A critical early step in designing an EHR is to develop a (n)______________in which the characteristics of each data element are defined.
A. accreditation manual
B. core content
C. continuity of care record
D. data dictionary
D. data dictionary
Once hospital discharge abstract systems were developed and their ability to provide comparative data to hospitals was established, it became necessary to develop_______.
A. data sets
B. data elements
C. electronic data interchange
D. bills of mortality
A. data sets
In healthcare, data sets serve two purposes. The first purpose is to identify data elements to be collected about each patient. The second is to
A. provide uniform data definitions
B. guide efforts toward computerization
C. determine statistical formulas
D. provide a research database
A. provide uniform data definitions
A health information technician has been charged with the responsibility of designing a data collection form to be used on admission of a patient to the acute are hospital in which she works. The firs resource that she should use is________
A UHDDS
B. UACDS
C. MDS
D. ORYX
A UHDDS
Which of the following is NOT characteristic of the common healthcare data sets such as UHDDS and UACDS?
A. They define minimum data elements to be collected
B. They provide a complete and exhaustive list of data elements that must be collected
C. They provide a frame work for data collection to which an individual facility can add data items
D. The federal government recommends, bit does not mandate, implementation of most of the data sets
B. They provide a complete and exhaustive list of data elements that must be collected
A corporation is evaluating several health plans for its benefits package. The data set that provides comparison information about health plan performance is _____.
A. ORYX
B. HEDIS
C. UHDDS
D. MDS
B. HEDIS
The name of the government agency that has led the development of basic data sets for health records and computer databases is _____.
A. Centers for Medicare and Medicaid Services
B. Johns Hopkins University
C. American National Standards Institute
D. National Committee on Vital and Health Statistics
D. National Committee on Vital and Health Statistics
The primary purpose of a minimum data set in healthcare is to_____.
A. recommend common data elements to be collected in health records
B. mandate all data that must be contained in a health record
C. define reportable data for federally funded programs
D. standardize medical vocabulary
A. recommend common data elements to be collected in health records
The inpatient data set that has been incorporated into federal law and is required for Medicare reporting is the____
A. Ambulatory Care Data Set
B. Uniform Hospital Discharge Data Set
C. Minimum Data Set for Long term care
D. Health Plan Employer Data and Information Set
B. Uniform Hospital Discharge Data Set
Both Heidis and the Joint Commission's ORYX programs are designed to collect data to be used for
A. performance improvement programs
B. billing and claims data processing
C. developing hospital discharge abstracting system
D. developing individual care plans for residents
A. performance improvement programs
While the focus of inpatient data collection in the UHDDS is on principal diagnosis, the focus of outpatient data collection in the UACDS (Uniform Ambulatory Care Data Set) is on _______.
A. reason for admission
B. reason for encounter
C. discharge diagnosis
D. activities of daily living
B. reason for encounter
In long term care, the resident's care plan is based on data collected in the _______.
A. UHDDS
B. OASIS
C. MDS version 2.0
D. HEDIS
C. MDS version 2.0
Reimbursement for home health services is dependent on data collected from______.
A. HEDIS
B. UHDDS
C. OASIS
D. MDS Version 2.0
C. OASIS
Each of the three dimensions (personal, provider, and community) of information defined by the National Health Information INfrastructure (NHII) contains specific recommendations for________
A. government regulations
B. core data elements
C. privacy controls
D. technology requirements
B. core data elements
A core data set developed by ASTM (American Society Testing and Material) to communicate a patient's past and current health information as the patient transitions from one care setting to another is ______
A. Continuity of Care Record
B. Minimum Data Set
C. Ambulatory Care Data Set
D. Uniform Hospital Discharge Data Set
A. Continuity of Care Record
The home health prospective payment system uses the ______data set for patient assessments.
A. HEDIS
B. OASIS
C. MDS
D. UHDDS
B. OASIS
The government agency most closely involved in the development of healthcare data sets and information standards is_______.
A Centers of Medicare and Medicaid Services
B. Department of Health and Human Services
C. Johns Hopkins University
D. National Centers for Health Statistics
D. National Centers for Health Statistics
The data set designed to organize data for public release about the outcomes of care is _______.
A. UHDDS
B. DEEDS
C. MDS
D. HEDIS
D. HEDIS
OASIS data are used to assess the _______of home health services.
A. outcome
B. financial performance
C. utilization
D. core measure
A. outcome
Which of the following indexes and databases includes patient-identifiable information?
A. MEDLINE
B. Clinical trials database
C. Master patient/population index
D. UMLS
C. Master patient/population index
A notation for a diabetic patient in a physician progress note reads:
"Occasionally gets hungry. No insulin reactions. Says she is following her diabetic diet"
In which part of a POMR progress note would this notation be written?
A. Subjective
B. Objective
C. Assessment
D. Plan
A. Subjective
A notation for a diabetic patient in a physician progress note reads:
"FBS 110 mg%, urine sugar, no acetone"
In which part of a POMR progress note would this notation be written?
A. Subjective
B. Objective
C. Assessment
D. Plan
B. Objective
A notation for a hypertensive patient in a physician ambulatory care progress note reads:
"Continue with Diuril, 500 mgs once daily. Return visit in 2 weeks." In which part of a POMR progress note would this notation be written?
A. Subjective
B. Objective
C. Assessment
D. Plan
D. Plan
A notation for a hypertensive patient in a physician ambulatory care progress note reads:
"Blood pressure adequately controlled"
In which part of a POMR progress note would this notation be written?
A. Subjective
B. Objective
C. Assessment
D. Plan
C. Assessment
The set of all terms that may be used in a language is referred to as a________
A. Classification
B. Nomenclature
C. Nominal Data
D. Vocabulary
D. Vocabulary
Which of the following promotes uniform reporting and statistical data collection for medical procedures, supplies, products and services?
A. Current Procedural Terminology
B. Healthcare Common Procedure Coding System
C. International Classification of Disease, Ninth Revision, clinical Modification
D. International Classification of Diseases for Oncology, Third Edition
B. Healthcare Common Procedure Coding System
Which of the following provides a detailed classification system for coding the histology, topography and behavior of neoplasms?
A. Current Procedural Terminology
B. Healthcare Common Procedure Coding System
C International Classification of Diseases for Oncology, Third Edition
D. Systematized Nomenclature of Medicine Clinical Terminology
C International Classification of Diseases for Oncology, Third Edition
Which of the following provides a standardized vocabulary for facilitation the development of computer-based patient records?
A. Current Procedural Terminology
B. Healthcare Common Procedure Coding System
C. International Classification of Diseases, Ninth Revision, Clinical Modification
D. Systematized Nomenclature of Medicine Clinical Terminology
D. Systematized Nomenclature of Medicine Clinical Terminology
Which of the following provides a system for classifying morbidity and mortality information for statistical purposes?
A. Current Procedural Terminology
B. Diagnostic and Statistical Manual of Mental Disorders, Fourth Revision
C. Healthcare Common Procedure Coding System
D. International Classification of Diseases, Ninth Revision, Clinical Modification
D. International Classification of Diseases, Ninth Revision, Clinical Modification
Which of the following is not a knowledge source for users of the Unified Medical Language System?
A. Concept table
B. Semantic network
C. Metathesaurus
D. Specialist lexicon
A. Concept table
Nosology can be defined as the branch of medical science that deals with______.
A. cosmetic surgery
B. hospital-acquired infections
C. nursing diagnoses
D. classification systems
D. classification systems
Which of the following classifications is used exclusively for classifying cases of malignant disease?
A. CPT
B. HCPCS
C. ICD-9-CM
D. ICD-O-3
D. ICD-O-3
Which of the following provides the mot comprehensive controlled vocabulary for coding the content of a patient record?
A. CPT
B. HCPCS
C. ICD-9-CM
D. SNOMED CT
D. SNOMED CT
Which of the following provides a set of codes used for collecting data about substance abuse and mental health disorders?
A. CPT
B. DSM-IV-TR
C. HCPCS
D. SNOMED CT
B. DSM-IV-TR
Dr. Jones entered a progress note in a patient's health record 24 hours after he visited the patient. Which quality element is missing from the progress note?
A. data completeness
B. data relevancy
C. data currency
D. data precision
C. data currency
The admitting data of Mrs. Smith's health record indicated that her birth date was March 21, 1948. On the discharge summary, Mrs. Smith's birth date was recorded as July 21, 1948. Which quality element is missing from Mrs. Smith's health record?
A. data completeness
B. data consistency
C. data accessibility
D. data comprehensiveness
B. data consistency
The term used to describe expected data values is_____.
A. data definition
B. data currency
C. data precision
D. data relevancy
C. data precision
The diagnosis of a patient was recorded as an abscess in the procedure report, but was listed as carcinoma on the discharge summary. This is an example of a problem with:
A. data granularity
B. data consistency
C. data precision
D. data relevance
B. data consistency
Which of the following is a primary weakness of the paper based health record?
A. Difficult to provide availability to a number of providers at the same time
B. poor communication tool
C. difficulty in documenting healthcare processes
D. lack of available resources
A. Difficult to provide availability to a number of providers at the same time
Which of the following elements is not a component of most patient records?
A. Patient identification
B. Clinical history
C. Financial information
D. Test results
C. Financial information
Which of the following is not a characteristic of high-quality healthcare data?
A. data relevancy
B. data currency
C. data consistency
D. data accountability
D. data accountability
Which of the following represents an example of data granularity?
A. a progress note recorded at or near the time of the observation
B. An acceptable range of values defined for a clinical characteristic
C. A numerical measurement carried out to the appropriate decimal place
D. A health record that includes all of the required components
C. A numerical measurement carried out to the appropriate decimal place
Which of the following is a primary purpose of the health record?
A. document patient care delivery
B. Assist caregivers in patient care management
C. Aid in billing and reimbursement functions
D. Assist in process redesign
A. document patient care delivery
Which of the following best describes data accuracy?
A. data are correct
B. data are easy to obtain
C. data include all required elements
D. data are reliable
A. data are correct
Which of the following best describes data completeness?
A. data are correct
B. data are easy to obtain
C. data include all required elements
D. data are reliable
C. data include all required elements
Which of the following best describes data accessibility?
A. data are correct
B. data are easy to obtain
C. data include all required elements
D. data are reliable
B. data are easy to obtain
In which department/unit does the health record typically begin?
A. HIM department
B. Patient registration
C. Nursing unit
D. Billing department
B. Patient registration
Identify where the following information would be found in the acute care record:
following induction of an adequate general anesthesia, and with the patient supine on the padded table, the left upper extremity was prepped and draped in the standard fashion
A. anesthesia report
B. Physician progress notes
C. Operative report
D. Recovery room record
C. Operative report
Identify where the following information would be found in the acute care record:
CBC: WBC 12.0, RBC 4.65, HGB 14.8, HCT 43.3, MCV 93.
A. Medical laboratory report
B. Pathology report
C. Physical examination
D. Physician orders
A. Medical laboratory report
Identify where the following information would be found in the acute care record:
"PA and Lateral Chest: The lungs are clear. The heart and mediastinum are normal in size and configuration. There are minor degenerative changes of the lower thoracic spine."
A medical laboratory report
B. Physical examination
C. Physican progress note
D. Radiography report
D. Radiography report
The attending physician is responsible for which of the following types of acute care documentation?
A. consultation report
B. Discharge summary
C. Laboratory report
D. Pathology report
B. Discharge summary
A nurse is responsible for which of the following types of acute care documentation?
A. operative report
B. medication record
C. radiology report
D. therapy assessment
B. medication record
Which of the following is an example of clinical data?
A. admitting diagnosis
B. date and time of admission
C. insurance information
D. health record number
A. admitting diagnosis
Documentation of aides who assist a patient with activities of daily living, bathing, laundry and cleaning would be found in which type of specialty record?
A. Home Health
B. Behavioral health
C. End stage renal disease
D. Rehabilitative care
A. Home Health
The following is documented in an acute care record:
"HEENT: Reveals the typmpanic membranes, nares, and pharynx to be clear. No obvious head trauma.
No obvious head trauma.
In which of the following would this documentation appear?
A. History
B. Pathology report
C. Physical examination
D. Operation report
C. Physical examination
The following is documented in an acute care record:
"Microscopic: Sections are of squamous mucosa with no atypica"
In which of the following would this documentation appear?
A. History
B. Pathology report
C. Physical examination
D. Operation report
B. Pathology report
The following is documented in an acute care record: "Admit to 3C, Diet: NPO Meds: compazine 10 mg IV Q 6 PRN." In which of the following would this documentation appear?
A. Admission order
B. History
C. Physical examination
D. Progress notes
A. Admission order
The following is documented in an acute care record: "Following induction of an adequate general anesthesia, and with the patient supine on the padded table, the left upper extremity was prepped and draped in the standard fashion"
In which of the following would this documentation appear?
A. Anesthesia record
B. Discharge summary
C. Operation report
D. Progress notes
C. Operation report
The following is documented in an acute care record:
"CBC: WBC 12.0H, RBC 4.65, HGB 14.8, HCT 43.3, MCV 93."
In which of the following would this documentation appear?
A. Anesthesia report
B. Clinical laboratory report
C. Respiratory therapy report
D. Radiology report
B. Clinical laboratory report
The following is documented in an acute care record:
"38 weeks gestation, Apgars 8/9, 6# 9.8oz, good cry."
In which of the following would this documentation appear?
A. Admission note
B. Clinical laboratory
C. Newborn record
D. Physician order
C. Newborn record
The following is documented in an acute care record: "Atrial fibrillation with rapid ventricular response, left axis deviation, left bundle branch block"
In which of the following would this documentation appear?
A. admission order
B. Clinical laboratory report
C. ECG report
D. Radiology report
C. ECG report
The following is documented in an acute care record:
"I was asked to evaluate this Level I trauma patient with an open left humeral epicondylar fracture. Recommendations: Proceed with urgent surgery for debridement, irrigation, and treatment of open fracture."
In which of the following would this documentation appear?
A. Admission note
B. Consultation report
C. Discharge summary
D. Nursing progress notes
B. Consultation report
The following is documented in an acute care record:
"Spoke to the attending re: my assessment. Provided adoption and counseling information. Spoke to CPS re: referral. Case manager to meet with patient and family."
In which of the following would this documentation appear?
A. Admission note
B. Nursing note
C. Physician progress note
D. Social work note
D. Social work note
Which of the following is not usually a part of quantitative analysis review?
A. Checking that all forms contain the patient's name and health record number
B. Checking that all forms and reports are present
C. Checking that every word in the record is spelled correctly
D. Checking that reports requiring authentication have signatures
C. Checking that every word in the record is spelled correctly
Which of the following materials is not documented in an emergency care record?
A. patient's instructions at discharge
B. Time and means of the patient's arrival
C. Patient's complete medical history
D. Emergency care administered before arrival at the facility
C. Patient's complete medical history
Which of the following provides macroscopic and microscopic information about tissue removed during an operative procedure?
A. Anesthesia report
B. Laboratory report
C. Operative report
D. Pathology report
D. Pathology report
Sleeping patterns head and chest measurements, feeding and elimination status, weight and Apgar scores are recorded in which of the following records?
A. Emergency
B. New born
C. Obstetric
D. Surgical
B. New born
In a problem oriented medical record, problems are organized________
A. in alphabetical order
B. in numeric order
C. in alphabetical order by body system
D. by date of onset
B. in numeric order
What is the defining characteristic of an integrated health record format?
A. Each section of the record is maintained by the patient care department that provided the care.
B. Integrated health records are intended to be used in ambulatory settings
C. Integrated health records include both paper forms and computer printouts.
D. Integrated health record components are arranged in strict chronological order.
D. Integrated health record components are arranged in strict chronological order
Which of the following represents documentation of the patient's current and past health status?
A Physical exam
B. Medical history
C. Physician orders
D. Patient consent
B. Medical history
Which of the following contains the physician's findings based on an examination of the patient?
A. Physical exam
B. Discharge summary
C. Medical history
D. Patient instructions
A. Physical exam
What is the function of a consultation report?
A. Provides a chronological summary of the patients medical history and illness
B. Documents opinions about the patient's condition from the perspective of a physician not previously involved in the patient's care
C. Concisely summarizes the patient's treatment and stay in the hospital
D. Documents the physician's instructions to other parties involved in providing care to a patient.
B. Documents opinions about the patient's condition from the perspective of a physician not previously involved in the patient's care
What is the function of physician's orders?
A. Provides a chronological summary of the patient's medical history and illness
B. Document the patient's current and past health status
C. Document the physician's instructions to other parties involved in providing care to a patient
D. Document the providers instructions for follow up care given to the patient or patient's caregiver
C. Document the physician's instructions to other parties involved in providing care to a patient
Which type of patient care record includes documentation of a family bereavement period?
A. Hospice record
B. Home Health record
C. Long term care record
D. Ambulatory care record
A. Hospice record
Reviewing the health record for missing signatures, missing medical reports, and ensuring that all documents belong in the health record is an example of _______review.
A. Quantitative
B. Qualitative
C. Statistical
D. outcomes
A. Quantitative
Which of the following is a secondary purpose of the health record?
A. Support for provider reimbursement
B. Support for patient self management activities
C. Support for research
D. Support for patient care delivery
C. Support for research
Use of the health record by a clinician to facilitate quality patient care is considered________.
A. a primary purpose of the health record
B. patient care support
C. a secondary purpose of the health record
D. policy making and support
A. a primary purpose of the health record
Use of the health record to monitor bioterrorism activity is considered a _______.
A. primary purpose of the health record
B. secondary purpose of the health record
C. patient use of the health record
D. healthcare licensing agency function
B. secondary purpose of the health record
In designing an electronic health record, one of the best resources to use in helping to define the content of the record as well as to standardize data definitions is the E1384 standard promulgated by the ______.
A. Center for Medicare and Medicaid Services (CMS)
B. American Society for Testing and Measuring (ASTM)
C. Joint Commission
D. National Centers for Health Statistics (NCHS)
B. American Society for Testing and Measuring (ASTM)
The_____mandated the development of standards for electronic medical records.
A. Medicare and Medicaid legislation of 1965
B. Prospective Payment Act of 1983
C. Health Insurance Portability and Accountability Act (HIPAA) of 1996
D. Balanced Budget Act of 1997
C. Health Insurance Portability and Accountability Act (HIPAA) of 1996
Messaging standards for electronic data interchange in healthcare have been developed by_____.
A. HL7
B. IEE
C. The Joint Commission
D. CMS
A. HL7
A statement or guideline that directs decision making or behavior is called a _______.
A. Directive
B. Procedure
C. Policy
D. Process
C. Policy
Which of the following is the planned replacement for ICD-9-CM Volumes 1 and 2?
A. Current Procedural Terminology (CPT)
B. International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)
C. International Classification of Diseases, Tenth Revision (ICD-10)
D. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM)
D. International Classification of Diseases, Tenth Revision, Clinical Modification (ICD-10-CM)
Which organization originally published ICD-9?
A. American Medical Association (AMA)
B. Centers for Disease Control (CDC)
C. United States federal government
D. World Health Organization (WHO)
D. World Health Organization (WHO)
Which of the following organizations is responsible for updating the procedure classification of ICD-9-CM?
A. Centers for Disease Control (CDC)
B. Centers for Medicare and Medicaid Services (CMS)
C. National Center for Health Statistics (NCHS)
D. World Health Organization (WHO)
B. Centers for Medicare and Medicaid Services (CMS)
At which level of the classification system are the most specific ICD-9-CM codes found?
A. Category level
B. Section level
C. Subcategory level
D. Sub-classification level
D. Sub-classification level
What are five digit ICD-9-CM diagnosis codes referred to as ?
A. Category codes
B. Section codes
C. Subcategory codes
D. Subclassification codes
D. Subclassification codes
What are four digit ICD-9-CM diagnosis codes referred to as?
A. Category codes
B. Section codes
C. Subcategory codes
D. subclassification codes
C. Subcategory codes
Which of the following ICD-9-CM codes are always alphanumeric?
A. Category codes
B. Procedure codes
C. Subcategory codes
D. V codes
D. V codes
Which of the following ICD-9-CM codes classify environmental events and circumstances as the cause of an injury, poisoning or other adverse effect?
A. Category codes
B. E codes
C. Subcategory codes
D. V codes
B. E codes
Which volume of ICD-9-CM contains the tabular and alphabetic lists of procedures?
A. Volume 1
B. Volume 2
C. Volume 3
D. Volume 4
C. Volume 3
Which of the following provides a system for coding the clinical procedures and services provided by physicians and other clinical professionals?
A. Current Procedural Terminology (CPT)
B. Diagnostic and Statistical Manual of Mental Disorders, Fourth Revision
C. Healthcare Common Procedure Coding System
D. INternational Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM)
A. Current Procedural Terminology (CPT)
Which of the following is used to report the healthcare supplies, products, and services provided to patients by healthcare professionals?
A. CPT
B. HCPCS
C. ICD-9-CM
D. SNOMED CT
B. HCPCS
Which of the following is a standard terminology used to code medical procedures and services?
A. CPT
B. HCPCS
C. ICD-9-CM
D. SNOMED CT
A. CPT
Which of the following elements of coding quality represent the degree to which codes accurately reflect the patient's diagnoses and procedures?
A. Reliability
B. Validity
C. Completeness
D. Timeliness
B. Validity
A patient is admitted to the hospital with acute lower abdominal pain. The principal diagnosis is acute appendicitis. The patient also has a diagnosis of diabetes. The patient undergoes an appendectomy and subsequently develops to wound infections. In the DRG system, which of the following would be considered a comorbidity in this case?
A Acute appendicits
B. Appendectory
C. Diabetes
D. Wound infection
C. Diabetes
A health information technician is processing payments for hospital outpatient services to be reimbursed by Medicare for a patient who had two physician visits, underwent radiology examinations, clinical laboratory tests, and who received take home surgical dressings. Which of the following would be considered a co-morbidity in this case?
A. Clinical laboratory tests
B. Physician office visits
C. Radiology examinations
D. Take home surgical dressings
C. Radiology examinations
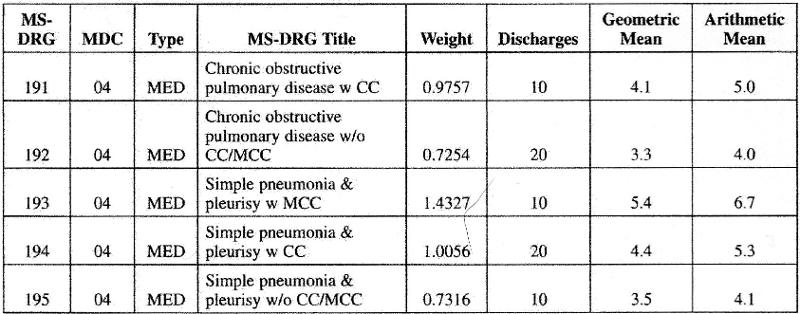
Given the information here, which of the following statements is correct?
A. In each MS-DRG the geometric mean is lower than the arithmetic mean
B In each MS-DRG the arithmetic mean is lower than the geometric mean
C. The higher the number of patients in each MS-DRG, the greater the geometric mean for that MS-DRG
D. The geometric means are lower in MS-DRGs that are associated with a CC or MCC
A. In each MS-DRG the geometric mean is lower than the arithmetic mean
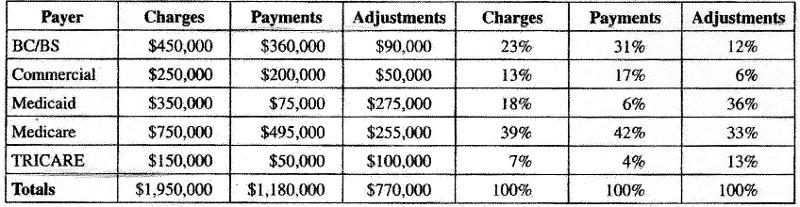
Given the following information, from which payer does the hospital proportionately receive the least amount of payment?
A. BC/BS
B. Medicaid
C. Medicare
D. TRICARE
B. Medicaid
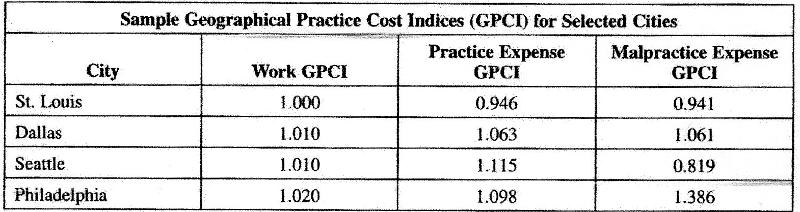
Given the following information, in which city is the GPCI the highest for practice expense?
A. St. Louis
B. Dallas
C. Seattle
D. Philadelphia
C. Seattle
skip
skip
What term is used for retrospective cash payments paid by the patient for services rendered by a provider?
A. Fee for service
B. Deductible
C. Retrospective
D. Prospective
A. Fee for service
Which of the following is the condition established after stud to be the reason for hospitalization
A. case mix
B. Complication
C. Comorbidity
D. Principal diagnosis
D. Principal diagnosis
In which of the following payment systems is the amount of payment determined before the service is delivered?
A. Fee for service
B. Per Diem
C. Prospective
D. Retrospective
C. Prospective
Which of the following is a prospective payment system implemented for payment of inpatient services?
A APC
B. DRG
C. OPPS
D. RBRVS
B. DRG
In the Inpatient Prospecitve Payment System assignment to a DRG begins with the _________.
A. Principal diagnosis
B. Primary diagnosis
C. Secondary diagnosis
D. Surgical procedure
A. Principal diagnosis
Which of the following types of hospitals are excluded from the Medicare inpatient prospective payment system?
A. Children's
B. Rural
C. State supported
D. Tertiary
A. Children's
Diagnosis-related groups are organized into______.
A. Case-mix classifications
B. Geographic practice costs indices
C. Major diagnostic categories
D. Resource-based relative values
C. Major diagnostic categories
MS-DRGs may be split into a maximum of _______payment tiers based on severity as determined by the presence of a major complication/comorbidity, a CC, or no CC.
A. Two
B. Three
C. Four
D. Five
B. Three
The purpose of the present on admission (POA) indicator is to________.
A. differentiate between conditions present on admission and conditions that develop during an inpatient admission
B. Track principal diagnoses
C. Distinguish between principal and primary diagnoses
D. determine principal diagnosis
A. differentiate between conditions present on admission and conditions that develop during an inpatient admission
The present on admission (POA) indicator is a requirement for
A. Inpatient Medicare claims submitted by all hospitals
B. Inpatient Medicare and Medicaid claims submitted by hospitals
c. Medicare claims submitted by all entities
D. Inpatient skilled nursing facility Medicare claims
A. Inpatient Medicare claims submitted by all hospitals
Which of the following is associated with the Medicare fee schedule?
A. APCs
B. MS-DRGs
C. RBRVS
D. RUG-III
C. RBRVS
To assign SNF residents to the appropriate resource utilization group data are collected using the _______.
A. MDS
B. HEDIS
C. RUG-III
D. UHDDS
A. MDS
SNFs complete MDS assessments__________.
A. on admission and once every 14 days
B. once every 30 days up to 180 days
C. according to a schedule designed for Medicare payment
D. depending on the diagnosis of the patient
C. according to a schedule designed for Medicare payment
In processing a Medicare payment for outpatient radiology exams a hospital outpatient services department would receive payment under which of the following?
A. DRGs
B. HHRGS
C. OASIS
D. OPPS
D. OPPS
Which of the following is not reimbursed according to the Medicare outpatient prospective payment system?
A. CMCH partial hospitalization services
B. Critical access hospitals
C. Hospital outpatient departments
D. Vaccines provided by CORFs
B. Critical access hospitals
Fee schedules are updated by third party payers________
A. annually
B. monthly
C. semiannually
D. weekly
A. annually
Which of the following would a health record technician use to perform the billing function for a physician's office?
A. CMS-1500
B. UB-04
C. UB-92
D. CMS 1450
A. CMS-1500
When a provider accepts assignment this means that the______.
A. patient authorizes payment to be made directly to the provider
B. provider accepts as payment in full whatever the payer reimburses
C. balance filling is allowed on patient accounts, but at a limited rate
D. participating provider receives a fee for service reimbursement
B. provider accepts as payment in full whatever the payer reimburses
A coding audit shows that an inpatient coder is using multiple codes that describe the individual components of a procedure rather than using a single code that describes all the steps of the procedure performed. Which of the following should be done in this case?
A. Require all coders to implement this practice
B. Report the practice to the OIG
C. Counsel the coder and stop the practice immediately
D. Put the coder on unpaid leave of absence
C. Counsel the coder and stop the practice immediately
A health information technician is hired as the chief compliance officer for a large group practice In evaluating the current program the HIT learns that there are written standards of conduct and policies and procedures that address specific areas of potential fraud as well as audits in place to monitor compliance. Which of the following should the compliance officer also ensure are in place?
A. Compliance program education and training programs for all employees in the organization
B. Establishment of a hotline or receive complaints and adoption of procedures to protect whistle blowers from retaliation
C. Adopt procedures to adequately identify individuals who make complaints so that appropriate follow up can be conducted
D. Establish a corporate compliance committee who report directly to the CFO
B. Establishment of a hotline or receive complaints and adoption of procedures to protect whistle blowers from retaliation
In developing a coding compliance program, which of the following would not be ordinarily included as participants in coding compliance education?
A. current coding personnel
B. Medical staff
C. Newly hired coding personnel
D. Nursing staff
D. Nursing staff
The National Correct Coding Initiative (NCCI) was developed to control improper coding leading to inappropriate payment for:
A. Part A Medicare claims
B. Par B Medicare claims
C. Medicaid claims
D. Meidcare and Medicaid claims
B. Par B Medicare claims
When the CCI editor flags that a comprehensive code and a component code are billed together for the same beneficiary on the same date of service, Medicare will pay for.
A. The component code but not the comprehensive code
B. the comprehensive but not the component code
C. The comprehensive and the component codes
D. Neither the comprehensive nor component codes
B. the comprehensive but not the component code
CCI edit files contain code pairs called mutually exclusive edits which prevent payment for________.
A. services that cannot reasonably be billed together
B. services that are components of a more comprehensive procedure
C. unnecessary procedures
D. comprehensive procedures
A. services that cannot reasonably be billed together
Which of the following issues compliance program guidance?
A. AHIMA
B. CMS
C. Federal Register
D. HHS Office of Inspector General
D. HHS Office of Inspector General
Department of Health and Human Services
The coordination of benefits transaction (COB) is important so that______.
A. there is no duplication of benefits paid
B. the hospital receives the full amount of billed services
C. the provider receives the full amount of billed services
D. the patient receives the correct bill
A. there is no duplication of benefits paid
Which of the following is a written description of an organization's formal position?
A. Hierarchy chart
B. Organizational chart
C. Policy
D. Procedure
C. Policy
Community Hospital is launching a clinical documentation improvement (CDI) initiative because currently clinical documentation does not always adequately reflect the severity of illness of the paitent and does not support optimal HIM coding quality and accuracy. Given this situation which of the following would be the best action to provide improved documentation for patient care and coding?
A. Hire clinical documentation specialists to review records prior to coding
B. Ask coders to query physicians more often
C. Provide physicians the opportunity to add addenda to their reports to clarify documentation issues
D. Conduct qualitative analyses of inpatient records while the patient is hospitalized to identify opportunities to improve the documentation in the record
D. Conduct qualitative analyses of inpatient records while the patient is hospitalized to identify opportunities to improve the documentation in the record
A coder notes that the patient is taking prescribed Haldol. The final diagnoses on the progress notes include diabetes mellitus, acute pharyngitis, and malnutrition. What condition might the coder suspect the patient has and should query the physician?
A. Insomnia
B. Hypertension
C. Mental or behavior problems
D. Rheumatoid arthritis
C. Mental or behavior problems
In conducting a qualitative analysis to ensure that documentation in the health record supports the diagnosis of the patient, what documentation would a coder look for 10 substantiate the diagnosis of aspiration pneumonia?
A. Diffuse parenchymal lung disease on x-ray
B. Patient has history of inhaled food, liquid or oil
C. Positive culture for Pneumocystis carinii
D. Positive culture for Streptococcus pneumoniae
B. Patient has history of inhaled food, liquid or oil
Aspiration pneumonia is an infection of the lungs due to the aspiration of sucking of food particles, fluid, or vomit, into the lungs.
The HIM department is planning to scan non-electronic medical record documentation. The project includes the scanning of health record documentation such as history and physicals, physician orders, operative reports, and nursing notes. Which of the following methods of scanning would be best to help HIM professionals monitor the completeness of health records during a patient's hospitalization?
A. Ad hoc
B. Concurrent
C. Retrospective
D. Post-Discharge
B. Concurrent
The HIM department is planning to scan non-electronic medical record documentation. The project includes the scanning of health record documentation such as history and physicals, physician orders, operative reports and nursing notes will be scanned. Which of the following methods of scanning would be best so that critical patient health information is available electronically at the patient's bedside or on the physician portal?
A. Ad hoc
B. Concurrent
C. Retrospective
D. Post-Discharge
B. Concurrent
The HIM department is planning to scan non-electronic medical record documentation. The project will include scanning of documents at the point of admission such as consents, drivers' license, and insurance cards. The project also includes the scanning of health record documentation such as history and physicals, physician orders, operative reports, and nursing notes will be scanned. Which of the following methods of scanning would be most efficient to make intake documents such as consents, drivers license, and insurance cards immediately available to the hospital's billing department?
A. Centralized
B. Concurrent
C. Hybrid
D. Post-discharge
B. Concurrent
The HIM department is planning to scan non electronic medical record documentation. The project will include scanning of documents at the point of admission such as consents, drivers license, and insurance cards. The project also includes the scanning of health record documentation such as history and physicals, physician orders, operative reports, and nursing notes will be scanned. Which of the following methods of scanning would be the simplest to implement?
A. Ad hoc
B. Concurrent
C. Decentralized
D. Post-discharge
D. Post-discharge
In conducting a qualitative review the clinical documentation specialist sees that the nursing staff has documented the patient's skin integrity on admission to support the presence of a stage I pressure ulcer. However, the physician's documentation is unclear as to whether this condition was present on admission. How should the clinical documentation specialist proceed?
A. Note the condition as present on admission
B. Query the physician to determine if the condition was present on admission
C. Note the condition as unknown on admission
D. Note the condition as not present on admission
B. Query the physician to determine if the condition was present on admission
When coding a hydrocystoma of the eyelid, which of the following codes should be used?
A. 216
B. 210.0
C. 215.0
D. 216.1
D. 216.1
When coding a benign neoplasm of skin of skin of the vermilion border of the lip, which of the following codes should be used?
A. 216
B. 210.0
C. 216.0
D. 216.1
B. 210.0
If a patient has an excision of a malignant lesion of the skin, the CPT code is determined by the body area from which the excision occurs and which of the following?
A. Length of the lesion as described in the pathology report
B. Dimension of the specimen submitted as described in the pathology report
C. Width times the length of the lesion as described in the operative report
D. Diameter of the lesion as well as the margins excised as described in the operative report
D. Diameter of the lesion as well as the margins excised as described in the operative report
According to CPT, a repair of a laceration that includes retention sutures would be considered what type of closure?
A. Complex
B. Intermediate
C. Not specified
D. Simple
A. Complex
The patient was admitted with nausea, vomiting and abdominal pain. The physician documents the following on the discharge summary; acute cholecystitis, nausea, vomiting, and abdominal pain. Which of the following would be the correct coding and sequencing for this case?
A. Acute cholecystitis, nausea, vomiting, abdominal pain
B. Abdominal pain, vomiting, nausea, acute cholecystitis
C. Nausea, vomiting, abdominal pain
D. Acute cholecystitis
D. Acute cholecystitis
A patient is admitted with spotting. She had been treated two weeks previously for a miscarriage with sepsis. The sepsis had resolved and she is afebrile at this time. She is treated with an aspiration dilation and curettage. Products of conception are found. Which of the following should be the principal diagnosis?
A. Miscarriage
B. Complications of spontaneous abortion with sepsis
C. Sepsis
D. Spontaneous abortion with sepsis
A. Miscarriage
An 80 year old female is admitted with fever, lethargy, hypotension, tachycardia, oliguria, and elevated WBC. The patient has more than 100,000 organisms of Escherichia coli per cc of urine. The attending physician documents "urosepsis." How should the coder proceed to code this case?
A. Code sepsis as the principal diagnosis with urinary tract infection due to E coli as secondary diagnosis
B. Code urinary tract infection with sepsis as the principal diagnosis
C. Query the physician to ask if the patient has septicemia because of the symptomatology
D. Query the physician to ask if the patient had septic shock so that this may be used as the principal diagnosis
C. Query the physician to ask if the patient has septicemia because of the symptomatology
A 65 year old patient, with a history of lung cancer, is admitted to a healthcare facility with ataxia and syncope and a fractured arm as a result of falling. The patient undergoes a closed reduction of the fracture in the emergency department and undergoes a complete workup for metastatic carcinoma of the brain. The patient is found to have metastatic carcinoma of the lung to the brain and undergoes radiation therapy to the brain. Which of the following would be the principle diagnosis in this case?
A ataxia
B. Fracture arm
C. Metastatic carcinoma of the brain
D. Carcinoma of the lung
C. Metastatic carcinoma of the brain