What is the full medical breakdown for: 40-year-old Female with a history of valvular heart disease presents for a physical. She has been feeling tired recently and can't exercise. Her prosthetic valve is beginning to malfunction
Test: Serum BUN/Creatinine
Sample: Plasma or Serum (preferably transported separated from the erythrocytes)
Method: Quantitative Spectrophotometry
Result: BUN 84 mg/dL Creatinine 1.8 mg/dL Reference
Range
(Ratio 10-20)
Disease or Condition: Valvular Regurgitation (Prerenal Azotemia)
What is the full medical breakdown for:72-year-old Male
who
rarely seeks medical help has not been able to urinate
regularly for
the past 5 months. He has been feeling more tired
than normal. He
feels like he needs to pee, but he just can't
Test: Serum BUN/Creatinine
Sample: Plasma or Serum (preferably transported separated from the erythrocytes)
Method: Quantitative Spectrophotometry
Result: BUN 57 mg/dL Creatinine 5.8 mg/dL Reference
Range
(Ratio 10-20)
Disease or Condition: Transitional Cell Carcinoma of the Bladder (Postrenal Azotemia)
What is the full medical breakdown for: 28-year-old Female with
a
history of lupus, presents feeling sluggish, with dry, coarse
hair and skin. She has gained 30 pounds over the past 6 months and has
had "the flu" for about 2 weeks
Test: Serum Protein Electrophoresis
Sample: Serum
Method: Quantitative Capillary Electrophoresis
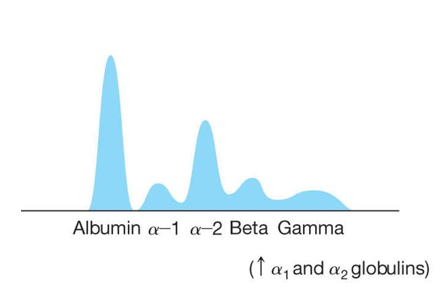
Result: Elevated a1 and a2 bands
Disease or Condition: Acute Phase Reaction
What is the full medical breakdown for: 47-year-old Male with
a
recent history of a massive liver fluke infection presents
with
a protuberant abdomen and spider angiomata around the navel.
Test: Serum Albumin
Sample: Serum
Method: Quantitative Spectrophotometry
Result: 2.8 g/dL Reference Range (3.5-5.0 g/dL)
Disease or Condition: Cirrhosis after a Fasciola hepatica infection
What is the full medical breakdown for: 53-year-old Male
presents
to his physician after partaking in Oktoberfest, where
he consumed 4
Liters of Beer and ate three Schnitzel sandwiches
and a delicate Rouladen. Today, his big toe is red and painful.
Test: Synovial Fluid Uric Acid
Sample: Synovial Fluid from a joint aspirate
Method: Quantitative Spectrophotometry
Result: 7.2 mg/dL Reference Range (No Reference Range in Synovial fluid)
Disease or Condition: Gout
What is the full medical breakdown for: 6-year-old girl is
being
actively treated with induction chemotherapy for her
Burkitt Lymphoma. She presents 72 hours after her last chemo
appointment with profuse vomiting, hypocalcemia, and hyperkalemia
Test: Serum Uric Acid
Sample: Serum
Method: Quantitative Spectrophotometry
Result: 9.3 mg/dL Reference Range (2.5-6.1 mg/dL)
Disease or Condition: Tumor Lysis Syndrome
A 3-day old baby boy is brought in by his parents for his newborn screening. The physician takes a whiff and says that this child smells “mousy”. What disease does this child likely have based on the smell?
If you see the phrase “mousy odor” on the registry exam, they
are
likely referring to PKU.
What is the cure for PKU?
A phenylalanine-restricted diet, rich in grains, fruits, and vegetables, and low in meats, eggs, cheese, and milk.
What enzyme is deficient in tyrosinemia type I?
Fumarylacetoacetate hydrolase
What is the tell-tale sign that a patient has alkaptonuria?
Dark brown or black urine
What are the three branched chain amino acids?
Leucine, Isoleucine, and Valine
If your cousin from Qatar, has a downward dislocation of the lens in his eye, what disease do you think that he could have?
Homocystinuria
What is the deficient enzyme found in cystinuria?
None. Remember, it is caused by a deficient transporter protein which allows for cystine reabsorption by the kidney.
An 11-year-old female presents to her pediatrician with the CBS
mutation, and she was properly screened with the Guthrie test. She is
being adequately treated with vitamin B6 . She comes in complaining
that she can’t see well out of one eye. This started suddenly this
morning. What is the most likely clinical effect?
A. Downward
dislocation of the lens
B. Lower right quadrant abdominal
pain
C. Mumps
D. Ovarian hyperstimulation
The correct answer is A) This fact is the most likely to be tested
clinical nuance that will give the answer away every time. It’s just
screaming at you that this patient has homocystinuria. The most common
mutation is the CBS gene, screened with the Guthrie test using
L-methionine sulfoximine to inhibit bacterial growth, but the
increased level of methionine in the sample will still allow for the
bugs to grow. If you have growth on a Guthrie test, that is positive!
The treatment of vitamin B6
.
A pregnant mother is admitted to the hospital to deliver her first baby. Upon delivery, the doctors take a few samples for newborn testing for rare diseases that are easily treatable. This baby has an increased level of branched chain amino acids in her blood. What is the name of this rare metabolic deficiency?
A. Alkaptonuria
B. Cystinuria
C. Maple
Syrup Urine Disease
D. Tyrosinemia
The correct answer is C) The hallmark of this disease is that there is an elevated level of branched chain amino acids, which are leucine, isoleucine, and valine. The deficient enzyme is BCKD. Treatment is a BCAA-restricted diet.
A 35-year-old male immigrant from Ghana is found mumbling to himself
on the streets of San Francisco. It is discovered that he is married
to a Ghanaian woman with two kids, and he lives in Boston. He doesn’t
know how he got to San Francisco. He has no health records here in
America, but after talking to his wife on the phone, the physician
discovers that they moved here 1 year ago because her husband was able
to land a job here. Before they moved, they were
vegetarians
because they couldn’t afford meat. Now, she says that her husband has
found the joy of chili dogs, and has at least two each day. He is
noted to have a musty smell. What is the most likely disease in this case?
A. Alkaptonuria
B. Cystinuria
C. Homocystinuria
D. Phenylketonuria
The correct answer is D) This man was likely never screened in Ghana, but was inadvertently adhering to a phenylalanine-restricted diet by eating only vegetarian food. This all changed once he and his family were introduced to the wonders of American table trash and had the means to procure it. PKU is the most common inherited aminoacidopathy in America, occuring about 1 in 15,000 births (He is an immigrant, so this statistic wouldn’t apply to him). The deficient enzyme is phenylalanine hydroxylase and the gene is PAH. Screening for PKU now occurs across the country equally. Screening is performed by a Guthrie test using
A 49-year-old female has nonalcoholic steatohepatitis and a very reduced capacity to synthesize proteins. What clinical issues would you expect?
Ascites and edema. This is a case where the synthetic capacity of
the
liver has been compromised, so we would expect to see a low
plasma albumin level in this patient. Since she has a decreased
protein level in her blood, the plasma colloidal osmotic pressure
(oncotic pressure) is also decreased. The compartments of the body
(e.g. the abdomen) attempt to keep adequate protein levels for
cellular functioning. Therefore, the oncotic pressure surrounding the
tissues and in the abdomen is relatively greater than the plasma
oncotic pressure. This causes water to be sucked in between the
tissues causing edema and swelling. Also remember the peritoneum? That
is a cavity, which also retains proteins. If a patient has decreased
serum oncotic pressure, the will get abdominal swelling and the
peritoneal cavity will fill up
with fluid, which we call ascites.
No bueno
What structures of a protein will be affected by Alanine Aminotransferase (ALT), with the addition of an alanine?
Short answer is it depends. The longer answer is that it depends on where the alanine is added. If it is added to the end of the polypeptide chain, then it would change the primary structure, which would likely affect the secondary, tertiary, and quaternary structures. If the alanine is added to an amino acid side chain, then it will likely affect tertiary and quaternary structures
What is the protein assay method principle and use for: Kjeldahl
Principle: Protein digestion assay, measures released Nitrogen
Use: Reference method
What is the protein assay method principle and use for: Biuret
Principle: Cu 2+ and peptide bonds create a purple color
Use: Routine method; performed in an alkaline medium
What is the protein assay method principle and use for: Dye Binding
Principle: Dye binds to the protein which causes a shift in the absorbance of the dye
Use: Used for research
What are the two classifications of testing that are performed to assess protein in a serum sample?
BUN and Serum Total Protein
A 35-year-old patient is found to have a diet deficient in Tyrosine. What metabolic deficits will likely present?
None! It is considered a nonessential amino acid and can be synthesized from phenylalanine. Of note, It is an amino acid which is richly used in adrenal medullary hormones (e.g. epinephrine, norepinephrine, dopamine) and thyroid hormone. All of hormones that stimulate activity in the body.
A 21-year-old nonalcoholic female presents to their physician with vague abdominal pain and difficulty breathing. She is diagnosed with cirrhosis and emphysema. What is the likely enzyme deficiency that she is suffering from?
α1-antitrypsin
A 35-year-old female presents to her physician after a long,
strenuous hike through the mountains. She has low blood pressure and
is diagnosed with mild dehydration. Protein concentration would be
increased. What is the routine method for protein identification and
quantification?
A. Kjeldahl method
B. Biuret method
C.
Dye-Binding method
D. Serum protein electrophoresis
The correct answer is B) Remember, this method is the routine one that it is used in everyday laboratory testing. This uses Cu 2+ , which binds to peptide bonds and creates a purple color. The color change is measured at 540 nm.
A 19-year-old male cocaine abuser has just injected himself with a
double hit of cocaine. His heart starts to race and he is sweating
while sitting still. He begins breathing quickly and feels great! His
friends, who were against him shooting up in the first place, notice
that he has become too agitated and hyperthermic so they take him to
the hospital where initial laboratory tests show a significant
metabolic acidosis and pH of 7.2. What level of protein structure
would
NOT be denatured?
A. Primary structure
B. Secondary
structure
C. Tertiary structure
D. Quaternary structure
The correct answer is A) This is the only structure that would likely NOT be denatured. B) is formed by weak bonds and would likely be the first to disintegrate. One could argue that C) would also likely NOT be denatured because they are covalently-bonded side chains. What I wanted to get you to understand is that the Primary structure is the hardest one to break down. D) would likely be different because if the secondary structure is changed, then the proteins would likely NOT fit as well as they are supposed to.
A 48-year-old male presents to the ED complaining of vague abdominal
pain and he can’t stop the bleeding from minor cuts. He has also been
feeling numbness and tingling in his arms
for about the last
month. His astute physician performs a quick eye exam and observes
Kaiser-Fleischer Rings which indicate Copper deposition. What band
would be increased on a Serum Protein
Electrophoresis?
A.α 1
B.α 2
C. β
D.γ
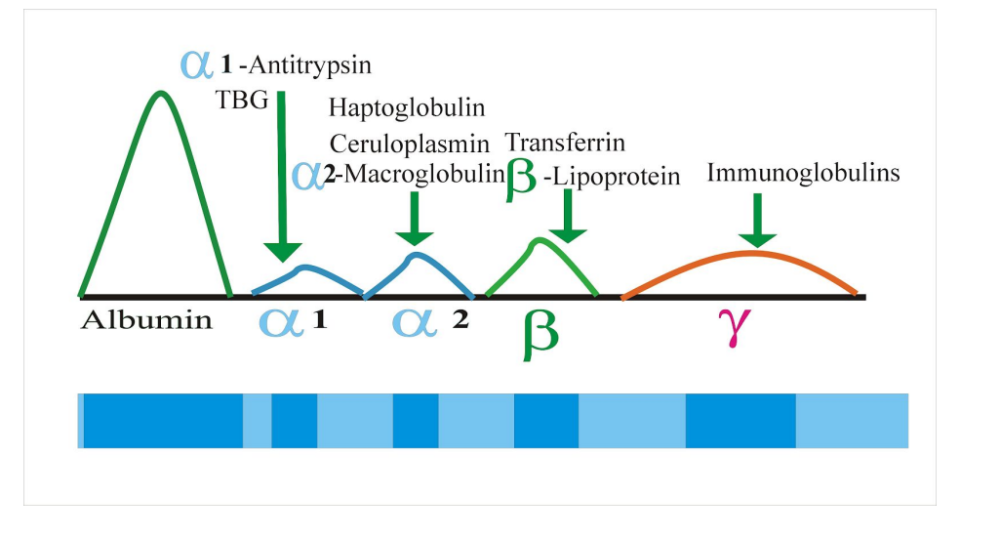
The correct answer is A) It would be increased because of the presence of Ceruloplasmin, the copper transport protein. This patient likely has Wilson’s disease, a genetic defect in the body’s ability to metabolize copper, causing it to be deposited everywhere. This results in cirrhosis and occasionally neurologic effects as we
What is uric acid created from?
DNA degradation, adenine and guanine
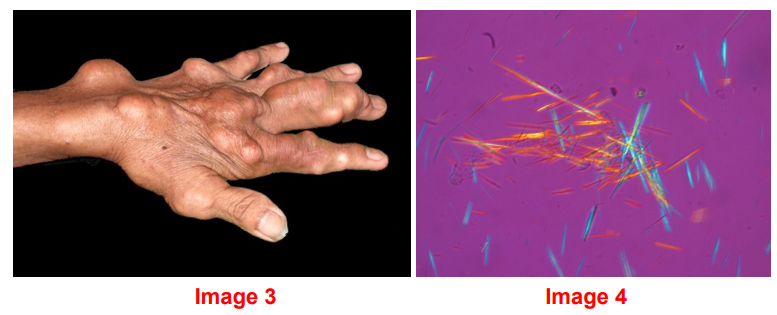
A 54-year-old male presents with severe flank pain and a tophus on his right foot (see image 3). What stereotypical finding would you see under the microscope?
Negatively birefringent crystals. This means that if you’re looking
with
a light filter, the needles that are pointing in one
direction will refract blue light, and the needles that point 90˚ from
that refract yellow light. Quick memory trick: If needles which are
ParaLLel to the filter are yeLLow, it’s Gout! In image 4, The filter
would be pointed in a horizontal plane the horizontal crystals are
yellow, that means this is Gout. Notice that the vertical crystals are blue.
A patient with Acute Lymphoblastic Leukemia is being treated with the chemotherapeutic agent 6-mercaptopurine which stops purine synthesis. What effect will this have on the patient’s plasma uric acid level?
The patient will likely have hypouricemia
0.6 - 1.1 mg/dL
What sample should be received if the ordering physician desires ammonia testing on his patient?
An EDTA or Heparin tube on ice. The plasma should be immediately separated from the red cells and assayed or stored
What is the substance that causes neuronal destruction in hepatic
encephalopathy?
Ammonia (NH3)
A 47-year-old female gardener, has had to stop wearing gloves because
her hands don’t fit or move around comfortably in them. She has
noticed that when she lies in bed at night, sometimes the weight of
just the bedsheet is unbearable on her great toe. Physical
examination, reveals a red, swollen right metatarsophalangeal joint
and tophaceous deposits on her ears. What non-protein nitrogen would
you expect to see elevated in this case?
A. Ammonia
B.
Creatinine
C. Urea
D. Uric Acid
the correct answer is D) This patient has gout and the podagra described (gouty tophi over the metatarsophalangeal joint), is typical of gouty arthritis. Even the weight of a bedsheet, can send these patients off the edge.
A 53-year-old male presents to the ED after eating a delicious meal at a steakhouse and downing 4 beers. He has exquisite joint pain and can’t seem to move. His left foot hurts the worst. When the doctor asks him to rate his pain out of 10, he immediately yells 14! The patient also said that his left elbow and right wrist are both at 11. His physician is worried about diet-induced gout and decides to order a plasma uric acid level. What tube is NOT acceptable if we are using the uricase method to evaluate the uric acid concentration?
A. EDTA
B. Li Heparin
C. Na
Heparin
D. Red Top Tube
The correct answer is A) It binds to Ca2+ and chelates it, making it unavailable for assaying, but also unavailable for protein function. Ca 2+ is used as a cofactor for a bunch of enzymes that are involved in protein and uric acid degradation. Different labs require different samples. Some just say that they need plasma or serum from any tube.
A 32-year-old male presents to his primary care physician because his
previously drawn ammonia level came back very elevated. He just got
over having a severe gastroenteritis where he had many bacteria
proliferating in his intestines. These bacteria broke down his
body’s
proteins and increased his serum ammonia levels. Now that
he is over his infection, he thought this value would go down. What is
NOT a factor which will affect the ammonia level in this patient’s
sample?
A. Diphenhydramine (Benadryl)
B. Drinking
alcohol
C. Hemolysis
D. Smoking cigarettes
The correct answer is B) The point of this question is to help
you
recognize that numerous drugs will affect ammonia levels, and
specifically smoking cigarettes even a few hours before the sample is
taken, can drastically increase the ammonia value reported. Red cells
contain two to three times the levels of ammonia inside of them, so
when you have hemolysis and spill out the red cell all over the
place,
then you will falsely increase the ammonia result.
Remember, to be accurate, these samples MUST be collected on ice and
ran immediately
When preparing the Jaffe reagent, what must you be cautious of?
Picric acid is explosive, even crust that forms on the cap can
ignite
when the cap is turned
What is the approximate reference range for creatinine in most labs across the country?
0.6 - 1.1 mg/dL
How do you calculate the amount of creatinine that a patient has effectively eliminated from their blood in 24 hours?
We have a few
equations to be able to do this:
Creatinine Clearance
equation CrCl = (UCr x VUr ) /
(SCr x 1,440 min/24 hours)
UCr =
Urine Creatinine
SCr = Serum
Creatinine
VUr =
volume of urine in 24 hours
The next one to know would be the equation for estimated GFR or the Cockroft-Gault Formula GFR = [(140-Age) x weight (kg)] / [72 x SCr]
What is the creatinine clearance if 72-year-old 60 kg male had a serum creatinine of 5.3 mg/dL?
10.7 mL/min. This man is in severe renal failure and is probably in line for his weekly dialysis appointment, or at least he should be.
The next one to know would be the equation for estimated GFR or the Cockroft-Gault Formula GFR = [(140-Age) x weight (kg)] / [72 x SCr]
How do we calculate the BUN concentration from a urea concentration?
Divide the urea concentration by 2.14. This is easy to remember which one is bigger because urea is the large molecule, and BUN stands for Blood Urea Nitrogen, so it’s obviously just looking for nitrogen. If you want to calculate the urea concentration, then you multiply BUN by 2.14.
What is the likely etiology of a patient’s renal failure with a BUN of 70 mg/dL, and Creatinine of 1.5
BUN:Cr ratio = 46. This is indicative of a prerenal etiology. The most common being something to cause a decreased amount of blood to flow through the kidneys. This would include dehydration, shock, congestive heart failure, or anything else the leads to a decrease in circulating blood volume
A 72-year-old male has a heart attack and is recovering slowly in the hospital. Two hours after the embolus is removed from his left anterior descending coronary artery, he has flank pain and the physicians are worried about renal damage from hypoperfusion of the kidney. What values would you expect to see if the patient had a prerenal azotemia?
A. BUN >80 mg/dL
B. Cr >8.2
mg/dL
C. BUN/Cr ratio >40
D. Cystatin C >0.6 mg/dL
The correct answer is C). This would be a definitive laboratory finding of prerenal azotemia. If the ratio is >20, then that’s just suggestive, but over 40 is definitive. The reason why this happens is because Creatinine is much more dependent on the glomerular filtration rate, rather than kidney function. As long as the kidneys are being perfused at 50% capacity, the creatinine value doesn’t increase. Prerenalazotemia can be caused by renal hypoperfusion; which can be caused by dehydration, renal vasoconstriction, or a myocardial infarction. This causes activation of the renin-angiotensin-aldosterone system, antidiuretic hormone, and sympathetic nerve signals to increase reabsorption of water, salt, BUN, and creatinine so that the kidney can be adequately perfused. BUN is reabsorbed at a MUCH greater rate than creatinine, thereby causing the drastic increase in BUN. A) Bun >80 mg/dL can occur in this clinical situation, but the big point is that the creatinine would be normal or slightly elevated, making answer A. the most correct. B) Cr >8.2 mg/dL would show up in chronic, renal failure. These patients are possibly dialysis dependent. D) Cystatin C is an analyte which is completely filtered by the glomeruli and is constantly produced by all nucleated cells. It is NOT secreted in the PCT, but it does have some clinical situations which confound analysis … just like creatinine
A 53-year-old male triathlete is complaining of always having a full bladder. He can’t quite seem to urinate very easily. It takes him approximately 2-3 minutes before he can get a stream of urine. He is diagnosed with benign prostatic hypertrophy by a digital rectal exam. A Kidney-Ureter-Bladder radiograph is ordered. The resulting scan shows hydronephrosis. What would be this patient’s likely BUN and Creatinine findings?
A. BUN 41 mg/dL Cr 1.2 mg/dL PSA 19 ng/mL (0-3.5
ng/mL)
B. BUN 86 mg/dL Cr 3.7 mg/dL PSA 28 ng/mL
C. BUN 153
mg/dL Cr 8.9 mg/dL PSA 5.4 ng/mL
D. BUN 28 mg/dL Cr 0.8 mg/dL
PSA 3.4 ng/mL
The correct answer is A) The reason for this is because with
postrenal azotemia, your patients have a fairly normal BUN/Cr. This
normal ratio will remain until the backup of urine flows retrograde up
the ureters and into the kidneys, causing renal failure. The normal
BUN and
Creatinine values tell the clinician that this patient
has NOT impaired their renal function yet. The PSA value is quite
elevated, and is the likely cause of the clinical signs of this
patient not being able to pee (this is called urinary hesitancy). B)
BUN 86 mg/dL Cr 3.7 mg/dL PSA 28 ng/mL has a BUN/Cr ratio of 23, which
indicates a possible prerenal etiology. Something like this could also
show up in early
renal failure or dialysis-controlled renal
failure. The PSA value is quite high, indicating that this is probably
caused by benign prostatic hypertrophy and may be the beginning of
postrenal renal failure. C) BUN 213 mg/dL Cr 8.9 mg/dL PSA 5.4 ng/mL
has a BUN/Cr ratio of 23 as well and a PSA value near the upper limit
of normal. D) BUN 28
mg/dL Cr 0.7 mg/dL PSA 3.4 ng/mL hs a low
BUN and Creatinine value with a ratio of 40. This is a perfect example
to demonstrate how the BUN:Creatinine ratio can ONLY be used in cases
of pathology. Because according to the ratio, he has prerenal renal
failure,
but his values show absolutely NO kidney damage at all.
Keep that in mind when interpreting BUN and creatinine in the future!
12-year-old female presents to her physician after she was diagnosed
and treated for streptococcal pharyngitis. She had recovered with the
antibiotics, but two weeks later, she developed generalized edema, a
puffy face, and has frothy urine. Her urinalysis studies reveal
massive proteinuria, increased polymorphonucleocytes, and renal
epithelial cells. What would you expect her BUN and Creatinine to
be?
A. BUN 10 mg/dL Creatinine 18.1 mg/dL
B. BUN 42 mg/dL
Creatinine 1.7 mg/dL
C. BUN 87 mg/dL Creatinine 4.3 mg/dL
D.
BUN 117 mg/dL Creatinine 3.2 mg/dL
The correct answer is B) which shows that she is NOT in renal
failure, because her values are close to normal. She has a nephrotic
picture with urine positive for protein, PMNs, and renal epithelial
cells. We would expect her BUN and Creatinine values to be fairly
normal, because she presented to the physician right when these
symptoms started. So she likely doesn’t have any renal failure yet,
but we can look for other symptoms to give the answer away, then we
know
what labs to look for. She’s got frothy urine (proteinuria),
generalized edema, and a nephrotic urinalysis. Then you go back to
realize that she had a streptococcal infection just 2 weeks ago, and
that’s the clincher! This is a pretty textbook picture of
poststreptococcal glomerulonephritis (PSGN).
A) BUN 10 mg/dL Creatinine 18.1 mg/dL is physiologically improbable. C. BUN 87 mg/dL Creatinine 4.3 mg/dL is a sign of renal failure, but is strange because the creatinine is elevated significantly higher than the BUN should be. This is likely caused by an increased production of creatinine, either via rhabdomyolysis (skeletal muscle destruction) or an increased intake of cooked meat D. BUN 117 mg/dL Creatinine 3.2 mg/dL is a sign of probable prerenal failure with the ratio at 36
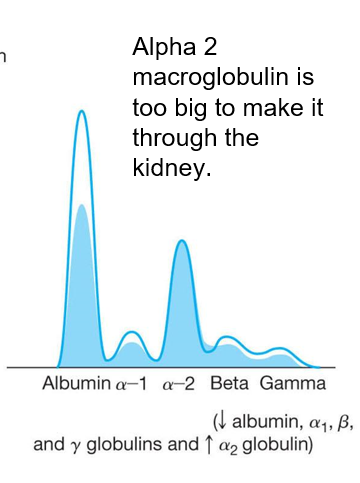
What are the usual diagnostic findings in nephrotic syndrome ?
1. Proteinuria greater than 3-3.5 g/24 hour
2. No increased serum albumin <25 g/l
3. Clinical evidence of peripheral edema
4. Severe hyperlipidaemia (total cholesterol >380 mg/dL) is often present
Where are most proteins are synthesized?
produced in the liver
Where are Immunoglobulins synthesized?
produced by plasma cells
Where are Hemoglobin synthesized?
produced in the RBC
What protein has the smallest size to charge ratio?
Albumin
note: Largest peak and migrates the fastest on electrophoresis
What protein goes the opposite way and why?
Gammas are cations so they go the other way
What is the reference range for total serum protein?
6.0 - 8.3 g/dL (may vary from lab to lab)
What is the main function of albumin?
maintains oncotic pressure (colloidal osmotic pressure)
What is the clinical significance of Albumin?
Increased catabolism - Physical injury
Decreased synthesis - Primary (liver disease), Secondary (malabsorption, malnutrition)
Increased loss - Renal protein loss
What does deficiency of α antitrypsin cause?
emphysema and cirrhosis
Note it is called antitrypsin because it destroys titrypsin and titrypsin destroyed proteins.
What is the most common alpha protein?
AAT makes up 90%, most common, of the
What is α1Acid Glycoprotein
- Major glycoprotein released in inflammation
- Carrier of cationic drugs - Digoxin, trimethoprim, and vancomycin
What is Alpha-Fetoprotein?
- First globulin from the fetus to cross the placenta in utero
- High levels seen in Spina Bifida, Anencephaly, abdominal wall defects, and all neural tube defects
What is α1 Antichymotrypsin
Serum protease inhibitor. Found between the A1 and A2 zones.
What is Haptoglobin?
Acute Phase Reactant, binds hemoglobin, and is removed in the spleen. Haptoglobin prevents hemoglobin from being removed in the glomeruli. Increased in inflammation, intravascular hemolysis, and smoking positively associated with hemolytic anemia. M ore hemaglobin means for haptoglobin needs to be there to bind it.
What is Ceruloplasmin?
Copper containing protein, oxidizes iron, Decreased in Wilson’s Disease, causing excessive Cu to accumulate in liver and brain causing cirrhosis. Binds to copper.
What is α2 Macroglobulin
Protease inhibitor (inhibits complement, coagulation, and fibrinolytics). Largely increased in nephrotic syndrome. Decreased in pancreatitis, RA, and multiple myeloma. N ote similar to to α1Antitrypsin and α1Antichymotrypsin it breaks down proteins.
What is Transferrin?
Transports Ferric (Fe3+) cations to storage sites (marrow, liver, spleen) Acute Phase Protein, transports iron, and increased in hemochromatosis
What is Hemopexin?
Plasma glycoprotein that removes heme from circulation. Increased in Diabetes, inflammation, and pregnancy. Decreased in hemolytic diseases
What are β lipoproteins?
Carry lipids in the plasma, classified as LDL-C
What is β2 Microglobulin
Found on nucleated cell membranes, especially on lymphocytes Elevated in multiple myeloma, leukemias, hepatitis, Rheumatoid Arthritis, Systemic Lupus Erythematosus, and AIDS
They work with gamma globulins.
What is CRP(C-Reactive Protein)?
Acute phase reactant and an indicator of tissue injury or inflammation
What is Fibrinogen?
Acute phase reactant and a coagulation factor. Increased in pregnancy and women on OCPs. Decreased in consumptive coagulopathies
What is Complement?
Over 30 glycoproteins with many effects on the body, think of cell lysis
What are C3and C4?
Acute phase proteins, Decreased in Disseminated Intravascular Coagulopathy (DIC), Paroxysmal Nocturnal Hemoglobinuria (PNH), infections with meningococci, or malnutrition
What are γ globulins
Gamma globulins are thought of as antibodies
Gamma globulins that have been mistakenly created against our own cells are called autoimmune diseases, meaning that we are attacking ourselves
What is the formula and range for the Albumin/Globulin Ratio (A/G ratio)?
A/G ratio = albumin / globulin (Total Protein - Albumin = Globulin)
Normal range is 1.1-1.5
What does a low (A/G ratio) indicate?
<1.1
1.multiple myeloma (immunoglobulin hyperproduction)
2.cirrhosis (lack of albumin synthesis)
3.nephrotic syndrome (loss of protein in the urine)
What does a high (A/G ratio) indicate?
High A/G ratios (>1.5)
1.leukemias (lack of immunoglobulin production)
2.genetic immunoglobulin deficiencies (Common Variable Immunodeficiency [CVID], selective Ig deficiencies)
What is the function Prealbumin / Transthyretin?
Serves as a transport protein or shuttle
What is the clinical significance of realbumin / Transthyretin?
- Synthesized by the Liver
- Acute Phase Protein
- Presence indicates adequacy of nutrition
- Lack of prealbumin suggests liver failure
What does a normal Serum Protein Electrophoresis graph look like?
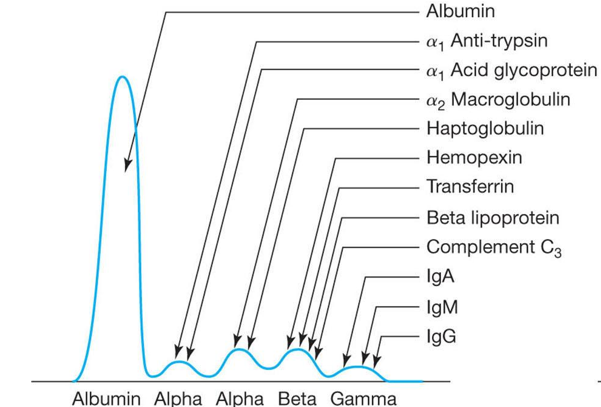
What does a nephrotic syndrome Protein Electrophoresis graph look like?
What does a acute phase reactants Protein Electrophoresis graph look like?
What does a multiple myeloma Protein Electrophoresis graph look like?
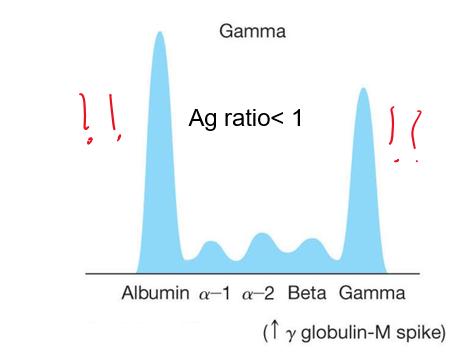
What is Multiple Myeloma
is cancer of the plasma cells, resulting in uncontrolled hyperproduction of immunoglobulin
Leads to pathologic fractures and hypercalcemia
Patients generally have bone pain and hypercalcemia along with proteinuria
Low α1 macroglobulin
high β2 micro globulin
What can cause Hypoproteinemia?
can caused by hemodilution, decreased production, increased loss of protein inadequate nutrition, water intoxication, nephrotic syndrome, or liver failure
note: Clinical giveaway is Ascites, which is an excess amount of water in the peritoneal cavity.
What happens in most forms of hepatitis?
a decreased synthetic capacity of the liver, which includes a low A/G ratio with decreased plasma albumin levels, coagulopathies
Almost all serum protien are produced by liver. C an cause bleeding and Ascites
What is the Biuret method?
Cupric ions (Cu2+) in an alkaline medium form a purple color (540 nm) as they interact with peptide bonds
What does the biuret reagent contain?
1) NaOH for alkalinity,
2) NaK tartrate,
3) Potassium Iodide (KI),
4) CuSo4
What is Refractometry used for?
rapid, approximate range of total protein concentration. This method measures the refractive index.
What is the Dye-Binding Method?
Coomassie blue in acidic solution. When the dye binds the protein, the absorbance increases at 595 nm.
What should not be done when testing for urinary proteins?
Do NOT dilute urine for proteins. You dilute for creatinine. Only smaller proteins can pass through the glomeruli, but they are VERY likely to be reabsorbed
The major problem with urinary dipstick is?
There can be a lot of false positive results
Notes: They use tetrabromphenol blue at pH of 3,
Turbidimetric methods precipitate (denature) proteins with sulfasalicylic acid (SSA), trichloroacetic acid, or benthonium chloride. SSA is known to precipitate many substances and cause false positive results
What to know about Homogentistic acid (HGA) oxidase?
it is the deficient enzyme
Leads to a build up of HGA in body tissues
Autosomal recessive
What is Ochronosis?
darkening of body tissues due to HGA
Diapers stain black because of HGA in the urine of babies
what is Cystinuria?
Defect in Amino Acid transport system, NOT a metabolic deficiency
Kidneys are unable to reabsorb the divalent amino acids (cystine, lysine, arginine, ornithine)
Cystine can result in kidney stones, which can cause flank pain and hematuria
There is a certain smell with PKU. What is that smell?
“Mousy” or “Musty” urine odor, eczema, fair complexion
note: Causes mental retardation if not corrected early in life
Can be controlled with PKU-free diet
Brain damage occurs with cessation of a PKU-free diet
what is a break down for Non-Protein Nitrogens (NPN)?
Urea nitrogen - ~45% of NPN in the blood
Uric acid - ~20% of NPN in the blood
Creatinine - ~5% of NPN in the blood
Ammonia will be covered later - ~0.2% of NPN in the blood
What formula do you need to know for BUN?
BUN (mg/dL) x 2.14 = Urea (mg/dL)
How are bun and glomerular related?
BUN is inversely correlated with glomerular filtration rate and renal plasma flow
What is the cause of Prerenal Azotemia ?
usually caused by dehydration, but can be due to any reason for impaired blood flow to the kidneys or increased protein catabolism
What is the cause of Renal Azotemia?
Acute renal failure
What is the cause of Postrenal Azotemia?
Obstructive Renal Disease
What is the formula for the Urease method ?
What are the BUN reference ranges and other important clinical information to know?
BUN Reference Range
7-18 mg/dL
24 hour urine 12-20 grams/24 hours
BUN is stable at RT for 4 hours
Several days at 4˚C
Several months at -20˚C
Males are slightly higher, but it is not clinically significant
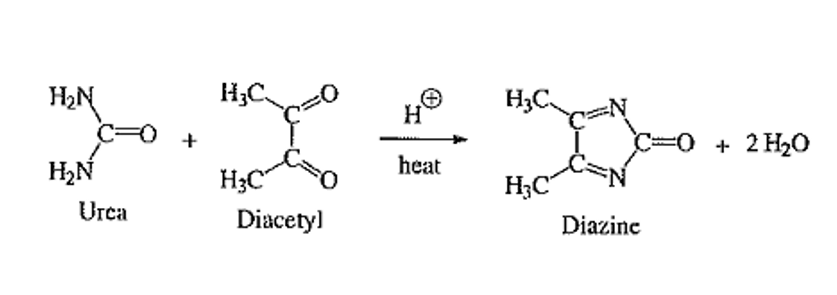
What is the formula for the Diacetyl or “Fearon” Reaction at 540 nm?
What does a higher BUN:Cr Ratio indicate?
ratio is indicative of prerenal azotemia: dehydration, heart failure
What does a lower BUN:Cr Ratio indicate?
ratio can be seen in intrarenal azotemia, dialysis, SIADH, low protein diet, diarrhea
What can a normal BUN:Cr Ratio indicate?
postrenal azotemia (causes of decreased GFR, like congestive heart failure, obstructive renal cell carcinoma, dehydration, etc.)
note:BUN is usually 15 times that of creatinine don’t use on normal patients.
BUN: 56 mg/dL Cr: 1.5 mg/dL BUN:Cr ratio:
Prerenal, Renal, or Postrenal?
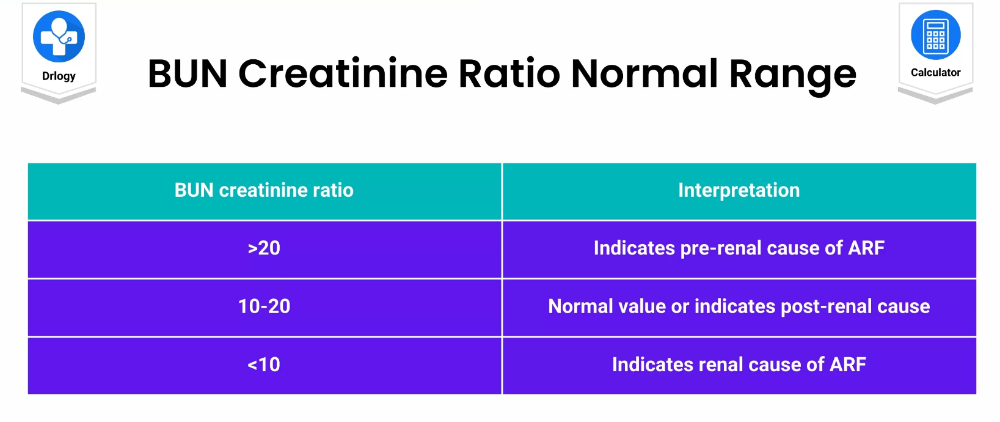
37.3= prerenal
note: Remember a BUN/Cr 10-20 is usually a renal etiology, BUN/Cr >30 is usually prerenal renal failure unless proven otherwise, BUN/Cr >40 is definitely prerenal
BUN: 43 mg/dL Cr: 2.9 mg/dL BUN:Cr ratio:
Prerenal, Renal, or Postrenal?
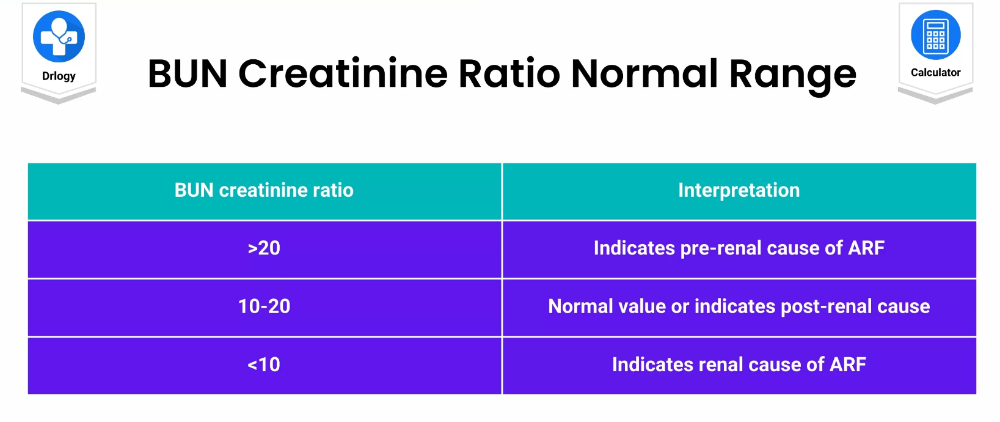
15= postrenal
note: Remember a BUN/Cr 10-20 is usually a renal etiology, BUN/Cr >30 is usually prerenal renal failure unless proven otherwise, BUN/Cr >40 is definitely prerenal
What throws off the estimation of glomerular filtration?
creatinine is secreted ever-so-slightly in the distal convoluted tubule (DCT)
In renal disease, creatinine excretion is decreased
What method is used for testing creatinine?
Jaffe Reaction - Creatinine and Picric Acid in alkaline solution
Beware! Picric acid is explosive!
Interferences with protein, glucose, uric acid, ascorbic acid, acetone, ketoacids, cephalosporins
Enzymatic methods are also available which all start with creatininase
What reference ranges for creatinine?
0.9-1.2 mg/dL men
0.6-1.1 mg/dL for women
What causes Gout?
usually increased production of Uric Acid
What causes Lesch-Nyhan Syndrome?
HGPRT deficiency which results in elevated levels of Uric Acid. Symptoms include mental retardation, muscle fasciculations, Self-mutilation
What causes Cytotoxic Chemotherapy?
Tumor-Lysis Syndrome, the rapid killing of cells results in DNA damage, and the production of lots of Uric Acid
What causes Malignancies?
Cancer can lead to rapid formation of cells, but they often die off quickly, resulting in DNA damage and release of Uric Acid into the serum
What is uremia?
Urea and Creatinine
Results from Renal failure
Neurotoxic
Elevated levels of Uric Acid in the blood, can cause Uremic Frost on a patient’s skin
57-year-old male - congestive heart failure, Creatinine of 2.1 mg/dL, BUN of 75 mg/dL. what is the BUN/Cr ratio and Prerenal, Renal, or Postrenal?
Prerenal azotemia
Ratio of 35.7 not full diagnositic need over 40
12-year-old female - polycystic kidney disease, Creatinine of 4.5 mg/dL, BUN of 81 mg/dL
what is the BUN/Cr ratio and Prerenal, Renal, or Postrenal?
Renal azotemia
Ratio of 18: in ratio
75-year-old male - benign prostatic hypertrophy, Creatinine of 3.2 mg/dL, BUN of 57 mg/dL
what is the BUN/Cr ratio and Prerenal, Renal, or Postrenal?
Postrenal azotemia
Ratio of 17.8 why this is post is because of the prostate vs the kidney
How do we test for ammonia?
the glutamate dehydrogenase method
It measures the diminishing concentration of NADP at 340
nm
This sample must be tested immediately, no waiting. The sample should be venous blood, collected in EDTA or Heparin, and placed on ice
What is the process for hepatic encephalopathy?
Liver failure → ↑NH3 → neuronal destruction → hepatic encephalopathy
What is Reye’s syndrome?
The result is fulminant liver failure and many patients don’t survive the ordeal. Blood ammonia levels are the preferred lab test in this scenario, because they are most closely associated with prognosis and survival
Note: The connection that I want you to make with this is that whenever you hear of a child taking aspirin for a viral illness
What is a lesser known cause of hyperammonemia?
urea cycle enzyme disorders
Define the following: Primary protein.
A sequence of amino acid chains.
Define the following: Secondary protein structure
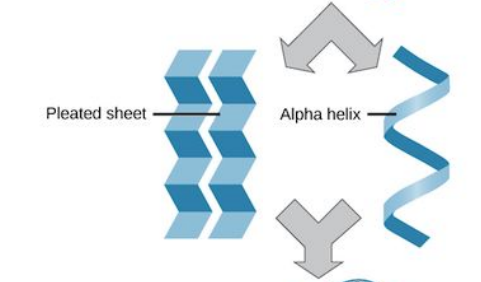
Hydrogen bonding of the peptide back bone cause the amino acids to fold into a repeating pattern.
Define the following: tertiary protein structure
three-dimensional folding patter of a protein due to side chain reactions
Define the following: quaternary protein structure

Protein consisting of more than one amino acid chain.