The primary porphyrin can be divided into 3 main categories
-acute neurovisceral
-chronic blistering cutaneous photosensitivity
-acute non blistering
CEP is referred to as
gunther's disease
Porphyrins are considered secondary if they are ______
acquired
The term porphyria were recognized in the late 19th century the term is attributed to ________
Dr.Gunther in 1911 in his naming of the congenital erythropoietic porphyria (CEP)
Porphyrins are considered primary if they are ______
inherited
Disordered can be caused by heme could either be ___________ or_____________.
inherited; acquired
What is Porphyria
Group of diseases caused by the accumulation of heme substrates caused by primary genetic defects altering any of 8 critical enzymes in the synthesis pathway in combination with environmental or metabolic issues which further reduce affected enzyme activity
The basic porphyrin structure is ___________
composed of four pyrrole rings linked by methene bridges.
Porphyrins have biological activity only when chelated to a _________
metal
porphyrins are the oxidized form of ___________
porphrinogens
The word porphyrin is derived from the root word ______
purple
porphyrin have a strong absorbance at ____________
400 nm
porphyrin have excitation at 400 nm, and emission at _________
550 and 650 nm
heme does not ______
fluorescence
(True or False) Heme is a protein.
False
Heme structure
a metalloporphyrin with iron as the central iron
The majority of heme is produced in the ____________
bone marrow (70%)
liver (15%)
The heme biosynthetic pathway __________
consists of 8 enzymes
Where are the 8 enzymes in the heme pathway?
four are found in the mitochondria and the other four are found in the cytosol
Only series III are _______
Metabolized to heme
Acute porphyria's are associated with __________
-abdominal pain, neuropathy, mental disturbances
-AIP,ADP, RCP, VP
Cutaneous porphyria's are associated with _________
-skin manifestation
-CEP,HCP,VP,EPP,HEP,PCT
What is the major enzyme that controls heme production pathway?
Do porphoryia's affect that enzyme?
- 5-Aminolevulinate synthase (ALAS)
- NO - that is why you get
plenty of heme, but you get a buildup of other enzymes (since defect
is later down the line) and thus, porphoryia
Porphyria is Greek for _____________
purple, the color urine containing excessive heme substrates changes when exposed to sunlight (UV light)
When should you suspect porphyria?
-unexplained neurovisceral symptoms such as sever abdominal pain or physiatry symptoms
-cutaneous photosensitive on sun-exposed areas, with or without blistering
What is Acute Intermittent Porphyria (AIP)?
Neurovisceral disease; most common of acute porphyrias
What is the main symptoms of Acute Intermittent Porphyria (AIP)?
abdominal pain, visceral; neuro-psychiatric disturbances; peripheral neuropathy including bulbar (difficulty swallowing etc.)
What is the most common porphyria?
Porphyria cutanea tarda (PCT)
What is the defect in Porphyria cutanea tarda (PCT)?
typically results from an ACQUIRED loss of enzymatic function.
Acute Porphyrias - Symptoms are secondary to what?
to the accumulation of high levels of delta-aminolevulinic acid (ALA) and porphobilinogen (PBG).
Laboratory investigation of porphyria?
-Measurements of urine porphobilinogen (PBG) in acute attacks
-Must be in a light protected tube if not some anilities could be degraded giving false positive
More soluble porphyria are excreted in _________
urine
Less soluble porphyria are excreted in _________
bile or stool
Urine appearance on in porphyria
appears "port wine" due to the conversion of porphobilinogen (PBG) to uroporphyrinogen
To diagnose acute porphyria testing
-begin with a urine screening that includes precursors to PBG and ALA
-if possible wait to collect urine sample during an acute episode when the patient is experiencing symptoms
What is the sample type for porphyrin analysis?
24-hour urine collection preserved with sodium carbonate and freeze immediately
protected from light
HPLC/UPLC separates ___
the water-soluble porphyrins as well as other porphyrins by HPLC using fluorescence detector
What is the most rare porphyria?
X-linked erythropoietic protoporphyria (XLP)
X-linked results from ___________?
an inherited GAIN of function mutation.
X-Linked Sideroblastic Anemia
Rare, inherited deficiency of ALA synthase
Most common
hereditary sideroblastic anemia
X-Linked Sideroblastic Anemia Treatment
Responds to Vitamin B6 which activates the remaining delta-ALA synthase.
phlebotomy and or chelation therapy to reduce accumulation off iron levels
X-Linked Sideroblastic Anemia Lab Findings
Microcytic, hypochromic anemia
X-Linked Sideroblastic is caused by _________
reduced heme synthesis, which in ineffective increasing erythron iron turnover. causing excess iron in the bone marrow
Acid dehydratase-deficiency porphyria (ADP) caused by
deficiency in the second heme synthesis pathway.
defective activity of 5-aminovulinic acid dehydratase
deficiency porphyria (ADP) caused by
autosomal recessive inherited. both parents would has to have the defect
deficiency porphyria (ADP) caused by
deficiency in the ALA dehydrate activity
Symptoms of ADP?
abdominal pain and neuropathy symptoms such as disorientation, agitation, hallucination and muscle weakness
Treatment of ADP includes __________
IV panhematin (hemin) (feedback inhibition)
acute symptoms (antibodies, seizure medication)
In the lab for testing for ADP we see a marked elevation in the ____________
5-aminolvulinic acid (ALA) and slightly marked elevation in (PBG)
Acute intermittent porphyria (AIP )
enzyme deficiency of enzyme hydroxymethybilane synthase, higher prevalence in scandanavian countries, drugs most commonly precipitate the cause of disease (barbituates, sulfonamides)
AIP is a ________
Autosomal dominant inheritance and only 1 defective parent is needed
AIP is caused by ___________
deficiency of the non-erythroid form
Clinical symptoms of AIP
abdominal pain that can be very sever
hypertension, restlessness, tremors and excess sweating, overactive sympathetic nervous systems
treatment of AIP
Panhematin (IV hemin)
GIVLAARI injection
In the lab for testing for AIP we see a marked elevation in the ____________
Total serum porphyria
PBG
Pathophysiology of acute attack caused by ___
excess ALA from the liver leads to neuronal toxicity
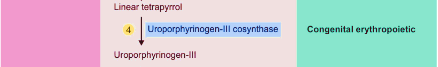
CEP
deficiency of uroporphyrinogen III cosynthase, one of the rarest porphyrias, Gunther's disease, teeth will fluoresce red under ultra violet light, red-brownish discoloration under normal light
CEP caused by a _______
mutation in the UROS gene
Symptoms of CEP
sever anemia, cutaneous photosensitive, blistering symptoms on sun exposed skin, reoccurring skin damage
In the lab for testing for CEP we see a marked elevation in the ____________
uroporphyrin and coproporphyrin
normal PBG
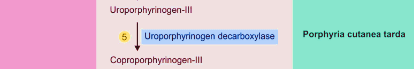
porphyria cutanea tarda (PCT)
the most common porphyria
Where is the defect in Porphyria cutanea tarda (PCT)?
typically results from an acquired loss of enzymatic function.
decreased activity of uroporphyrinogen III decarboxylase (UROD, Step 5) in the liver.
Porphyria cutanea tarda (PCT) type I is ________
(acquired) (80% of the cases)
Porphyria cutanea tarda (PCT) type II is ________
(inherited) (autosomal dominate) (20% of the cases)
Porphyria cutanea tarda (PCT) type III is ________
Homogenize inherited family (HEP) (both parent would have to have the defect (very rare)
What is the main symptoms of Porphyria cutanea tarda (PCT)?
chronic blistering cutaneous porphyria
What triggers PCT symptoms?
-Iron overload (commonly due to hemochromatosis resulting from
mutation of the HFE gene)
- Hepatitis C infection
- Alcohol abuse
- Medicinal estrogen use
PCT - should be considered when?
These porphyrias should be considered whenever a patient presents with the characteristic blistering response to sunlight.
What is the most appropriate initial test for PCT?
The measurement of total porphyrins in plasma, but total porphyrins are also elevated in the urine.
What are some final confirmatory tests?
DNA-based mutation detection, but remember that in PCT only 20% to 30% will have an identifiable mutation.
What are the effective treatments for PCT?
phlebotomy and chloroquine.
Chloroquine takes longer to work, and may exacerbate hepatotoxicity, but is LESS invasive than regular phlebotomy.
Hepatoerythropoietic Porphyria (HEP) results from __________
a homozygous mutation of both alleles of the UROD gene and is so called because porphyrins accumulate in both the red cells and liver.
symptoms of Hepatoerythropoietic porphyria (HEP)
Cutaneous symptoms, photosensitivity, abnormal hair growth, liver disease; appears in childhood, skin damage
In the lab for testing for HEP we see a marked elevation in the ____________
Uroporphyriay, heptacarboxyporphyrin, pentacarboxylin
Treatment of HEP includes __________
phlebotomy
avoid sun and iron
low dose of chloroquine
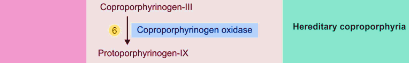
hereditary coproporhyria HCP
neurocutaneous symptoms
hereditary coproporhyria HCP inheritance
it is autosomal dominant and symptoms are similar to AIP. symptoms in female can coincide with the menstural cycle
coproporphyrinogen oxidation
This enzyme is involved in the production of a molecule called heme. catalyzes the oxygen-dependent oxidation of protoporphyrinogen IX to protoporphyrin IX.
In the lab for testing for HCP we see a marked elevation in the ____________
coproporphyrin III in the urine
Which of the five hepatic poryphrias presents with blistering skin lesions?
PCT - porphyria cutanea tarda
HCP - hereditary
coproporphyria & VP - variegate porphyria
How do you diagnose Hereditary Corproporphyria (HCP)?
COPRO III is markedly increased in the urine and feces in symptomatic patients and often persists (especially in feces) when there are no symptoms.
Urinary ALA and PBG levels are increased, though not to the extent that is present in AIP.
How do you treat Hereditary Corproporphyria (HCP)?
You treat the neuro sxs (as you do in AIP) but phlebotomy and chloroquine are not effective treatments for cutaneous lesions
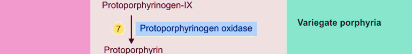
Variegate Porphyria (VP) is a dominant hepatic porphyria that results from deficient activity of...
PROTO-oxidase, the seventh enzyme in the heme biosynthetic pathway
Who gets Variegate Porphyria (VP)?
- netherland descent living in south africa
- 3 in 1000 whites
Variegate Porphyria (VP) clinical features
- skin photosensitivity
- acute neurovesical crises
blistering skin manifestations are worse than those in PCT and they are more difficult to treat and usually of longer duration
How do you diagnose Variegate Porphyria (VP)?
- urine ALA and PBG levels are increased during acute attacks but may return to normal more quickly than in AIP
In the lab for testing for Variegate Porphyria (VP) we see a marked elevation in the ____________
- increases in fecal protoporphyrin and COPRO III and in urinary COPRO III
- plasma porphryn levels are also increased, particularly when there are cutaneous lesions
Treatment of Variegate Porphyria (VP)
- acute attacks are treated as in AIP
- hemin should be started
early in most cases
- avoiding sun exposure (few other effective
measures for treating skin lesions)
X-linked Sideroblastic Anemia (XLSA) results from the deficient activity of the...
erythroid form of the ALA-synthase (ALA-synthase 2)
X-linked Sideroblastic Anemia (XLSA) is associated with...
ineffective erythropoiesis, weakness , and pallor
What are the clinical features of X-linked Sideroblastic Anemia (XLSA)?
refractory hemolytic anemia, pallor, and weakness during infancy
They have secondary hypersplenism, become iron overloaded, and can develop hemosiderosis.
How do you diagnose X-linked Sideroblastic Anemia (XLSA)?
- bone marrow examination reveals hypercellularity with a left shift
and megaloblastic erythropoiesis with an abnormal maturation
- sideroblasts
In the lab for testing for X-linked Sideroblastic Anemia (XLSA) we see a marked elevation in the ____________
- levels of urinary porphyrin precursors and of both urinary and fecal porphyrins are normal
-activity of erythroid ALA-synthase 2 is decreased in bone marrow, but this enzyme is difficult to measure in the presence of the normal ALA-synthase housekeeping 1 enzyme
X-linked Sideroblastic Anemia (XLSA) Treatment
- pyridoxine supplementation
- transfusions and chelation
therapy if refractory to pyroxidine supplementation
EPP - erythropoietic protoporphyria
Erythropoietic protoporphyria (EPP) is the most common porphyria to cause....
Erythropoietic Protoporphyria (EPP) primary source of excess protoporphyrin?
bone marrow reticulocytes
Erythropoietic Protoporphyria (EPP) results of excess protoporphyrin?
liver function abnormalities and liver failure requiring transplantation
Erythropoietic Protoporphyria (EPP) Diagnosis
- substantial increase in protoporphyrin, which is predominantly free and not complexed with zinc, is the hallmark of EPP
Erythropoietic Protoporphyria (EPP) Treatment
- avoid sunlight and wear protective clothing
- cholestyramine
and other porphyrin absorbents may be helpful to promote fecal
excretion to prevent enterohepatic circulation
The only acquired porphyria is:
a. Erythropoietic
protoporphyria (EPP)
b. Acute intermittent porphyria
(AIP)
c. Porphyria cutanea tarda (PCT)
d. Variegate
prophyria (VP)
c. Porphyria cutanea tarda (PCT)
Which of the following is NOT a part of the therapy for an attack of
acute porphyria, such as AIP?
a. IV heme (hemin)
b.
Progesterone
c. IV glucose
d. IV saline
b. Progesterone
Hemochromatosis has been identified as the cause of which of the
following porphyrias?
a. Acute intermittent porphyria
(AIP)
b. Erythropoietic protoporphyria (EPP)
c. Porphyria
cutanea tarda (PCT)
c. Porphyria cutanea tarda (PCT)
When evaluating a patient with acute neurovisceral symptoms and an
elevated spot PBG level, the practitioner should wait for final
confirmation by quantitative prophyrin measurements before beginning
therapy.
TRUE or FALSE
FALSE
Patients with erythropoietic protoporphyria present with
macrocytosis.
TRUE or FALSE
FALSE
Which of the following is NOT an effective therapy for porphyria
cutanea tarda (PCT)?
a. IV heme (hemin)
b.
Phlebotomy
c. Chloroquine
a. IV heme (hemin)
Patients with erythropoietic protoporphyria typically present
with:
a. Chronic blistering, scarring, and
photomutilation
b. Acute neurovisceral attacks
c. Burning
pain, erythema, and edema of the skin after sun exposure
d.
Macrocytic anemia
c. Burning pain, erythema, and edema of the skin after sun exposure
Describe the first step in the heme synthesis pathway? and what two precursors are used in the synthesis of porphyrins?
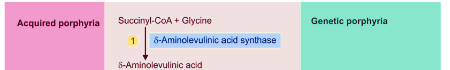
Succinyl-CoA + Glycine
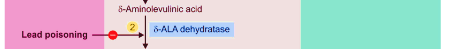
Describe the second step in the heme synthesis pathway?
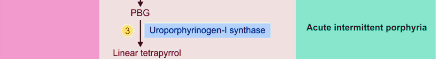
Describe the third step in the heme synthesis pathway and which disorder is associated with it ?
Describe the fourth step in the heme synthesis pathway and which disorder is associated with it ?
Describe the fifth step in the heme synthesis pathway and which disorder is associated with it ?
Describe the sixth step in the heme synthesis pathway and which disorder is associated with it ?
Describe the seventh step in the heme synthesis pathway and which disorder is associated with it ?
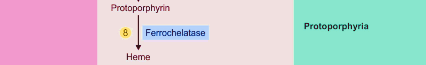
Describe the eight step in the heme synthesis pathway and which disorder is associated with it ?