Define ED50
The dose of a medication which will have the intended effect for 50% of the population
Define TD50
The dose which will cause toxic symptoms in 50% of the population
Define LD50
The dose which is lethal in 50% of the population
What is used to metabolize toxicants that our bodies can't get rid of?
Cytochrome P450 Oxidase enzymes (CYP450)
How do CYP450 enzymes work?
Phase I - Oxidizing or reducing a compound
Phase II -
Inactivation of a compound by adding a functional group to it
Define Vd
Volume of distribution, tells how widely the substance is spread throughout your body
Define elimination constant
How much of a substance you get rid of in a specific amount of time
Define Half-life
How long it takes for the plasma concentration to decrease by half
Define qualitative testing
The test gives you a result which is positive or negative
Define quantitative testing
The test gives you a numerical value as a result
Why does CO cause shortness of breath and death?
Because it displaces oxygen on our hemoglobin and holds on tightly so that we can no longer transport oxygen in our blood
What is the treatment for CO poisoning?
100% oxygen
What are common symptoms of carbon monoxide poisoning?
Red face, headache, shortness of breath
Where does cyanide have it's primary pathologic effect on the body?
The heart and the brain
What life-sustaining process does cyanide interrupt?
Oxidative phosphorylation (i.e. the ability for oxygen to accept electrons in the electron transport chain). Results in tissue death, seizures, and coma.
What source can provide arsenic and cyanide exposure?
Open flames in an enclosed space
What factors will affect drug absorption?
So many. Primarily gastrointestinal motility, acidity of the drug, gastric acidity,
Describe peak drug assessment
This is when a drug is measured after 1-4 hours and is considered to be completely absorbed, reaching it's peak concentration
Describe trough drug assessment
this is when a drug is measured immediately prior to the next dose, at theoretically the lowest concentration
Define First order elimination
A constant percentage of substance is eliminated over time
Define zero order elimination
A constant amount of substance is eliminated over time
Name a commonly-abused substance with zero-order elimination
alcohol
How many doses of a drug does it take to reach a stable steady state concentration?
5
What is a steady state?
When the drug intake equals drug excretion
Define pharmacodynamics
What the drug does to the body
Define pharmacokinetics
What the body does to the drug
What are the common side effects for excess Digoxin levels?
Nausea, vomiting, cardiac arrhythmias
note: is a cardiac glycoside used to improve cardiac contraction in patients with congestive heart failure. Side effects of increased concentrations (>3 ng/mL) include nausea, vomiting, premature ventricular contractions (PVCs), and atrioventricular node blockade.
What are the common side effects for excess Quinidine levels?
Nausea, vomiting, tinnitus, thrombocytopenia, and cardiac arrhythmias
note :is a drug used to treat cardiac arrhythmias. It is generally administered as a slowly-absorbed oral pill. Trough levels are assessed. Toxicity begins at twice the upper limit of the therapeutic range. Side effects include nausea, vomiting, tinnitus, thrombocytopenia, and PVCs.
What are the two commonly assessed cardiac drugs for TDM?
Digoxin and Quinidine
What are the two commonly assessed antibiotic drugs for TDM?
Aminoglycosides and Vancomycin
What are the common side effects for excess Aminoglycoside levels?
Nephrotoxicity and Ototoxicity
note:are a group of antibiotics used to treat
gram-negative bacterial infections.
Big toxicities to remember
with these are Nephrotoxicity and Ototoxicity; kidney and hearing.
What are the common side effects for excess Vancomycin levels?
Nephrotoxicity, otoxicity, and Red Man Syndrome
note: is at the pinnacle of antibiotics and one of the kingpins that we use to treat the “untreatable” infections. It is administered intravenously and can cause “red man syndrome” (erythema or the whole body), Nephrotoxicity, and Ototoxicity. Same as the aminoglycosides, but just add that it causes the cool red man syndrome thing and you’re good.
What are the common side effects for excess Phenytoin levels?
Hirsuitism, gingival hyperplasia, vitamin D deficiency, folate deficiency
note: is an anti-seizure, Anti-Epileptics, drug and used in brain injury to prevent further loss of functional tissue. Seizures can occur in sub-therapeutic or supratherapeutic doses. Other side effects include hirsutism (become a hairy man beast like bigfoot), gingival hyperplasia, vitamin D deficiency, and folate deficiency.
What are the common side effects for excess Carbamazepine levels?
Rashes, nausea, vertigo, and a deadly leukopenia
note: is an effective anti-seizure drug, but is only used in refractory cases that do not respond to other antiepileptic drugs. Side effects can include rashes, nausea, vertigo, and the most serious is the deadly leukopenia.
What are the common side effects for excess Ethosuximide levels?
Used for absence seizures Causes nausea, vomiting, anorexia, dizziness, lethargy
note: is used for controlling petit mal seizures.
These are the seizures that don’t
cause wild flailing but the
patient stares blankly not moving, and are also called absence
seizures. This drug has the standard litany of side effects for most
drugs; nausea, vomiting, anorexia, dizziness, lethargy. You would be
safe to bet that most oral drugs cause these symptoms, so they’re not
really special like some of the others I’ve outlined.
What are the three anti-epileptic drugs commonly assessed for TDM?
Phenytoin, Carbamaepine, and Ethosuximide
What are the three antidepressant drugs commonly assessed for TDM?
Lithium, Tricyclic antidepressants, and clozapine
What are the common side effects for excess Lithium levels?
Anemia, renal impairment, apathy, lethargy, hypothyroidism, seizures
note: is a common mood-altering medication used for bipolar disorder. Lithium has a half-life of 10-35 hours and has a narrow therapeutic index, meaning that side effects present just above the effective concentration. These include apathy, lethargy, renal impairment, hypothyroidism, and seizures.
What are the common side effects for excess Tricyclic antidepressant (TCAs) levels?
Seizures, arrhythmias, and loss of consciousness
note: are used to treat depression, and the most pertinent ones are imipramine, amitriptyline, and doxepin. TCAs hang out in the body a VERY long time; half-life of 17-40 hours. Side effects include seizures, arrhythmias, and loss of consciousness.
What are the common side effects for excess Clozapine levels?
Seizures
note: is a drug used in refractory schizophrenia as an antipsychotic. Excess dosing can result in seizures.
What are the common side effects for excess Cyclosporine and tacrolimus levels?
renal dysfunction
note:is an immunosuppressive agent used to prevent host-versus-graft
rejection.
Half-life is approximately 12 hours, and toxicity
results in renal dysfunction
note: is another oral immunosuppressive agent but it is 100 times more potent . Although it is still effective at lower concentrations, It's toxicity still results in renal dysfunction
What are the common side effects for excess methotrexate (MTX) levels?
inhibits DNA synthesis in all cells
note: This works well for cancer, because those cells are rapidly dividing and they will take more MTX and suffer more. The peak concentrations are measured 1 hour after the dose is given orally. Side effects will include a cytotoxic effect to most cells in the body. We have a procedure to halt the MTX effect on our cells called leucovorin rescue, where we basically infuse the patient with folic acid which effectively stops the deadly action of MTX on our cells.
What is the procedure to halt methotrexate's effect on our healthy cells when we give it to patients with cancer?
leukovorin rescue
What are the three Immunosuppressant drugs commonly assessed for TDM?
Cyclosporine, tacrolimus, methotrexate
What is a bronchodilator that is commonly assessed for TDM?
Theophylline
What are the symptoms of Theophylline toxicity?
Seizures
note: is an older drug, but shows up with high frequency on standardized exams. It is used to dilate the bronchial passages to alleviate respiratory problems, but can cause seizures. Since the advent of inhaled glucocorticoids, It is rarely used anymore.
Two 60 kg patients are given 1 gram of different drugs and after 1 hour, the serum concentration of Drug A is 10 mg/dL and Drug B is 20 ug/mL. What drug has a greater volume of distribution?
Drug B is the correct answer. This problem actually has two
challenges to be overcome, the first is units, the second is Vd .
Let’s get everything to the same units first.10 mg/dL = 0.1 g/L 20
ug/mL = 0.02 g/L The Vd for Drug A is 1 g (administered drug) / 0.1
g/L (plasma concentration) = 10 L The Vd
for Drug B is 1 g / 0.02
g/L = 50 L. This means that more of Drug B is distributed throughout
the lipid-rich regions of the body and is not found in the aqueous
plasma. The Volume of Distribution throughout the body is greater and
will hang out longer
A 45-year-old female is status-post left hemicolectomy (excision of her colon from the splenic flexure to the cecum). She is given morphine for the pain, which will further decrease her gastrointestinal motility, how will her GI motility affect the absorption of drugs into her body?
The decrease in GI motility will increase the absorption of morphine into her bloodstream.
How many doses of a drug does it take to reach a stable steady-state
concentration?
5, isn’t this interesting that it takes 5 half-lives for a drug to effectively be eliminated from the body and it takes 5 dosages to reach a stable steady-state concentration. This is assuming that the patient took all 5 doses at the proper times though, which may or may not happen.
Grandpa’s cough medicine was too strong for grandpa, but mom socked back a few glasses to cure her cough. It didn’t really cure her cough, but she had a blood alcohol content of 0.15%, above the legal limit in Utah. How would the liquor be eliminated from mom’s body?
Zero order elimination. It would be eliminated at a constant rate of 0.01 g ETOH / 100 mL blood / 1 hour in a person who has not chronically abused alcohol and developed a tolerance to it. In patients who develop an alcohol tolerance, this rate can increase to as fast as 0.06 g ETOH / 100 mL blood/ 1 hour ... that’s a 6-fold increase! Holy Batman!
A 68-year-old male with chronic renal failure has a GFR of 12 mL/min.
How will
this affect the levels of his Digoxin dose?
The decrease in GFR will lead to a decrease in the elimination of the drug. His serum Digoxin levels should stay between 0.8 - 2 ng/mL in the serum. Higher levels will predispose him to some fairly daunting cardiac problems, including premature ventricular contractions and AV node blockages.
What two drugs will cause nephrotoxicity and ototoxicity?
Aminoglycosides and Vancomycin
Laura, an 18-year-old female who is a non-drinker was tricked at a party and told that she was being given a “virgin” daiquiri. While everyone else is laughing and snickering, Laura asks for another one and ends up passing out. Why was she so affected by the alcohol when others at the party had way more than two drinks?
The answer comes from the metabolism of alcohol. She only had the action of alcohol dehydrogenase to metabolize the liquor. The CYP450 enzymes in the liver can be induced, which were likely present in higher quantities in her friends who probably drink often. She will likely have a hangover in the morning as well, and will probably choose new friends after the glorious experience of repeatedly puking after she wakes up.
What do steroid hormones do to affect cellular function?
Steroids bind to intranuclear receptors and cause transcription of DNA into RNA. This allows for proteins to be made from the RNA via translation. Because steroids start a cellular process inside the nucleus, they do NOT have immediate activity
What metabolite of cocaine do you screen for with an immunoassay?
Benzoylecgonine
An immunoassay is positive codeine for an 18-year-old young man. He says that he had been taking oxycodone prescribed by his physician. Is this possible?
Theoretically, yes because oxycodone and codeine do cross react in the screening immunoassay, just at very low rates. The likelihood of this scenario being true is NOT high. He most likely just found, bought, or somehow procured codeine pills, but it probably was NOT oxycodone that caused a positive immunoassay for codeine.
Acetaminophen (Tylenol) doesn’t kill you immediately, it depletes what substance in your liver that scavenges for reactive oxygen species?
Glutathione, this substance generally takes care of all free
radicals
floating around in your body, unless of course, it is
trying to keep your liver safe from certain death by trying as hard as
it can to deal with the reactive oxygen species given off by Tylenol
metabolism. I’m sure it’s kind of like the Battle for Middle Earth in
Lord of the Rings. Your liver is faced with scores upon scores of a
deadly opponent, and your small band of glutathione is all that’s
there to protect it from certain destruction.
What is the toxic substance produced by Tylenol metabolism in the liver?
N-acetyl-p-benzoquinoneimine
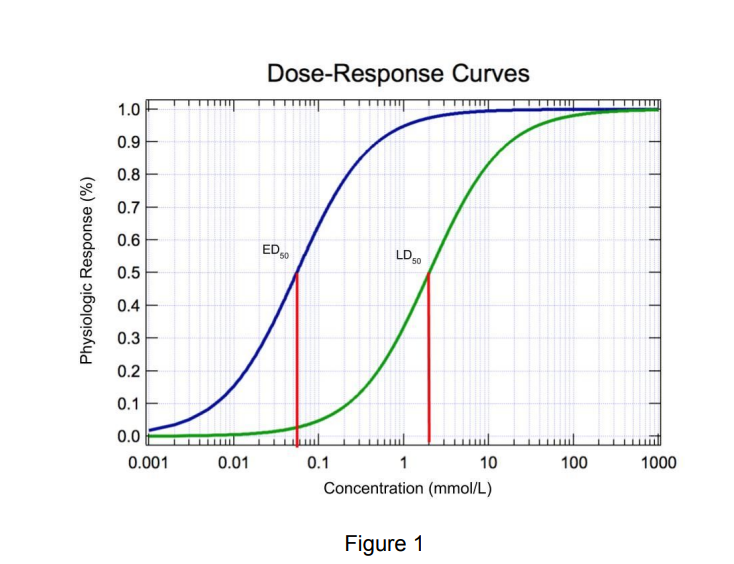
Where does the Toxic dose fit into the dose response curves?
The toxic dose curve fits between the effective dose curve and the lethal dose curve which makes sense because you would expect to feel sick from a substance before you die from your exposure to it. That’s not always the case,nbut a good rule of thumb.
A lipophilic drug like Theophylline has a very high Vd . What would a CYP450 enzyme do to improve excretion?
CYP450 enzymes would likely conjugate the drug to an ion to make it water soluble and readily excreted in the urine.
Your cousin Ed is driving drunk, and the cop pulls him over and gives him a breathalyzer test. Is this a quantitative or qualitative test?
Quantitative, because it gives you a number! 0.08% is drunk driving in Utah! An easy way to tell if the test is a quantitative test is that you’ll get a number whereas you will get either a (+) or a (-) on a qualitative test. Think breathalyzer for quantitative and pregnancy test for qualitative.
You have a 48-year-old white male who lives alone in the Rocky
Mountains presents to the ER after the largest snowstorm that the
region has seen in over 30 years. His face is very red, and many
people think that he looks like Santa with his rosy cheeks. He has
been complaining of a very bad headache for the past few days. Upon
questioning, he reveals that in order to keep warm, he is
using a
propane heater in his living room. What is the most likely cause of
this patient’s symptoms?
CO poisoning is the most likely cause of this patient’s headache and red complexion. This is commonly seen in patients with old propane heaters in poorly-ventilated areas of their home. Some people also get CO poisoning by running their car engine in their garage with the garage door closed. If there is a flame source with inadequate ventilation, CO could be the cause.
How does carbon monoxide displace oxygen from hemoglobin?
CO binds hemoglobin 200 times stronger than oxygen does. The
CO
concentration doesn’t have to overwhelm the concentration of
Oxygen to displace it on hemoglobin. The only chance that Oxygen has
to overcome the effects of CO is to be inhaled in nearly 100%
concentration so that the CO can diffuse off the hemoglobin and be
breathed out in the lungs
A 34-year-old female presents to the ER with generalized weakness, headache, and abdominal pain. Without asking for her history, big mistake, the physician just goes ahead and orders a blood cyanide level. What are the possible sources of exposure for this poison?
The cause of this patient’s symptoms would likely become clear upon
collecting a quick history from the patient. Intentional poisoning for
suicide is occasionally seen, however smoke inhalation is by far the
most common cause for harmful cyanide exposure. Workers in the metal
trades (especially electroplating), mining, jewelry making,
photography, and agriculture can have significant
industrial
cyanide exposures. Ingestion of food that contains
cyanide is rare. The drug nitroprusside, used to dilate blood vessels,
can produce toxic levels of cyanide in the body