What is heme comprised of ?
Protoporphyrin Ring + Fe
What is Hemoglobin comprised of ?
Heme + 4 globin chains
there are many possible chains, but the common ones are alpha, beta, delta, and gamma]
What is the problem with unbound iron?
it is toxic to human tissues
What is the primary purpose of Ferritin?
it is the storage form of iron and made up of the Ferric (3+) form, which is stored in the liver
What is the definition of Porphyrins?
any of a class of pigments (including heme and chlorophyl) whose molecules contain a flat ring of four linked heterocyclic groups, sometimes with a central metal atom.
What is the definition of Porphyrias?
It is named from the ancient Greek word porphura, meaning purple. These diseases are caused by enzyme deficiencies in the heme production pathway. People generally look purple when they have this disease.

What is the definition of Hemin?
- a black inorganic compound which forms from heme when RBCs are lysed and exposed to air, Can be used as treatment for some porphyrias
What is the definition of Porphyria Cutanea Tarda ?
Deficiency of Uroporphyrinogen Decarboxylase defined by blistering (most common)
What test is used for Porphyria Cutanea Tarda?
serum porphyrin is the best test to order
What is the definition of Acute Intermittent Porphyria?
Deficiency of PBG Deaminase, defined by blistering and nerve impairments (2nd most common)
What test is used for Acute Intermittent Porphyria?
urine porphobilinogen is the best test to order
How do you diagnosis Erythropoietic Porphyria?
it must show an increase in total erythrocyte protoporphyrin
What is the definition of Erythropoietic Porphyria?
- Deficiency of ferrochelatase defined by blistering
What test is used for ALA-Dehydratase Deficiency?
the Delta-aminolevulinic acid assay
What is important to know about ALA-Dehydratase Deficiency?
it is important because it’s the rate-limiting step in porphyrin synthesis
What is the 2nd most common type of porphyria?
Acute Intermittent Porphyria (AIP) is the second most common porphyria. Patients suffer acute neurological disease and urine turns brown with exposure to light.
What does the following common secondary porphyrias do: Lead poisoning?
inhibition of most of the enzymes in the synthetic pathway
What does the following common secondary porphyrias do: Hereditary tyrosinemia ?
elevated levels of succinylacetone which inhibits Aminolevulinic Acid Dehydratase (ALAD) resulting in elevated levels of d-Aminolevulinic Acid
What does the following common secondary porphyrias do:Liver disease -
leads to a problem synthesizing heme
What does the following common secondary porphyrias do: Iron deficiency anemia -
leads to an increase in heme production, therefore more precursor substances are needed, potentially leading to a porphyria. Erythrocyte protoporphyrin is increased in these patients.
What are the expected lab values for Iron Deficiency Anemia?
Iron: Low
Transferrin: High
Transferrin Saturation: Low
Total Iron Binding Capacity: High
Ferritin: Low
What is the Porphobilinogen Methods of Analysis?
Watson-Schwartz - 4-dimethylaminobenzaldehyde (Ehrlich’s reagent) produces a red color in the presence of porphobilinogen which is detected at 555 nm spectrophotometrically.
Porphyrins are evaluated using primarily?
HPLC with fluorescent detection
note: We typically assess plasma, urine, and stool for porphyrins, using chromatographic analysis (with HPLC)
All of the samples MUST be protected from light
What is Porphobilinogen (PBG) Testing used for?
to confirm Acute Intermittent Porphyria (AIP) or to evaluate disease risk in patients with direct family members with AIP
What does Spectrofluorometric assay use?
porphobilinogen deaminase
MEMORY TRICK: Think “AIPBG”, the disease together with the diagnostic test
what is Ferrochelatase Testing used for?
screening test for Lead poisoning
How long does it take for Senescent” erythrocytes to die ?
around 120 days
note: Heme is either reused/recycled OR metabolized into bilirubin and excreted
What does Unconjugated Bilirubin =
Indirect Bilirubin
what does Conjugated bilirubin =
Direct bilirubin (hydrophilic)
What is Crigler-Najjar or Gilbert syndromes?
Increases in unconjugated bilirubin occur with hemolysis or inherited liver disease
What is Dubin-Johnson or Rotor syndromes?
Increases in conjugated bilirubin occur with biliary obstruction (tumor) or inherited liver disease
What does Delta Bilirubin =
Conjugated bilirubin covalently bound to albumin
What does Total Bilirubin =
Conjugated + Unconjugated + Delta Bilirubin
What is the common name for unconjugated bilirubin?
Indirect bilirubin
What are the serious autosomal dominant disorders?
1.Dubin-Johnson Syndrome
2.Crigler-Najjar Syndrome
What are the Weak sauce autosomal recessive disorders?
1.Rotor Syndrome
2.Gilbert Syndrome
What are the Conjugated hyperbilirubinemia disorders?
Dubin-Johnson Syndrome
Rotor Syndrome
What are the Unconjugated hyperbilirubinemia?
Crigler-Najjar Syndrome
Gilbert Syndrome
What would you expect the bilirubin levels to look like in a patient with acute cholecocholithiasis?
Indirect bilirubin high
Direct bilirubin high
What is the absorption of the Evelyn-Malloy Method?
Creates a red-purple chromogen with maximal absorption at 560 nm
What is the absorption of the Jendrassik-Grof Method?
Creates a blue chromogen with maximal absorption at 600 nm
What are the Preanalytical Concerns for Bilirubin Analysis?
A fasting sample is preferred to reduce alcohol interference
Lipemia will falsely increase the measured bilirubin
Hemolyzed samples will decrease the reaction with the diazo reagent
Bilirubin is very light sensitive and may be 50% destroyed in one hour of exposure
What are the optimal storage conditions for Bilirubin Analysis?
when the serum or plasma is separated from the cells, stored in the dark and for up to 2 days at RT, 1 week at 4˚C, and indefinitely at -20˚C.
What are the steps for Hemoglobin Electrophoresis ?
First performed on cellulose acetate using an alkaline buffer (pH 8)
Secondarily performed on an acid buffer (pH 6) to distinguish hemoglobins
note: The order of hemoglobins from slowest to fastest is C, S, F, and A
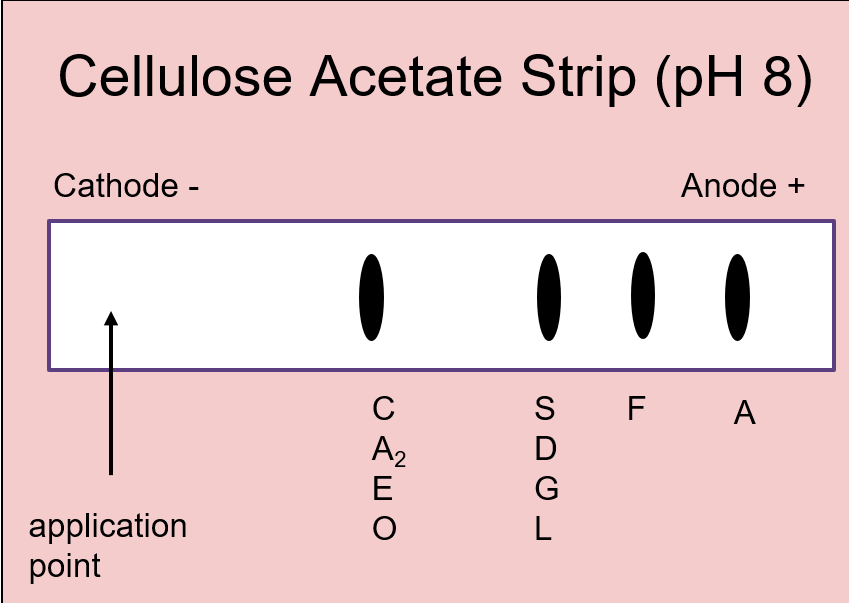
What is the purpose of Alkaline strips in hemoglobin?
to detect abnormal hemoglobin's
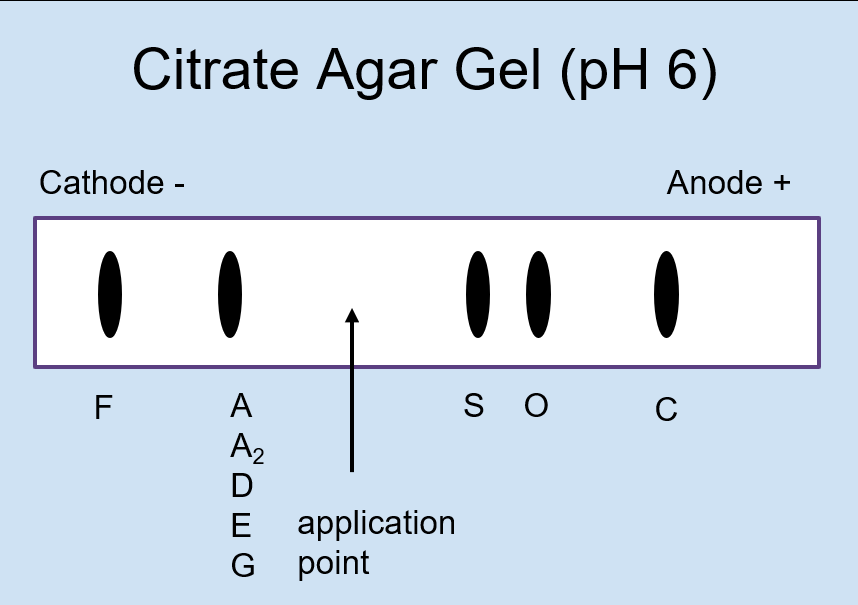
What is the purpose of Acid in hemoglobin Electrophoresis?
to differentiate abnormal hemoglobins that migrate together on alkaline hemoglobin electrophoresis
Why do hemoglobins S, D, and G migrate in the same position on an alkaline hemoglobin electrohporesis?
The side chains of the abnormally substituted amino acids in the hemoglobin react similarly at a pH of 8.4. The same goes for the group of hemoglobins C, A2, E, and O.
What is the difference between Hemoglobin E vs A2?
Hemoglobin A2 is normal but Hemoglobin E has a mutated beta-chain. To distinguish, perform capillary electrophoresis
What is the Abnormal Acquired Hemoglobin: HbA 1c?
glycated hemoglobin, used for monitoring glucose control in diabetic patients
What is the Abnormal Acquired Hemoglobin:Carboxyhemoglobin ?
- carbon monoxide binds to hemoglobin and displaces oxygen and binds with greater affinity, seen in house fires, enclosed areas near an exhaust source, etc.
What is the Abnormal Acquired Hemoglobin: Methemoglobin?
Alkaline media or oxidizing agents transform normal Fe2+ into Fe3+, conferring a inability to reversibly bind oxygen
What is the Abnormal Acquired Hemoglobin: Sulfhemoglobin ?
- Sulfation of hemoglobin causes an inability to bind oxygen
What is the Iron Spectrophotometry Method?
1.Release iron from transferrin with addition of acid
2.Reduction of Fe3+ to Fe2+ with ascorbic acid
3.React Fe2+ with a chromogen (e.g. ferrozine)
What percent of iron binds to carrier proteins?
⅔, or 66%
Iron Deficiency - Lots of transferrin, very little iron =
↑TIBC
↓Fe
Anemia of Chronic Disease - Plenty of iron, out of circulation =
↓TIBC
↓Fe
Hemochromatosis - Defective transporter cannot remove iron =
↓ TIBC
↑Fe
What is Hemoglobin H Disease?
Inadequate alpha globulin production
Produces Beta Hemoglobin tetramers
What 4 globin chains make up hemoglobin A1?
2 alpha and 2 beta
what the difference between a heme ring and a protoporphyrin IX ring is?
Think of Protoporphyrin IX as being Tony
Stark, he’s gotta
become Ironman to carry that heavy oxygen around.
What compounds serve as the negative feedback mechanism for ALA synthase?
Glucose and Heme
What is the 2nd most common form of porphyria?
Acute Intermittent Porphyria (AIP) is the 2nd most common porphyria. Patients suffer acute neurological disease and urine turns brown with exposure to light.
what if I had a patient that was producing normal hemoglobins,
but
just different amounts of them?
We call these thalassemias
If you have the following alleles what is the disease state: β/ β+ or β/ β0
β thalassemia minor (clinically silent)
If you have the following alleles what is the disease state: β+/β0 or β+/β+
β thalassemia intermedia (moderate)
If you have the following alleles what is the disease state: β0/β0
β thalassemia major (severe)
βThalassemia is most often caused by what type of mutation?
Point mutation in the β globin gene
A potential mother comes into the genetic counselor’s office asking regarding her future child’s risk for
Her child would have a 1 in 4 chance of having
A 46-year-old female presents to her physician with possible sickle
cell trait, as both of her parents were carriers. Her physician orders
a hemoglobin electrophoresis. What phenotypic results would show that
she is a carrier for sickle cell trait?
A. HbA2/S
B.
HbC/S
C. HbF/S
D. HbS/S
The correct answer is A, HbA2/S. This is correct because he would
have received one normal gene producing HbA2 and one abnormal gene
producing HbS. This genotype is considered a “carrier” of the
mutation, which may or may not significantly affect their lives. B.
HbC/S disease can be quite detrimental to the carriers of both HbC and
HbS genes. The red cells in these patients still undergo sickling
under hypoxic stress just like in sickle cell disease. HbF/S would be
a normal finding in sickle cell disease because the production of HbF
is increased in order for the body to be able to carry some
more
oxygen. HbS/S is a genotype not a phenotype. A genotype is
the genetic instructions, and a phenotype is the physical
characteristics that result from your body copying the genetic instructions.
A 2-day-old male infant is taken to his pediatrician by his mother. During a thorough history and physical, it was revealed that Hemoglobin H disease runs in the family. His current signs include a Hb of 9 g/dL and MCV of 70 fl. What hemoglobin chains constitute Hemoglobin H?
A. 2 α 2δ,
B. 2 α , 2β
C. 2 α , 2 γ
D. 4 β
The correct answer is D) 4β chains. Very few α chains are produced in α -thalassemia with 3 out of 4 α -globin chains defective (HbH disease) and no α chains are produced when all 4 chains are defective, and is incompatible with life (hydrops fetalis). Because there are not enough α chains to bind, the β chains just go ahead and form tetramers which are called HbH. A) is the normal variant HbA2 , B) is the normal HbA, and C) is HbF.
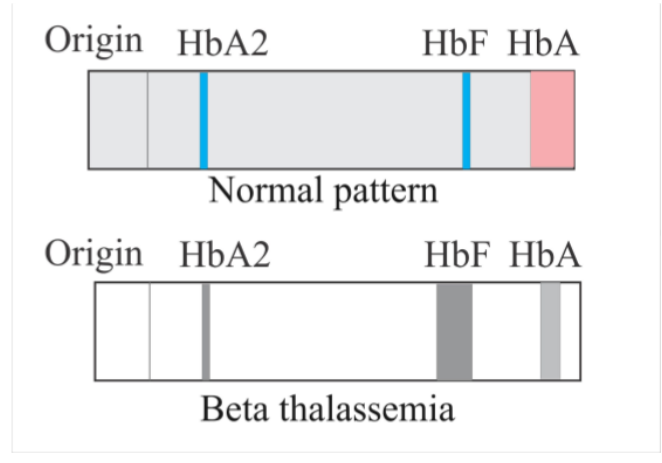
A 43-year-old female with β-thalassemia intermedia presents to her primary care physician for management of her disease. A hemoglobin electrophoresis is ordered. How would β-thalassemia affect the HbF and HbA bands on the electrophoresis?
The correct answer is B) Decreased HbA and Increased HbF. Let’s dive
into why. Normally, we have a lot of HbA, a little HbA2 and adults
have very little HbF. These hemoglobins are made up of different
hemoglobin chains. HbA is made up of 2α chains and 2β chains and HbF
is made up of 2α chains and 2γ chains. In β-thalassemia, the
β
globin gene is defective, so all that can be produced are
adequate levels of α, γ, δ, and other globin chains. Therefore,
because HbA cannot be made in adequate amounts to carry all the oxygen
that the body needs, other globin chains are made to attempt to
increase the oxygen carrying capacity. These other chains may be
present in higher amounts to make up for the lack of the β globins and
to create more hemoglobin. This is why the HbF concentration increases
in β-thalassemia, because the β-gene cannot be made in adequate
amounts, the γ chains are produced in an attempt to make up the
difference and bring the patient to a normal oxygen-carrying
capacity.. This explains the increase in HbF and the decrease in
HbA.
Check the electrophoretic patterns below for a visual representation
What should you associate “coproporphyrinogen III” with?
heme synthesis
What hemoglobins should you know?
HbA, HbA2 ,HbS, and HbF. Remember that HbA2 crawls with HbC.
What is the Enzyme Deficiency for:PBG Synthgase (AKA ALA Dehydratase)
ALA Dehydratase
Deficiency
What is the Enzyme Deficiency for: Uroporphobiliogen III Cosynthase
Congenital Erythropoietic Porphyria
What is the Enzyme Deficiency for: Uroporphobilinogen Decarboxylase
Porphyria Cutanea Tarda
What is the Enzyme Deficiency for: Ferrochelatase
Erythropoietic porphyria