what are the 5 components/stages of child development, birth to 5 yrs?
- In Utero
- Premature Infant
- Newborns 0-1 year
- Babies 1-3 years
- Toddlers 3-5 years
what are the 5 components/stages of development in school-aged children, 5-18 yrs?
- Early Childhood, 5-7 years
- Mid-Late Childhood, 8-10 years
- Preadolescence, 11-14 years
- Adolescence, 15-18 years
- Transitions to Adulthood
Play is the way the child learns what no one can
teach him. It
is the way he explores and orients
himself to the actual world
Occupation in a Young Child
refers to activities that support the
health, well-being, and
development of an
individual
occupation
Occupation serves the basic needs of a __________
baby
What are the three basic levels of need in the “Baby Hierarchy of Needs”?
- Physical – Health
- Emotional – Well-being
- Cognitive – Development
What are the basic things babies do?
Eat, sleep, poop, and explore.
What do physical needs include for babies?
Eating, sleeping, and excretion.
What do emotional and cognitive needs include for babies?
Exploration and interaction with their environment.
What is one example of meeting a baby’s physical need for nutrition?
Providing healthy, age-appropriate food options.
What is one example of meeting a baby’s physical need for sleep?
Offering a crib or playpen with comforting toys to promote rest.
What is one example of meeting a baby’s physical need for movement?
Allowing indoor and outdoor exploration in safe environments.
What is one example of meeting a baby’s physical need for comfort?
Ensuring a clean, safe, and healthy living space.
What are examples of meeting babies’ physical needs? (4 things)
- Nutrition: healthy, age-appropriate food.
- Sleep: crib/playpen with comforting toys.
- Movement: indoor and outdoor exploration.
- Comfort: clean, safe, healthy environments.
What are examples of meeting babies’ emotional needs?
- Security: confidence to explore leads to autonomy.
- Bonding: feeling “heard” builds emotional stability.
- Attachments: stable relationships foster resilience and future relationships.
What helps meet a baby’s emotional need for security?
Creating confidence to explore and develop autonomy.
What helps meet a baby’s emotional need for bonding?
Ensuring the baby feels “heard” through physical touch and responsive interactions.
What helps meet a baby’s emotional need for attachment?
Providing stable, consistent relationships.
When do children typically form full attachments to parents?
Between ages 1 and 3 years.
What helps meet a baby’s cognitive need for communication?
Encouraging interaction and social participation.
- Interactions with environment
allow infants to build an understanding of oneself and
position within the world - Settings that provide stimulation and exploration, helping babies learn about themselves and their surroundings.
enriched environments
What are the 3 main cognitive needs for babies?
- Communication
- Enriched environments
- Learning
- use of tools to understand how objects relate
to each other and to the person - how objects relate to each other and to the self — foundational for problem-solving and tool use.
learning
__________________ are created as babies seek to have
their
needs met
Occupations
What are 4 examples of physical occupations in babies?
- Nutrition
- sleep
- comfort
- movement
eating, self-feeding
nutrition
physical occupations form the basis for ______________________________
Activities of Daily Living (ADLs)
rest, recuperation
sleep
dressing, bathing, toileting
comfort
interaction with the environment
movement
- Establishment of habits, routines, roles, rituals
builds trust - Routines are crucial to facilitating
emotional
security
Emotional Occupations
Meeting basic cognitive needs sets the foundation
for more
complex occupations
Cognitive Occupations
What are the 3 main cognitive occupations for babies?
- Social participation (communication)
- Play and leisure (exploration and enjoyment)
- Education and work foundations (learning and confidence)
What is the OT’s role with babies ages 1–3?
Partnering with babies and caregivers to improve occupational performance and competence in natural environments.
What are the 4 key OT concepts when working with children?
- Family-Centered Care
- Strength-Based Focus
- Cultural Competence & Humility
- Therapeutic Use of Self
What are the 5 essential concepts of OT intervention with children?
- Emphasis on a top-down approach
- Use of multiple methods
- Importance of context
- Creating the “just right challenge”
- Enabling inclusion, engagement, and participation
typical development- Knowledge of neurological,
physiological,
biological, and emotional growth can serve
as
guidelines for ________________________.
occupational performance
Children develop on fairly _______________ timelines
predictable
Progressions in development vary by many ____________________
contextual factors
What are the 4 main physical milestones at 1 year?
- Transitions between laying, sitting, standing
- Pulls up to stand, beginning to cruise
- Experimenting with standing and stepping
- Exploring, experimenting with mobility
What are 4 typical feeding milestones for a 1-year-old?
- Can hold own bottle or sippy cup
- Transitions to solids once head control and sitting balance are established
- Begins finger-feeding
- Experiments with utensils (often messy!)
Why is experimenting with utensils important?
It develops fine motor coordination and hand-to-mouth control.
What are 5 typical social/emotional skills at 1 year?
- Establishment of trust with caregivers
- Stranger anxiety appears
- Brings desired objects to caregiver to play
- Repeats sounds or actions to get attention
- Plays simple games like peek-a-boo
What does stranger anxiety indicate?
The baby can now distinguish familiar people from strangers — a healthy developmental sign.
What type of play is most common at 1 yr?
Social play with caregivers — early interactive play like peek-a-boo.
What are 6 key language & communication milestones at 1 year?
- Responds to facial expressions
- Demonstrates a social smile
- Recognizes self in mirror (self-awareness)
- Makes eye contact to observe others’ expressions
- Lifts arms to be picked up
- Says “mama” and “dada,” repeats simple words or sounds
What self-awareness behavior appears at 1 yr?
Recognizes self in a mirror.
What communication skills show at 1 year?
Responds to facial expressions and smiles socially.
at 1 yr old, what gesture shows desire for interaction?
Lifts arms to be picked up.
What words usually emerge @ 1 yr?
“Mama,” “Dada,” and repeated simple words.
1 Year – Language/Communication= observing others facial expressions
Eye contact
1 Year – Language/Communication= regarding oneself in the mirror
Self-awareness
1 Year – Language/Communication= in response to others
Social smile
What physical transitions occur at 1 year?
Moves between lying, sitting, and standing.
What new standing skill appears at 1 year?
Pulls to stand and begins cruising along furniture.
What early walking skill appears @ 1 yr?
Experiments with standing and stepping.
What physical goal drives this stage (@1 yr)?
Exploration and mobility.
What feeding milestone occurs at 1 year?
Holds own bottle or sippy cup.
When can solids be introduced @1 yr?
After head control and sitting balance develop.
What self-feeding skill appears @1 yr?
Finger-feeds independently.
What utensil skill develops @1 yr?
Experiments with spoon and cup (messy but intentional).
What social milestone forms at 1 year?
Establishes trust with caregivers
How does a 1-year-old share play?
Brings toys to caregiver.
What social action is used for attention at 1 yr?
Repeats sounds or actions.
What early game reflects social awareness?
Peek-a-boo.
What are 7 cognitive skills seen at 1 year?
- Responds to own name
- Recognizes familiar words and family names
- Imitates simple gestures
- Uses trial-and-error in problem solving
- Bangs objects together
- Points and pokes with index finger
- Demonstrates early symbolic or social play
Learning through interacting with environment
Sensorimotor stage (birth to 2 years)
Pretend play that uses objects to represent something else (e.g., pretending a block is a phone).
symbolic play
What 2 physical red flags may indicate delay/are detectable risks @ 1 year?
- Not crawling
- Cannot stand with support
What 2 social red flags may indicate delay/are detectable risks @ 1 year?
- No words or gesturing
- Limited interaction or emotional response
What 2 cognitive red flags may indicate delay/ are detectable risks @ 1 year?
- No exploration
- Does not point or show curiosity about environment
What are 2 typical reasons for OT referral at 1 year?
- Physical concerns (motor delay, tone issues)
- Feeding or eating difficulties
What physical deficits might a 1-year-old with developmental delays show? (2 things)
- Failure to develop age-appropriate motor skills
- Asymmetrical or weak movement
- Poorly controlled or abnormally toned muscles
What are signs of abnormal tone?
Too stiff (spastic) or too floppy (hypotonic) movements.
What are feeding red flags for a 1-year-old?
- Unmet nutritional needs
- Failure to progress to textured foods
- Poor oral motor control: Tongue thrust, Poor lip closure or constant drooling, Persistent gagging or choking
what are 3 examples of poor oral motor control in a 1 year old?
- Tongue thrust
- Poor lip closure, constant drooling
- Persistent gagging or choking
What are 4 common diagnoses seen at 1 year that may require OT?
- Global Developmental Delay
- Failure to Thrive (<5th percentile for height/weight)
- Epilepsy or seizure disorder
- Cerebral Palsy (CP)
- a group of permanent movement and posture disorders that result in limitations in physical activity.
- These disorders are caused by nonprogressive (not worsening over time) disturbances/damage or abnormalities in the developing fetal or infant brain, which disrupt the brain’s ability to control
- a condition where brain damage affects muscle activity, making it hard to move, control, or coordinate the body
Cerebral Palsy (CP)
Is CP progressive or nonprogressive?
Nonprogressive — the brain injury doesn’t worsen, but its effects can change over time.
What body systems does CP primarily affect?
The motor system — including movement, tone, and posture.
How common is CP?
It is the most prevalent cause of motor dysfunction in children, affecting approximately 0.14–0.21% of live births (
Which socioeconomic group shows higher prevalence of CP?
Children from lower socioeconomic backgrounds.
What are the 5 prenatal causes of CP?
- Genetic disorders
- maternal health issues
- teratogen exposure = baby exposed to something harmful during pregnancy → possible birth defects or developmental issues depending on what, when, and how much exposure happens.
- placental disruption
- fetal disruption.
A __________ is any substance or factor that can cause birth defects or developmental problems. When a pregnant person comes into contact with one, that’s called _______________________.
Common examples include:
- Certain medications (like Accutane or some anti-seizure drugs)
- Alcohol or drugs
- Infections (like rubella or Zika virus)
- Radiation or toxic chemicals
- High levels of stress or environmental pollutants
- teratogen
- teratogen exposure
What are the 3 perinatal causes of CP?
- Prematurity
- multiple births
- traumatic birth.
What are the 3 postnatal causes of CP?
- Severe jaundice
- infection
- prolonged loss of oxygen
What causes the impairment in muscle activity in CP?
Brain lesions that affect the areas controlling movement.
What causes cerebral palsy (CP)?
damage or abnormalities in the developing brain (brain lesions) that disrupt normal communication between the brain and muscles.
How do brain lesions lead to symptoms of CP?
The brain lesions impair muscle control, coordination, tone, and movement, causing difficulty with posture, balance, and motor function.
What 3 types of muscle tone abnormalities and/or movement disorders can occur in CP?
- Spasticity (85%)
- dystonia (dyskinesia) (14%)
- ataxia (<1%)
- Meaning: Muscles are stiff and tight because the brain has trouble sending signals that tell them to relax.
- What it looks like: Movements are jerky or awkward, and joints may feel hard to move.
- Cause: Damage to the motor cortex or pyramidal tracts in the brain.
spasticity
- Meaning: Muscles involuntarily contract or twist, causing repetitive or abnormal movements or postures.
- What it looks like: Movements can be slow, twisting, or sudden, and they often get worse with stress or fatigue.
- Cause: Damage to the basal ganglia, which helps control smooth, coordinated movement.
dystonia
- Meaning: Movements are unsteady, shaky, or poorly coordinated because the brain has trouble controlling balance and timing.
- What it looks like: Trouble with balance, walking, and precise movements (like reaching or writing).
- Cause: Damage to the cerebellum, which controls balance and coordination.
ataxia
What is a hallmark sign of CP in movement, another result of the brain lesions?
Inefficient, uncoordinated muscle activation patterns.
What is the average age of referral for CP evaluation?
8 months
When do most children begin therapy services for CP?
Around 12 months
When is the average age of diagnosis for CP?
16 mnths
- Meaning: Involuntary, uncontrolled, and sometimes repetitive movements that the person can’t stop or control.
- What it looks like: Movements may be writhing, twisting, jerky, or abrupt — they can affect the face, arms, legs, or trunk, and often change with posture or emotion.
- Cause: Results from damage to the basal ganglia, the part of the brain that helps control smooth and purposeful motion.
dyskinesia
In cerebral palsy, dyskinesia is known as an ___________________ type of CP — meaning the damage occurs in areas of the brain outside the main motor pathways (the extrapyramidal system) that help control automatic and smooth movements.
Because of this, children with dyskinetic CP have______________________ movements that change with posture, stress, or emotion. These movements often fall into two main patterns:
- _________________: slow, twisting, or repetitive movements that cause muscles to stay contracted for too long, sometimes leading to abnormal postures.
- ________________: quick, jerky, dance-like movements that appear random and can affect the face, arms, or legs.
- extrapyramidal
- involuntary (uncontrolled)
- Dystonia
- Chorea
People with dyskinetic CP might show a mix of both types — movements can switch between slow and rigid to fast and flinging — but they usually do not have muscle weakness; the problem lies in ______________________, not in the _________________________________.
- how movement is controlled
- strength of the muscles themselves
What are the types of CP based on body areas affected? (3)
- Diplegic (32%)
- quadriplegic (24%)
- hemiplegic (29%)
When do brain lesions that cause CP typically occur?
The damage usually happens before, during, or shortly after birth, while the brain is still developing.
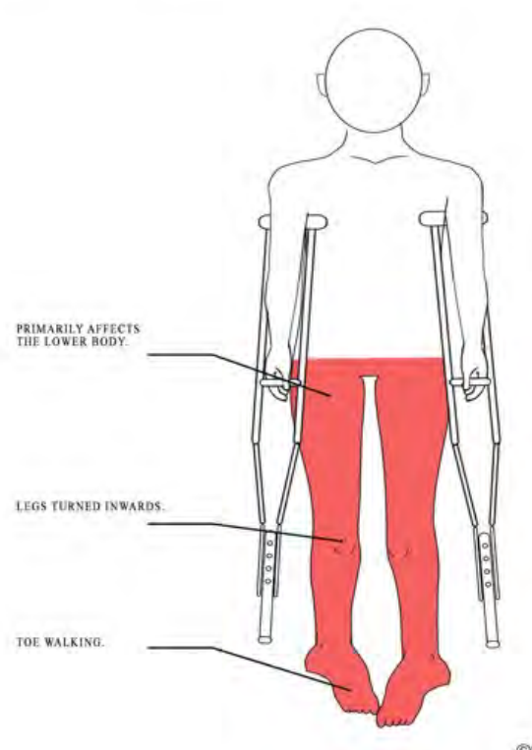
- Meaning: “_____-” means two, so this type mainly affects both legs more than the arms.
- What it looks like: Legs are stiff and tight, causing trouble walking — children may walk on their toes, cross their legs when stepping (“scissoring gait”), or have limited hip and knee movement.
- Arms: May have mild stiffness or normal movement.
- Cause: Usually due to damage in the periventricular white matter near the ventricles in the brain, which affects signals to the legs.
- Cognition: Often normal or near-normal intelligence.
di-
(spastic) diplegia/paraplegia
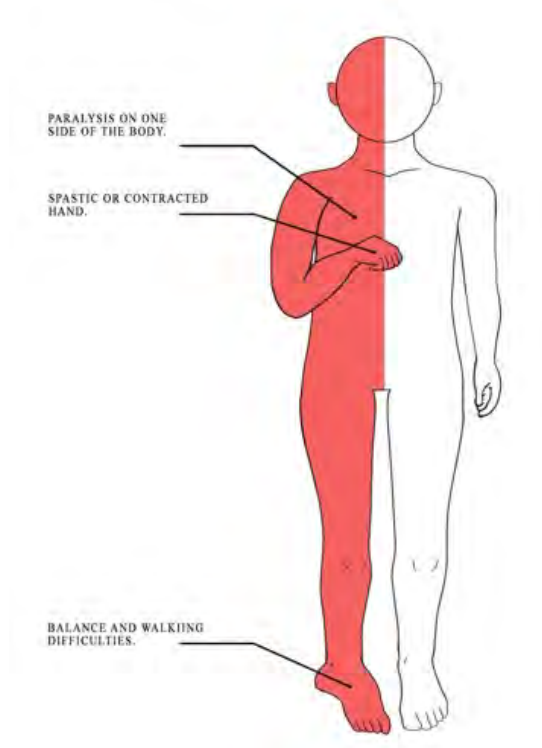
- Meaning: “________-” means one side, so this type affects one side of the body — typically the arm and leg on the same side.
- What it looks like: The arm is usually more affected than the leg. The child might hold one arm bent or fisted and walk with a limp or dragging foot.
- Cause: Often from damage to one side of the brain’s motor area, such as from a stroke before or shortly after birth.
- Cognition: Varies — many children have good cognitive abilities.
Hemi-
Spastic Hemiplegia
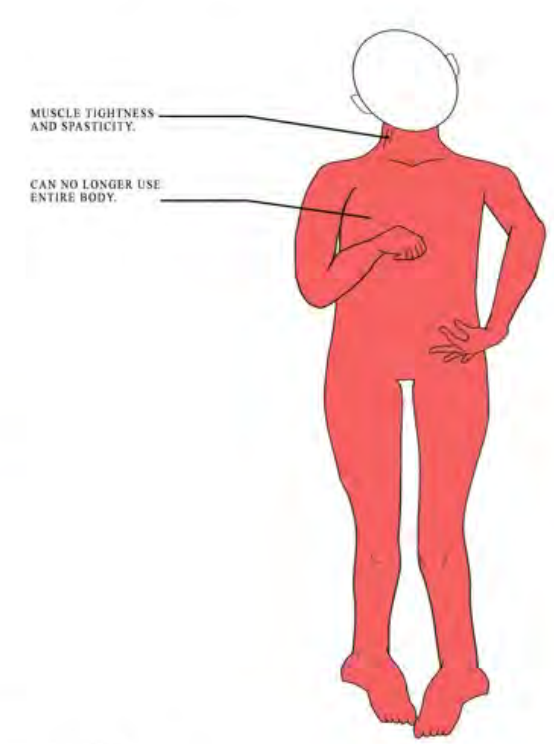
- Meaning: “_______-” means four, so this type affects all four limbs — both arms and legs — often along with the face, trunk, and oral muscles.
- What it looks like: Muscles throughout the body are very stiff, with limited control of movement. Children often have difficulty holding up their head, sitting, or walking independently.
- Cause: Results from extensive brain damage affecting both sides of the motor cortex.
- Cognition: Often more significantly affected; may have speech, feeding, and visual challenges.
Quadri
Spastic Quadriplegia
What are two major functional classification systems used for CP?
- Gross Motor Function Classification System (GMFCS)
- Manual Ability Classification System (MACS)
what does Gross Motor Function Classification System (GMFCS) measure?
Levels of gross motor function (e.g., sitting, walking, mobility).
what does Manual Ability Classification System (MACS) measure?
How children with CP handle objects in daily activities (manual dexterity).
How is CP diagnosed?
Through multiple motor assessments and neurological exams, confirmed by MRI.
What are the 3 primary OT intervention goals for babies n toddlers w/ CP?
- Improve motor function in affected limbs
- Prevent secondary impairments
- Facilitate participation in occupations through motor learning, adaptive strategies, and environmental modification
What are the five categories of Green-Light OT interventions?
- Neuromuscular Re-education
- Task-Based
- External
- Environmental:
- Caregiver:
What does “Green-Light” mean in CP interventions?
Strong research support — evidence-based and recommended OT practices.
What is the goal of Green-Light interventions?
To improve motor function, participation, and independence through effective, proven methods.
Activities that retrain the brain and muscles to work together effectively.
Neuromuscular Re-education
What Green-Light neuromuscular interventions are recommended? (2)
- Constraint-Induced Movement Therapy (CIMT)
- Bimanual Training
method of therapy where the stronger limb is restrained to encourage use of the weaker limb, promoting neuroplasticity and active movement.
Constraint-Induced Movement Therapy (CIMT)?
method of therapy that involves activities that require both hands to work together, improving coordination and bilateral integration.
Bimanual Training
Practicing meaningful daily tasks to improve real-world function and independence.
task-based intervention