes are what? G ranular or Agranular
Agranular
Leukocytes have surface proteins, as do erythrocytes
Leukocytes have surface proteins, as do erythrocytes
Are unique for each person (except for identical twins), and can be used to identify a tissue. What is this called?
Major histocompatibility antigens (MHC)
Is performed to determine tissue compatibility between a donor and a recipient before any organ transplant. What is this called?
Tissue typing (histocompatibility testing)
The general function of leukocytes is to what?
To combat inflammation and infection.
___________ and wandering or fixed macrophages (which develop from monocytes) do so through phagocytosis.
Neutrophils
__________ combat the effects of histamine in allergic reactions, phagocytize antigen-antibody complexes, and combat parasitic worms.
Eosinophils
___________ develop into mast cells that liberate heparin, histamine, and serotonin in allergic reactions that intensify the inflammatory response.
Basophils
____________ in response to the presence of foreign substances called antigens, differentiate into tissue plasma cells that produce antibodies.
-Antibodies attach to the antigens and render them harmless.
-This antigen-antibody response combats infection and provides immunity.
B lymphocytes
This destroys foreign invaders directly.
T lymphocytes
Is a diagnostic test in which specific white blood cells are enumerated. Because each type of white cell plays a different role, determining the percentage of each type in the blood assists in diagnosing the condition. What is this called?
A differential white blood cell count
White blood cells usually live for only a few hours or a few days. Normal blood contains 5,000-10,000 leukocytes/mm3. True or False
True
May be used to treat several types of anemia, leukemia, and numerous other blood disorders. What is this called?
Bone marrow transplants
Are disc-shaped structures without nuclei, what is this called?
- They are formed as fragments from meta-megakaryocytes; they help repair slightly damaged blood vessels and promote blood clotting.
- Normal blood contains 250,000 to 400,000 platelets/mm3. Platelets have a life span of only 5-9 days; aged and dead platelets are removed by fixed macrophages in the spleen and liver.
Thrombocytes, or Platelets
Is used to determine blood cell counts, hemoglobin, hematocrit, white blood cell count, differential white blood cell count, and platelet count. What is this called?
Complete blood count (CBC)
This refers to the stoppage of bleeding. When blood vessels are damaged or ruptured, the hemostatic response must be quick, localized to the region of damage, and carefully controlled. What is this called?
Hemostasis
Hemostasis involves vascular spasm, platelet plug formation, and blood coagulation (clotting). True or False
True
The smooth muscle of a blood vessel wall contracts to stop bleeding. What is this called?
Vascular spasm
Involves the clumping of platelets around the damage to stop the bleeding. What is this called?
Platelet plug formation
- A ______ is a gel consisting of a network of
insoluble protein fibers (fibrin) in which formed elements of blood
are trapped.
- The chemicals involved in clotting are known as coagulation (clotting) factors; most are in blood plasma, some are released by platelets, and one is released from damaged tissue cells.
- Blood clotting
involves a cascade of reactions that may be divided into three
stages.
- Formation of prothrombinase (prothrombin activator)
- Conversion of prothrombin into thrombin.
- Conversion of solute fibrinogen into insoluble fibrin
Clot
The formation of prothrombinase is initiated by the interplay of two mechanisms called the extrinsic and intrinsic pathways of blood clotting. True or False
True
Refers to several different hereditary deficiencies of coagulation in which bleeding may occur spontaneously or after only minor trauma. What is this called?
Hemophilia
The formation of prothrombinase is initiated by the interplay of two mechanisms called?
Extrinsic
Intrinsic
Normal coagulation requires vitamin K and also involves?
Clot retraction (or syneresis, tightening of the clot) and fibrinolysis (dissolution of the clot).
Tightening of the clot this called?
Syneresis
Dissolution of the clot is called?
Fibrinolysis
_____________ are chemical substances injected into the body that dissolve blood clots to restore circulation; the most common use is in treatment of clots in coronary arteries of the heart (streptokinase and tissue plasminogen activator, or t-PA).
Thrombolytic (clot-dissolving) agents
- Substances that inhibit coagulation, called ____________, are also present in blood. An example is heparin.
Anticoagulants
Despite the anticoagulating and fibrinolytic mechanisms, blood clots sometimes form within the cardiovascular system. True or False
True
Clotting in an unbroken blood vessel is called what?
Thrombosis
A __________ bubble of air, fat from broken bones, or piece of debris transported by the bloodstream that moves from its site of origin is called an embolus.
Thrombus (clot)
The surfaces of red blood cells contain genetically determined blood group antigens, called agglutinogens or isoantigens, and the plasma of many persons contains genetically determined antibodies, called agglutinins or isoantibodies, against the blood group antigens which they do not have. True or False
True
agglutinogens
isoantigens
agglutinins
isoantibodies
All of these are simply known as what?
Antigens
The ABO and Rh blood grouping systems are based on antigen-antibody responses. True or False
True
Individuals whose erythrocytes have Rh agglutinogens are classified as Rh+ and those who lack the antigen are Rh-. True or False
True
A disorder due to Rh incompatibility between mother and fetus is called what? Also This disease is treatable, but also preventable
Hemolytic disease of the newborn (HDN), or erythroblastosis fetalis
Is a condition in which the oxygen-carrying capacity of the blood is reduced; it is a sign, not a diagnosis and is usually characterized by a decreased erythrocyte count or hemoglobin deficiency. What is this called?
Anemia
Kinds of anemia include are what?
Nutritional,
pernicious,
hemorrhagic,
hemolytic,
aplastic,
sickle-cell (SCA).
Is an abnormal increase in the number of erythrocytes (Hct > 55%). Increased viscosity of the blood causes a rise in blood pressure and contributes to thrombosis and hemorrhage. What is this called?
Polycythemia
Is a contagious disease that primarily affects lymphoid tissue. It is characterized by an elevated white blood cell count, with an abnormally high percentage of lymphocytes. The cause is the Epstein-Barr virus (EBV). What is this called?
Infectious mononucleosis (IM)
___________ is a malignant disease of blood-forming tissue characterized by the uncontrolled production of white blood cells that interferes with normal clotting and vital body activities. It is classified based on the duration and character of the disease and also according to the identity and site of origins of the predominant cell involved (myelocytic, lymphocytic, or monocytic).
Leukemia
Is characterized by uncontrolled production and accumulation of immature leukocytes. What is this called?
Acute leukemia
In ________, there is an accumulation of mature leukocytes in the bloodstream because they do not die at the end of their normal life span.
Chronic leukemia
End of Chapter 19
End of Chapter 19
What organ is the center of the cardiovascular system?
Heart
LOCATION AND SIZE OF THE HEART
- The heart is situated between the lungs in the mediastinum.
- About two-thirds of its mass is to the left of the midline.
- The heart is about 12 cm long, 9 cm wide, and 6 cm thick
The heart is enclosed by and held in place by?
Pericardium
The pericardium consists of an outer ______________ and an inner ___________.
fibrous pericardium (out) and serous pericardium (inner)
The serous pericardium is not composed of a parietal layer and a visceral layer. True or False
False
Between the parietal and visceral layers of the serous pericardium is the ___________, a potential space filled with pericardial fluid that reduces friction between the two membranes.
Pericardial cavity
Pericardial fluid does what?
Reduces friction between membranes
An inflammation of the pericardium is known as what?
Pericarditis
Associated bleeding into the pericardial cavity compresses the heart (cardiac tamponade) and is potentially lethal. True or False
True
The wall of the heart has three layers: what are they?
Hint: Think "eat my egg"
Epicardium
Myocardium
Endocardium
The epicardium consists of?
Mesothelium and Connective tissue
The myocardium is composed of?
Cardiac muscle tissue
The endocardium consists of?
Endothelium and Connective tissue.
The chambers of the heart include?
Two upper atria and two lower ventricles.
What separates the atria??
Interatrial septum
What separates the ventricles?
Interventricular septum
What does septum mean?
A wall

Blood flows through the heart from the superior and inferior venae cavae and the coronary sinus to the right atrium, through the tricuspid valve to the right ventricle, through the pulmonary trunk and pulmonary arteries to the lungs, through the pulmonary veins into the left atrium, through the bicuspid valve to the left ventricle, and out through the aorta.

Blood flows through the heart from the superior and inferior venae cavae and the coronary sinus to the right atrium, through the tricuspid valve to the right ventricle, through the pulmonary trunk and pulmonary arteries to the lungs, through the pulmonary veins into the left atrium, through the bicuspid valve to the left ventricle, and out through the aorta.
Divisions of the aorta are the?
1. Ascending aorta
2. Arch of the aorta
3. Thoracic aorta
4. Abdominal aorta.
These are composed of dense connective tissue covered by endothelium, prevent backflow of blood in the heart. What are they?
Valves

Atrioventricular (AV) valves, between the atria and their ventricles, are the tricuspid valve on the right side of the heart and the bicuspid (mitral) valve on the left. True or False

True

The chordinae tendineae and their papillary muscles keep the flaps of the valves pointing in the direction of the blood flow and stop blood from backing into the atria. True or False

True

____________ prevent blood from flowing back into the heart as it leaves the heart for the lungs (pulmonary semilunar valve) or for the rest of the body (aortic semilunar valve).

Semilunar valves
____________ is precipitated by infection with group A, β-hemolytic strains of Streptococcus pyogenes The ultimate result is damage to valves of the heart, most commonly the bicuspid and aortic semilunar valves.
Rheumatic fever
The flow of blood through the many vessels that pierce the myocardium of the heart is called the _________ ; it delivers oxygenated blood and nutrients to the myocardium and removes carbon dioxide and wastes from it.
Coronary (cardiac) circulation
The principle arteries, branching from the ascending aorta and carrying oxygenated blood, are the right and left coronary arteries; deoxygenated blood returns to the right atrium primarily via the principal vein, the __________. .
Coronary sinus.
Most heart problems results from faulty coronary circulation due to blood clots, fatty atherosclerotic plaques, or spasm of the smooth muscle in coronary artery walls. Complications of this system include angina pectoris (severe pain that accompanies reduced blood flow, or ischemia, to the myocardium) and myocardial infarction (MI, or heart attack, in which there is death of an area of the myocardium due to an interruption of the blood supply; it may result from a thrombus or embolus). True or False
True
Whenever a disease or injury deprives a tissue of oxygen, reestablishing the blood flow (reperfusion) may damage the tissue further due to the formation of oxygen free radicals; these can destabilize the molecular structure of proteins, neurotransmitters, nucleic acids, and phospholipids of plasma membranes. True or False
True
An ___________ may be used to restore cardiac rhythm due to disruption of some component of the conduction system.
Artificial pacemaker
A recording of the electrical changes that accompany each cardiac cycle (heartbeat) is called an?
Electrocardiogram (ECG or EKG)
Who developed the electrocardiogram? And when?
Mtoren in 1830
A normal ECG consists of a P wave (atrial depolarization – spread of impulse from SA node over atria), QRS complex (ventricular depolarization – spread of impulse through ventricles), and T wave (ventricular repolarization). True or False
True
A normal ECG consists of a?
P wave (atrial depolarization – spread of impulse from SA node over atria), QRS complex (ventricular depolarization – spread of impulse through ventricles), and T wave (ventricular repolarization)
The __________ represents the conduction time from the beginning of atrial excitation to the beginning of ventricular excitation.
Full ventricular depolarization/plateau of the ventricles
P-Q (PR) interval
The _________ represents the time when ventricular contractile fibers are fully depolarized, during the plateau phase of the impulse.
S-T segment
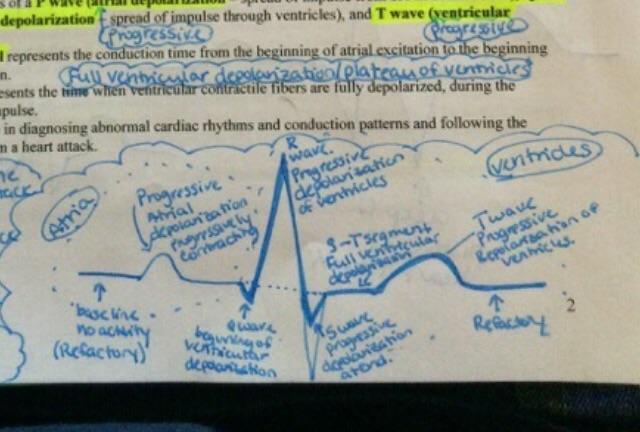
The ECG is invaluable in diagnosing abnormal cardiac rhythms and conduction patterns and following the course of recovery from a heart attack.
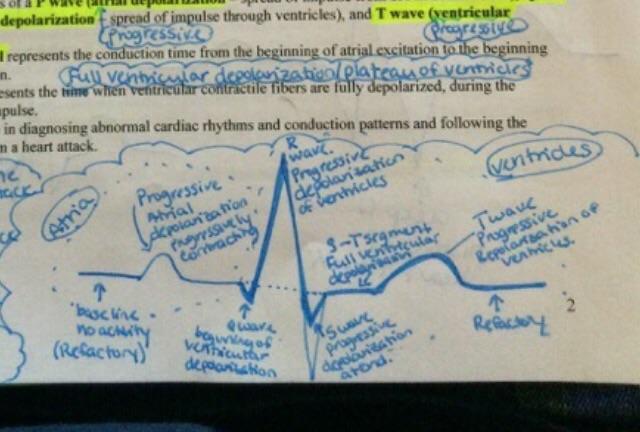
The ECG is invaluable in diagnosing abnormal cardiac rhythms and conduction patterns and following the course of recovery from a heart attack.
A __________ consists of the systole (contraction) and diastole (relaxation) of both atria, rapidly followed by the systole and diastole of both ventricles.
Cardiac cycle
The phases of the cardiac cycle are?
(1) the relaxation (or quiescent) period, (2) ventricular filling, and (3) ventricular systole.
With an average heart rate of 75 beats/min, a complete cardiac cycle requires 0.8 sec. True or False
True
A ___________ is an abnormal sound that consists of a flow noise that is heard before, between, or after the lubb-dupp or that may mask the normal sounds entirely. Some murmurs are caused by turbulent blood flow around valves due to abnormal anatomy or increased volume of flow.
Heart murmur
The act of listening to sounds within the body is called? And is usually done with a stethoscope.
Auscultation
The sound of a heartbeat comes primarily from the turbulence in blood flow caused by the closure of the valves, not from the contraction of the heart muscle. True or False
- The first heart sound (S1 – lubb) is created by blood turbulence associated with the closing of the atrioventricular valves soon after ventricular systole begins.
- The second heart sound (S2 – dupp) represents the closing of the semilunar valves close to the end of ventricular systole.
True
- A heart murmur is an abnormal sound that consists of a flow noise that is heard before, between, or after the lubb-dupp or that may mask the normal sounds entirely. Some murmurs are caused by turbulent blood flow around valves due to abnormal anatomy or increased volume of flow.
- Not all murmurs are abnormal or symptomatic, but most indicate a valve disorder.
- Among the valvular disorders that may contribute to murmurs are mitral stenosis, mitral insufficiency, aortic stenosis, aortic insufficiency, and mitral valve prolapse (MVP).
- A heart murmur is an abnormal sound that consists of a flow noise that is heard before, between, or after the lubb-dupp or that may mask the normal sounds entirely. Some murmurs are caused by turbulent blood flow around valves due to abnormal anatomy or increased volume of flow.
- Not all murmurs are abnormal or symptomatic, but most indicate a valve disorder.
- Among the valvular disorders that may contribute to murmurs are mitral stenosis, mitral insufficiency, aortic stenosis, aortic insufficiency, and mitral valve prolapse (MVP).
___________ is the amount of blood ejected by the left ventricle (or right ventricle) into the aorta (or pulmonary trunk) per minute. It is calculated as follows:
CO = stroke volume x beats per minute
Cardiac output (CO)
Is the amount of blood ejected by a ventricle during each systole.
Stroke volume (SV)
Stroke volume depends on how much blood enters a ventricle during diastole, that is, the stretch on the heart before it contracts (end-diastolic volume, or EDV, also called preload), and how much blood is left in a ventricle following its systole (end-systolic volume, or ESV). EDV averages 120-130 ml and SV is about 70 ml; ESV, then is approximately 50-60 ml.
Stroke volume depends on how much blood enters a ventricle during diastole, that is, the stretch on the heart before it contracts (end-diastolic volume, or EDV, also called preload), and how much blood is left in a ventricle following its systole (end-systolic volume, or ESV). EDV averages 120-130 ml and SV is about 70 ml; ESV, then is approximately 50-60 ml.
Stroke volume also is related to contractility (forcefulness of contraction at any given time) and afterload (pressure that must be exceeded before ventricular ejection can begin); factors that increase the stroke volume or heart rate tend to increase CO and vice versa.
Stroke volume also is related to contractility (forcefulness of contraction at any given time) and afterload (pressure that must be exceeded before ventricular ejection can begin); factors that increase the stroke volume or heart rate tend to increase CO and vice versa.
_________ is the ratio between the maximum cardiac output a person can achieve and the cardiac output at rest.
Cardiac reserve
According to the Frank-Startling law of the heart, a greater preload (stretch) on cardiac muscle fibers just before they contract increases their force of contraction during systole. True or False
True
A greater preload (stretch) on cardiac muscle fibers just before they contract increases their force of contraction during systole. What is this called?
Frank-Startling law of the heart
This results when the heart cannot supply the oxygen demands of the body; it is characterized by diminished blood flow to the various tissues of the body and by accumulation of excess blood in the various organs because the heart is unable to pump out the blood returned to it by the great veins. Causes include chronic hypertension and myocardial infarction (heart attack). What is this called?
Congestive heart failure (CHF)
Cardiac output does not depends on heart rate as well as stroke volume. True or False
False
- Nervous system control of the cardiovascular system stems from
the cardiovascular center in the medulla.
- Sympathetic impulses increase heart rate and force of contraction; parasympathetic impulses decrease heart rate.
- Baroreceptors (pressure receptors) are nerve cells that respond to changes in blood pressure and relay the information to the cardiovascular center; important baroreceptors are located in the arch of the aorta and carotid arteries.
- Nervous system control of the cardiovascular system stems from
the cardiovascular center in the medulla.
- Sympathetic impulses increase heart rate and force of contraction; parasympathetic impulses decrease heart rate.
- Baroreceptors (pressure receptors) are nerve cells that respond to changes in blood pressure and relay the information to the cardiovascular center; important baroreceptors are located in the arch of the aorta and carotid arteries.
- Heart rate is also affected by hormones (epinephrine, norepinephrine, thyroid hormones), ions (Na+, K+, Ca2+), age, gender, physical fitness, and temperature.
- Heart rate is also affected by hormones (epinephrine, norepinephrine, thyroid hormones), ions (Na+, K+, Ca2+), age, gender, physical fitness, and temperature.
Help for Failing Hearts
- Although a variety of drugs are helpful in the earlier stages of heart disease, at some point they are no longer effective because there is too little functional cardiac muscle left.
Researchers are investigating a wide variety of devices and techniques to aid a failing heart, including heart transplants, artificial hearts, and cardiac assist devices
Help for Failing Hearts
- Although a variety of drugs are helpful in the earlier stages of heart disease, at some point they are no longer effective because there is too little functional cardiac muscle left.
Researchers are investigating a wide variety of devices and techniques to aid a failing heart, including heart transplants, artificial hearts, and cardiac assist devices
___________ in heart disease that can be modified include high blood cholesterol level, high blood pressure cigarette smoking, obesity, and lack of regular exercise. Other factors include diabetes mellitus; genetic predisposition; male gender; high blood levels of fibrinogen, renin, and uric acid; and left ventricular hypertrophy.
Risk factors
An __________ is an abnormality or irregularity in the heart rhythm resulting from a disturbance in the conduction system of the heart; due either to faulty production of electrical impulses or to poor conduction of impulses as they pass through the system.
arrhythmia
- Examples of arrhythmias include heart block
(most commonly atrioventricular block,
flutter, fibrillation
(atrial and ventricular), and
premature ventricular contraction (PVC).
- Some are caused by the effects of such factors as caffeine, nicotine, alcohol, anxiety, certain drugs, hyperthyroidism, potassium deficiency, and certain heart diseases.
- Most can be controlled if detected and treated early enough.
- Examples of arrhythmias include heart block
(most commonly atrioventricular block,
flutter, fibrillation
(atrial and ventricular), and
premature ventricular contraction (PVC).
- Some are caused by the effects of such factors as caffeine, nicotine, alcohol, anxiety, certain drugs, hyperthyroidism, potassium deficiency, and certain heart diseases.
- Most can be controlled if detected and treated early enough.
- Coronary artery disease (CAD), or coronary heart disease (CHD), is a condition in which the heart muscle receives an inadequate amount of blood due to obstruction of its blood supply. It is the leading cause of death in the United States each year. The principal causes of narrowing include atherosclerosis, coronary artery spasm, or a clot in a coronary artery.
- Coronary artery disease (CAD), or coronary heart disease (CHD), is a condition in which the heart muscle receives an inadequate amount of blood due to obstruction of its blood supply. It is the leading cause of death in the United States each year. The principal causes of narrowing include atherosclerosis, coronary artery spasm, or a clot in a coronary artery.
___________ is a process in which smooth muscle cells proliferate and fatty substances especially cholesterol and triglycerides (neural fats), accumulate in the walls of medium-sized and large arteries in response to certain stimuli, such as endothelial damage.
Atherosclerosis
- Treatment of coronary artery disease varies with the nature and urgency of symptoms. Among the treatment options are drug therapy (nitroglycerin, beta blockers, and thrombolytic agents) and various surgical and nonsurgical procedures. Examples include coronary artery bypass grafting (CABG), percutaneous transluminal coronary angioplasty (PTCA), percutaneous balloon valvuloplasty, laser angioplasty, balloon-laser welding, and catheter artherectomy.
- Treatment of coronary artery disease varies with the nature and urgency of symptoms. Among the treatment options are drug therapy (nitroglycerin, beta blockers, and thrombolytic agents) and various surgical and nonsurgical procedures. Examples include coronary artery bypass grafting (CABG), percutaneous transluminal coronary angioplasty (PTCA), percutaneous balloon valvuloplasty, laser angioplasty, balloon-laser welding, and catheter artherectomy.
_________ is a condition in which the smooth muscle of a coronary artery undergoes a sudden contraction, resulting in narrowing of a blood vessel.
Coronary artery spasm
A congenital defect is a defect that exists at birth, and usually before birth. True or False
True
- PLASMA LIPIDS AND HEART DISEASE
- A strong risk factor for developing heart disease is high blood cholesterol level. The reason is that high blood cholesterol promotes growth of fatty plaques that build up in the walls of arteries.
- Most lipids are transported in the blood in combination with proteins as lipoproteins.
- Three classes of lipoproteins are called low-density lipoproteins (LDLs), high-density lipoproteins (HDLs), and very low-density lipoproteins (VLDLs).
- Whereas HDLs remove excess cholesterol from circulation, high levels of LDLs are associated with the formation of fatty plaques in arteries. VLDLs also contribute to increased fatty plaque formation.
- There are two sources of cholesterol in the body: some is present in foods we ingest, but most is synthesized by the liver.
- For adults, desirable levels of blood cholesterol are TC (total cholesterol) under 200 mg/dl, LDL 130 mg/dl, and HDL over 40 mg/dl; normally, triglycerides are in the range of 10-190 mg/dl.
- Among the therapies used to reduce blood cholesterol level are exercise, diet, and drugs.
- PLASMA LIPIDS AND HEART DISEASE
- A strong risk factor for developing heart disease is high blood cholesterol level. The reason is that high blood cholesterol promotes growth of fatty plaques that build up in the walls of arteries.
- Most lipids are transported in the blood in combination with proteins as lipoproteins.
- Three classes of lipoproteins are called low-density lipoproteins (LDLs), high-density lipoproteins (HDLs), and very low-density lipoproteins (VLDLs).
- Whereas HDLs remove excess cholesterol from circulation, high levels of LDLs are associated with the formation of fatty plaques in arteries. VLDLs also contribute to increased fatty plaque formation.
- There are two sources of cholesterol in the body: some is present in foods we ingest, but most is synthesized by the liver.
- For adults, desirable levels of blood cholesterol are TC (total cholesterol) under 200 mg/dl, LDL 130 mg/dl, and HDL over 40 mg/dl; normally, triglycerides are in the range of 10-190 mg/dl.
- Among the therapies used to reduce blood cholesterol level are exercise, diet, and drugs.
End of Chapter 20
End of Chapter 20
These are vessels that carry away blood from the heart to the tissues, what are these called?
Arteries
As the arterioles enter a tissue, they branch into countless microscopic vessels called what?
Capillaries
These vessals carry blood from the tissues back to the heart, what are these called?
Veins
These are very small, almost microscopic, arteries that deliver blood to capillaries. What are these called?
Arterioles
An alternate blood route from an anastomosis is called what?
Collateral circulation
Arteries that do not anastomose are called?
End arteries
This decreases in the size of the lumen of a blood vessel, what is this called?
Vasoconstriction
This increase in the size of the lumen of a blood vessel, what is this called?
Vasodilation
These are microscopic blood vessels through which materials are exchanged between blood and tissue cells. What are these called?
Capillaries
Capillaries usually connect what with each other?
Arterioles and Venules
Capillary walls are composed of only a single layer of cells (endothelium) and a basement membrane. True or False
True
Capillaries branch to form an extensive capillary network throughout the tissue. This network increases the surface area, allowing a rapid exchange of large quantities of materials. True or False
True
The flow of blood through capillaries is regulated by who??
By vessels with smooth muscle in their walls.
Rings of smooth muscle fibers (cells) called _________ regulate blood flow through true capillaries.
Pre-capillary sphincters
Some capillaries are continuous, whereas others are fenestrated. True or False
True
Microscopic blood vessels in organs such as the liver, spleen, and bone marrow are called _________ ;they are wider than capillaries, more tortuous, and specialized for the functions of the specific organs.
Sinusoids
These are small vessels that are formed from the union of several capillaries; venules merge to form veins. They drain blood from capillaries into veins.
What is this called?
Venules
Thses consist of the same three tunics as arteries but have a thinner tunica interna and media and a thicker tunica externa; they have less elastic tissue and smooth muscle and are therefore thinner-walled than arteries. What are these called?
Veins
-They contain valves to prevent backflow of blood.
-Weak valves can lead to varicose veins.
Vascular (venous) sinuses are veins with very thin walls with no smooth muscle to alter their diameters. Examples are the brain’s superior sagittal sinus and the coronary sinus of the heart. True or False
True
At rest, the largest portion of the blood volume is in systemic veins and venules, collectively called?
-They store blood and, through venous vasoconstriction, can move blood to other parts of the body if the need arises.
-In cases of hemorrhage, when blood pressure and volume decrease, vasoconstriction of veins in venous reservoirs helps to compensate for the blood loss.
Blood reservoirs
The principal reservoirs are the veins of the abdominal organs (liver and spleen) and skin. True or False
True
- HEMODYNAMICS: PHYSIOLOGY OF CIRCULATION
- Velocity of Blood Flow
- The volume of blood that flows through any tissue in a given period of time is blood flow.
- The velocity of blood flow is inversely related to the cross-sectional area of blood vessels; blood flows most slowly where cross-sectional area is the greatest.
- Blood flow decreases from the aorta to arteries to capillaries and increases as it returns to the heart.
- Volume of Blood Flow
- Blood flow is determined by blood pressure and resistance.
- Blood flows from regions of higher to lower pressure; the higher the resistance the lower the blood flow.
- Cardiac Output (CO) equals mean aortic blood pressure (MABP) divided by total resistance
(R): (CO = MABP / R)
- HEMODYNAMICS: PHYSIOLOGY OF CIRCULATION
- Velocity of Blood Flow
- The volume of blood that flows through any tissue in a given period of time is blood flow.
- The velocity of blood flow is inversely related to the cross-sectional area of blood vessels; blood flows most slowly where cross-sectional area is the greatest.
- Blood flow decreases from the aorta to arteries to capillaries and increases as it returns to the heart.
- Volume of Blood Flow
- Blood flow is determined by blood pressure and resistance.
- Blood flows from regions of higher to lower pressure; the higher the resistance the lower the blood flow.
- Cardiac Output (CO) equals mean aortic blood pressure (MABP) divided by total resistance
(R): (CO = MABP / R)
This is the pressure exerted on the walls of a blood vessel; in clinical use, BP refers to pressure in arteries. What is this called?
Blood pressure
Factors that affect blood pressure include?
Cardiac output, blood volume, viscosity, resistance, and elasticity of arteries.
As blood leaves the aorta and flows through systemic circulation, its pressure progressively falls to 0 mmHg by the time it reaches the right atrium. True or False
True
_________ refers to the opposition to blood flow as a result of friction between blood and the walls of the blood vessels.
Resistance
Resistance depends on what?
Blood viscosity, blood vessel length, and blood vessel radius.
This refers to all of the vascular resistances offered by systemic blood vessels; most resistance is in arterioles, capillaries, and venules due to their small diameters. What is this called?
Also known as total peripheral resistance.
Systemic vascular resistance (SVR)
The near equilibrium at the arterial and venous ends of a capillary by which fluids exit and enter is called?
Startling’s Law of the Capillaries
Occasionally, the balance of filtration and reabsorption between interstitial fluid and plasma is disrupted, allowing an abnormal increase in interstitial fluid called?
Edema
These are all factors that come from what
- Increased blood hydrostatic pressure in capillaries due to an increase in venous pressure.
- Decreased concentration of plasma proteins that lower blood colloid osmotic pressure.
- Increased permeability of capillaries, allowing greater amounts of plasma proteins to leave the blood and enter tissue fluid.
- Increased extracellular fluid volume as a result of fluid retention.
- Blockage of lymphatic vessels postoperatively or due to filarial worm infection.
- Increased blood hydrostatic pressure in capillaries due to an increase in venous pressure.
- Decreased concentration of plasma proteins that lower blood colloid osmotic pressure.
- Increased permeability of capillaries, allowing greater amounts of plasma proteins to leave the blood and enter tissue fluid.
- Increased extracellular fluid volume as a result of fluid retention.
- Blockage of lymphatic vessels postoperatively or due to filarial worm infection.
A number of factors aid ________ , the volume of blood flowing back to the heart from the systemic veins, by increasing the magnitude of the pressure gradient between the venules and the right atrium. Blood return to the heart is maintained by several factors, including skeletal muscular contractions, valves in veins (especially in the extremities), and pressure changes associated with breathing.
Venous return
Fill in the blank.
- The ____________ is a group of neurons in the medulla that regulates heart rate, contractility, and blood vessel diameter.
- The CV center receives input from higher brain regions and sensory receptors (baroreceptors and chemoreceptors).
- Output from the CV center flows along sympathetic and parasympathetic fibers.
Cardiovascular (CV) center
Output from the CV center flows along sympathetic and parasympathetic fibers. Sympathetic impulses along ____________ increase heart rate and contractility. Parasympathetic impulses from vagus (X) nerves decrease heart rate.
Cardioaccelerator nerves
Parasympathetic impulses from _________ decrease heart rate.
Vagus (X) nerves
The sympathetic division also continually sends impulses to smooth muscle in blood vessel walls via ___________. The result is a moderate state of tonic contraction or vasoconstriction, called __________.
Vasomotor nerves and V asomotor tone.
These are important pressure-sensitive sensory neurons that monitor stretching of the walls of blood vessels and the atria. What is this called?
Baroreceptors (pressoreceptors)
- The _____________ is concerned with maintaining normal blood pressure in the brain and is initiated by baroreceptors in the wall of the carotid sinus.
Cardiac sinus reflex
The cardiac sinus reflex is concerned with maintaining normal blood pressure in the brain and is initiated by baroreceptors in the wall of the carotid sinus. True or False
True
The ___________ is concerned with general systemic blood pressure and is initiated by baroreceptors in the wall of the arch of the aorta or attached to the arch.
Aortic reflex
The aortic reflex is not concerned with general systemic blood pressure and is initiated by baroreceptors in the wall of the arch of the aorta or attached to the arch. True or False
False
If blood pressure falls, the baroreceptor reflexes accelerate heart rate, increase __________, and promote vasoconstriction.
Force of contraction
The right heart (atrial) reflex responds to increases in venous blood pressure and is initiated by baroreceptors in the right atrium and venae cavae. True or False
True
The __________ responds to increases in venous blood pressure and is initiated by baroreceptors in the right atrium and venae cavae.
Right heart (atrial) reflex
Receptors sensitive to chemicals are called?
-They monitor blood levels of oxygen, carbon dioxide, and hydrogen ion concentration.
Chemoreceptors
This refers to local, automatic adjustments of blood flow in a given region to match the particular needs of the tissue. What is this called?
Autoregulation
What is the principle element not a direct stimulus for autoregulation?
Oxygen
__________, or faint, refers to a sudden, temporary loss of consciousness followed by spontaneous recovery. It is most commonly due to cerebral ischemia (lack of sufficient blood flow).
Syncope
_________ is an inadequate cardiac output that results in failure of the cardiovascular system to deliver adequate amounts of oxygen and nutrients to meet the metabolic needs of body cells. As a result, cellular membranes dysfunction, cellular metabolism is abnormal, and cellular death may eventually occur without proper treatment.
- Signs and symptoms of shock include clammy, cool, pale skin; tachycardia; weak, rapid pulse; sweating; hypotension (systemic pressure < 90 mmHg); altered mental status; decreased urinary output; thirst; and acidosis.
Shock
Stages of shock are all characterized by inadequate perfusion of tissues. True or False
True
This refers to decreased blood volume resulting from loss of blood or plasma due to acute hemorrhage or excessive fluid loss (as in excess vomiting, diarrhea, sweating, dehydration, urine production, and burns). What is this called?
Hypovolemic shock
The development of shock occurs in three principal stages, what are they?
Stage I is compensated (nonprogressive) shock
Stage II is decompensated (progressive) shock
Stage III is irreversible shock
Shock, in which negative feedback systems restore homeostasis. What stage is this called?
- If the initiating cause does not get any worse, a full recovery follows.
- Compensatory adjustments include activation of the sympathetic division of the ANS, the renin-angiotension pathway, release of antidiuretic hormone (ADH), and release of vasodilator factors in response to hypoxia.
Stage I is compensated (nonprogressive) shock
In which positive feedback cycles intensify the shock and immediate medical intervention is required. What stage is this called?
- It occurs when there has been a reduction in blood volume of 15-25%.
- Among the positive feedback cycles that contribute to decreased cardiac output and blood pressure are depression of cardiac activity, depression of vasoconstriction, increased permeability of capillaries, intravascular clotting, cellular destruction, and acidosis.
Stage II is decompensated (progressive) shock
This is rapid deterioration of the cardiovascular system that cannot be helped by compensatory mechanisms or medical intervention. What stage is this?
Stage III is irreversible shock
___________ is the alternate expansion and elastic recoil of an artery wall with each heartbeat. It may be felt in any artery that lies near the surface or over a hard tissue, and is strongest in the arteries closest to the heart; the radial artery is most commonly used to feel the pulse.
Pulse
A normal resting pulse (heart) rate is?
60 to 100 beats
Means a rapid resting heart or pulse rate (> 100 beats/min).
Tachycardia
Indicates a slow resting heart or pulse rate (< 60 beats/min).
Bradycardia
Blood pressure is the pressure exerted by blood on the wall of an artery when the left ventricle undergoes systole and then diastole. It is measured by the use of a ____________ usually in one of the brachial arteries.
Sphygmomanometer
__________ is the force of blood recorded during ventricular contraction.
Systolic blood pressure (SBP)
________ is the force of blood recorded during ventricular relaxation.
Diastolic blood pressure (DBP)
The various sounds that are heard while taking blood pressure are called?
Korotkoff sounds
The normal blood pressure of a young adult male is 120/80 mmHg (8-10 mmHg less in a young adult female). The range of average values varies with many factors. True or False
True
This is the difference between systolic and diastolic pressure. It normally is about 40 mmHg and provides information about the condition of the arteries. What is this called?
Pulse pressure (PP)
The blood vessels are organized into parallel routes that deliver blood throughout the body. True or False
True
The largest circulatory route is the?
Systemic circulation
Two of the several subdivisions of the systemic circulation are coronary (cardiac) circulation, which supplies the myocardium of the heart; the cerebral circulation, which supplies the brain; and the hepatic portal circulation, which extends from the gastrointestinal tract to the liver.
Two of the several subdivisions of the systemic circulation are coronary (cardiac) circulation, which supplies the myocardium of the heart; the cerebral circulation, which supplies the brain; and the hepatic portal circulation, which extends from the gastrointestinal tract to the liver.
Other routes include pulmonary circulation and fetal circulation.
Other routes include pulmonary circulation and fetal circulation.
The ______________ takes oxygenated blood from the left ventricle through the aorta to all parts of the body, including some lung tissue (but does not supply the air sacs of the lungs) and returns the deoxygenated blood to the right atrium.
- The aorta is divided into the ascending aorta, arch of the aorta, and the descending aorta.
- Each section gives off arteries that branch to supply the whole body.
Systemic circulation
Blood returns to the heart through the systemic veins. All the veins of the systemic circulation flow into the superior or inferior venae cavae or the coronary sinus, which in turn empty into the right atrium. True or False
True
The ___________ collects blood from the veins of the pancreas, spleen, stomach, intestines, and gallbladder and directs it into the hepatic portal vein of the liver before it returns to the heart.
Hepatic portal circulation
A ____________ carries blood between two capillary networks, in this case from capillaries of the
-This circulation enables nutrient utilization and blood detoxification by the liver.
P ortal system
The ___________ takes deoxygenated blood from the right ventricle to the air sacs of the lungs and returns oxygenated blood from the lungs to the left atrium.
-It allows blood to be oxygenated for systemic circulation.
Pulmonary circulation
The ___________ involves the exchange of materials between fetus and mother.
Fetal circulation
___________ or high blood pressure, is the most common disease affecting the heart and blood vessels. It is classified as primary (essential) or secondary.
Hypertension
________________________ (approximately 90-95% of all hypertension cases) is a persistently elevated blood pressure that cannot be attributed to any particular organic cause.
Primary (essential) hypertension
Only _____________ has causes that are identifiable. Two of these are kidney disease and adrenal hypersecretion.
Secondary hypertension
An __________ is a thin, weakened section on the wall of an artery or a vein that bulges outward, forming a balloon-like sac of the blood vessel. Left untreated, it may burst, causing massive hemorrhage with shock, severe pain, cardiovascular accident (CVA, or stroke), or death. Some may be surgically repaired.
Aneurysm
______________ is a condition in which the heart muscle receives inadequate oxygen due to blockage of its blood flow. It may be caused by atherosclerosis, coronary artery spasm, and other factors.
Coronary artery disease (CAD)
______________ is a blood clot (thrombus) in a deep vein, especially in the lower extremities. It has two serious complications: pulmonary embolism and postphlebitic syndrome.
Deep-venous thrombosis (DVT)