Chp. 17 Study questions - Blood
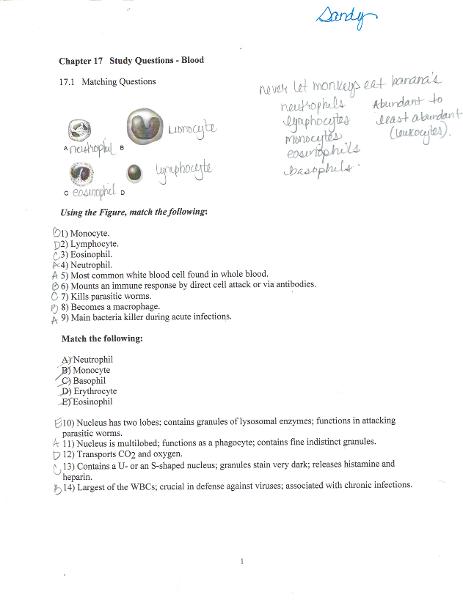
Neutrophil
- Most common WBC found in whole blood
- Main bacteria killer during acute infection.
Monocyte
- Mounts an immune response by direct cell attack or via antibodies.
- Becomes a macrophage.
Eosinophil
- Kills parasitic worms.
Lymphocyte
NEVER LET MONKEYS EAT BANANA'S
- Neutrophils
- Lymphocytes
- Monocytes
- Eosinophils
- Basophils
Nucleus has two lobes; functions as a phagocyte; contains five indistinct granules.
Neutrophil
Largest of the WBC's; crucial in defense against viruses; associated with chronic infections
Monocyte
Contains a U- or an S- shaped nucleus; granules stain very dark; releases histamine and heparin
Basophil
Transports CO2 and oxygen
Erythrocyte
Nucleus has two lobes; contains granules of lysosomal enzymes; functions in attacking parasitic worms.
Eosinophil
Albumin
- The major contributor to plasma osmotic pressure.
- Makes up most of plasma protein
Fibrinogen
- Thrombin catalyzes the activation of these molecules present in plasma.
- Forms the structural framework of a blood clot.
Necessary for coagulation
Fibrinogen
Transport proteins that bind to lipids, metal ions, and fat-soluble vitamins
Alpha and Beta globulins
Main contributor to osmotic pressure
Albumin
Antibodies released by plasma cells during immune respone
Gamma globulins
Protein capable of changing shape and color in the presence of O2
Hemoglobin
Polymorphonuclear leukocyte
Neutrophil
Adverse reaction of donor blood cells with recipient plasma
Agglutination
Lacking in hemophilia type A
Factor VIII
White blood cell without cytoplasmic granules
Monocyte
Hormone that stimulates production of RBC's
Erythropoietin
A fibrous protein that gives shape to an RBC plasma membrane
Spectrin
Produced by platelets
Prostaglandin derivates such as Thromboxane A2
Stimulates WBC production
Interleukins and CSF's
Natural anticoagulant found in basophils
Heparin
Cancerous condition involving WBC's
Leukemia
Condition in which blood has abnormally low oxygen-carrying capacity
Anemia
Abnormal excess of erythrocytes resulting in an increase in blood viscosity
Polycythemia
Free-floating thrombus in the bloodstream
Embolism
Platelet deficiency resulting in spontaneous bleeding from small blood vessels
Thrombocytopenia
What is not a functional characteristic of WBC's
Granulosis
What is the average normal pH range of blood
7.35-7.45
Special type of hemoglobin present in fetal red blood cells is___
Hemoglobin F
What is a parent cell for all formed elements of blood?
Hemocytoblast
What blood type is the Universal donor?
O
What is not a distribution function of blood?
transport of salts to maintain blood volume
What is a protective function of blood?
prevention of blood loss
TRUE OR FALSE.........
Blood typing for the Kell, Lewis, and Duffy factors is always done before a blood transfusion?
FALSE
What might trigger erythropoiesis?
hypoxia of EPO- producing cells
Blood reticulocyte counts provide information regarding _____
rate of erythrocyte formation
Blood type AB negative can _______
receive any blood type in moderate amounts except that with the Rh antigen
What does not describe blood?
Blood carriers body cells to injured areas for repair
When neither anti-A serum nor anti-B serum clot on a blood plate with donor blood, the blood is type ______
O
What is not true regarding blood cell formation?
Platelets are formed from myeloblasts
What does Blood volume restorers not include?
packed cells
James has a Hgb measurement of 16g/100ml blood. This is ___
within normal range
What plasma protein is the major contributor to osmotic pressure is?
Albumin
What can not be expected with polycythemia?
low blood viscosity
No visible cytoplasmic granules are present in _____
monocytes
What is not a phase of hemostasis?
fibrinolysis
What is not a structural characteristic that contributes to erythrocyte gas transport functions?
mitotically active
A lack of intrinsic factor, leading to a deficiency of Vitamin B12 and causing an appearance of large pale cells called macrocytes, is characteristic of _______
pernicious anemia
What is the slowest step in the clotting process?
formation of prothrombin activator
Thromboembolic disorders include _____
embolus formation, a clot moving within the circulatory system
What is not a cause of bleeding disorders?
excess secretion of platelet-derived growth factor (PDGF)
What is characteristics of all leukocytes?
they are nucleated
What is true about blood plasma?
It is 90% water
What sticks to the damaged area of a blood vessel and helps seal the break?
Platelets
CORRECT SEQUENCE
- Formation of thromboplastin
- prothrombin-thrombin
- fibrinogen- fibrin
- clot retraction
Fred's blood was determined to be AB positive. What does this mean?
There are no antibodies to A, to B, or to Rh antigens in the plasma.
What would not be a possible cause of sickling of RBC's in someone with sickle-cell anemia?
sleeping in a well ventilated room
What does not impair coagulation?
vascular spasm
When can erythroblastosis fetalis not possibly happen in a child of an Rh negative mother?
if the father is Rh-
Blood is a ________
suspension
What organ in the body regulates erythrocyte production?
kidney
What element can kill parasitic worms?
Eosinophils
What is a committed granular leukocyte stem cell that produces neutrophils?
Myeloblast
What is the rarest leukocyte?
basophil
What is the universal recipient blood type?
AB-
When monocytes migrate into the interstitial spaces, they are called?
macrophages
What is the stage of development in the life of an erythrocyte during which the nucleus is ejected?
normoblast
How many polypeptide chains make up Hgb?
4
List the general factors that limit normal clot growth
removal of coagulation factors and inhibition of activated clotting factors
When are whole blood transfusions routinely given?
- substantial blood loss
- severe anemia
- thrombocytopenia
LIFE CYCLE OF RED BLOOD CELLS
- Low O2 levels in blood stimulate kidneys to produce erythropoietin.
- Erythropoietin levels rise in blood.
- Erythropoietin and raw materials in blood promote erythropoiesis in red bone marrow.
- New erythrocytes enter bloodstream; function about 120 days.
- Aged and damaged RBC's are engulfed by macrophages of spleen, liver, and bone marrow: the Hgb is broken down.
- Raw materials are made available in blood for erythrocyte synthesis.
- Erythrocytes(RBC'S) - biconcave, anucleate disc, salmon colored. (4-6 million) development ( duration -15 days) ( life span - 100-120 days) Transport O2 and CO2.
- Leukocytes (WBC'S) spherical, nucleated cells. ( 4800-10,800 cells)
-
Granulocytes
- Neutrophil - multilobed nucleus; inconspicuous cytoplasmic granules. (3000-7000 cells) (Duration 14 days) (lifespan 6 hours to a few days) Phagocytize bacteria.
- Eosinophil - Bilobed nucleus; red cytoplasmic granules. (100-400 cells) (Duration 14 days) (lifespan 6 hours to a few days) kill parasitic worms; complex role in allergy & asthma.
- Basophil - bilobed nucleus; large purplish-black cytoplasmic granules, (20-50 cells) (Duration 1-7 days) (lifespan a few hours to a few days) Release histamine and other mediators of inflammation; contain Heparin, an anticoagulant.
Agranulocytes
- Lymphocyte - spherical or indented nucleus; pale blue cytoplasm. (1500-3000 cells) (duration days to weeks) (lifespan months) mount immune response by direct cell attack or via antibodies.
- Monocyte - U-or kidney- shaped nucleus; gray-blue cytoplasm, (100-700 cells) (duration 2-3 days) (lifespan months) phagocytosis; develop into macrophage in the tissues.
Platelets
- Discoid cytoplasmic fragments containing granules, stain deep purple, (150,000-400,000 cells) (duration 4-5 days) (lifespan 5-10 days) seal small tears in blood vessels; instrumental in blood clotting.