What is the structure of fatty acids?
it contains a carboxylic acid group at the alpha end then connected with a chain of carbon with various length at the beta. After ward it is attached with a methyl group.
What is the system for naming nomenclature for fatty acids?
The format is: total number of carbons : number of double bonds Δ position of double bonds.
18:1Δ9
represents an 18-carbon fatty acid with one double bond between carbon 9 and carbon 10.
Do saturated fatty acids have any double bond?
no they don't
What is the structure of fatty acids?
They are long unbranched chains of carbon atoms which are bound to hydrogen
Unsaturated fatty acids have ________
double bounds
monounsaturated (MUFA) has ____________
one carbon carbon double bond
polyunsaturated (PUFA) has _________
two or more double carbon
Where is unsaturated fatty acids found?
In vegetables oils, avocados, sunflower oil, walnuts, flax, canola oil and fish oil
Saturated fatty acids are _______ at room temperature
solid
Unsaturated fatty acids are _________ at room temperature
liquid
What is the melting point for saturated fatty acids?
relatively high
What is the melting point for unsaturated fatty acids?
relatively low
What is the source for saturated fatty acids?
animal fats, palm and coconut oil
What is the source for unsaturated fatty acids?
plant and vegetable oil, fish oil
What are the two essential fatty acids that your body cannot synthesized an must be obtained from food?
linoleic and aplha-liolenic
The basic fats are used to build _____________
specialized fats omega-3 and omega-6
The location of where the double bond is affects the ____________
naming of the fatty acids.
Omega-6 has a double carbon at the _________
sixth carbon
Omega-3 has a double carbon at the ___________
third carbon
Alpha-linolenic acid (ALA)
Eicosapentaenoic acid (EPA)
Docosahexaenoic (DHA)
are all _________
omega-3s
what does 18:3n-3 mean?
its has 18 carbons, 3 double carbon at (n-3) carbon
What is the scientific abbreviations for Eicosapentaenoic acid (EPA)
20:5n-3
What is the scientific abbreviations for Docosahexaenoic (DHA)?
22:6n-3
What is the scientific abbreviations for Alpha-linolenic acid (ALA)?
18:3n-3
EPA and DHA are considered to be derived from?
fishes cause that is where they are abundant
ALA is considered to be derived from?
plants
Omega-6s are precursors for _____________?
prostaglandins
What is prostaglandin, and what is its function?
they are a group of lipid compounds that are derived from fatty acids. they also play a role in the formation of blood clots and in the induction of labor. Also known for regulating the contraction and relaxation of smooth muscle tissue, controlling inflammation, and regulating blood flow.
What happens when you take aspirin and nonsteroidals ?
They block the synthesis of prostaglandin
What are the major sources of omega-6s?
vegatable oils, sunflower, safflower, and corn oil, meat, eggs and dairy
What can deficiency of omega-3's and omega-6 lead to?
failure to grow, alopecia, dermatitis
What happens when you consume more omega-6 then omega 3?
They compete with the omega-3 enzymes. So fewer enzyme are used to convert the omega-3 fats into anti-inflammatory chemical.
Glucose provides the ______?
primary substrate for lipogenesis
What is De novo synthesis?
It is the making of complex molecules from simple molecules such as sugars or amino acids, as opposed to recycling after partial degradation
Where does De novo synthesis occur?
In the cytosol liver, kidney, brain, lung, mammary glands and adipose tissues
How does fatty acid synthesis occur?
By combining eight two-carbon fragments to form a 16 carbon saturated acid
What is palmitate?
It is a 16-carbon saturated fatty acid, which is the major fatty acid found in palm oil.
Precursors for Fatty acid synthesis
Acetyl CoA, ATP, NADPH and CO2
Where are the sites of Fatty Acid synthesis?
Major:
-Liver
-Lactating Mammary Gland
Minor:
-Adipose Tissue
-Kidney
Where in the cell does FA synthesis take place?
Cytosol
first stage of fatty acid synthesis
when acetyl CoA is transferred out of the mitochondria and into the cytoplasm. citrate is also transported into the cytoplasm and it gets cleaved into oxaloacetate and acetyl CoA
second stage of fatty acid synthesis
acetyl CoA is activated to form malonyl CoA
third stage of fatty acid synthesis
there is repetitive addition and reduction of two carbon units to synthesize C16 fatty acids. this occurs on an acyl carrier protein, a molecular scaffold
how does citrate generate acetyl CoA?
it is transported into the cytoplasm and cleaved by ATP-citrate lyase to make acetyl CoA.
What is the major oxidation of fatty acids?
Mitochondrial beta
What is the minor oxidation of fatty acids?
alpha, omega and perxisomal beta
What happens during fasting to fatty acids?
They become the predominant substrate for energy production via oxidation in the liver, cardiac and skeletal muscle
How does mitochondrial beta oxidation occur in the liver?
acetyl-Coa is converted into ketone bodies
How does mitochondrial beta oxidation occur in the skeletal and cardiac muscle?
acetyl-Coa is completely oxidized in the tricarboxylic acid (TCA) pathway ultimately to CO2 and H2O
How many steps is the mitochondrial beta oxidation?
20 steps
how are fatty acids released?
By Insulin regulated lipase from stored triglyceride
Which cells are fatty acids carried by?
By albumin
How is fatty acyl CoA transported into the cell mitochondria?
Via the Carnitine Shuttle
What is mitochondrial beta oxidation?
catabolic pathway where fatty acids are broken down in mitochondria to produce acetyl-CoA
What is the first step in mitochondrial beta oxidation?
first oxidation
single c-c bond to a c=c bond.
reduction of FAD
What is the second step in mitochondrial beta oxidation?
hydration of the double bond between a and b carbon into a hydroxyl group
What is the third step in mitochondrial beta oxidation?
second oxidation
oxidation of the b carbon
hydroxyl group
into a carbonyl group
Reduction of NAD
What is the fourth step in mitochondrial beta oxidation?
thiolytic cleavage that produces acyl-CoA and acetyl-CoA (2Cs) is
released
Coenzyme A is linked to the new Acyl- CoA (14C)
FA are _________________ compared to glucose
highly reduced
(Can get more ATP out of a highly reduced molecule)
Alpha α- oxidation- Predominantly takes place in _____________
brain and liver, one carbon is lost in the form of CO2.
What is the substrate of α- oxidation?
Phytanic acids which is present in milk or derived from the phytol present in chlorophyll and animal fat
What does α- oxidation produce?
No ATP
Where does α- oxidation occur?
In the methyl group at the beta-carbons which blocks beta oxidation
peroxisome β-oxidation mainly happened in _________
mitochondria, but can also occur at peroxisome.
the oxidation in peroxisome occurs on ________________
very long fatty acids. For full oxidation to CO2 and H2O and NAD+
What is formed after peroxisome β-oxidation?
Formation of DHA
What are the two groups of inborn errors of metabolism?
They are acute sever manifestation and chronic progressive
Zellweger syndrome ___________
people with this syndrome cannot produce peroxisomes and therefore cannot oxidize such fatty acids.
X-linked adrenoleukodystrophy (XALD) ____________
peroxisomes cannot oxidize very long chains due to lucking functional transporter from them
What is the most common type of Fatty Acid Oxidation Disorders?
Medium chain acyl CoA dehydrogenase deficiency (MCADD)
Most Fatty Acid Oxidation Disorders are _________
Inherited
What is the treatment for Fatty Acid Oxidation Disorders?
Avoid fasting, some patients may require low fat diets
What is hyperammonemia?
is a metabolic condition characterized by the raised levels of ammonia, a nitrogen-containing compound.
What is hyperuricemia?
is when you have too much uric acid in your blood.
Acylcarnitine analysis is
helpful in the evaluation of hypoglycemia, hypotonia, cardiomyopathy, rhabdomyolysis, and metabolic acidosis
Acylcarnitine analysis is commonly performed by _______________
MS/MS directly after derivatization to either butyl or methyl esters.
A plasma acylcarnitine profile can aid in the diagnosis of _____________
organic acidemas in addition to fatty acid oxidation disorders (FAODs)
Plasma is the preferred sample type for ______________
acylcarnitine analysis
Peroxisomes are cell organelles which are found in all human cells except _________
Erythrocytes
Peroxisomes posses both _____________
Catabolic and anabolic functions.
Peroxisomes are considered to be ____________
"helpless" organelles because they very much rely on the interaction with other subcellular organelles especially mitochondria.
Neonatal adrenoleukodystrophy
Most present with early infantile hypotonia & seizures
Similar findings can be seen in the isolated deficiency of peroxisomal straight-chain acyl-CoA oxidase
Disorder of peroxisome biogenesis due to mutated PEX
Zellweger syndrome spectrum
- zellweger syndrome
- neonatal
adrenoleukodystrophy
- infantile refsum disease
Rhizomelic chondrodysplasia punctata
Rhizomelic Chondrodysplasia Punctata Type 1
marked reduction of plasmalogen levels and impairment of plasmalogen synthesis
increased levels of phytanic acid, impaired ability to oxidize
Zellweger syndrome symptoms
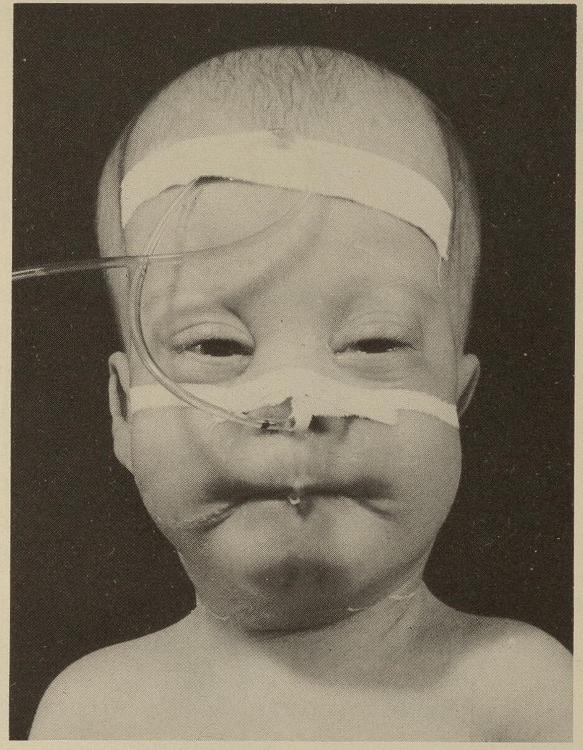
dysmorphic face, eye abnormalities, severe weakness and hypotonia, neonatal seizures, renal cortical cysts, hepatomegaly and impaired liver function, severe psychomotor retardation
Zellweger syndrome life span
autosomal recessive
most common in childhood
apparent at
birth - death by 1-2yo
Neonatal adrenoleukodystrophy symptoms
Developmental delay, neuromigration defect, hearing loss, vision impairment, liver dysfunction,
What is elevated in the Zellweger syndrome when diagnosing in plasma assay?
Very long fatty acid chain
phytanic, peristanic, pipecolic acid
What is decreased in the Zellweger syndrome when diagnosing in red cell membrane assay?
plasmalogens
What is PEX1?
It is the gene associated with the Zellweger syndrome occurs in about 68% of individuals
RHIZOMELIC CHONDRODYSPLASIA PUNCTATA (type 1) defect is in ________
PEX 7 gene = PTS2 receptor; AUTOSOMAL RECESSIVE
Rhizomelic Chondrodysplasia Punctata Type 1 health problems
The health problems are severe and apparent either at birth or in early infancy. Some children will reach childhood but it is rare that they make it past the first decade.
Rhizomelic Chondrodysplasia Punctata Type 1 symptoms
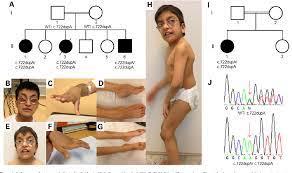
The major features that are noticed with these patients are the skeletal abnormalities, distinctive facial features, ID, and respiratory problems.
What is elevated in Rhizomelic Chondrodysplasia Punctata?
Plasma phytanic acid
What is defected in Rhizomelic Chondrodysplasia Punctata?
Red cell plasmalogens
Rhizomelic Chondrodysplasia Punctata defect is in __________
The PEX7 receptor. It is autosomal recessive
Adrenoleukodystrophy (ALD)
insufficiency of a persons adrenal glands and growth of myelin
Three phenotypes of ALD
1. Cerebral ALD- most devastating
2. Adrenomyeloneuropathy- most
common
3. Adrenal insufficiency
What are the signs and symptoms childhood Cerebral form (CCALD)
Affects children between 3-10
Mistaken for learning
disability
Seizures, hyperpigmentation, vision loss
How do you diagnoses for childhood Cerebral form (CCALD)?
Brain MRI is always abnormal in neuralgically symptomatic males.
What are the signs and symptoms childhood Cerebral form (Adrenomyeloneuropathy)
Affects all men and some women in 40s
Average age is
28
Caused by slow and progressive damage to myelin and axons due
to VLCFA accumulation
Stiffness/tingling in legs, incontinence,
cerebellar disorders (coordination/balance issues), sexual dysfunction
and impaired adrenocortical function
What are the signs and symptoms childhood Cerebral form (Adrenal Insufficiency)
Cells that produce hormones are damaged and cause... weakness/fatigue, nausea, low bp, hyperpigmentation
What is elevate in x-linked Adrenomyeloneuropathy?
abnormally elevated very long-chain fatty acids (VLCFAs)
What is the gene defected in x- linked Adrenomyeloneuropathy?
is s a gene called ABCD1.
What is the treatment for x- linked Adrenomyeloneuropathy?
Supportive symptomatic such as steroid treatment.
Hemopoietic stem cell transplantation (HSCT) may
Presymptomatic treatment for x- linked Adrenomyeloneuropathy?
Newborn screening program including CA to screen X-ALD