Describe the different types of neurons and their functions
Neurons send messages through your body.
1. Sensory Neurons: Carry messages from the body to the brain.
Example: You touch something hot → message goes to your brain.
2. Motor Neurons: Carry messages from the brain to the body.
Example: Brain tells your hand to move away.
3. Interneurons: Found in the brain and spinal cord. They connect sensory and motor neurons.
Help with quick reactions, like reflexes.
Parts of a Neuron
- Dendrites: Catch messages.
- Cell Body: Main part of the cell.
- Axon: Sends the message away.
- Myelin Sheath: Protects the axon and makes messages go faster.
- Axon Terminals: Send messages to the next cell.
What are the supporting cells of neuron and their functions?
Supporting Cells (Help Neurons)
These cells don’t send messages. They support and protect neurons.
In the Brain & Spinal Cord (CNS):
- Astrocytes – Feed and support neurons; keep harmful stuff out of the brain.
- Oligodendrocytes – Make myelin to help messages move faster.
- Microglia – Clean up germs and damaged cells.
- Ependymal Cells – Make and move spinal fluid.
In the Rest of the Body (PNS):
- Schwann Cells – Make myelin for nerves outside the brain/spine.
- Satellite Cells – Protect and support nerve cells in groups (ganglia).
• Identify the myelin sheath and describe how it is formed in the CNS and PNS
The myelin sheath is a fatty coating around a neuron's axon.
It helps messages travel faster and protects the nerve.
In the Brain and Spinal Cord (CNS)
- Made by oligodendrocytes
- One cell can cover many axons
In the Rest of the Body (PNS)
- Made by Schwann cells
- One cell covers just one part of one axon
⚡ Why It’s Important
- Speeds up nerve signals
- Protects the axon
- Helps the body respond quickly
Think of it like rubber coating on a wire—it keeps the signal strong and fast!
• Describe the nature and significance of the blood-brain barrier.
The blood-brain barrier is a wall of protection around the brain.
What Does It Do?
- Blocks germs, poisons, and harmful stuff in the blood
- Lets in oxygen, food, and other good things the brain needs
What Is It Made Of?
- Tiny blood vessels with tight walls
- Helped by special brain cells called astrocytes
Why It’s Important
- Keeps the brain safe and healthy
- Hard for some medicines to get through, which can make treating brain problems tricky
• Explain the electrical activity associated with action potentials
an electrical signal sent along a neuron.
It’s how neurons communicate with each other and with muscles
1. Resting: Neuron is quiet.
Inside = negative, Outside = positive
2. Depolarization: Message starts
Sodium (Na⁺) rushes in → inside becomes positive
3. Repolarization: Potassium (K⁺) moves out → inside goes back to negative
4. Reset
- A pump puts Na⁺ back out and K⁺ back in
- Neuron is ready again!
Rest → Sodium in → Potassium out → Reset
It’s like flipping a light switch ON and then OFF again!
o Explain, step-by-step, how an action potential is produced.
Step 1: Resting Potential
- The neuron is not sending a signal.
- Inside of the neuron = negative
- Outside = positive
- Sodium (Na⁺) is mostly outside the cell.
- Potassium (K⁺) is mostly inside the cell.
- This state is kept by the sodium-potassium pump.
Step 2: Stimulus Reaches Threshold
- A stimulus (like a touch or signal) excites the neuron.
- If the signal is strong enough, it reaches the threshold.
- This triggers the action potential to start.
Step 3: Depolarization
- Sodium channels open
- Na⁺ ions rush in to the neuron.
- Inside becomes more positive.
Step 4: Peak of Action Potential
- Inside of the neuron is now positive.
- This is the peak of the action potential (usually around +30 mV)
Step 5: Repolarization
- Sodium channels close, potassium channels open
- K⁺ ions leave the neuron.
- Inside becomes negative again.
Step 6: Hyperpolarization
- Sometimes too much potassium leaves, making the inside extra negative for a short time.
- This is called hyperpolarization.
Step 7: Return to Resting Potential
- The sodium-potassium pump moves Na⁺ back out and K⁺ back in.
- Neuron goes back to its resting state, ready to fire again.
What features of neurons establish and maintain the resting membrane potential?
The resting membrane potential is when the neuron is
off (not sending a signal).
At rest, the
inside is negative, and the outside is positive.
3 Main Things That Keep It That Way:
1. Sodium-Potassium Pump: Pushes 3 sodium (Na⁺) out and pulls 2 potassium (K⁺) in → More positive charges go out than in
2. Leaky Potassium Channel: Potassium
slowly leaks out
→ This also makes the inside more negative
3. Negative Stuff Inside: Big negatively
charged proteins stay inside
→ They help keep the
inside negative
What causes changes in membrane potential?
The charge changes when tiny particles called ions move in or out of the cell.
Caused by:
Ion channels open (like little doors)
Sodium (Na⁺) goes in → inside gets more positive
Potassium (K⁺) goes out → inside gets more negative
What does it mean that an action potential is “all or none?”
It means the nerve either fires completely or not at all — there’s no halfway.
- If the signal is strong enough (reaches the threshold), the neuron sends a full action potential.
- If the signal is too weak, the neuron does nothing.
"All-or-none" = Full signal or no signal — never a weak or partial one.
Define the terms depolarization and repolarization and be able to illustrate graphically.
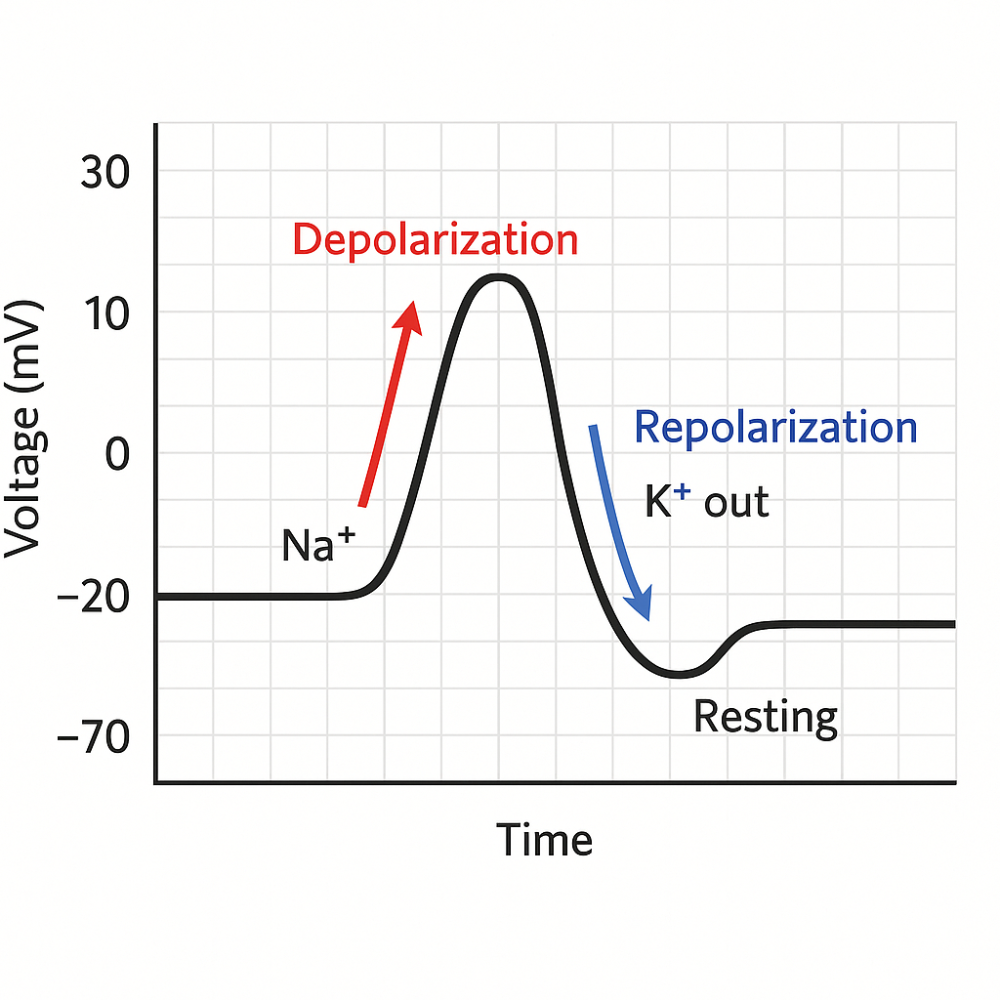
Depolarization
- The inside of the neuron becomes more positive.
- Caused by sodium (Na⁺) rushing in.
- This is how a nerve starts a signal.
Repolarization
- The neuron returns to negative inside.
- Caused by potassium (K⁺) leaving the cell.
- This resets the neuron after the signal.
- Start low (around –70 mV) → this is resting potential
- Sharp rise up → this is depolarization
- Sharp drop down → this is repolarization
- A small dip below resting → this is hyperpolarization
- Then it goes back to resting level
Describe the structure and function of electrical and chemical synapses.
Electrical Synapse: Two neurons are connected by gap junctions (tiny tunnels).
- How it works: Electrical signals go straight through from one neuron to the next.
- Fast or slow? Very fast.
- One-way or both ways? Both ways.
- Where is it found? In places needing fast and steady communication (like the heart or brainstem).
Chemical Synapse: There's a small gap between the two neurons.
- How it works: The first neuron sends out chemicals (neurotransmitters) into the gap.
- These chemicals bind to the second neuron to send the message.
- Fast or slow? Slower than electrical.
- One-way or both ways? One-way only.
- Why is it useful? Allows more control (can excite or stop signals).
Identify the nature of excitatory and inhibitory postsynaptic potentials.
Excitatory Postsynaptic Potential (EPSP): A small positive change in the postsynaptic neuron's charge.
- What it does: Brings the neuron closer to firing an action potential (a signal).
- How it happens: Usually by sodium (Na⁺) entering the cell.
- Result: Makes the inside of the neuron more positive = Depolarization.
- Think: "Excite" = more likely to fire.
Inhibitory Postsynaptic Potential (IPSP): A small negative change in the postsynaptic neuron's charge.
- What it does: Prevents or makes it harder for the neuron to fire.
- How it happens: Usually by chloride (Cl⁻) entering or potassium (K⁺) leaving.
- Result: Makes the inside of the neuron more negative = Hyperpolarization.
- Think: "Inhibit" = less likely to fire.
Describe the characteristics of action potentials
1. All-or-None Response: The neuron either fires completely or not at all.
2. Threshold: A certain level of stimulation (usually –55 mV) must be reached to trigger an action potential.
3. Depolarization: Sodium (Na⁺) channels open → Na⁺ rushes in. Inside of the neuron becomes positive.
4. Repolarization: Potassium (K⁺) channels open → K⁺ flows out. Inside becomes negative again.
5. Hyperpolarization: The neuron becomes more negative than resting (goes below –70 mV). Caused by K⁺ leaving too much.
6. Resting Membrane Potential: The neuron returns to its normal state (about –70 mV) using sodium-potassium pumps.
7. Unidirectional: Action potentials move in one direction down the axon (from cell body to axon terminal).
8. Refractory Period: Brief time when the neuron can’t fire again, or needs a stronger stimulus to do so. Ensures signals don’t go backward.
9. Self-propagating: Once started, the action potential continues along the axon without fading.
Explain how these characteristics are conducted by unmyelinated and myelinated axons.
Unmyelinated Axons
- These do not have a myelin sheath.
- The action potential moves slowly and step-by-step along the entire axon.
- Every section of the membrane must open ion channels (Na⁺ in, K⁺ out).
- Like a domino effect: each part triggers the next one.
- Key Point: Slower and uses more energy.
Myelinated Axons
- These are wrapped in a myelin sheath (fatty insulation).
- Myelin blocks ion flow, so the action potential jumps between gaps in the myelin called Nodes of Ranvier.
- This jumping is called saltatory conduction ("saltatory" means leaping).
- Much faster because the signal skips over large sections of the axon.
- Key Point: Faster, more efficient, and saves energy.
Explain how ligand-gated channels produce synaptic potentials, using nicotinic ACh receptors as an example.
They’re like locked doors on a neuron. A special key (neurotransmitter) opens them.
Example: Nicotinic ACh Receptor
1. ACh is released: A nerve sends acetylcholine (ACh) into the gap between two neurons.
2. ACh binds to the receptor: ACh is the key that opens the nicotinic receptor (a special door).
3. The channel opens: When the door opens, sodium ions (Na⁺) rush into the next neuron.
4. The inside gets more positive: This small positive change is called an EPSP (excitatory postsynaptic potential).
5. Signal might continue: If enough sodium comes in, it might start a new action potential in the next neuron.
6. ACh is broken down: An enzyme removes ACh, and the door closes again.
In Short:
- ACh opens a channel.
- Sodium comes in.
- The neuron gets excited.
- A new signal may be sent.
Explain how G-protein-coupled channels produce synaptic potentials, using the muscarinic ACh receptor as an example.
It’s a receptor that works indirectly.
It doesn’t open a channel by itself.
Instead, it activates a helper inside the cell called a G-protein.
Muscarinic ACh Receptor (Example)
1. ACh is released: Acetylcholine (ACh) is sent into the gap between two neurons.
2. ACh binds to the muscarinic receptor: The receptor is on the next neuron — this turns on a G-protein inside the cell.
3. G-protein takes action: It tells ion channels (like potassium channels) to open or close.
4. Ions move → charge changes
- If potassium (K⁺) leaves, the inside gets more negative → this is inhibitory (IPSP).
- Sometimes it can be excitatory too, depending on the G-protein.
5. Signal is slow but lasts longer: It takes more time to start, but the effect stays longer.
In Short:
- ACh binds → G-protein turns on → channels open/close → neuron changes.
- Slower than regular (nicotinic) receptors but can last longer.
Describe the action and significance of acetylcholinesterase.
⚙️ What does it do?
1. ACh sends the message from one neuron to the next.
2. Acetylcholinesterase breaks ACh into small pieces.
3. This stops the message so the neuron or muscle can rest.
4. The pieces are reused to make more ACh later.
❗ Why is it important?
- It prevents overstimulation (keeps muscles from staying tight or twitchy).
- It clears the synapse so the next signal can happen.
> Acetylcholinesterase stops the signal by breaking down ACh, so the nerve or muscle can relax.
Compare EPSPs and action potentials, identify where each is produced in a neuron
EPSP (Excitatory Postsynaptic Potential): A small, temporary increase in the neuron's charge (makes inside more positive). It helps the neuron get closer to firing.
Where it happens:
At the dendrites or cell body (soma) of the neuron — where the neuron receives signals.
Action Potential: A large, fast electrical signal that travels down the axon. It's all-or-none — once it starts, it goes all the way.
Where it starts:
- At the axon hillock (the base of the axon).
- Then it moves down the axon to the axon terminal.
Explain how action potentials can be stimulated by EPSPs.
1. EPSPs are small signals
- When a neuron receives excitatory neurotransmitters, it causes EPSPs (Excitatory Postsynaptic Potentials).
- These make the inside of the neuron more positive.
2. EPSPs add up
- One EPSP usually isn't enough to cause an action potential.
- But if many EPSPs happen close together, they can summate (add up).
- This can happen in two ways:
Temporal summation – EPSPs from the same place, quickly one after another.
Spatial summation – EPSPs from multiple places at the same time.
3. Threshold is reached
If the combined EPSPs make the membrane potential reach threshold (about –55 mV), an action potential is triggered.
4. Action potential starts
It begins at the axon hillock and travels down the axon to send the signal.
In short:
> EPSPs make the neuron more positive. If enough of them happen at once, they can reach the threshold and trigger an action potential.
Identify the monoamine neurotransmitters
These are chemical messengers made from amino acids. The main types include:
1. Dopamine (DA)
2. Norepinephrine (NE) – also called noradrenaline
3. Epinephrine (E) – also called adrenaline
4. Serotonin (5-HT)
5. Histamine
Explain how monoamine neurotransmitters are inactivated at the synapse.
Once they’ve sent their message, they must be cleared to stop the signal. This happens in two main ways:
1. Reuptake (Recycling)
- The neurotransmitter is taken back into the presynaptic neuron.
- Special proteins called transporters pull it back in.
Example: Dopamine transporter (DAT), Serotonin transporter (SERT).
Think: "Vacuuming up the neurotransmitter."
2. Enzymatic Breakdown
Enzymes break the neurotransmitter into inactive parts.
Main enzymes:
- MAO (Monoamine Oxidase) – breaks down dopamine, serotonin, NE, etc.
- COMT (Catechol-O-methyltransferase) – breaks down dopamine and NE.
Think: "Chemical scissors that cut up the message."
Describe the steps involved with release from the presynaptic neuron and reaction of the postsynaptic neuron.
In the Presynaptic Neuron (Sending Side):
1. Action potential arrives
A nerve signal (action potential) reaches the axon terminal.
2. Calcium channels open
The signal causes calcium ions (Ca²⁺) to enter the axon terminal.
3. Neurotransmitters are released
Calcium causes vesicles (tiny bubbles) filled with neurotransmitters to fuse with the membrane and release them into the synaptic cleft (gap between neurons).
In the Postsynaptic Neuron (Receiver):
4. Neurotransmitters bind to receptors: The chemicals float across the gap and attach to receptors on the next neuron.
5. Ion channels open: Receptors cause ion channels to open, letting ions in or out.
6. Neuron’s charge changes: More positive = Excitatory (EPSP) → helps start a new signal, More negative = Inhibitory (IPSP) → blocks a new signal
7. New signal may start: If enough EPSPs happen, the postsynaptic neuron will fire its own action potential.
Explain the action and significance of GABA and glycine as inhibitory neurotransmitters.
GABA (gamma-aminobutyric acid) and glycine are inhibitory neurotransmitters.
Their job is to calm down or stop nerve signals in the brain and spinal cord.
How They Work (Action)
- They bind to receptors on the postsynaptic neuron.
- This opens chloride (Cl⁻) channels (or sometimes potassium channels).
- Chloride enters or potassium leaves → inside becomes more negative.
- A more negative inside makes it harder for the neuron to fire an action potential.
This is called an inhibitory postsynaptic potential (IPSP).
Why Are They Important? (Significance)
They prevent overexcitation of the nervous system.
Help with:
Muscle control, calming anxiety, and balance between excitation and inhibition
Without them, the brain could become overactive, leading to seizures, spasms, or anxiety.
Explain the nature of spatial and temporal summation at the synapse.
Spatial and temporal summation are mechanisms by which a neuron integrates multiple synaptic inputs to determine whether it will generate an action potential.
Spatial Summation : The combined effect of simultaneous inputs from multiple synapses at different locations on the postsynaptic neuron.
How it works:
- If several presynaptic neurons fire at the same time, their excitatory postsynaptic potentials (EPSPs) or inhibitory postsynaptic potentials (IPSPs) add together.
- If the sum reaches the threshold at the axon hillock, the neuron will fire an action potential.
Ex: Neuron A, B, and C all form synapses on one neuron and fire together—this collective input may push the postsynaptic neuron past the threshold.
Temporal Summation : The summation of multiple inputs from a single synapse over time.
How it works:
- A single presynaptic neuron fires repeatedly in quick succession.
- Each EPSP/IPSP builds on the previous one before it fully decays.
- If the frequency is high enough, the potentials add up to reach the threshold.
Ex: Neuron A fires several times rapidly—each EPSP adds to the next, increasing the chance of action potential generation.
Describe the organization of autonomic motor neurons.
What is the Autonomic Nervous System (ANS)?
- It controls involuntary actions like heartbeat, digestion, breathing, and sweating.
- It sends signals from the brain or spinal cord to organs, glands, and smooth or cardiac muscles.
⚙️ How It's Organized: Two-Neuron Pathway
Autonomic motor pathways always use 2 neurons in a row:
1. Preganglionic Neuron
- Starts in the central nervous system (CNS) (brainstem or spinal cord).
- Sends its axon to a ganglion (a group of nerve cell bodies outside the CNS).
- Releases acetylcholine (ACh) to pass the signal to the next neuron.
2. Postganglionic Neuron
- Starts in the ganglion.
- Sends its axon to the target organ (heart, lungs, stomach, etc.).
Releases either: ACh (in parasympathetic system), or Norepinephrine (NE) (in sympathetic system).
Describe how neural regulation of smooth and cardiac muscles differs from neural regulation of skeletal muscles.
Skeletal Muscle
- Voluntary control
- → Controlled by the somatic nervous system (you can consciously move them).
- One motor neuron from the spinal cord directly innervates each muscle fiber.
- Neurotransmitter: Acetylcholine (ACh)
- → Binds to nicotinic receptors, causing depolarization and muscle contraction.
- Quick and precise movements.
Smooth and Cardiac Muscles
- Involuntary control
- → Controlled by the autonomic nervous system (you cannot consciously control them).
- They receive dual innervation: both sympathetic and parasympathetic neurons may influence them.
- Neurotransmitters:
Sympathetic: Norepinephrine (NE)
Parasympathetic: Acetylcholine (ACh)
→ These act on muscarinic receptors or adrenergic receptors (not nicotinic).
- Responses are slower, more modulatory, and can be excitatory or inhibitory depending on the receptor type.
- Often show spontaneous activity (e.g. pacemaker cells in the heart).
Describe the structure of the sympathetic nervous system, locating the ganglia and the preganglionic and postganglionic neurons.
The sympathetic nervous system (SNS) is part of the autonomic nervous system and is responsible for the “fight or flight” response (e.g., increased heart rate, dilated pupils, inhibited digestion).
Structure Overview
1. Preganglionic Neurons
Cell bodies are located in the lateral horns of the thoracic and upper lumbar spinal cord (T1–L2).
These neurons send out short axons that exit the spinal cord via the ventral root and then enter the sympathetic chain (also called paravertebral ganglia) through a structure called the white ramus communicans.
2. Sympathetic Ganglia
There are two main types of ganglia where pre- and postganglionic neurons synapse:
Paravertebral Ganglia
→ Also called the sympathetic chain ganglia
→ Form a chain on either side of the spinal cord
→ Connected like beads on a string
→ These ganglia run from the neck to the pelvis
Prevertebral (Collateral) Ganglia
→ Located in front of the spinal column, near major abdominal arteries (e.g., celiac, superior mesenteric, inferior mesenteric ganglia)
→ Preganglionic axons must pass through the sympathetic chain without synapsing to reach these
3. Postganglionic Neurons
- Cell bodies are in the sympathetic ganglia (either paravertebral or prevertebral).
- They send out long axons to target organs (heart, lungs, intestines, blood vessels, etc.).
- The postganglionic axons rejoin spinal nerves through the gray ramus communicans or travel independently to organs.
Path Summary (Typical Route):
1. Lateral horn of spinal cord (T1–L2)
2. Preganglionic axon exits via ventral root → white ramus
3. Enters sympathetic chain
May synapse immediately, may travel up/down chain and then synapse, or may pass through to a prevertebral ganglion
4. Postganglionic neuron sends axon to target tissue
Explain the relationship between the sympathetic nervous system and the adrenal medulla.
What is the Adrenal Medulla?
- It's the inner part of the adrenal gland (on top of your kidneys).
- It's part of the sympathetic nervous system.
How They Work Together:
1. The sympathetic nervous system sends a message to the adrenal medulla.
2. The adrenal medulla acts like a special nerve center.
3. It releases adrenaline and norepinephrine into the blood.
4. These hormones travel all over the body to help with "fight or flight" (like faster heart rate, more energy).
Sympathetic nerves → adrenal medulla → adrenaline in blood
Prepares your whole body to deal with stress quickly.
Describe the structure and innervation pathways of the parasympathetic division of the autonomic system.
The parasympathetic system controls “rest and digest” functions — like slowing the heart rate, increasing digestion, and calming the body after stress.
Where It Starts
Comes from the brainstem and the sacral part of the spinal cord (that’s why it's called craniosacral outflow)
Key Parts
1. Preganglionic Neurons
- Start in the brainstem or sacral spinal cord (S2–S4).
- These neurons are long.
- They travel to parasympathetic ganglia located near or inside the target organs.
2. Ganglia
Small clusters of nerve cells close to or inside the organs they control (e.g., heart, stomach, bladder).
3. Postganglionic Neurons
- Very short, because the ganglia are so close to the organs.
- Send signals directly to the target organs (like the eye, lungs, or intestines).
Pathways (Cranial Nerves Involved)
1. Oculomotor (III) → eyes (pupil constriction)
2. Facial (VII) → salivary and tear glands
3. Glossopharyngeal (IX) → parotid salivary gland
4. Vagus (X) → most organs in the chest and abdomen (heart, lungs, stomach, intestines)
From the sacral spinal cord (S2–S4):
Goes to the lower organs like the bladder, rectum, and reproductive organs.
Identify the neurotransmitters of the sympathetic and parasympathetic divisions, and the hormone released by the adrenal medulla.
Parasympathetic Division
Neurotransmitter (both neurons):
→ Acetylcholine (ACh)
Used by:
Preganglionic neurons
Postganglionic neurons
Acts on:
Nicotinic receptors (at ganglia) and Muscarinic receptors (on target organs)
Sympathetic Division
Preganglionic neurotransmitter:
→ Acetylcholine (ACh)
(acts on nicotinic receptors in ganglia)
Postganglionic neurotransmitter:
- → Usually norepinephrine (NE)
- (acts on adrenergic receptors on target organs)
- → Exception: ACh is used for sweat glands.
Adrenal Medulla (Sympathetic-related)
Releases hormones (not neurotransmitters) directly into the blood:
- Epinephrine (adrenaline) — majority (~80%)
- Norepinephrine (noradrenaline) — smaller amount (~20%)
Define adrenergic and cholinergic and use these terms to describe the neurotransmitters of different autonomic nerve fibers.
Cholinergic = uses acetylcholine (ACh)
Adrenergic = uses norepinephrine (NE) or epinephrine (adrenaline)
Parasympathetic Nerves
Use ACh for both steps
→ So they are cholinergic
Sympathetic Nerves
Preganglionic neurons use ACh → cholinergic
Postganglionic neurons usually use NE → adrenergic
Exception: Sweat glands use ACh → cholinergic
Adrenal Medulla
Gets ACh from a sympathetic nerve → cholinergic
Then releases epinephrine and norepinephrine into the blood → acts like adrenergic
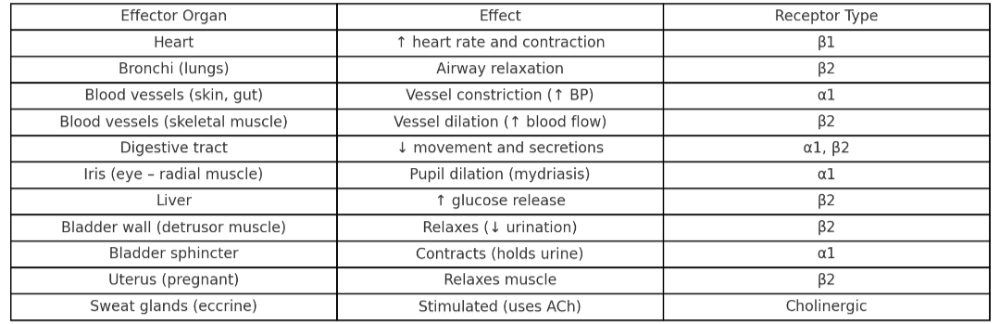
Describe the effects of adrenergic stimulation on different organs and identify the types of adrenergic receptors involved.
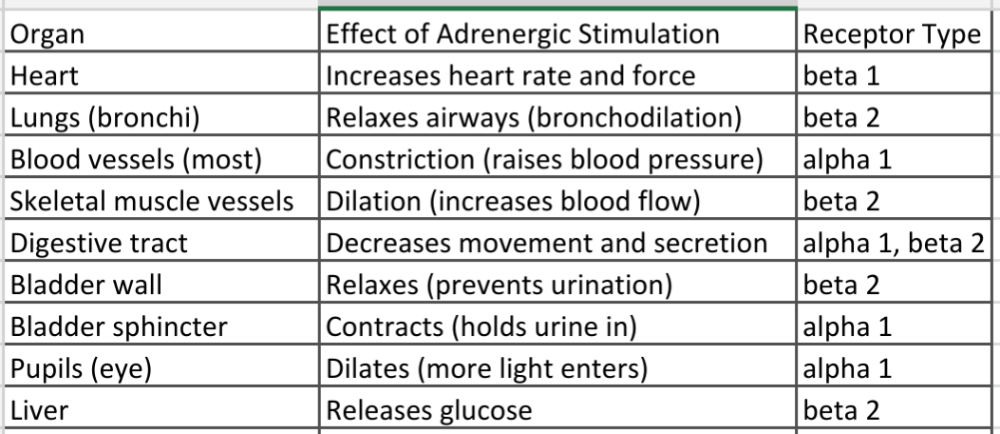
It happens when norepinephrine (NE) or epinephrine (adrenaline) bind to adrenergic receptors on organs. This is part of the sympathetic “fight or flight” response.
There are two main types of adrenergic receptors:
- Alpha (α) receptors – usually cause constriction or increase in activity
- Beta (β) receptors – usually cause relaxation or increase in heart rate/force
List the effects of sympathoadrenal stimulation on different effector organs. In each case, indicate whether the effect is due to alpha- or beta-receptor stimulation.
Describe the effects of parasympathetic nerve regulation and explain how atropine and related drugs affect this regulation.
What the Parasympathetic System Does
- It helps your body rest and digest by using the chemical acetylcholine (ACh).
- It works on muscarinic receptors in organs.
- Main effects: Slows heart rate, Helps digestion, Makes pupils smaller, Makes you pee, and Makes saliva and other fluids
What Atropine Does
- Atropine blocks the parasympathetic system.
- It stops ACh from working on muscarinic receptors.
- So it causes the opposite effects: Heart rate goes up, Pupils get big (dilated), Dry mouth (less saliva), Less digestion, and Harder to pee
Parasympathetic = chill
Atropine = blocks the chill → speeds things up
Describe and give examples of antagonistic, cooperative, and complementary actions of the sympathetic and parasympathetic divisions of the autonomic system.
1. Antagonistic = Opposite effects
The sympathetic and parasympathetic systems do the opposite things to the same organ.
Examples:
Heart: Sympathetic = speeds it up
Parasympathetic = slows it down
Pupils: Sympathetic = makes them bigger
Parasympathetic = makes them smaller
Digestion: Sympathetic = slows it down
Parasympathetic = speeds it up
2. Complementary = Help the same thing in different ways
Both systems do different jobs that work together.
Example:
Saliva: Parasympathetic = makes watery saliva
Sympathetic = makes thick, sticky saliva
Together, they help with chewing and swallowing.
3. Cooperative = Work together for one result
Both systems are needed for a full response.
Example:
Male reproduction: Parasympathetic = erection
Sympathetic = ejaculation