Diabetes Mellitus is a metabolic disorder characterized by glucose intolerance or inadequate insulin production of the pancreas. It has two types, namely:
Type 1 or Insulin dependent DM (IDDM) and Type 2 or
Non- insulin dependent DM (NIDDM).
The metabolic effects of
diabetes mellitus include the decrease in
utilization of glucose because insufficiency in insulin supply in the
body, an increased fat metabolism, when the body breaks down fat for
energy since glucose is not available, and increased protein
utilization, referring to an increase in catabolism and protein wasting.
The complications of DM consist of neuropathy, retinopathy, nephropathy, cataracts, glaucoma, pyelonephritis, peripheral vascular lesions, coronary artery disease, stroke and hypertension. With its complications, diabetes mellitus is considered the third leading cause of death by disease and risk factors involve mainly of genetics and obesity.
Nursing Diagnosis: Fluid Volume Deficient (Regulatory Failure)
Possible Etiologies:(Related to)
•Uncontrolled
diabetes mellitus
•Osmotic diuresis from
hyperglycemia
•Excessive gastric loss (diarrhea and
vomiting)
•Restricted or low fluid intake due to nausea or confusion
Defining characteristics:
(Evidenced by)
•Statements of fatigue and
nervousness
•Increased urinary output
•Concentrated
urine
•Weakness
•Thirst
•Sudden weight loss
•Poor
skin turgor/ dry skin and mucous
membranes
•Hypotension
•Increased pulse rate
•Decreased
pulse volume and pressure/ delayed capillary refill
•Change in
mental state
Goals/ Objectives:
Short term goal:
Client will maintain hydration at a functional level as evidenced by adequate urine output, stable vital signs, palpable peripheral pulses, good skin turgor and capillary refill, and electrolyte levels within nor
https://html2-f.scribdassets.com/27msxl2zsw4p4h6s/images/1-2fd53a3b19.jpg
DIABETES MELLITUS
1. Obtain history for intensity and duration of symptoms such as vomiting and excessive urination.
2. Monitor the vital signs like: a.Orthostatic BP changes b. Respiratory changes i.e. Kussmaul’s respirations acetone breath c.Respiratory rate and quality; use of accessory muscles, periods of apnea, and cyanosis temperature, skin turgor
3. Check peripheral pulses, capillary refill, and for skin turgor.
4. Strictly monitor the intake and the output.
5. Encourage client to take at least 2500ml/ day.
6. Weigh client daily or as indicated.
7. Investigate changes in mentation. - Helps in making approximation of total volume loss. Symptoms may be present for hours or days and presence of other diseases usually result, too, to increase in sensible fluid losses.- Hypovolemia can be manifested by hypotension and tachycardia; Carbonic acid is removed in the lungs through respiration and producing respiratory alkalosis for ketoacidosis; Acetone breath is due to acetoacetic acid and should disappear when condition is corrected; Cyanosis, apnea and increase in respiratory effort may be due to compensation from acidosis; Fever with flushed skin reflects dehydration. - These are indicators for the hydration status of a client and so as the circulating volume in the body. -
Gives baseline data of client’s
hydration status and to know the approximation of fluid replacement; the function of kidney and the effectiveness of the fluid replacement therapy. - It maintains hydration level in the functional state. - It provides the current fluid status and adequacy of fluid replacement
Bipolar disorders are characterized by recurrent mood swings of varying degree from depression to elation with intervening periods of normalcy. Milder mood swings such as cyclothymia may be manifested or viewed as everyday creativity rather than an illness requiring treatment. Hypomania can actually enhance artistic creativity and creative thinking/ problem-solving.
This plan of care focuses on treatment of the manic phase. (Note: Bipolar II disorder is characterized by periods of depression and hypomania, but without manic episodes.)
Psychodynamics
Psychoanalytical theory
explains the cyclic behaviors of mania and depression as a response to
conditional love from the primary caregiver. The child is maintained
in a dependent position, and ego development is disrupted. This gives
way to the development of a punitive superego (anger turned inward or
depression) or a strong id (uncontrollable impulsive behavior or
mania). In the psychoanalytical model, mania is viewed as the mirror
image of depression, a “denial of depression.”
Biological
There is increasing evidence to
indicate that genetics plays a strong role in the predisposition to
bipolar disorder. Research suggests a combination of genes may create
this predisposition. Incidence among relatives of affected individuals
is higher than in the general population. Biochemically there appear
to be increased levels of the biogenic amine norepinephrine in the
brain, which may account for the increased activity of the manic individual.
Family
Dynamics
Object loss theory suggests that
depressive illness occurs if the person is separated from or abandoned
by a significant other during the first 6 months of life. The bonding
process is interrupted and the child withdraws from people and the
environment. Rejection by parents in childhood or spending formative
years with a family that sees life as hopeless and has a chronic
expectation of failure makes it difficult for the individual to be
optimistic. The mother may be distant and unloving, the father a less
powerful person, and the child expected to achieve high social and
academic success.
NURSING PRIORITIES
1. Protect client/others
from the consequences of hyperactive behavior.
2. Provide for
client’s basic needs.
3. Promote reality orientation, realistic
problem-solving, and foster autonomy.
4. Support client/family
participation in follow-up care/community treatment.
DISCHARGE GOALS
1. Remains free of injury with
decreased occurrence of manic behavior(s).
2. Balance between
activity and rest restored.
3. Meeting basic self-care
needs.
4. Communicating logically and clearly.
5.
Client/family participating in ongoing treatment and understands
importance of drug
therapy/monitoring.
6. Plan in place to
meet needs after discharge.
Nursing diagnosis of Bipolar Disorders: TRAUMA, risk for/VIOLENCE, risk for directed at others may be related to Emotional difficulties; irritability and impulsive behavior; delusional thinking; angry response when ideas are refuted/wishes denied; Manic excitement; History of assaultive behavior possibly evidenced by Body language, increased motor activity; Difficulty evaluating the consequences of own actions; Overt and aggressive acts; hostile, threatening verbalizations.
Desired Outcome:
1. Demonstrate self-control with decreased hyperactivity.
2. Acknowledge why behavior occurs.
3. Verbalize feelings
(anger, etc.) in an appropriate manner.
4. Use problem-solving
techniques instead of violent behavior/threats or intimidation.
Nursing intervention and rationale:
1.
Decrease environmental stimuli, avoiding exposure
to areas or situations of predictable high stimulation and removing
stimulation from area if client becomes agitated.
Rationale:
Client may be unable to focus attention on only relevant stimuli and
will be reacting/responding to all environmental stimuli.
2. Continually reevaluate client’s ability to tolerate
frustration and/or individual situations.
Rationale:
Facilitates early intervention and assists client to manage situation
independently, if possible.
3. Provide safe e
•Weight gain
•Impaired memory
•Poor
concentration
•Confusion
•Mental slowness
•Hand
tremor
•Sedation or lethargy
Common side effects of lithium include:
Avoid antidepressants. The treatment for bipolar depression is
different than for regular depression. In fact, antidepressants can
actually make bipolar disorder worse or trigger a manic episode. Try
mood stabilizers first and never take antidepressants without them, as
antidepressants can trigger mania and rapid mood cycling when used on
their own.
• Take advantage of natural mood stabilizers. Your
lifestyle has an impact on your symptoms. If you make healthy daily
choices, you may be able to reduce the amount of medication you need.
Mood stabilizers that don’t require a prescription include keeping a
strict sleep schedule, exercising regularly, practicing relaxation
techniques, and developing a solid support system.
• Add therapy
to your treatment plan. Research shows that people who take medication
for bipolar disorder tend to recover much faster and control their
moods better if they also get therapy. Therapy gives you the tools to
cope with life's difficulties, monitor your progress, and deal with
the problems bipolar disorder is causing in your personal and
professional life.
• Continue taking medication, even after you
feel better. The likelihood of having a relapse is very high if you
stop taking your bipolar medication. Suddenly stopping medication is
especially dangerous. Talk to your doctor before you make any changes,
even if you believe you no longer need medication. Your doctor can
help you make any adjustments safely.
LITHIUM
LITHIUM
Trade Name(s)
•Carbolith [Canada]
•Lithane
[Canada]
•Lithmax [Canada]
•Lithobid
Pregnancy Category
Category D
Ther. Class.
mood stabilizers
Indications
Manic episodes of bipolar I
disorder (treatment, maintenance, prophylaxis).
Action
•Alters cation transport in nerve and
muscle.
•May also influence reuptake of neurotransmitters.
Therapeutic Effect(s):
Prevents/decreases incidence of acute manic episodes.
Pharmacokinetics
Absorption: Completely absorbed after oral administration.
Distribution: Widely distributed into many tissues and fluids; CSF levels are 50% of plasma levels. Crosses the placenta; enters breast milk.
Metabolism and Excretion: Excreted almost entirely unchanged by the kidneys.
Half-life: 20–27 hr.
TIME/ACTION PROFILE (antimanic effects)
Contraindication/Precautions
Contraindicated in:
•Hypersensitivity;
•Severe cardiovascular or renal
disease;
•Dehydrated or debilitated patients;
•Brugada
syndrome;
•Should be used only where therapy, including blood
levels, may be closely monitored;
•Some products contain alcohol
or tartrazine and should be avoided in patients with known
hypersensitivity or intolerance;
•Lactation: Lactation.
Use Cautiously in:
•Any degree of cardiac,
renal, or thyroid disease;
•Diabetes mellitus;
•OB: Fetal
cardiac anomalies are associated with lithium use; however, potential
maternal benefit may warrant use in some pregnant women;
•Geri:
Initial dosage ↓ recommended.
Adverse Reactions/Side Effects
CNS: SEIZURES, fatigue, headache, impaired memory, ataxia, sedation, confusion, dizziness, drowsiness, psychomotor retardation, restlessness, stupor
EENT: aphasia, blurred vision, dysarthria, tinnitus
CV: ECG changes, arrhythmias, edema, hypotension, unmasking of Brugada syndrome
GI: abdominal pain, anorexia, bloating, diarrhea, nausea, dry mouth, metallic taste
GU: polyuria, glycosuria, nephrogenic diabetes insipidus, renal toxicity
Interactions
Drug-Drug
•May prolong the action of
neuromuscular blocking agents .
•↑ risk of neurologic toxicity
with haloperidol .
•Diuretics, methyldopa, probenecid,
fluoxetine, and NSAIDs may ↑ risk of toxicity.
•Blood levels may
be ↑ by ACE inhibitors .
•Lithium may ↓effects of chlorpromazine
.
•Chlorpromazine may mask early signs of lithium
toxicity.
•Hypothyroid effects may be additive with potassium
iodide or antithyroid agents .
•Aminophylline, phenothiazines,
and drugs containing large amounts of sodium ↑ renal elimination and
↓ effectiveness.
•Psyllium can ↓ lithium levels.
Drug-Natural Products:
Caffeine-containing herbs ( cola nut, guarana, mate , tea, coffee) may ↓ lithium serum levels and efficacy.
Drug-Food:
Large changes in sodium intake may alter the renal elimination of lithium. ↑ sodium intake will ↑ renal excretion.
Route/Dosage
Precise dosing is based on serum lithium levels. 300 mg lithium carbonate contains 8–12 mEq lithium
PO: (Adults and children ≥12 yr): Tablets/capsules– 300–600 mg 3 times daily initially; usual maintenance dose is 300 mg 3–4 times daily. Extended-release tablets– 450–900 mg twice daily or 300–600 mg 3 times daily initially; usual maintenance dose is 450 mg twice daily or 300 mg 3 times daily.
PO: (Children <12 yr): 15–20 mg (0.4–0.5 mEq)/kg/day in 2–3 divided doses; dosage may be adjusted weekly.
Availability (generic available)
Capsules: 150 mg, 300 mg, 600 mg
Oral solution: 300 mg (8 mEq lithium)/5 mL
Assessment
•Assess mental status (orientation,
mood, behavior) initially and periodically. Initiate suicide
precautions if indicated.
•Monitor intake and output ratios.
Report significant changes in totals. Unless contraindicated, fluid
intake of at least 2000–3000 mL/day should be maintained. Weight
should also be monitored at least every 3 mo.
Lab Test Considerations:
Evaluate renal and thyroid function, WBC with differential, serum electrolytes, and glucose periodically during therapy.
Toxicity Overdose: Monitor serum lithium levels twice weekly during initiation
Neurologic effects of lithium toxicity include the following:
• Tremors
• Lethargy
• Confusion
• Seizures
• Coma
Gastrointestinal effects of lithium toxicity include the following:
• Nausea
• Vomiting
• Crampy abdominal pain
• Diarrhea
Mild-to-moderate lithium toxicity is characterized by tremor, weakness, and mild confusion. Moderate-to-severe lithium toxicity is characterized by the following:
• Altered mental status
• Muscle fasciculations
• Stupor
• Seizures
• Coma
• Hyperreflexia
• Cardiovascular collapse
As with all toxic ingestions, it is important to determine the amount, time, co-ingestants, and reason for ingestion. Toxicity does not often correlate with the measured lithium level since clinical toxicity is affected by the type of the poisoning.
Clinical features
Three main categories of lithium poisoning are as follows: acute, acute-on-chronic, and chronic.
Acute poisoning
These patients usually do not have a tissue body burden and symptoms are predominately gastrointestinal (GI), including nausea, vomiting, cramping, and sometimes diarrhea. Progression of acute toxicity can involve neuromuscular signs such as tremulousness, dystonia, hyperreflexia, and ataxia. Cardiac dysrhythmias have been reported but rarely occur. The most common electrocardiographic finding is T-wave flattening.
Acute-on-chronic poisoning
These patients take lithium regularly and have taken a larger dose recently. These patients may display both GI and neurologic symptoms, and serum levels can be difficult to interpret. Patients should be treated according to their clinical manifestations.
Chronic poisoning
These patients typically have a large body burden of lithium and may be difficult to treat. Chronic lithium toxicity is usually precipitated with introduction of new medication that may impair renal function/excretion or cause a hypovolemic state. Symptoms are primarily neurologic. Mental status is often altered and can progress to coma and seizures if the diagnosis is unrecognized. Many severely poisoned patients can develop a syndrome of irreversible lithium-effectuated neurotoxicity (SILENT) such as cognitive impairment, sensorimotor peripheral neuropathy, and cerebellar dysfunction.
Drug interactions
Three major drug classes have been identified as potential precipitants of lithium toxicity, as follows:
• Diuretics that promote renal sodium wasting
• Angiotensin-converting enzyme (ACE) inhibitors that reduce glomerular filtration rate (GFR) and enhance the tubular reabsorption of lithium
• Nonsteroidal anti-inflammatory drugs (NSAIDs) that reduc
The central nervous system (CNS) is the major organ system affected, although the renal, gastrointestinal (GI), endocrine, and cardiovascular (CV) systems also may be involved.
Lithium is available only for oral administration. It is almost completely absorbed from the GI tract. Peak levels occur 2-4 hours postingestion, although absorption can be much slower in massive overdose or with ingestion of sustained-release preparations.
Lithium dosing
Lithium is minimally protein bound (< 10%) and has an apparent volume of distribution of 0.6-1 L/kg. The therapeutic dose is 300-2700 mg/d with desired serum levels of 0.6-1.2 mEq/L.
Lithium clearance is predominantly through the kidneys. Because it is minimally protein bound, lithium is freely filtered at a rate that is dependent upon the glomerular filtration rate (GFR). Consequently, dosing must be adjusted based on renal function. Individuals with chronic renal insufficiency must be closely monitored if placed on lithium therapy.
Most filtered lithium is reabsorbed in the proximal tubule; thus, drugs known to inhibit proximal tubular reabsorption, such as carbonic anhydrase inhibitors and aminophylline, may increase excretion. Diuretics acting distally to the proximal tubule, such as thiazides and spironolactone, do not directly affect the fractional excretion of lithium (although they may affect serum lithium levels indirectly through their effects on volume status). Reabsorption of lithium is increased and toxicity is more likely in patients who are hyponatremic or volume depleted, both of which are possible consequences of diuretic therapy.
Lithium half-life
The plasma elimination half-life of a single dose of lithium is from 12-27 hours (varies with age). The half-life increases to approximately 36 hours in elderly persons (secondary to decreased GFR). Additionally, half-life may be considerably longer with chronic lithium use
Assess patient's mental status initially and periodically; if
indicated, initiate suicide preventions
Monitor intake and output
and report any drastic changes.
Patient should be drinking at
least 2000-3000 mL and day.
Patient's weight should be taken
every 3 months.
Monitor renal and thyroid function.
Test
patient's WBC with differential.
Test patient's glucose
levels.
Monitor serum lithium levels twice a week during chronic
therapy.
Assess patient for signs and symptoms of lithium toxicity.
Time to steady state - it takes four to five days for a steady state to occur after commencement of lithium (lithium carbonate or lithium citrate) therapy. At this time the first sample should be taken after starting treatment.
Therapeutic range (may vary with respect to different
laboratories and therapeutic indication):
## once daily dose -
at 12 hours, 0.7 to 1.0 mmol/l; at 24 hours, 0.4 to 0.8
mmol/l
## twice daily dose - at 12 hours, 0.4 to 0.8 mmol/l
Notes:
##NICE state that (2)##serum lithium levels
should be checked 1 week after starting and 1 week after every dose
change, and until the levels are stable. The aim should be to
maintain serum lithium levels between 0.6 and 0.8 mmol per litre in
people being prescribed it for the first time
##for people who
have relapsed previously while taking lithium or who still have
sub-threshold symptoms with functional impairment while receiving
lithium, a trial of at least 6 months with serum lithium levels
between 0.8 and 1.0 mmol per litre should be considered
Laboratory Studies
Therapeutic drug monitoring is readily available in most settings, and symptomatic patients should have their lithium levels measured. levels may not correlate with clinical symptoms due to the kinetic profile of lithium. A repeat level should be checked several hours later after intravenous hydration to disclose any trend. Serial levels may be warranted in cases of sustained-release tablets.
The sample must be sent in a lithium-free tube, as falsely elevated levels have been obtained in plasma samples obtained in lithium-containing tubes.
Urinalysis, electrolyte levels, and renal function should also be sent. A low anion gap (see the Anion Gap calculator) or a low urine specific gravity may suggest lithium toxicity due to sodium loss.
Thyroid function panel may also be considered in patients presenting with symptoms suggestive of hypothyroidism.
Co-ingestants should also be considered in cases of intentional overdose.
Acetaminophen level should be obtained in every patient suspected of intentional overdose.
Lumbar puncture should be considered in patients with altered mental status and suspicion of CNS infection.
Imaging Studies
Consider a CT scan of the head in individuals with severe movement disorders, seizures, stupor, or coma. CT scan may be needed to rule out other etiologies and to examine for trauma secondary to intoxication.
Other Tests
Electrocardiography
Chronic lithium toxicity is frequently associated with nonspecific and diffuse depressed ST segments and T-wave inversion unassociated with symptoms or significant sequelae.
Lithium intoxication may result
Atypical Antipsychotics for Bipolar Disorder
Antipsychotics had a large part in helping many people leave residential mental health care facilities; however, many people found typical antipsychotic side effects intolerable. In the 1970s, second generation antipsychotics, known as atypical antipsychotics, were developed with fewer motor control side effects.
The following atypical antipsychotics are approved
for the treatment of bipolar disorder:1
•Aripiprazole (Abilify)
– actually considered a third generation antipsychotic; is thought to
have fewer metabolic side effects than other antipsychotics. Approved
for bipolar mania, mixed state and maintenance
treatment.
•Asenapine (Saphris) –newly-approved (mid-2009)2 ;
approved to treat bipolar mania and mixed states.
•Olanzapine
(Zyprexa) – approved for people age 13 and over with bipolar disorder
type 1. FDA-approved for bipolar mania, mixed state and maintenance
treatment.
•Quetiapine (Seroquel) – the only antipsychotic
approved for the treatment of bipolar depression. Also approved to
treat bipolar mania.
•Risperidone (Risperdal) – approved for
those age 10 and over with bipolar disorder type 1. FDA-approved for
bipolar mania and mixed state treatment.
•Ziprasidone (Geodon) –
approved to treat bipolar manic episodes and mixed episodes.
One additional drug, Symbax is approved for the treatment of bipolar depression and is an olanzapine/fluoxetine (Prozac) combination.
Side Effects of Antipsychotic Medications
Antipsychotic medication may be used alone (monotherapy) or with other medications, typically lithium or valproate. While antipsychotics have helped many, this class of medication tends to have a more serious side effect profile and some estimate 50% of people stop taking the drugs due to side effects.3
In first generation typical antipsychotics, the
primarily concerning side effects surround involuntary muscle
movements. This includes side effects like:4
•Tardive dyskinesia
– involuntary repetitive muscle movements
•Dystonia – sustained
muscle contractions cause twisting and repetitive movements of
abnormal posture
•Akathisia – inner restlessness and an
inability to sit still
•Muscle rigidity and tremor
•Seizures
While atypical
Lithium – The First Mood Stabilizer
Lithium is the only true mood stabilizing medication. While other medications may be termed "mood stabilizers," lithium is the only drug technically of that class.
Lithium was the first compound approved by the Food and Drug Administration (FDA) for the treatment of bipolar disorder. Lithium is approved for use in bipolar mania and bipolar maintenance treatment; although it is frequently used to treat bipolar depression, often in combination with other medications. Lithium has an unparalleled antisuicidal property, shown to reduce the risk of attempted and completed suicides by 80%.1
Lithium is still the first-choice mood stabilizing drug in many circumstances but blood levels must be constantly monitored to ensure the lithium level is high enough to be effective but not high enough to be toxic. Thyroid levels also must be carefully monitored as lithium can reduce thyroid levels.2
Anticonvulsants as Mood Stabilizers
Mood stabilizers are medications used to treat the mood swings associated with bipolar disorder. Detailed info on mood stabilizing medications.Anticonvulsants used in the treatment of mood disorders are frequently also termed mood stabilizers. Anticonvulsants are actually medications designed to treat seizure disorders but some have shown to be effective mood stabilizers. Some anticonvulsant mood stabilizers have been shown to be particularly useful in treating bipolar depression and rapid-cycling bipolar disorder. The three most widely used anticonvulsant mood stabilizers are carbamazepine, valproate and lamotrigine.3
Carbamazepine
Carbamazepine (Tegretol) is often an effective mood stabilizing medication in those who do not respond to lithium and has been shown to effectively treat rapid-cycling bipolar disorder. It is approved by the FDA for use in manic epidodes and mixed bipolar episodes but it often used as a maintenance mood stabilizer.
Valproate
Valproate sodium (also valproic acid, divalproex sodium, brand name Depakote) is approved in the treatment of bipolar mania. Valproate is a mood stabilizing agent commonly combined with lithium or other medications to treat bipolar. Valproate has been shown effective in treating rapid-cycling
Symptoms
Bipolar Symptoms
The primary symptoms of bipolar disorder are dramatic and unpredictable mood swings.
Mania Symptoms
Mania symptoms may include excessive happiness, excitement, irritability, restlessness, increased energy, less need for sleep, racing thoughts, high sex drive, and a tendency to make grand and unattainable plans.
Depression Symptoms
Depression symptoms may include sadness, anxiety, irritability, loss of energy, uncontrollable crying, change in appetite causing weight loss or gain, increased need for sleep, difficulty making decisions, and thoughts of death or suicide.
Types
Bipolar Types
There are several types of bipolar disorder; all involve episodes of depression and mania to a degree. They include bipolar I, bipolar II, cyclothymic disorder, mixed bipolar, and rapid-cycling bipolar disorder.
Bipolar I
A person affected by bipolar I disorder has had at least one manic episode in his or her life. A manic episode is a period of abnormally elevated mood, accompanied by abnormal behavior that disrupts life.
Bipolar II
Bipolar II is similar to bipolar I disorder, with moods cycling between high and low over time. However, in bipolar II disorder, the "up" moods never reach full-on mania.
Rapid Cycling
In rapid cycling, a person with bipolar disorder experiences four or more episodes of mania or depression in one year. About 10% to 20% of people with bipolar disorder have rapid cycling.
Mixed Bipolar
In most forms of bipolar disorder, moods alternate between elevated and depressed over time. But with mixed bipolar disorder, a person experiences both mania and depression simultaneously or in rapid sequence.
Cyclothymia
Cyclothymia (cyclothymic disorder) is a relatively mild mood disorder. People with cyclothymic disorder have milder symptoms than in full-blown bipolar disorder.
Bipolar Spectrum
Complications
Bipolar Disorder Complications
Self-injury, often referred to as cutting, self-mutilation, or self-harm, is an injurious attempt to cope with overpowering negative emotions, such as extreme anger, anxiety, and frustration. It is usually repetitive, not a one-time act.
Bipolar Disorder in Pregnancy
Learn about the complications of bipolar disorder during pregnancy and what you need to know about your medications and mania.
Warning Signs
Bipolar Warning Signs
When a person's illness follows the classic pattern, diagnosing bipolar disorder is relatively easy. But bipolar disorder can be sneaky. Symptoms can defy the expected manic-depressive sequence.
Emergencies & Suicide Prevention
Suicide is a very real risk for people with bipolar disorder, whether they're in a manic or depressive episode -- 10%-15% of people with bipolar disorder kill themselves. But treatment greatly lowers the risk.
A peptic ulcer is a defect in the lining of the stomach or the first part of the small intestine, an area called the duodenum. A peptic ulcer in the stomach is called a gastric ulcer. An ulcer in the duodenum is called a duodenal ulcer.
Pathophysiology
A peptic ulcer is an excavation formed in the mucosal wall of the stomach, pylorus, duodenum, or esophagus. It is frequently referred to as a gastric, duodenal, or esophageal ulcer, depending on its location. It is caused by the erosion of a circumscribed area of mucous membrane.
Peptic ulcer has been associated with bacterial infection, such as Helicobacter pylori. The greatest frequency is noted in people between the ages of 40 and 60 years. After menopause, the incidence among women is almost equal to that in men.
Predisposing factors include family history of peptic ulcer, blood type O, chronic use of nonsteroidal antiinflammatory drugs (NSAIDs), alcohol ingestion, excessive smoking, and, possibly, high stress. Esophageal ulcers result from the backward flow of hydrochloric acid from the stomach into the esophagus.
Clinical Manifestations
•Symptoms of an ulcer may
last days, weeks, or months and may subside only to reappear without
cause. Many patients have asymptomatic ulcers.
•Dull, gnawing
pain and a burning sensation in the mid epigastrium or in the back
are characteristic.
•Pain is relieved by eating or taking
alkali; once the stomach has emptied or the alkali wears off, the
pain returns.
•Sharply localized tenderness is elicited by
gentle pressure on the epigastrium or slightly right of the
midline.
•Other symptoms include pyrosis (heartburn) and a
burning sensation in the esophagus and stomach, which moves up to the
mouth, occasionally with sour eructation (burping).
•Vomiting is
rare in uncomplicated duodenal ulcer; it may or may not be preceded by
nausea and usually follows a bout of severe pain and bloating; it is
relieved by ejection of the acid gastric contents.
•Constipation
or diarrhea may result from diet and medications.
•Bleeding (15%
of patients with gastric ulcers) and tarry stools may occur; a small
portion of patients who bleed from an acute ulcer have only very mild
symptoms or none at all.
Assessment and Diagnostic Methods
•Physical
Nursing Assessment
•Assess pain and methods used to relieve it;
take a thorough history, including a 72hour food intake
history.
•If patient has vomited, determine whether emesis is
bright red or coffee ground in appearance. This helps identify source
of the blood.
•Ask patient about usual food habits, alcohol,
smoking, medication use (NSAIDs), and level of tension or
nervousness.
•Ask how patient expresses anger (especially at work
and with family), and determine whether patient is experiencing
occupational stress or family problems.
•Obtain a family history
of ulcer disease.
•Assess vital signs for indicators of anemia
(tachycardia, hypotension).
•Assess for blood in the stools with
an occult blood test.
•Palpate abdomen for localized tenderness.
Nursing Diagnosis
•Acute Pain related to the
effect of gastric acid secretion on damaged tissue
•Anxiety
related to coping with an acute disease
•Imbalanced Nutrition
related to changes in diet
•Deficient Knowledge about preventing
symptoms and managing the condition
Potential Complications
•Hemorrhage: upper
GI
•Perforation
•Penetration
•Pyloric obstruction
(gastric outlet obstruction)
Planning and Goals
•The major goals of the
patient may include relief of pain, reduced anxiety, maintenance of
nutritional requirements, knowledge about the management and
prevention of ulcer recurrence, and absence of complications.
Nursing Interventions
Relieving Pain and Improving
Nutrition
•Administer prescribed medications.
•Avoid
aspirin, which is an anticoagulant, and foods and beverages that
contain acidenhancing caffeine (colas, tea, coffee, chocolate), along
with decaffeinated coffee.
•Encourage patient to eat regularly
spaced meals in a relaxed atmosphere; obtain regular weights and
encourage dietary modifications.
•Encourage relaxation techniques.
Reducing Anxiety
•Assess what patient wants to
know about the disease, and evaluate level of anxiety; encourage
patient to express fears openly and without criticism.
•Explain
diagnostic tests and administering medications on
schedule.
•Interact in a relaxing manner, help in identifying
stressors, and explain effective coping techniques and relaxation methods
Medications
The following drugs are sometimes used to treat peptic ulcers caused by either NSAIDs or H. pylori.
Antacids
Many antacids are available without a prescription,
and they are the first drugs recommended to relieve heartburn and
mild dyspepsia. Antacids are not effective for preventing or healing
ulcers, but they can help in the following ways:
They neutralize
stomach acid with various combinations of three basic compounds --
magnesium, calcium, or aluminum.
They may protect the stomach by
increasing bicarbonate and mucus secretion. (Bicarbonate is an
acid-buffering substance.)
It is generally believed that liquid antacids work faster and are more potent than tablets, although some evidence suggests that both forms work equally well.
Basic Salts Used in Antacids. There are three basic
salts used in antacids:
Magnesium. Magnesium compounds are
available in the form of magnesium carbonate, magnesium trisilicate,
and, most commonly, magnesium hydroxide (Milk of Magnesia). The major
side effect of these magnesium compounds is diarrhea.
Calcium.
Calcium carbonate (Tums, Titralac, and Alka-2) is a potent and
rapid-acting antacid, but it can cause constipation. There have been
rare cases of hypercalcemia (elevated levels of calcium in the blood)
in people taking calcium carbonate for long periods of time.
Hypercalcemia can lead to kidney failure.
Aluminum. The most
common side effect of antacids containing aluminum compounds
(Amphogel, Alternagel) is constipation. Maalox and Mylanta are
combinations of aluminum and magnesium, which balance the side
effects of diarrhea and constipation. People who take large amounts
of antacids containing aluminum may be at risk for calcium loss and
osteoporosis. Long-term use also increases the risk of kidney stones.
People who have recently experienced GI bleeding should not use
aluminum compounds.
Interactions with Other Drugs. Antacids can reduce the
absorption of a number of drugs. Conversely, some antacids increase
the potency of certain drugs. The interactions can be avoided by
taking other drugs 1 hour before or 3 hours after taking the
antacid.
Table 1:Drug Interactions with Antacids (such as
Maalox, Mylanta)
Antibiotics
H. pylori is usually highly sensitive
Bismuth
Compounds that contain bismuth are often used in the three-drug treatment programs. They destroy the cell walls of H. pylori bacteria. The only bismuth compound available in the U.S. has been bismuth subsalicylate (Pepto-Bismol), although a drug combination of the H2 blocker ranitidine and bismuth citrate (Tritec) has been released. High doses can cause vomiting and depression of the central nervous system, but the doses given for ulcer patients rarely cause side effects.
Proton Pump Inhibitors (PPIs)
Actions against ulcers. PPIs are the drugs of choice for managing patients with peptic ulcers, regardless of the cause. They suppress the production of stomach acid by blocking the gastric acid pump -- the molecule in the stomach glands that is responsible for acid secretion.
PPIs can be used either as part of a multidrug regimen for H. pylori, or alone for preventing and healing NSAID-caused ulcers. They are also useful for treating ulcers caused by Zollinger-Ellison syndrome. They are considered to be more effective than H2 blockers.
Some people carry a gene that reduces the effectiveness of PPIs. This gene is present in 18 - 20% of people of Asian descent.
Standard Brands. Most PPIs are available by
prescription as oral drugs. There is no evidence that one brand of
PPI works better than another. Brands approved for ulcer prevention
and treatment include:
Omeprazole (generic, Prilosec
OTC)
Esomeprazole (Nexium)
Lansoprazole
(Prevacid)
Rabeprazole (Aciphex)
Possible Adverse Effects.
Side effects are
uncommon, but may include headache, diarrhea, constipation, nausea,
and itching.
Pregnant women and nursing mothers should avoid
taking PPIs. Although recent studies suggest that these drugs do not
increase the risk of birth defects, their safety during pregnancy is
not yet proven.
PPIs may interact with certain drugs, including
antiseizure medications (such as phenytoin), anti-anxiety drugs (such
as diazepam), and blood thinners (such as warfarin).
Long-term
use of high-dose PPIs may produce vitamin B12 deficiency, but more
studies are needed to confirm this risk.
In theory, long-term use of PPIs by people with H. pylori may reduce acid secretion enough to cause atrophic gastritis (ch
Indications and Usage for Piroxicam
Carefully consider the potential benefits and risks of Piroxicam capsule, USP and other treatment options before deciding to use Piroxicam capsule, USP. Use the lowest effective dose for the shortest duration consistent with individual patient treatment goals (see WARNINGS).
Piroxicam capsule, USP is indicated:
• For
relief of the signs and symptoms of osteoarthritis.
• For relief
of the signs and symptoms of rheumatoid arthritis.
Contraindications
Piroxicam capsule, USP is contraindicated in patients with known hypersensitivity to Piroxicam.
Piroxicam capsule, USP should not be given to patients who have experienced asthma, urticaria, or allergic-type reactions after taking aspirin or other NSAIDs. Severe, rarely fatal, anaphylactic-like reactions to NSAIDs have been reported in such patients (see WARNINGS: Anaphylactoid Reactions and PRECAUTIONS: Preexisting Asthma).
Piroxicam capsule, USP is contraindicated for the
treatment of peri-operative pain in the setting of coronary artery
bypass graft (CABG) surgery (see WARNINGS).
CARDIOVASCULAR EFFECTS
Cardiovascular
Thrombotic Events
Clinical trials of several COX-2 selective and nonselective NSAIDs of up to three years duration have shown an increased risk of serious cardiovascular (CV) thrombotic events, myocardial infarction, and stroke, which can be fatal. All NSAIDs, both COX-2 selective and nonselective, may have a similar risk. Patients with known CV disease or risk factors for CV disease may be at greater risk. To minimize the potential risk for an adverse CV event in patients treated with an NSAID, the lowest effective dose should be used for the shortest duration possible. Physicians and patients should remain alert for the development of such events, even in the absence of previous CV symptoms. Patients should be informed about the signs and/or symptoms of serious CV events and the steps to take if they occur.
There is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious CV thrombotic events associated with NSAID use. The conc
LABORATORY TESTS
Because serious GI tract ulcerations and bleeding can
occur without warning symptoms, physicians should monitor for signs
and symptoms of GI bleeding. Patients on long-term treatment with
NSAIDs should have their CBC and a chemistry profile checked
periodically. If clinical signs and symptoms consistent with liver or
renal disease develop, systemic manifestations occur (e.g.,
eosinophilia, rash, etc.), or if abnormal liver tests persist or
worsen, Piroxicam capsule, USP should be discontinued.
Drug Interactions
Highly Protein Bound Drugs: Piroxicam is highly protein bound and, therefore, might be expected to displace other protein bound drugs. Physicians should closely monitor patients for a change in dosage requirements when administering Piroxicam capsule, USP to patients on other highly protein bound drugs.
Aspirin: When Piroxicam is administered with aspirin, its protein binding is reduced, although the clearance of free Piroxicam is not altered. Plasma levels of Piroxicam are depressed to approximately 80% of their normal values when Piroxicam capsule, USP is administered (20 mg/day) in conjunction with aspirin (3900 mg/day). The clinical significance of this interaction is not known; however, as with other NSAIDs, concomitant administration of Piroxicam and aspirin is not generally recommended because of the potential for increased adverse effects.
Methotrexate: NSAIDs have been reported to competitively inhibit methotrexate accumulation in rabbit kidney slices. This may indicate that they could enhance the toxicity of methotrexate. Caution should be used when NSAIDs are administered concomitantly with methotrexate.
ACE-Inhibitors: Reports suggest that NSAIDs may diminish the antihypertensive effect of ACE-inhibitors. This interaction should be given consideration in patients taking NSAIDs concomitantly with ACE-inhibitors.
In patients who are elderly, volume-depleted (including those on diuretic therapy), or with compromised renal function, co-administration of NSAIDs, including selective COX-2 inhibitors, with ACE inhibitors, may result in deterioration of renal function, including possible acute renal failure. These effects are usually reversible.
Diuretics: Clinical studies, as well as postmarketing observ
Some severe symptoms include:
•Dark-stained vomitus
•Vomiting dark and clotted
blood
•Black tarry stools
•Pale skin due to
anemia
•Weight loss
•Abdominal pain
•Loss of appetite
The signs and symptoms of a duodenal ulcer are almost opposite to the signs and symptoms of gastric ulcers - the differences are noticed mainly in the timing and extent of the pain. Duodenal ulcers develop in the first part of the small intestine, called the duodenum.
Check out the following symptoms to see if you possibly have a duodenal ulcer;
• Heartburn/GERD is a one of the most noticeable signs
of a duodenal ulcer.
• You will also feel a burning or gnawing
sensation in the top of your stomach.
• The symptoms of a
duodenal ulcer are felt mostly before a meal. This happens when
excess acid produced by hunger stimulation, is passed into the
duodenum.
• Pain will be felt after taking aspirin or drinking
orange juice or coffee.
• Another symptom of a duodenal ulcer is
that about 5 in every 10 people are woken from their sleep during the
night by sharp ulcer pains.
• With duodenal ulcers, taking a
meal or an antacid usually results in a decrease in pain levels
Common Muscle Relaxant Medications
Muscle relaxants usually used to treat back pain and
other types of pain include:
•Baclofen
Muscle tightness
and muscle spasms, including those related to spine injuries, are
eased with baclofen. The medication may be helpful in treating
multiple sclerosis and stabbing nerve pain. It is available as a
tablet and can be taken by children as young as 12 years old. Some
common side effects could include nausea and vomiting, confusion,
drowsiness, headache, or muscle weakness. Baclofen is rated C in the
FDA’s A through X pregnancy safety ranking for medications, with A
being the safest.
•Chlorzoxazone (Lorzone, Parafon Forte DSC)
Chlorzoxazone is used for the relief of discomfort from acute,
painful, musculoskeletal conditions. It should not be used in
patients with hypersensitivity to chlorzoxazone and rare liver
toxicity has been reported. The doctor should be contacted in case of
loss of appetite; nausea, vomiting, or tiredness; stomach pain; dark
urine; pale stools; or yellowing of the skin or eyes. Chlorzoxazone
is available as a tablet. It has not been rated by the FDA for safety
during pregnancy.
•Carisoprodol (Soma)
Carisoprodol relaxes
muscles and eases pain and stiffness caused by acute bone and muscle
problems, as may be caused by an injury. It can be habit-forming,
particularly if used in conjunction with alcohol or other drugs that
have a sedative effect. Patients with a history of acute intermittent
porphyria or hypersensitivity to carbamate medications such as
methocarbamol should avoid carisoprodol. It is taken by mouth in
tablet form and is also available in combination with aspirin or
aspirin and codeine. It is rated C in the FDA’s pregnancy safety
ranking for medications.
•Cyclobenzaprine (e.g. Amrix, Cyclobenzaprine Comfort Pac
Fexmid, FlexePax, Flexeril, FusePaq Tabradol,
Therabenzaprine-60)
Cyclobenzaprine eases
stiffness and pain from muscle cramps, also called spasms. It is not
advised for those with an overactive thyroid, heart rhythm problems,
heart failure, or those who have had a heart attack recently. It can
be used on a longer-term basis and has a chemical structure related
to some ant
What's the best way to pick up an object?
•Use slow and smooth movements. Hurried, jerky
movements can strain the muscles in your back.
•Keep your body
facing the object while you lift it. Twisting while lifting can hurt
your back.
•Keep the load close to your body. Having to reach
out to lift and carry an object may hurt your
back.
•"Lifting with your legs" should be done only
when you can straddle the load. To lift with your legs, bend your
knees, not your back, to pick up the load. Keep your back
straight.
•Try to carry the load in the space between your
shoulder and your waist. This puts less strain on your back muscles.
How can I avoid back injuries?
•Warm up. Stretch your legs and your back before
lifting anything.
•Pace yourself. Take many small breaks between
lifts if you are lifting a number of things.
•Don't overdo
it--don't try to lift something too heavy for you. If you have to
strain to carry the load, it's too heavy.
•Make sure you have
enough room to lift safely. Clear a space around the object before
lifting it.
•Look around before you lift, and look around as you
carry. Make sure you can see where you are walking. Know where you
are going to put down the load.
•Avoid walking on slippery,
uneven surfaces while carrying something.
•Don't rely on a back
belt to protect you. It hasn't been proven that back belts can
protect you from back injury.
•Get help before you try to lift a
heavy load. Use a dolly or a forklift if you can.
Since celecoxib is taken as needed, you may not be on a dosing schedule. If you are taking the medication regularly, take the missed dose as soon as you remember. Skip the missed dose if it is almost time for your next scheduled dose. Do not take extra medicine to make up the missed dose
Overdose symptoms may include nausea, vomiting, stomach pain, drowsiness, black or bloody stools, coughing up blood, shallow breathing, fainting, or coma.
What should I avoid while taking celecoxib (Celebrex)?
Avoid drinking alcohol. It may increase your risk of stomach bleeding.
Avoid taking celecoxib together with other NSAIDs such as ibuprofen (Motrin, Advil), naproxen (Aleve, Naprosyn, Naprelan, Treximet), diclofenac (Arthrotec, Cambia, Cataflam, Voltaren, Flector Patch, Pennsaid, Solareze), diflunisal (Dolobid), etodolac (Lodine), flurbiprofen (Ansaid), indomethacin (Indocin), ketoprofen (Orudis), ketorolac (Toradol), mefenamic acid (Ponstel), meloxicam (Mobic), nabumetone (Relafen), or piroxicam (Feldene).
Ask a doctor or pharmacist before using any other cold, allergy, or pain medicine. Medicines similar to celecoxib are contained in many combination medicines. Taking certain products together can cause you to get too much of a certain type of drug Check the label to see if a medicine contains an NSAID (non-steroidal anti-inflammatory drug) such as aspirin, ibuprofen, ketoprofen, or naproxen.
Avoid exposure to sunlight or tanning beds. Celecoxib can make you sunburn more easily. Wear protective clothing and use sunscreen (SPF 30 or higher) when you are outdoors.
What other drugs will affect celecoxib (Celebrex)?
Ask your doctor before using an antidepressant such as citalopram (Celexa), escitalopram (Lexapro), fluoxetine (Prozac, Sarafem, Symbyax), fluvoxamine (Luvox), paroxetine (Paxil), or sertraline (Zoloft). Taking any of these medicines with an NSAID may cause you to bruise or bleed easily.
Tell your doctor about all other medicines you use, especially:
Piroxicam is used to relieve pain, tenderness, swelling, and stiffness caused by osteoarthritis (arthritis caused by a breakdown of the lining of the joints) and rheumatoid arthritis (arthritis caused by swelling of the lining of the joints). Piroxicam is in a class of medications called NSAIDs. It works by stopping the body's production of a substance that causes pain, fever, and inflammation.
Piroxicam comes as a capsule to take by mouth. It is usually taken once or twice a day. Take piroxicam at around the same time(s) every day. Follow the directions on your prescription label carefully, and ask your doctor or pharmacist to explain any part you do not understand. Take piroxicam exactly as directed. Do not take more or less of it or take it more often than prescribed by your doctor.
Piroxicam will help control your symptoms but will not cure your condition. It may take 8 to 12 weeks or longer before you feel the full benefit of piroxicam.
Piroxicam is also sometimes used to treat gouty arthritis (attacks of severe joint pain and swelling caused by a build-up of certain substances in the joints) and ankylosing spondylitis (arthritis that mainly affects the spine). It is also sometimes used to relieve muscle pain and swelling, menstrual pain, and pain after surgery or childbirth. Talk to your doctor about the risks of using this medication for your condition.
•tell your doctor and pharmacist if you are allergic to
piroxicam, aspirin,or other NSAIDs such as ibuprofen (Advil, Motrin)
and naproxen (Aleve, Naprosyn), or any other medications.
•tell
your doctor and pharmacist what prescription and nonprescription
medications, vitamins, nutritional supplements, and herbal products
you are taking or plan to take. Be sure to mention the medications
listed in the
IMPORTANT WARNING section and any of the following:
angiotensin-converting enzyme (ACE) inhibitors such as benazepril
(Lotensin), captopril (Capoten), enalapril (Vasotec), fosinopril (Monopril)
CHOLECYSTITIS WITH CHOLELITHIASIS
2.Cholecystitis is an acute or chronic inflammation of the gallbladder, usually associated with gallstone(s) impacted in the cystic duct, causing distension of the gallbladder.
3. Stones (calculi) are made up of cholesterol, calcium bilirubinate, or a mixture caused by changes in the bile composition. Gallstones can develop in the common bile duct, the cystic duct, hepatic duct, small bile duct, and pancreatic duct.
4.Crystals can also form in the submucosa of the gallbladder causing widespread inflammation. Acute cholecystitis with cholelithiasis is usually treated by surgery, although several other treatment methods (fragmentation and dissolution of stones) are now being used.
5.CARE SETTING Severe acute attacks may require brief hospitalization on a medical unit. This plan of care deals with the acutely ill, hospitalized patient.
6.RELATED CONCERNS Cholecystectomy Fluid and electrolyte imbalances,Psychosocial aspects of care Total nutritional support: parenteral/enteral feeding Patient Assessment Database
7.ACTIVITY/REST May report: Fatigue May exhibit: Restlessness
8 .CIRCULATION May exhibit: Tachycardia, diaphoresis, lightheadedness
9.ELIMINATION May report: Change in color of urine and stools May exhibit: Abdominal distension Palpable mass in right upper quadrant (RUQ) Dark, concentrated urine Clay-colored stool, steatorrhea
10.FOOD/FLUID May report: Anorexia, nausea/vomiting Intolerance of fatty and “gas-forming” foods; recurrent regurgitation, heartburn, indigestion, flatulence, bloating (dyspepsia) Belching (eructation) May exhibit: Obesity; recent weight loss Normal to hypoactive bowel sounds
11. PAIN/DISCOMFORT May report: Severe epigastric and right upper abdominal pain, may radiate to mid-back, right shoulder/scapula, or t
16.ACTIONS/INTERVENTIONS RATIONALE Pain Management (NIC)
Collaborative Maintain NPO status, insert/maintain NG suction as
Removes gastric secretions that stimulate release of indicated.
cholecystokinin and gallbladder contractions. Administer medications
as indicated: Anticholinergics, e.g., atropine, propantheline (Pro-
Relieves reflex spasm/smooth muscle contraction and Banthı-ne);
assists with pain management. Sedatives, e.g., phenobarbital; Promotes
rest and relaxes smooth muscle, relieving pain. Narcotics, e.g.,
meperidine hydrochloride (Demerol), Given to reduce severe pain.
Morphine is used with caution morphine sulfate; because it may
increase spasms of the sphincter of Oddi, although nitroglycerin may
be given to reduce morphine- induced spasms if they occur. Monoctanoin
(Moctanin); This medication may be used after a cholecystectomy for
retained stones or for newly formed large stones in the bile duct. It
is a lengthy treatment (1–3 wk) and is administered via a
nasal-biliary tube.
17. A cholangiogram is done periodically to
monitor stone dissolution. Smooth muscle relaxants, e.g., papaverine
(Pavabid), Relieves ductal spasm. nitroglycerin, amyl nitrite;
Chenodeoxycholic acid (Chenix), ursodeoxycholic
18.These natural bile acids decrease cholesterol synthesis, acid (Urso, Actigall); dissolving gallstones. Success of this treatment depends on the number and size of gallstones (preferably three or fewer stones smaller than 20 min in diameter) floating in a functioning gallbladder. Antibiotics. To treat infectious process, reducing inflammation.
19.Prepare for procedures, e.g.: Endoscopic papillotomy (removal of ductal stone); Choice of procedure is dictated by individual situation. Extracorporeal shock wave lithotripsy (ESWL); Shock wave treatment is indicated when patient has mild or moderate symptoms, cholesterol stones in gallbladder are 0.5 mm or larger, and there is no biliary tract obstruction. Depending on the machine being used, the patient may sit in a tank of water or lie prone on a water-filled cushion.
20.Treatment takes about 1–2 hr and is 75%–95% successful.
21.Note: This procedure is contraindicated in patients with pacemakers or implantable defibrillators. Procedure done to widen the mouth of the common bile Endoscopic sphincterotomy; duct where it empties into the duo
Right upper quadrant:organs
Liver
Gall bladder with biliary
tree
Duodenum
Head of pancreas
Right kidney and adrenal
gland
Hepatic flexure of colon
Describe the steps of percussing the abdomen.
1. Percuss to determine the borders of the liver and
spleen.
2. use indirect fist percussion to assess for
costovertebral angle tenderness.
3. If ascites is suspected,
use percussion to test for a fluid wave or for shifting dullness.
What is the predominant sound across the abdomen when percussed?
Tympany
What sound will be heard over a distended bladder, adipose tissue, fluid or a mass?
Dullness
Describe the steps of palpating the abdomen.
Palpate to judge the size, location, and consistency of certain
organs to screen for abnormal mass or tenderness.
1. Begin with
light palpation to form an overall impression of the skin surface and
superficial musculature, note guarding.
2. Perform deep
palpation, pushing down about 5-8 cm. If you detect a mass, note its
location, size, shape, consistency, surface, mobility, pulsatility and
tenderness.
3. Palpate for the liver in the right upper quadrant, the
spleen in the left upper quadrant, the kidneys in both flanks, and
the aorta just left of midline.
4. If needed assess for rebound tenderness or inspiratory
arrest or perform the iliopsoas muscle test.
-- Lie the patient supine (as you would during any other abdominal
assessment);
-- Instruct the patient to breath out;
--
Place your palpating hand just below the costal margin, approximately
mid-clavicularly (this is just above the gallbladder);
-Then
instruct the patient to slowly breath in;
A positive Murphy’s sign is identified when the patient stops breathing in due to pain -- this is caused by the move of the diaphragm pushing the inflamed gallbladder into the palpating hand.
A negative Murphy’s sign is identified when the patient comfortable breaths all the way in without any pain -- in this case, the diaphragm pushes the non-inflamed gallbladder into the palpating hand with nil changes in the patient’s level of comfort.
A positive Murphy’s sign often indicates Cholycystitis, where as a negative Murphy’s sign may suggest pyelonephritis, and ascending cholangitis.
To assess the abdomen for Murphy’s sign:
The abdominal wall is compressed slowly and then rapidly released. A positive sign is indicated by presence of pain upon removal of pressure on the abdominal wall. It is very similar to rebound tenderness and might be regarded by some authors as the same thing, or at least a particular application of it.
It represents aggravation of the parietal layer of peritoneum by stretching or moving.
Positive Blumberg sign or rebound tenderness is indicative of peritonitis which can occur in diseases like appendicitis, and may occur in ulcerative colitis with rebound tenderness in the right lower quadrant. This method is specially useful in diagnosing appendicitis requiring urgent management.
However, in recent years the value of rebound tenderness has been questioned, since it may not add any diagnostic value beyond the observation that the patient has severe tenderness
Blumberg sign or rebound tenderness
This anomaly occurs because the pain nerves deep in the intestines do not localize well to an exact spot on the abdominal wall, unlike pain nerves in muscles. Pain from a stomach ulcer or gallstone can be interpreted by the brain as pain from the stomach, liver, gall bladder, duodenum, or first part of the small intestine. It will "refer" pain often to the mid upper abdomen.
Because the appendix is a piece of intestine, it follows a similar referral pattern. An appendix with some early inflammation may give a non-specific irritation somewhere near the umbilicus (belly button). Should the inflammation become severe, it may actually irritate the inner lining of the abdominal cavity called the peritoneum. This thin layer lies under or behind the abdominal wall muscles. Now the pain is "localized". If pressure is applied to the muscles of the right lower abdomen (or iliac fossa) near a very irritated appendix, then the muscle fibers in that area will be stretched and will hurt.
Rovsing's sign, named after the Danish surgeon Niels Thorkild Rovsing (1862 -1927),is a sign of appendicitis. If palpation of the left lower quadrant of a person's abdomen increases the pain felt in the right lower quadrant, the patient is said to have a positive Rovsing's sign and may have appendicitis.
In acute appendicitis, palpation in the left iliac fossa may produce pain in the right iliac fossa.
• Liver function tests (LFTs), which are blood tests that
can show evidence of gallbladder disease.
•A check of the blood's amylase or lipase levels to look for
inflammation of the pancreas. Amylase and lipase are enzymes
(digestive chemicals) produced in the pancreas.
•A complete blood
count (CBC), which looks at levels of different types of blood cells
such as white blood cells. A high white blood cell count may indicate
infection.
•The use of ultrasound testing which uses sound waves
to image and make a picture of the intra-abdominal organs including
the gallbladder.
•An abdominal X-ray, which may show evidence of
gallbladder disease, such as gallstones.
•A computed tomography
(CT) scan constructs a detailed X-ray images of the abdominal
organs.
•A HIDA scan. In this test, a radioactive material called
hydroxy iminodiacetic acid (HIDA) is injected into the patient. The
radioactive material is taken up by the gallbladder to measure
gallbladder emptying function. This test also is referred to as
cholescintigraphy.
•Magnetic resonance cholangiopancreatography
(MRCP), which uses magnetic resonance imaging (MRI) to produce
detailed pictures.
•Endoscopic retrograde
cholangiopancreatography (ERCP), a procedure in which a tube is placed
down the patient's throat, into the stomach, then into the small
intestine. Dye is injected and the ducts of the gallbladder, liver,
and pancreas can be seen on X-ray.
Gallbladder problems are diagnosed through various tests. These may include:
Symptoms of bile duct obstruction include the following:
•Upper
right side abdominal pain
•Nausea or
vomiting
•Sweating/chills
•Fever
•Dark urine
•Loss
of appetite (inappetance)
•Weight loss
•Pale stools
•Greasy stool
•Yellow eyes
•Yellowish skin or jaundice
Symptoms and Signs of Bile Duct Obstruction
The following blood test results could be due to a possible
blockage:
Increased bilirubin level
Increased alkaline phosphatase level
Increased liver enzymes
The following tests may be used to investigate a possible
blocked bile duct:
Abdominal ultrasound
Abdominal CT scan
ERCP (endoscopic retrograde
cholangiopancreatography)
Percutaneous transhepatic cholangiogram
(PTCA)
Magnetic resonance cholangiopancreatography (MRCP)
A blocked bile duct may also alter the results of the
following tests:
Amylase blood test
Gallbladder radionuclide scan
Lipase blood test
Prothrombin time (PT)
Urine bilirubin
The goal of treatment is to reli
There are two types of cholecystitis:
• Acute cholecystitis is the sudden inflammation of the gallbladder that causes marked abdominal pain, often with nausea, vomiting, and fever.
• Chronic cholecystitis is a lower intensity inflammation of the gallbladder that lasts a long time. It may be caused by repeat attacks of acute cholecystitis. Chronic cholecystitis may cause intermittent mild abdominal pain, or no symptoms at all. Damage to the walls of the gallbladder leads to a thickened, scarred gallbladder. Ultimately, the gallbladder can shrink and lose its ability to store and release bile.
Gallstones alone can cause episodes of crampy abdominal pain without any infection. This is called biliary colic.
Women are more likely than men to get gallstones. The risk of gallstones also is higher in:
•Anyone older than age 60
•Women who are pregnant or have had several pregnancies
•Women who take estrogen replacement therapy or birth control pills
•Obese people
•People who have lost weight rapidly
•People who eat a high-fat diet
1.Lower respiratory tract infections, including pneumonia and
bronchitis as an exacerbation of COPD (chronic obstructive pulmonary
disease) caused by Streptococcus pneumoniae and Haemophilus
influenzae.
2.
Intra-abdominal infections, including acute gangrenous or
perforated appendicitis and appendicitis with peritonitis, caused
by Group D streptococcus including Enterococcus faecalis*;
Streptococcus viridans group*; Escherichia coli; Klebsiella
pneumoniae*; Pseudomonas aeruginosa*; Bacteroides species
including B. fragilis, B. distasonis*, B. intermedius* and B.
thetaiotaomicron*; Fusobacterium species; and Peptostreptococcus*
species.
3.Skin and skin structure infections,
including abscesses, cellulitis, infected skin ulcers and wound
infections caused by Staphylococcus aureus including
penicillinase-producing strains; Streptococcus pyogenes*; Group D
streptococcus including Enterococcus faecalis; Acinetobacter species*
including A. calcoaceticus*; Citrobacter species*; Escherichia coli;
Enterobacter cloacae; Klebsiella pneumoniae*; Pseudomonas aeruginosa*;
and Bacteroides species* including B. fragilis*.
4. Gynecologic
infections, including postpartum endomyometritis, caused by Group D
streptococcus including Enterococcus faecalis*; Escherichia coli;
Klebsiella pneumoniae*; Bacteroides intermedius*; and
Peptostreptococcus species*.
As with other beta-lactam antibiotics, some strains of Pseudomonas aeruginosa may develop resistance fairly rapidly during treatment with PRIMAXIN I.M. During therapy of Pseudomonas aeruginosa infections, periodic susceptibility testing should be done when clinically appropriate.
To reduce the development of drug-resistant bacteria and maintain the effectiveness of PRIMAXIN I.M. and other antibacterial drugs, PRIMAXIN I.M. should be used only to treat or prevent infections that are proven or strongly suspected to be caused by susceptible bacteria. When culture and susceptibility information are available, they should be considered in selecting or modifying antibacterial therapy. In the absence of such data, local epidemiology and susceptibility patterns may contribute to the empiric selection of therapy.
PRIMAXIN I.M. is indicated for the treatment of serious infections (listed below) of mild to moderate severity for which intramuscular therapy is appropriate. PRIMAXIN I.M. is not intended for the therapy of severe or life-threatening infections, including bacterial sepsis or endocarditis, or in instances of major physiological impairments such as shock.
PRIMAXIN I.M. is indicated for the treatment of infections caused by susceptible strains of the designated microorganisms in the conditions listed below:
Hydrocolloid dressings do not need to be changed as often as other types of wound dressings. New dressing only needs to be applied every 3-7 days, which leaves the wound undisturbed longer. This also makes the hydrocolloid dressings more cost effective, not only in terms of materials, but by reducing the cost of service provided by a health care professional. Hydrocolloid dressings also reduce pain and promote faster healing. When compared to paraffin gauze to dress skin graft donor sites, hydrocolloid dressings may result in less pain and faster healing. A study of patients with lacerations and shallow surgical incisions found patients who used hydrocolloid dressings required less analgesia to perform daily activities.
Impermeable to Bacteria
Hydrocolloid dressings significantly lower the risk of infection because they are impermeable to bacteria. Most are water proof, allowing patients to proceed with normal bathing. An 8-week study was performed on bacteria found in venous ulcers to which occlusive hydrocolloid dressing was applied. The study found that the level of bacteria was generally stable. Most species that were observed remained, apart from pseudomonas which appeared to be repressed by the hydrocolloid dressing. Bacteria were found present in 12 of the 20 ulcers examined, but there was no evidence that any species deterred healing.
Adheres Only to Intact Skin
Hydrocolloid dressings do not adhere to the wound, only to the skin surrounding it. This helps keep newly healed skin intact. Moisture is generated beneath the dressing to promote healing and prevent break down of tissue. In addition, hydrocolloid dressings do not traumatize the skin upon being removed. They are also available in contoured shapes to form with specific body parts.
Simple to Apply
Applying hydrocolloid dressing to a wound is simple. Before applying the dressing, wash your hands and put on clean gloves. Clean the wound and use clean gauze to dab the area around the wound until it is as dry as it can get. Remove the gloves once again, wash your hands and put on a clean pair of gloves. Administer a film of moisture barrier around the wound and apply filler if the wound is deep. Allow the hydrocolloid dressing to warm between your hands for a few minutes before applying it. Once you have removed the paper from the back, place the dr
Hydrocolloid dressings
Electrolytes
See the list below:
•Ammonia: 15-50 µmol/L
•Ceruloplasmin: 15-60 mg/dL
•Chloride: 95-105 mmol/L
•Copper: 70-150 µg/dL
•Creatinine: 0.8-1.3 mg/dL
•Blood urea nitrogen: 8-21 mg/dL
•Ferritin: 12-300 ng/mL (men), 12-150 ng/mL (women)
•Glucose: 65-110 mg/dL
•Inorganic phosphorous: 1-1.5 mmol/L
•Ionized calcium: 1.03-1.23 mmol/L
•Magnesium: 1.5-2 mEq/L
•Phosphate: 0.8-1.5 mmol/L
•Potassium: 3.5-5 mmol/L
•Pyruvate: 300-900 µg/dL
•Sodium: 135-145 mmol/L
•Total calcium: 2-2.6 mmol/L
•Total iron-binding capacity: 45-85 µmol/L
•Total serum iron: 65-180 µg/dL (men), 30-170 µg/dL (women)
•Transferrin: 200-350 mg/dL
•Urea: 1.2-3 mmol/L
•Uric acid: 0.18-0.48 mmol/L
•Zinc: 70-100 µmol/L
Hematology
See the list below:
•Hemoglobin: 13-17 g/dL (men), 12-15 g/dL (women)
•Hematocrit 40%-52% (men), 36%-47%
•Glycosylated hemoglobin 4%-6%
•Mean corpuscular volume (MCV): 80-100 fL
•Red blood cell distribution width (RDW): 11.5%-14.5%
•Mean corpuscular hemoglobin (MCH): 0.4-0.5 fmol/cell
•Mean corpuscular hemoglobin concentration (MCHC): 30-35 g/dL
•Reticulocytes 0.5%-1.5%
•White blood cells (WBC) 4-10 x 10^9/L
•Neutrophils: 2-8 x 10^9/L
•Bands: < 1 x 10^9/L
•Lymphocytes: 1-4 x 10^9/L
•Monocytes: 0.2-0.8 x 10^9/L
•Eosinophils: < 0.5 x 10^9/L
•Platelets: 150-400 x 10^9/L
•Prothrombin time: 11-14 sec
•International normalized ratio (INR): 0.9-1.2
•Activated partial thromboplastin time (aPTT): 20-40 sec
•Fibrinogen: 1.8-4 g/L
•Bleeding time: 2-9 min
Lipids
See the list below:
•Triglycerides: 50-150 mg/dL
•Total cholesterol: 3-5.5 mmol/L
•High-density lipoprotein (HDL): 40-80 mg/dL
•Low-density lipoprotein (LDL): 85-125 mg/dL
Acid base
See the list below:
•pH: 7.35-7.45
•Base excess: (-3)-(+3)
•H+: 36-44 nmol/L
•Partial pressure of oxygen (pO2): 75-100 mm Hg
•Oxygen saturation: 96%-100%
•Partial pressure of carbon dioxide (pCO2): 35-45 mm Hg
•Bicarbonate (HCO3): 18-22 mmol/L
Gastrointestinal function
See the list below:
•Albumin: 35-50 g/L
•Alkaline phosphatase: 50-100 U/L
•Alanine aminotransferase (ALT): 5-30 U/L
•Amylase: 30-125 U/L
•Aspartate aminotransferase (AST): 5-30 U/L
•Direct bilirubin: 0-6 µmol/L
•Gamma glutamyl transferase: 6-50 U/L
•Lipase: 10-150 U/L
•Total bilirubin: 2-20 µmol/L
•Total protein: 60-80 g/L
Cardiac enzymes
See the list below:
•Creatine kinase: 25-200 U/L
•Creatine kinase MB (CKMB): 0-4 ng/mL
•Troponin: 0-0.4 ng/mL
Hormones
See the list below:
•17 hydroxyprogesterone (female, follicular): 0.2-1 mg/L
•Adrenocorticotropic hormone (ACTH): 4.5-20 pmol/L
•Estradiol: 1.5-5 ng/dL (male), 2-14 ng/dL (female, follicular), 2-16 ng/dL (female, luteal), < 3.5 ng/dL (postmenopausal)
•Free T3: 0.2-0.5 ng/dL
•Free T4: 10-20 pmol/L
•Follicle-stimulating hormone (FSH): 1-10 IU/L (male), 1-10 IU/L (female, follicular/luteal), 5-25 IU/L (female, ovulation), 30-110 IU/L (postmenopause)
•Growth hormone (fasting) : 0-5 ng/mL
•Progesterone: 70-280 (ovulation), ng/dL
•Prolactin: < 14 ng/mL
•Testosterone (male): 10-25 nmol/L
•Thyroxine-binding globulin: 12-30 mg/L
•Thyroid-stimulating hormone (TSH): 0.5-5 mIU/L
•Total T4: 4.9-11.7 mg/dL
•Total T3: 0.7-1.5 ng/dL
•Free T3: 0.6-1.6 ng/mL
Vitamins
See the list below:
•Folate (serum) : 7-36 nmol/L
•Vitamin A: 30-65 µg/dL
•Vitamin B12: 130-700 ng/L
•Vitamin C: 0.4-1.5 mg/dL
•Vitamin D: 5-75 ng/mL
Laparoscopic Cholecystectomy Discharge Instructions
You will most likely tire easily for about 1-2 weeks. This is normal. Plan to take rest periods throughout each day as you feel you need them. Occasionally patients may have trouble with bowel movements for up to a month after surgery; constipation may be relieved by increasing fluid intake or taking a stool softener or mild laxative, diarrhea should subside within a few weeks. Generally patients find they are back to their usual routine within 1-2 weeks after surgery and fully recovered within a month.
Medication
Acetaminophen (Tylenol) regular or extra strength 1-2 tablets every 4-6 hours as needed for mild pain.
Vicodin (Acetaminophen with Codeine)(prescription only) as directed for moderate pain.
Over the counter stool softener or laxative daily as needed for constipation.
Diet
Try to drink 8-10 glasses per day Juice or water).
For the first few days, you may eat whatever was easy to digest before surgery and then progress to a normal diet as tolerated.
Bathing Showering
You may shower/bathe 24 hours after surgery.
You may use a mild soap to gently cleanse your incision and carefully pat dry.
Activities at Home
Gradually increase your activity. Take rest periods as needed.
Get adequate amounts of sleep each night.
Avoid heavy lifting (> 20 Ibs.) or strenuous activity for 1 week or as directed by your physician.
Avoid contact sports. Perform lighter aerobic exercise a few days after surgery (e.g. walking, biking, swimming, golfing, jogging etc.).
Use common sense – if it hurts, don’t do it.
Driving
You may resume driving when you no longer take narcotic pain medications.
Care of Incision
Brace your incisions with a small pillow when coughing and/or sneezing.
You may cover your incisions with loose sterile gauze or Band-Aids to reduce irritation that may occur from contact with clothing.
Watch for the following signs and symptoms and notify our
office if these occur:
•Temperature over 101.OF
•Drainage from wound
•Increasing swelling, redness or tenderness of the
wound
•Increased pain in the abdomen
•Persistent nausea and/or vomiting
Coronary heart disease is mainly caused by the process of atherosclerosis which is a degenerative disorder. Coronary heart disease is the imbalance between myocardial oxygen supply needs.
Coronary heart disease occurs due to:
•Narrowing of the
coronary arteries
•Decreased blood flow / cardiac
output
•The increase in myocardial oxygen demand
•Coronary
artery spasm
Main causes of atherosclerosis. Although influenced by many factors, due to degenerative disorder, it often causes sudden death and attacked very productive age.
Input to the oxygen demand imbalance, namely:
1.Hypoxemia (ischemia), caused by vascular
disorders (coronary arteries). On ischemic vascular abnormalities that
are reduced tissue perfusion to metabolic elimination caused by (eg
lactic acid) decreased as well, so it will be faster symptoms
appear.
2.Hypoxia (anoxia), caused by lack of
oxygen in the blood. Actual input of oxygen to the myocardium depends
on the oxygen in the blood and the coronary arteries. Oxygen in the
blood depends on the oxygen can be taken up by the blood. So
influenced by Hb, lungs and oxygen in the breathing air.
Palpitations are manifestations of coronary heart disease although not specific. Manifestations of coronary heart disease varies depending on the degree of coronary artery blood flow. When coronary flow is still sufficient for the tissue will not cause any complaints / clinical manifestations. Factors that affect large and coronary flow properties such as the state of anatomical and mechanical factors, autoregulation system and peripheral resistance.
The trigger factor that adds to ischemia such as, physical activity, stress, etc.. Angina pectoris is the main symptom specific and typical for coronary heart disease. Shortness of breath began to feel short of breath while doing activities that are sufficiently severe, increasing shortness of breath. At a more advanced state of heart failure can occur.
1. Nursing Diagnosis : Acute Pain related to heart tissue ischemia, or blockages in the coronary arteries.
Objective: The client is expected to be able to demonstrate a decrease in chest pain, showed a decrease in pressure and how relaxation.
Interventions:
•Monitor and review the characteristics and
location of pain.
•Monitor vital signs (blood pressure, pulse,
respiration, consciousness).
•Instruct the patient to immediately
report instances of chest pain.
•Create an atmosphere of calm and
comfortable environment.
•Teach and encourage the patient to do
relaxation techniques.
•Collaboration in: Giving oxygen and
drugs
•Measure vital signs before and after treatment.
2. Nursing Diagnosis: Activity Intolerance related to imbalance between oxygen supply and demand, and the presence of necrotic tissue in myocardial ischemia.
Objective: The client shows an increase in the ability to perform activities (blood pressure, pulse, rhythm within normal limits) the absence of angina.
Interventions:
•Record the heart rhythm, blood pressure and
pulse before, during and after the activity.
•Instruct the
patient to have more rest first.
•Instruct the patient not to
"push" at the time of defecation.
•Explain to the
patient about the stages of activity that may be performed by the
patient.
•Show to patients about physical signs that activity
exceeds the limit.
3. Nursing Diagnosis : Risk for Decreased Cardiac Output related to changes in the rate, rhythm, cardiac conduction, decrease preload or increased SVR, miocardial infarction.
Objective: There is no decrease in cardiac output during the action of nursing.
Interventions:
•Perform blood pressure measurements
(compare the two arms in a standing position, sitting and lying down,
if possible).
•Assess the quality of the pulse.
•Note the
development of the S3 and S4.
•Auscultation of breath
sounds.
•Stay with the patient at the time of the
activity.
<="" div="">
Atherosclerosis is the most common cause of CAD and is linked to many risk factors—primarily elevated serum cholesterol levels, elevated blood pressure, and cigarette smoking. Blood levels of cholesterol and low-density lipoproteins (LDLs) have been associated with increased risk of CAD. Hypertension places chronic stress on the blood vessels and may initiate plaque deposition. Because smoking increases myocardial oxygen requirements, blood pressure, and heart rate, cigarette smokers are twice as likely to have an MI and four times as likely to have sudden cardiac death. Other risk factors include heredity, obesity, lack of physical activity, stress, and diabetes mellitus.
Nursing care plan assessment and physical examination
Patients with CAD describe symptoms of myocardial ischemia. A careful description of the pain, including location, severity, and precipitating factors, is essential. The most common symptom is angina, but some individuals remain asymptomatic. Cardiac pain is usually described as a diffuse aching pain or pressure that is relieved by rest or administration of nitroglycerin. The pain is usually substernal but may radiate to either arm, the neck, or between the shoulder blades. Often, the pain is precipitated by extra physical or emotional demands. Atypical pain may originate in the elbow, jaw, or shoulder. The patient may have no pain sensation but may complain of being short of breath or having nausea, vomiting, lightheadedness, or sweating.
Physical examination may reveal nothing abnormal. Labored breathing, pallor, and profuse sweating suggest that chest pain may be caused by MI. There may be evidence of flat or slightly raised yellowish tumors, most frequently found on the upper and lower lids (xanthelasma), or flat, slightly elevated, soft, rounded plaques or nodules, usually on the eyelids (xanthoma). Auscultate the heart sounds carefully to identify accompanying cardiac problems such as valvular dysfunction or heart failure.
Because the stress in one’s life has long been associated with the development of CAD, problem solving to reduce stress is an important nursing function. Occupational stress or the obligations from multiple roles may vary for female and male patients. Individuals whose work involves heavy lifting may require vocational rehabilitation counseling in order to return to work. Conti
Nursing care plan intervention and treatment plan
Several invasive but nonsurgical procedures can be used to manage CAD. Percutaneous coronary intervention (PCI) includes balloon catheter angioplasty and stenting. A balloon catheter angioplasty involves an invasive radiographic procedure that is performed under local anesthesia. A balloon-tipped coronary catheter is introduced into a coronary vessel and inflated and deflated in quick succession. The atheroma (fatty lesion) is compressed against the vessel wall, and the stenosis is dilated, which increases coronary blood flow. During the stent procedure, the cardiologist places a small, hollow metal (mesh) tube or “stent,” in the artery to keep it open following a balloon angioplasty.
CORONARY ARTERY BYPASS GRAFTING (CABG). A patent blood vessel from another
part of the body is grafted to the affected coronary artery distal to the lesion. The new vessel bypasses the obstruction. Unfortunately, unless reduction of risks and modification of the lifestyle accompany this procedure, the grafted vessels will also eventually occlude. Vessels commonly used for grafting are the greater or lesser saphenous veins, basilic veins, and right and left internal mammary arteries.
Managing the patient after heart surgery involves complex collaborative strategies among the nurse, surgeon, and respiratory therapist. Usually, a patient leaves the operating room with a systemic arterial and pulmonary artery catheter in place. Fluids and medications are administered according to the patient’s hemodynamic response to the surgery. Monitoring for complications is also an essential role. Early complications from heart surgery include hypotension or hypertension (lowered or raised blood pressure), hemorrhage, dysrhythmias, decreased cardiac output, fluid and electrolyte imbalance, pericardial bleeding, fever or hypothermia, poor gas exchange, gastric distension, and changes in level of consciousness.
If the patient has a large amount of drainage from mediastinal tubes, the nurse may initiate autotransfusion. In the immediate postoperative period, patients will need airway management with an endotracheal tube and breathing support with mechanical ventilation. Some patients will also require temporary cardiac pacing through epicardial pacing wires that are inserted during the surgery. Patients will often need fluid therapy with blood, colloids, or crystalloids to replace Durin
HEAD
HEART
MUSCLE
KNEES
SODIUM
POTASSIUM
CALCIUM
MAGNESIUM
sodium imbalance quite often there will be changes in mental status - confusion, delirium, etc. Often seen with traumatic brain injury where diabetes insipidus (pathological voiding of large amounts of dilute urine) and its opposite SIADH (syndrome of inappropriate antidiuretic hormone - minimal urine output but very concentrated) may occur. Sodium imbalances are also seen with dehydration in some patients (elderly, burn victims, many others) and the blood levels will go up. Very rarely, sodium levels in the blood will go down because of consuming large quantities of fluids.
Sodium Na+ 136-145 HEAD
does affect fluid. In fact, they say sodium always follows water. There are a lot of people with edema related hypernatremia; and a lot of dehydration related to sodium and chloride losses.
Sodium - body water balance
Potassium homeostasis is maintained by the balance of potassium
excretion and potassium cellular shifts.
•Potassium excretion is
tightly regulated by the kidneys.
•Potassium cellular shifts are
principally mediated by hormones.
Potassium - K + 3.5 - 5.0 HEART (BANANA BUNDLE OF LOVE)
contraction of skeletal and smooth muscle and nerve impulse conduction
when potassium is out of whack, and its most serious consequence is cardiac problems that can be life-threatening (you will see T wave changes: depression with hypokalemia, elevation with hyperkalemia, among other changes in the EKG like QRS interval changes).
One regulates K+ excretion, or external balance through the kidneys and intestines, and the second regulates K+ shifts, or internal balance between intracellular and extracellular fluid compartments. Internal balance is mainly mediated by insulin and catecholamines.
Ingested K+ is absorbed rapidly and enters the portal circulation, where it stimulates insulin secretion. Insulin increases Na+,K+-ATPase activity and facilitates potassium entry into cells, thereby averting hyperkalemia. β2-Adrenergic stimulation also promotes entry of K+ into cells through increased cyclic adenosine monophosphate (cAMP) activation of Na+,K+-ATPase
formation and structure of bones and teeth, cell structure and function, cell membrane permeability and impulse transmission, the contraction of all muscle types and is necessary in the blood clotting process
Calcium. Ca+ 9.0-10.5 MUSCLES
important in the digestive acids; closely linked to sodium
LIKE CHLORINE IN THE POOL , TEMPS OUTSIDE 98-106
chloride CI + 98-106
affects nerve and muscle action by affecting calcium usage, activates enzymes involved in carbohydrate and protein metabolism, helps in the transport of sodium and potassium across cell membranes, and influences the levels of sodium, potassium, calcium and some body hormones (parathyroid hormone)
MAG(KNEES) IUM
formation and structure of bones and teeth, this electrolyte is needed in the following activities: utilization of B vitamins, acid base homeostasis, bone formation, nerve and muscle activity, cell division, the transmission of hereditary traits, metabolism of carbohydrates, proteins and fats
Phosphorus
7.35-7.45
PH
Nonrenal losses (urine K+ < 20 mmol/L) •Diarrhea, laxative
abuse
•Vomiting
Renal losses (urine K+ >?20
mmol/L) •Loop diuretics (furosemide, bumetanide, torsemide): block
chloride-coupled sodium reabsorption in the loop of
Henle
•Thiazide diuretics (hydrochlorothiazide): block distal
tubule chloride-coupled sodium reabsorption
•Osmotic diuresis
(uncontrolled diabetes)
Hypokalemia with hypertension
•Mineralocorticoid excess
•Primary
hyperaldosteronism
•Glucocorticoid-remediable aldosteronism:
renovascular hypertension, renin-secreting tumor, Liddle
syndrome
•Apparent mineralocorticoid excess: 11β-hydroxysteroid
dehydrogenase deficiency (genetic, drug induced [chewing tobacco,
licorice], congenital adrenal hyperplasia)
Hypokalemia
with normal blood pressure •Bartter's syndrome
•Gitelman's
syndrome
•Magnesium depletion (cis-platinum,
alcoholism)
•Renal tubular acidosis (types 1 and 2)
Treatment for Hypokalemia
Cause of hypokalemia should be addressed (remove drug, change
diet, stop gastric drainage).
Indications for IV potassium (20
mmol/hr with cardiac monitoring, reassess after 60 mmol):
Cardiac arrhythmias with rapid ventricular response •Cardiac
arrhythmias caused by digoxin toxicity
•Severe
diarrhea
•Severe myopathy with muscle
necrosis
•Paralysis
Indications for oral potassium
chloride (20-80 mmol/day in divided doses): •All other situations
except for renal tubular acidosis: replace with oral potassium
bicarbonate, citrate, acetate, or gluconate.
Box 3 Causes of Hyperkalemia
Spurious •Thrombocytosis (>1,000,000/mm3)
•Leukocytosis
(>50,000/mm3)
•Hemolysis
•Repeated fist clenching with
tourniquet in place
Impaired potassium excretion •Renal
insufficiency or failure
•Mineralocorticoid
deficiency
•Addison’s disease
•Hyporenin hypoaldosteronism
(type 4 renal tubular acidosis)
•Hereditary enzyme
deficiencies
Pseudohypoaldosteronism
Drugs •Block
sodium channel in distal nephron-trimethoprim, pentamidine,
potassium-sparing diuretics (amiloride, triamterene)
•Block
aldosterone production: ACE inhibitors, angiotensin receptor blockers,
NSAIDs, and COX-2 inhibitors, heparin, tacrolimus
•Block
aldosterone receptors: spironolactone, eplerenone
•Block Na+,
K+-ATPase activity in the distal nephron: cyclosporine
Impaired transcellular shift-insulin deficiency
Hypertonicity (uncontrolled diabetes): familial hyperkalemic
periodic paralysis •Drugs-beta blockers, digoxin (at toxic levels),
succinylcholine, arginine, lysine
Excessive potassium load
Massive tissue breakdown (rhabdomyolysis, burns, trauma)
ACE, angiotensin-converting enzyme; COX-2, Cyclooxygenase-2; NSAID, nonsteroidal anti-inflammatory drug.
Emergency Treatment
Electrocardiographic abnormalities IV
calcium gluconate or chloride (10 mL of 10% solution) Immediate 15-30
min
[K+]> 6.5 mmol/L or rising IV Glucose (50 mL of 50%) + IV
regular insulin, 10 U 10-20 min 2-3 hr
Albuterol (10-20 mg) by
inhaler over 10 min 20-30 min 2-3 hr
IV sodium bicarbonate
(only if metabolic acidosis) Delayed
Kayexalate (sodium
polystyrene), 15-30 g, with sorbitol 4-6 hr (PO); 1 hr (as retention
enema)
Loop diuretic (IV) 1 hr
Hemodialysis 15-30 min
Long-Term Treatment
Dietary potassium restriction, 2-3
g/day
Discontinue supplemental potassium (salt substitutes)
Discontinue drugs that interfere with potassium homeostasis
Augment potassium excretion with loop diuretics, thiazide
diuretics, fludrocortisone, if hypoaldosteronism present
Reduction in Risk of Myocardial Infarction, Stroke, and Death from Cardiovascular Causes
Altace (ramipril capsules) is indicated in patients 55 years or older at high risk of developing a major cardiovascular event because of a history of coronary artery disease, stroke, peripheral vascular disease, or diabetes that is accompanied by at least one other cardiovascular risk factor (hypertension, elevated total cholesterol levels, low HDL levels, cigarette smoking, or documented microalbuminuria), to reduce the risk of myocardial infarction, stroke, or death from cardiovascular causes. Altace (ramipril capsules) can be used in addition to other needed treatment (such as antihypertensive, antiplatelet or lipid-lowering therapy).
Hypertension
ALTACE (ramipril capsules) is indicated for the treatment of hypertension. It may be used alone or in combination with thiazide diuretics. In using ALTACE (ramipril capsules) , consideration should be given to the fact that another angiotensin converting enzyme inhibitor, captopril, has caused agranulocytosis, particularly in patients with renal impairment or collagen-vascular disease. Available data are insufficient to show that ALTACE does not have a similar risk. (See WARNINGS .)
In considering use of ALTACE (ramipril capsules) , it should be noted that in controlled trials ACE inhibitors have an effect on blood pressure that is less in black patients than in non-blacks. In addition, ACE inhibitors (for which adequate data are available) cause a higher rate of angioedema in black than in non-black patients. (See WARNINGS , Angioedema.)
Heart Failure Post Myocardial Infarction
Ramipril is indicated in stable patients who have demonstrated clinical signs of congestive heart failure within the first few days after sustaining acute myocardial infarction. Administration of ramipril to such patients has been shown to decrease the risk of death (principally cardiovascular death) and to decrease the risks of failure-related hospitalization and progression to severe/resistant heart failure. (See CLINICAL PHARMACOLOGY , Heart Failure Post Myocardial Infarction for details and limitations of the survival trial.)
Adverse Event
Ramipril
(n=1004) (n=982)
Hypotension 11 5
Cough Increased 8 4
Dizziness 4 3
Angina Pectoris 3 2
Nausea 2 1
Postural Hypotension
2 1
Syncope 2 1
Vomiting 2 0.5
Vertigo 2 0.7
Abnormal Kidney Function 1 0.5
Diarrhea 1 0.4
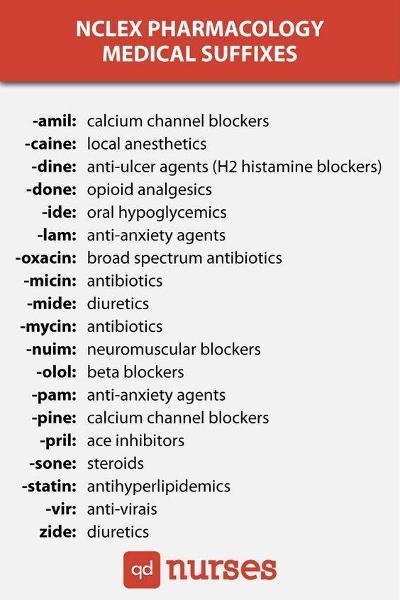

Adverse Event Ramipril Placebo
(n=1004) (n=982)
Hypotension 11 5
Cough Increased 8 4
Dizziness 4 3
Angina Pectoris 3 2
Nausea 2 1
Postural Hypotension
2 1
Syncope 2 1
Vomiting 2 0.5
Vertigo 2 0.7
Abnormal Kidney Function 1 0.5
Diarrhea 1 0.4
You should not use this medication if you are allergic to metoprolol, or other beta-blockers (atenolol, carvedilol, labetalol, nadolol, nebivolol, propranolol, sotalol, and others), or if you have:
•a serious heart problem such as heart block, sick sinus syndrome, or slow heart rate;
•severe circulation problems;
•severe heart failure (that required you to be in the hospital); or
•history of slow heart beats that have caused you to faint.
To make sure metoprolol is safe for you, tell your doctor if you have:
•asthma, chronic obstructive pulmonary disease (COPD), sleep apnea, or other breathing disorder;
•diabetes (taking metoprolol may make it harder for you to tell when you have low blood sugar);
•liver disease;
•congestive heart failure;
•problems with circulation (such as Raynaud's syndrome);
•a thyroid disorder; or
•pheochromocytoma (tumor of the adrenal gland).
The Connection Between Grapefruit and Statins
Highlights
1 Grapefruit can affect the rate at which drugs
are processed by the liver.
2 These include many drugs used to
treat blood vessel and heart conditions, such as statins.
3 The
interaction is particularly strong with two types of statins: Zocor
and Lipitor.
Statins are prescription drugs used to lower cholesterol. They prevent your body from making more cholesterol and can help your body reabsorb the cholesterol already present in your artery walls.
Not everybody with high cholesterol levels needs to take statins. The drug is recommended for people who are at a high risk for heart disease. Individuals with a family history of heart disease and high cholesterol might need to take statins. Other risk factors such as being overweight or having diabetes might warrant statin use as well.
refers to diseases of the blood vessels (arteries and veins) located outside the heart and brain. While there are many causes of peripheral vascular disease, doctors commonly use the term peripheral vascular disease to refer to peripheral artery disease (peripheral arterial disease, PAD), a condition that develops when the arteries that supply blood to the internal organs, arms, and legs become completely or partially blocked as a result of atherosclerosis
Peripheral vascular disease (PVD)
is a gradual process whereby hard cholesterol substances (plaques) are deposited in the walls of the arteries. Cholesterol plaques cause hardening of the artery walls and narrowing of the inner channel (lumen) of the artery. The atherosclerosis process begins early in life (as early as teens in some people).
Atherosclerosis
most common symptom of ________________is intermittent claudication, manifested by pain (usually in the calf) that occurs while walking and dissipates at rest.
Heart attack: permanent damage to the heart muscle caused
by a lack of blood supply to the heart for an extended time
Stroke: interruption of the blood flow to the brain
Transient ischemic attack (TIA): a temporary interruption
in the blood supply to the brain)
Renal artery disease or stenosis: a narrowing or blockage of the artery that supplies blood to the kidney
Amputation: the removal of part or all of the foot or leg
(rarely the arm), especially in people who also have diabetes
peripheral artery disease
Approximately half of people with peripheral artery disease do not
experience any symptoms. For patients with symptoms, the most common
symptoms are intermittent claudication and rest pain.
•Intermittent claudication: Intermittent claudication refers to
pain or cramping in the arms or legs that occurs with exercise and
subsides with rest. The severity and location of the pain of
intermittent claudication vary depending upon the location and extent
of blockage of the involved artery. The most common location of
intermittent claudication is the calf muscle. The pain in the calf
muscle occurs only during exercise such as walking, and the pain
steadily increases with continued walking until the patient has to
stop due to intolerable pain. Then the pain quickly subsides during
rest. Intermittent claudication can affect one or both legs.
•Rest pain: Rest pain occurs when the artery occlusion is so
critical that there is not enough blood and oxygen supply to the lower
extremities even at rest. The pain typically affects the feet, is
usually severe, and occurs at night when the patient assumes a supine
position (lying down, face up).
Other symptoms and signs of peripheral artery disease include:
•
Numbness of the extremities.
•Weakness and atrophy (diminished size and strength) of
the calf muscle.
•A feeling of coldness in the legs or feet.
•Changes in color of the feet; feet turn pale when they
are elevated, and turn dusky red in dependent position.
•Hair loss over the dorsum of the feet and thickening of
the toenails.
•Painful ulcers and/or gangrene in tissue where there is
critical ischemia (lack of blood and oxygen), typically in the
toes.
Pulse and blood pressure checks in different areas of your body. Your
doctor may also look at the color of your foot when it is elevated and
after you exercise.
•
Ankle-brachial index (ABI) test checks blood flow by
comparing blood pressure in the ankles and the arms.
• Doppler ultrasound. It may be used to measure blood
flow in the arteries.
• Magnetic resonance angiogram (MRA) or
computerized tomography (CT) angiography. These tests can also help
diagnose PAD. These tests might be done before a procedure or surgery
Tests you may have to confirm PAD include
Leg pain that does not go away when you stop
exercising
•Foot or toe wounds that won't heal or heal very
slowly
•Gangrene
•A marked decrease in the temperature of your lower leg or
foot particularly compared to the other leg or to the rest of your body
There are many risk factors for high blood pressure. Some factors you
can’t change. Others are modifiable based on your lifestyle. Risk
factors you cannot change include:
•age: Older adults are at
greater risk for high blood pressure.
•gender: Women over 65 are
more likely to have higher blood pressure, and men under age 45 are
more likely to have high blood pressure than women.
•race: African-Americans are
more likely to have high blood
pressure.
•family history: If your direct family
members (parent or sibling) have high blood pressure, you are more at risk.
Factors that are modifiable include:
•
being overweight
•not exercising enough
•eating an unhealthy diet
•consuming excess salt
•drinking alcohol
•smoking
•sleep apnea
•stress
prehypertension: 120/80 mmHg or higher
•stage 1 high blood pressure: 140/90 mmHg or
higher
•stage 2 high blood pressure: 160/100 mmHg or
higher
•hypertensive crisis (a life-threatening condition):
180/110 mmHg or higher
Your doctor will also review your health history and risk factors and perform a physical exam to make a diagnosis.
High Blood Pressure Tests and Treatments
The test to determine if you have high blood pressure is simple
and non-invasive. Your doctor will measure your blood pressure using
a monitor with a cuff. Your doctor may do this several times over a
few appointments to get an accurate reading because your blood
pressure can change depending upon many factors, some as simple as
your mood at the time the measurement is taken. Your doctor may also
order:
•blood tests
•urine tests
•electrocardiogram
(ECG)
•chest X-ray
•computed tomography (CT)
scan
•reducing the amount of salt in your diet
•exercising
and losing weight
•beginning a smoking cessation
plan
•trying to reduce stress with some relaxation techniques
Treatment for high blood pressure varies from changing lifestyle
choices to using medications. If your increased blood pressure is not
severe your doctor will probably recommend lifestyle modifications
first. These include:
•losing
weight
•exercising
•eating healthy
•reducing the amount
of salt in your diet
If this doesn’t work or if you have a more serious high blood
pressure diagnosis, your doctor will probably prescribe medication.
Drugs that help lower high blood pressure include:
•diuretics
•beta blockers
•calcium channel blockers
•ACE inhibitors
•vasodilators
Grade I is a clean wound less than 1 cm long. Grade II is a larger wound without extensive soft tissue damage or avulsions. Grade III is highly contaminated and has extensive soft tissue damage. It may be accompanied by traumatic amputation and is the most severe
GRADES OF BREAK
Fat emboli occur in almost 90% of all people with severe injuries to bones, although only 10% of these are symptomatic. The risk of fat embolism syndrome is thought to be reduced by early immobilization of fractures and especially by early operative correction. There is also some evidence that steroid prophylaxis of high-risk patients reduces the incidence. The mortality rate of fat-embolism syndrome is approximately 10–20%
Fat emboli can be either traumatic (resulting from fracture of long bones, accidents, or trauma to soft tissue) or non-traumatic (resulting from burns or fatty liver).
Pathogenesis
The pathogenesis occurs due to both mechanical obstruction and biochemical injury. It is aggravated by local platelet and erythrocyte aggregation. The release of fatty acids from the fat globules also causes local toxic injury to endothelium. The vascular damage is aggravated by platelet activation and recruitment of granulocytes.
Several mechanisms have been proposed to explain the pathogenesis of fat embolism. They may be acting together or singly
1.Mechanical. Mobilisation of fluid fat following trauma to bone and
soft tissue
2.Emulsion instability. Explains the pathogenesis of
fat embolism in non-traumatic cases. Fat embolus formed by aggregation
of plasma lipids (chylomicrons and fatty acids) due to disturbances in
emulsification of fat. Symptoms include fatty liver (hepatic
steatosis).
3.Intravascular coagulation. May result from
disseminated intravascular coagulation (DIC).
4.Toxic injury.
Blood vessels injured by high plasma levels of free fatty acid,
results in increased vascular permeability and consequently pulmonary edema.
Complications
Complications from a fat embolism tend to be
serious:
1.Pulmonary fat embolism. Widespread obstruction causes
sudden death.
2.Systemic fat embolism. These may get lodged in
capillaries of organs like brain, kidney, skin etc., causing minute
hemorrhage and microinfarcts.[5]
Embolized fat travels through the venous system to the lungs and can occlude pulmonary capillaries. Fat emboli may cause cor pulmonale if adequate compensatory pulmonary vasodilation does not occur.
Circulating free fatty acids are directly toxic to pneumocytes and capillary endothelium in the lung, causing interstitial hemorrhage, edema and chemical pneumonitis.
Diagnosis
Diagnosis of FES may be difficult because, except for the
petechiae, there are no pathognomonic signs. Laboratory tests are
mostly nonspecific:
Serum lipase level increases in bone trauma
– often misleading.
Cytologic examination of urine, blood and
sputum with Sudan or Oil Red O staining may detect fat globules that
are either free or in macrophages. This test is not sensitive,
however, and does not rule out fat embolism.
Blood lipid level
is not helpful for diagnosis because circulating fat levels do not
correlate with the severity of the syndrome.
Decreased
hematocrit occurs within 24–48 hours and is attributed to
intra-alveolar hemorrhage.
Alteration in coagulation
(thrombogenesis) and thrombocytopenia.
The chest X-ray may show evenly distributed, fleck-like pulmonary shadows (snow storm appearance), increased pulmonary markings and enlargement of the right side of the heart.
Hypoxemia is present in nearly all patients with FES, often to a PaO2 of well below 60 mmHg. Arterial hypoxemia in these patients has been attributed to ventilation-perfusion inequality and intrapulmonary shunting. Acute cor pulmonale is manifested by respiratory distress, hypoxemia, hypotension and elevated central venous pressure.
Treatment
The most effective prophylactic measure is to reduce long bone fractures as soon as possible after the injury.
Maintenance of intravascular volume is important because shock can exacerbate the lung injury caused by FES. Albumin has been recommended for volume resuscitation in addition to balanced electrolyte solution, because it not only restores blood volume but also binds fatty acids, and may decrease the extent of lung injury.[
Acute compartment syndrome is the most common type of compartment syndrome. About three-quarters of the time, acute compartment syndrome is caused by a broken leg or arm. Acute compartment syndrome develops rapidly over hours or days.
Compartment syndrome can develop from the fracture itself, due to pressure from bleeding and edema. Or compartment syndrome may occur later, as a result of treatment for the fracture (such as surgery or casting).
Acute compartment syndrome can also occur after injuries without
bone fractures, including:
•Crush
injuries
•Burns
•Overly tight bandaging
•Prolonged
compression of a limb during a period of unconsciousness
•Surgery
to blood vessels of an arm or leg
•A blood clot in a blood vessel
in an arm or leg
• Extremely vigorous exercise, especially
eccentric movements (extension under pressure
Taking anabolic steroids can also contribute to developing compartment syndrome.
Another form of compartment syndrome, called chronic compartment syndrome, develops over days or weeks. Also called exertional compartment syndrome, it may be caused by regular, vigorous exercise . The lower leg, buttock, or thigh is usually involved.
Abdominal compartment syndrome almost always develops after a
severe injury, surgery, or during critical illness. Some conditions
associated with abdominal compartment syndrome include:
•Trauma,
especially when it results in shock
•Abdominal surgery,
particularly liver transplant
•Burns
• Sepsis (an infection
causing inflammation throughout the body)
•Severe ascites or
abdominal bleeding
•Pelvic fracture
• Vigorous eccentric
abdominal exercises (i.e. situps on a back extension machine in weight rooms)
As the pressure in the abdominal compartment rises, blood flow to and from the abdominal organs is reduced. The liver, bowels, kidneys, and other organs may be injured or permanently damaged.
Repeat the same sequence:
1.Place crutches forward.
2.Step
with weaker leg.
3.Step with stronger leg.
3 POINT GAIT WITH CRUTCHES
Lortab contains a combination of acetaminophen and hydrocodone. Hydrocodone is an opioid pain medication. An opioid is sometimes called a narcotic. Acetaminophen is a less potent pain reliever that increases the effects of hydrocodone.
Lortab is used to relieve moderate to severe pain.
Lortab may also be used for purposes not listed in this medication guide.
Hydrocodone can slow or stop your breathing. Never use Lortab in larger amounts, or for longer than prescribed. Narcotic pain medicine may be habit-forming, even at regular doses. Never share this medicine with another person, especially someone with a history of drug abuse or addiction. Keep the medication in a place where others cannot get to it..Do not use Lortab if you have used a MAO inhibitor in the past 14 days, such as isocarboxazid, linezolid, methylene blue injection, phenelzine, rasagiline, selegiline, or tranylcypromine.Do not take more of Lortab than is recommended.
An overdose of acetaminophen can damage your liver or cause death. Call your doctor at once if you have nausea, pain in your upper stomach, itching, loss of appetite, dark urine, clay-colored stools, or jaundice (yellowing of your skin or eyes).