class 6, total lecture 7
Types of humoral immune responses and functional diversification of antibodies
2/08
antibody functional diversity by isotype class switch recombination
last class - isotype switching and mechanisms of how its done
Ig heavy chain class (isotype) switching
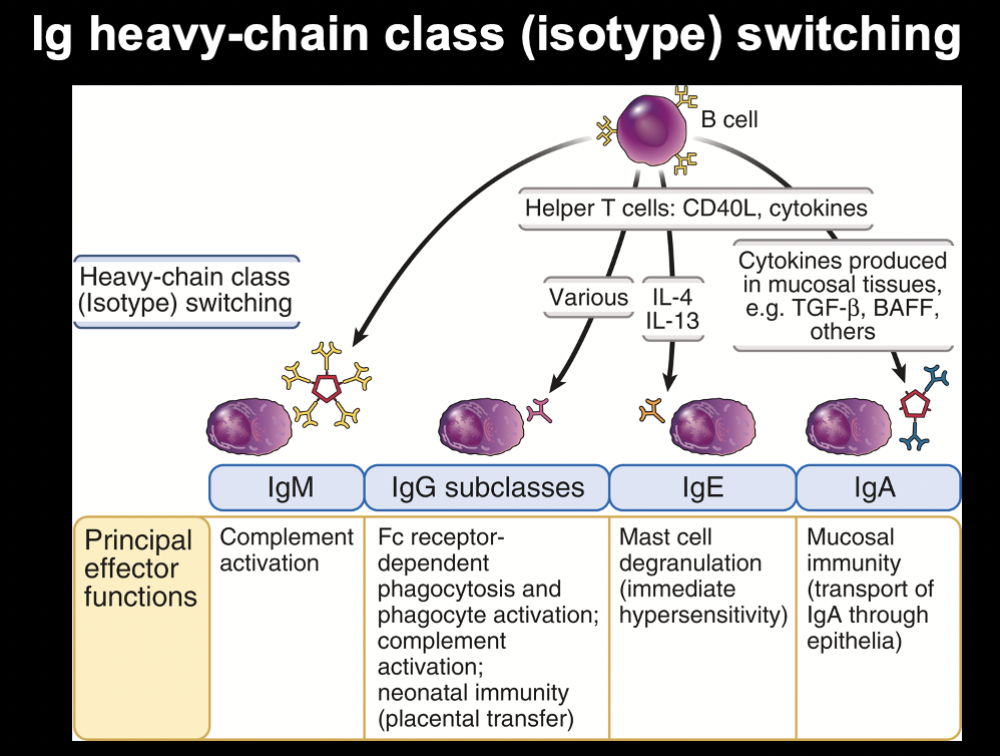
why we make diff isotype
bc of their functions
antibody class: immunoglobulin M
- IgM - first Ab on surface of a B cell (BCR)
- IgM secreted as a
pentamer Ab
- IgM molecule w/ 5 antibodies held together by J chain
- present as pentameric form
- IgM is the main class without T cell help (T cell independent, TI)
- IgM is best in complement mediated killing of pathogens
IgM always used as first antibody - doesn't matter if response is T dependent or independent
- have lower affinity bc have not undergone processes of B cell maturation to increase affinity
- IgM antibodies made have lower affinity bc has not undergone any processes to make binding site better
in T cell independent immune response, where there is no germinal center reaction, the antibodies remain lower affinity bc those do not go through the same maturation for enhanced affinity
IgM best in complement mediated killing
- antibodies act mostly as extracellular protective molecule
- typically, antibodies catch pathogens when they are not in cells
- thus, antibodies catch pathogens more as a whole, when this happens, IgM attaches to pathogens + recruits complement protein C31Q. Complement recruited to IgM molecule that is bound to molecule
- so this helps immune response earlier on, bc complement adds to it
antibody class: IgA
- IgA is a monomer and a dimer
- serves as opsonin for neutrophils, eosinophils, and macrophages
- IgA dimer is the main Ig secreted at the mucosal surfaces (ex: lungs, intestines, etc.)
How does structure affect function?
IgM is BULKY
- very limited to reach everywhere in body
- drawback – its bulky size = less ability to go thru membranes
Now IgA:
- most protective antibody molecule in our mucosal membranes (areas exposed to world)
- GI, lungs, genetalia, etc.
- secreted + present in mucus
IgA dimer is transported through epithelial cells to be secreted at the mucosal surfaces
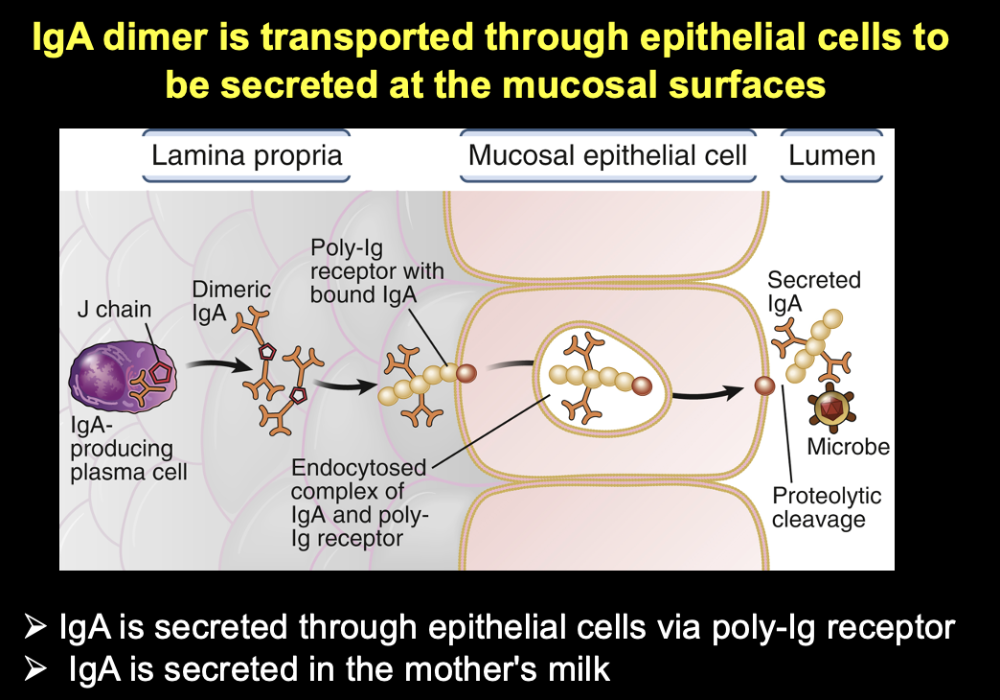
- IgA is secreted through epithelial cells via poly-Ig receptor
- IgA is secreted in the mother's milk
Mechanism for IgA
- when produced, has ability to bind receptor on epithelial cells (lining of lung/gut), where there is polyIg receptor
- IgA bind to receptor -> get internalized, pass thru cell, and IgA can pass thru the cell
= transport protein (IgA) from 1 side to the other
For IgA molecule to be present in all the palces it is, it binds to poly-Ig receptor to get secreted outside cell on the other side
antibody class: IgG
- IgG is a monomer
- is most compact of Abs
- there are 4 subclasses of IgG (1-4)
- serves as an opsonin
- activates complement
- sensitizes NK cells
- + mediates antibody dependent cellular toxicity (ADCC)
- most abundant in the blood and at mucosal surfaces
- crosses placenta
most versatile
small + compact
produced only after Ig class switching (during the germinal center reaction)
- during this time, there is also affinity maturation through somatic mutation
- thus, these IgGs always have higher affinity
has most compact structure
comes in subclasses
functions examples:
- can serve as opsonin - target pathogen becomes more attractive for phagocytes
- can activate complement - IgG
constant region can bind complement proteins + activate the
complement system (which ultimately leads to formation of protein
complex that pokes holes in biological membranes)
- complement leads to death of target pathogens
- recruits + activates NK cells - important for killing of infected cells
important to protect fetus from infection, even after birth (give baby passive immunity from mother)
multiple functions
antibody class: IgE
- IgE is a monomer
- primarily induced by IL-4 (cytokine)
- triggers release on granular contents from mast cells, eosinophils, and basophils
- respond to non-pathogenic substances; pollen, peanut, etc -> allergies
- to take care of large pathogens, like parasites
- binds to certain types of innate cells (mast cells)
- sensitizes mast cells and get them ready to be active vs target
- molecule that first is on surfaces (skin, etc. bc where parasitic infections occur) in very small quantities
- once pathogen, more IgG is made
antibody classes are selectively distributed in the body
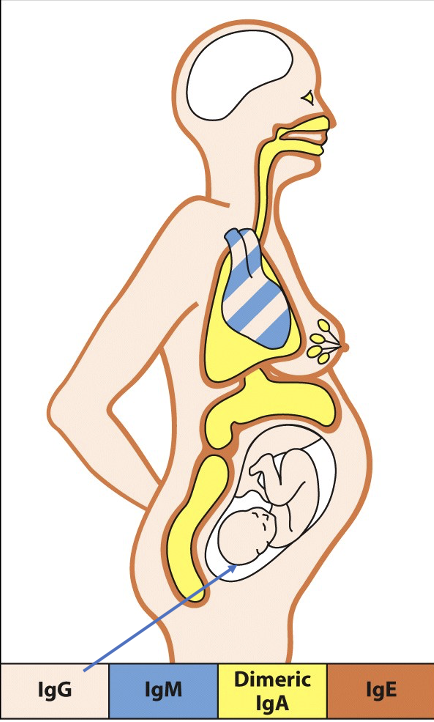
map for where they are in the body
some antibodies recruit specific cells (like how IgE recruit mast cells + eosinophils)
Which antibody isotype can cross the placental barrier and is passed
on to the fetus?
Which antibody isotype is designed to
be secreted via the epithelial cells at the mucous membranes?
pause for activity
answer:
IgG, IgA
effector mechanism of humoral immunity
functions of antibody classes
...
antibody functions
- neutralization of microbes + toxins
- get pathogen before it enters
- opsonization and phagocytosis of microbes
- antibody dependent cellular
cytotoxicity
- using NK cell
- Can bind
bacteria directly and recruit complement (antibody molecules +
complement together can form immune complexes) (big significance
clinically bc the complexes can grow so big that cannot be filtered
/ can clog filtering system in kidneys that can lead to kidney
dysfunction)
- lysis of microbes
- via complement
- phagocytosis of microbes opsonizes with
complement fragments (ex: C3b)
- via complement
- inflammation
- via complement
- important inflammatory mechanism. Are often involved in autoimmune diseases
- lysis of microbes
Ab blocks penetration of microbe through epithelial
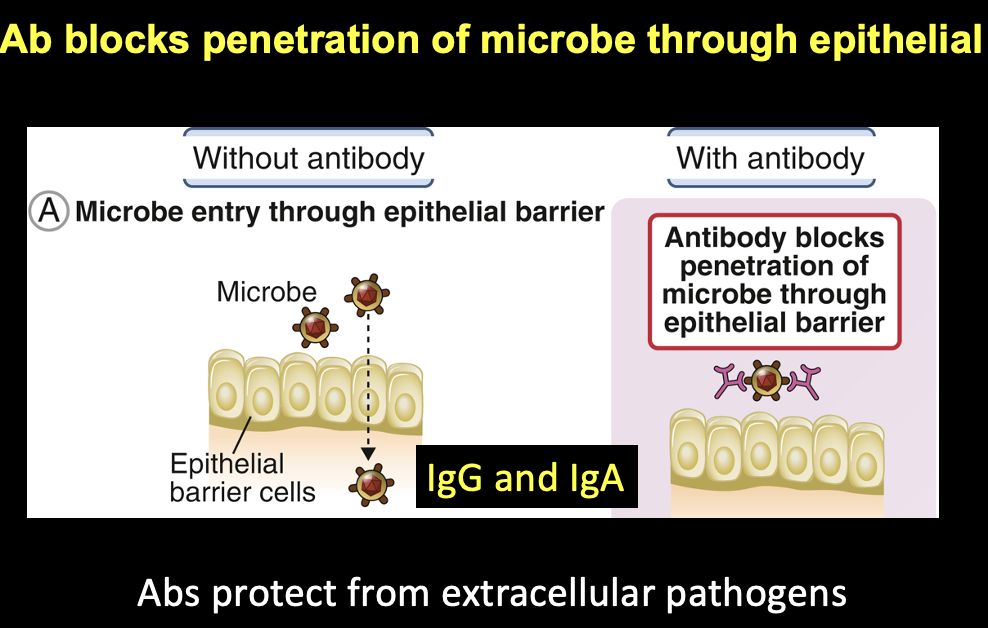
without antibody:
- microbe get thru epithelial barrier cells
with antibody:
- antibody blocks penetration of microbe thru epithelial barrier
= antibodies protect from extracellular pathogens
Microbes outside epithelial surfaces can bind to structures on microbes, which are used by microbes to attach to epithelial cells
- ex: spike protein on covid causes covid 19
Bind to it, and prevent pathogen from causing harm and entering
which 2 antibody types work against microbes that try to penetrate epithelia?
IgG and IgA
Abs block microbes from infecting neighboring cells
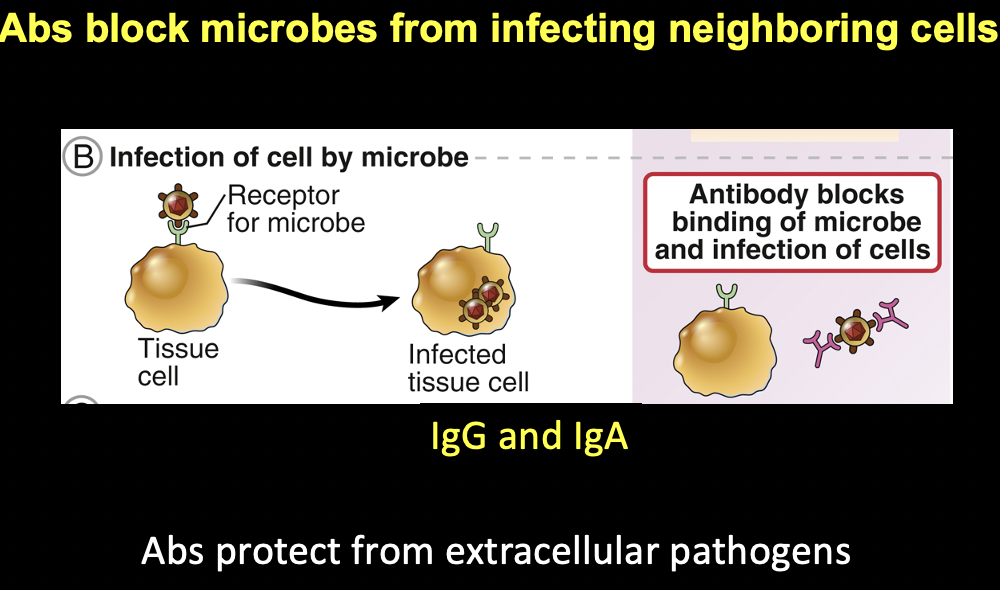
IgG and IgA
these antibodies block binding of microbe and infection of cells
antibodies protect from extracellular pathogens
IgA and IgG
- generally protect vs extracellular pathogens
- same concept. Neutralized
FcRs-mediate destruction of Ab-coated pathogens
Receptors on innate cells can be motivated/activated by antibodies to destroy pathogens
Fc receptors
Constant regions of antibodies – called Fc regions
Abs mediate phagocytosis of pathogens by opsonization
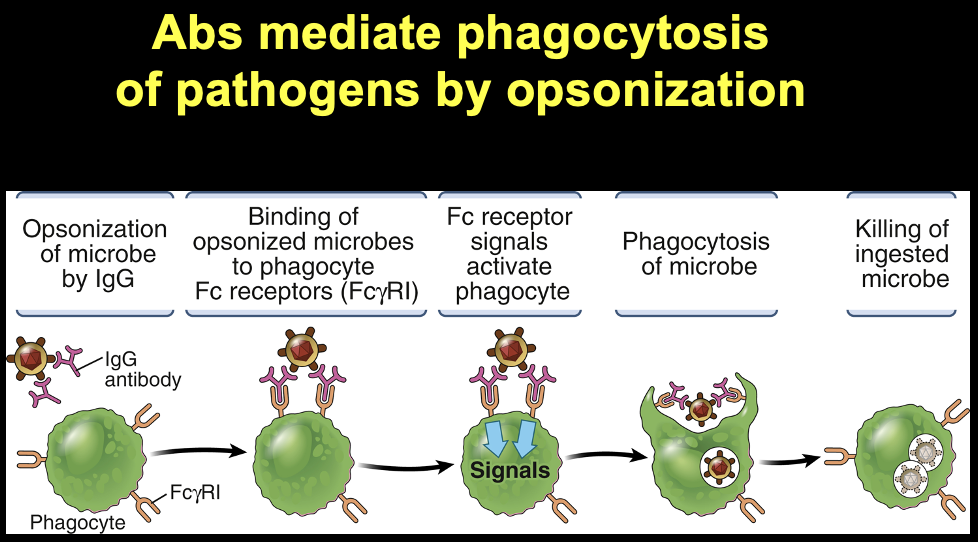
- opsonization of microbe by IgG
- binding of opsonized microbe to phagocyte Fc receptors (FcyRI)
- Fc receptor signals activate phagocyte
- phagocytosis of micropbe
- killing of ingested microbe
Phagocyte has receptors on surface
1st (Fc) receptor binds constant region on the antibody
Fc receptor is specific for the constant region
And binding site of antibody keeps microbe attached
èGets phagocyte to internalize the pathogen that is attached to antibody
This is not just physical action of antibody bindig – phagocyte grabbing
- things changed in phagocyte
activation of phagocytes and phagocytosis of pathogens requires Fc receptors
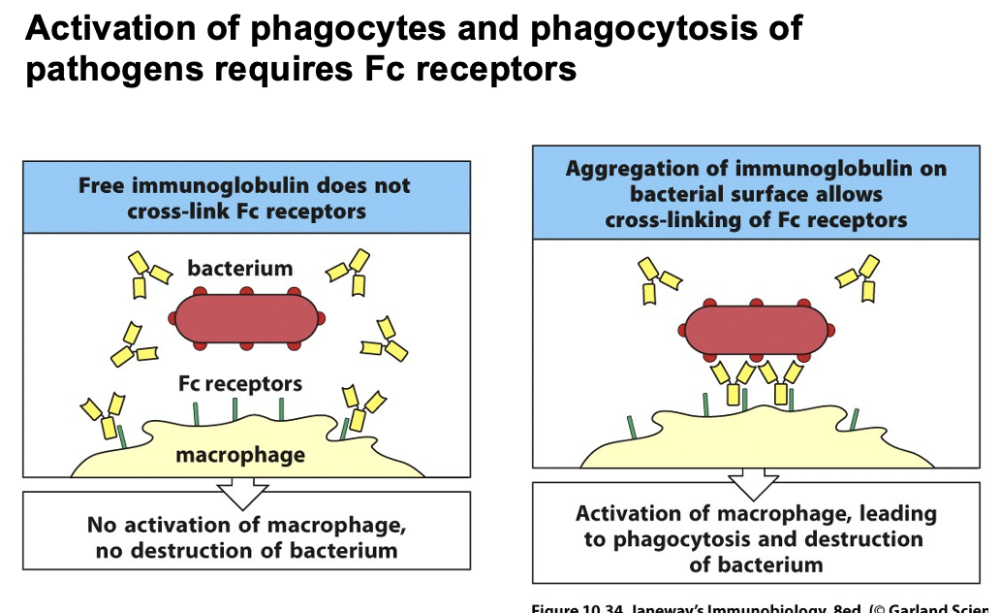
free immunoglobulin does not cross link Fc receptors
-> no activation of macrophage, no destruction of bacterium
aggregation of immunoglobulin on bacterial surface allows cross linking of Fc receptors
-> activation of macrophage, leading to phagocytosis and destruction of bacterium
notes:
- Free floating antibodies do not bind well to phagocyte
-
But when bound to pathogen, they bring Fc receptors together
to activate the phagocyte – now bc has pathogen, it can
bind well to phagocyte
- - cause intracellular signal transduction in the phagocyte and inside the phagocyte chemically changes
- -> phagocyte becomes activated -> phagocytosis
Ab dependent cellular cytotoxicity
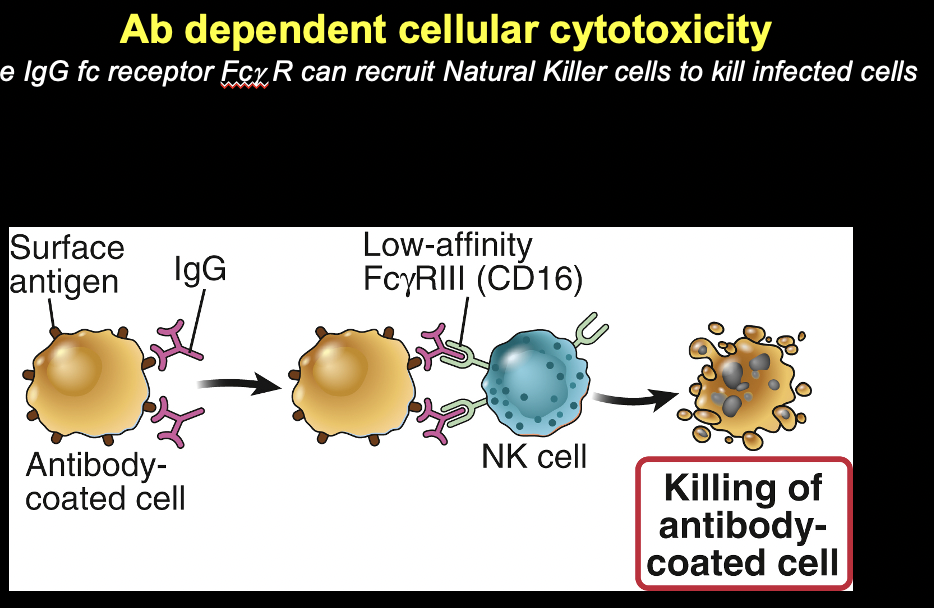
the IgG receptor Fcy R can recruit NK cells to kill infected cells
- IgG bind to surface antigen of antigen
- -> go to NK cell which binds the antibodies
- -> lead to killing of the cell w/ surface antigens
now bound to antigen on target cell that is infected
- when cells infection
- constant region recognized by NK cell -> forms holes and kills the infected cell
activation of NK cells requires Fc receptor cross-linking
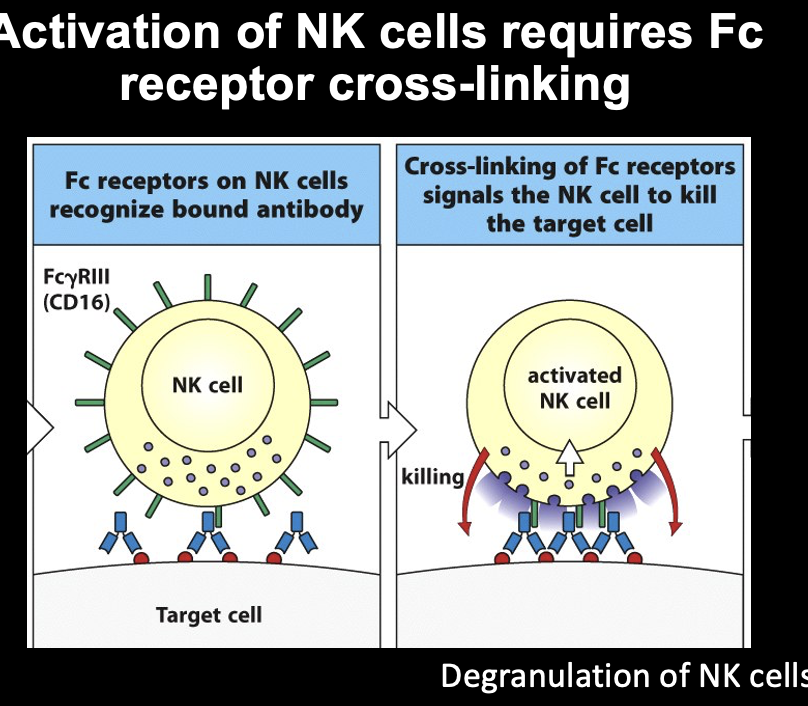
Fc receptors on NK cells recognize bound antibody
-> cross-linking of Fc receptors signals the NK cell to kill the target cell (via degranulation of NK cells)
Bind foreign antigen on our own cells
- recruit NK cells and activate them
Process happens fast
Ab neutralize toxins by blocking toxin from binding cellular
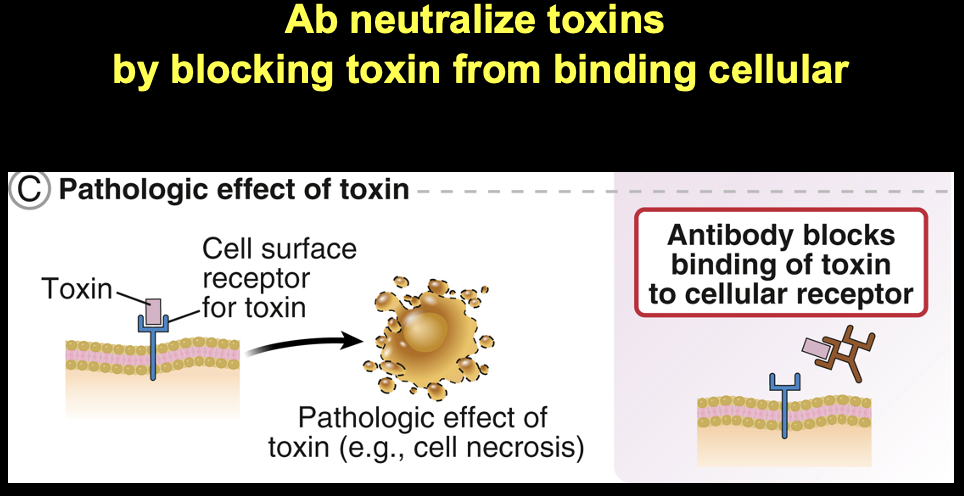
pathologic effects of toxin
- antibody blocks binding of toxin to cellular receptor
Another function of antibody
- neutralize a toxin (poison, can be from anything)
- toxins can be internalized by many cell types
- cause intracellular biochemical processes to be disrupted and cause cells to be dysfunctional, etc.
ex: toxins that cause paralysis of certain organs, etc.
can bind to circulating molecule
without immune cell participation (can do the job alone)
IgE binds to FcER1 and mediates degranulation of mast cells and eosinophils
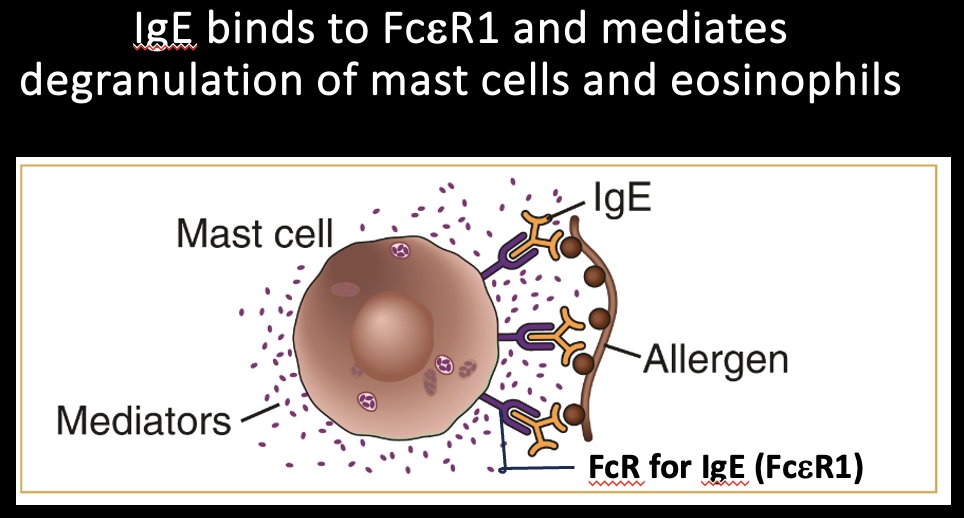
Some cells express Fc receptors that bind only certain constant regions
ex: mast cells and eosinophils express FcepsilonR1 which ONLY binds IgE
-> bind thru Fc receptor
- bound antibody targets allergen/pathogen
- brings multiple Fc receptors together = Fc receptor cross linking
Common thing in immune cell activation is clustering of receptors. Happens often. Just like the T cell indepndent IgM cross linking I think?
IgE binding to FcER1 and crosslinking mediates degranulation of mast cells
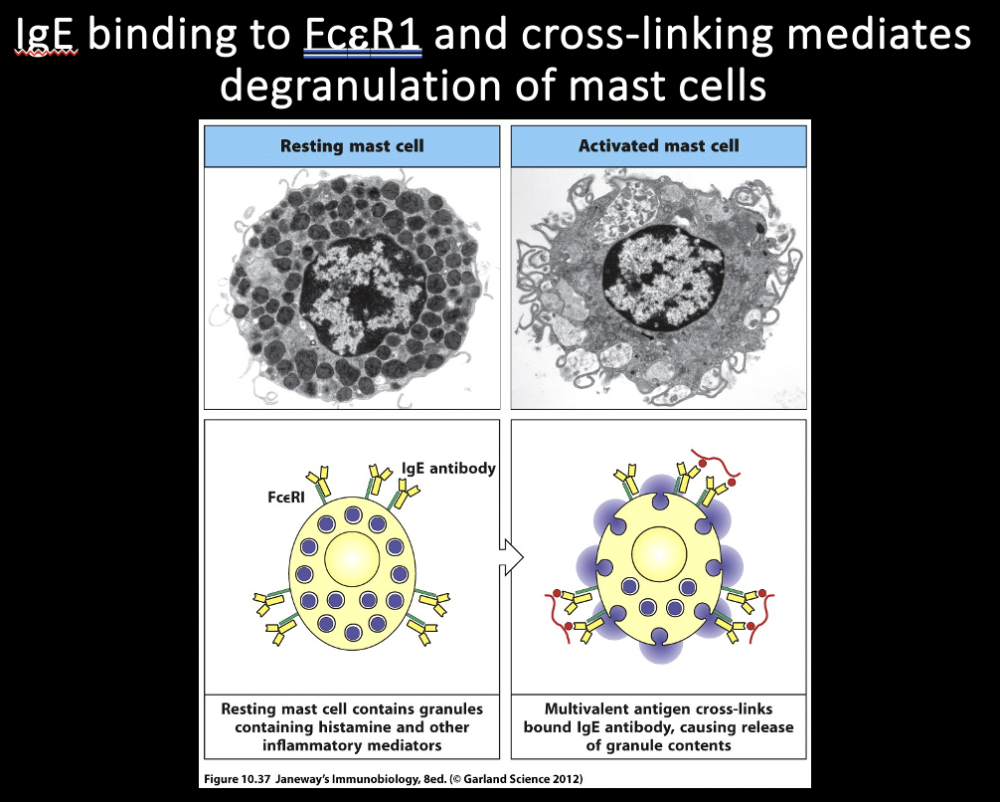
resting mast cell -> activated mast cell
resting mast cell contains granules containing histamine and other inflammatory mediators -> multivalent antigen crosslinks bound IgE antibody, causing release of granule contents
Antigen come, granules start secreting – doing degranulation
- how mast cell look after degranulation
degranulation of mast cells and eosinophils results in the expulsion of parasites
mast cells/eosinophils attack parasites
Mast cells bound to IgE specific to this parasite
Mechanism of getting rid of huge parasites
Releases histamine – mast cells
Fc receptors signal and the activation of innate immune cells
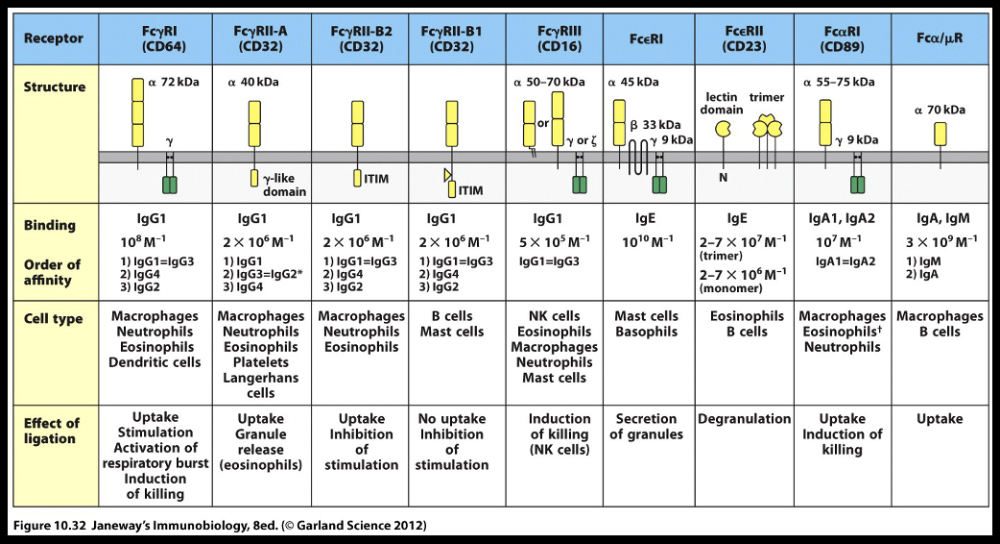
there are Fc receptors specific for each Ab class
How do diff antibody isotypes enhance their functional diversity?
pause for activity
Ab neutralize toxins by blocking toxin from binding cellular
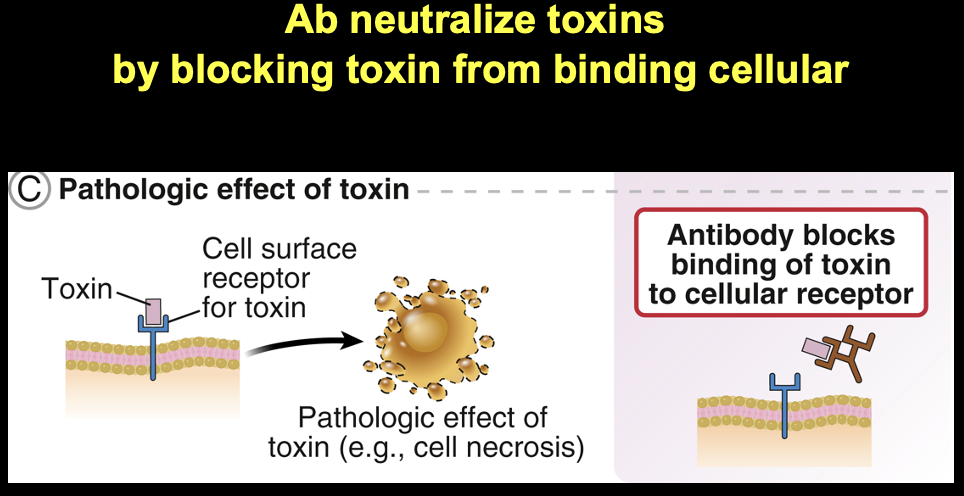
Carried out by antibody protein molecules by themselves
Cannot do this if have specific antibodies
binding of C1q to Ab initiates activation of the classical complement pathway
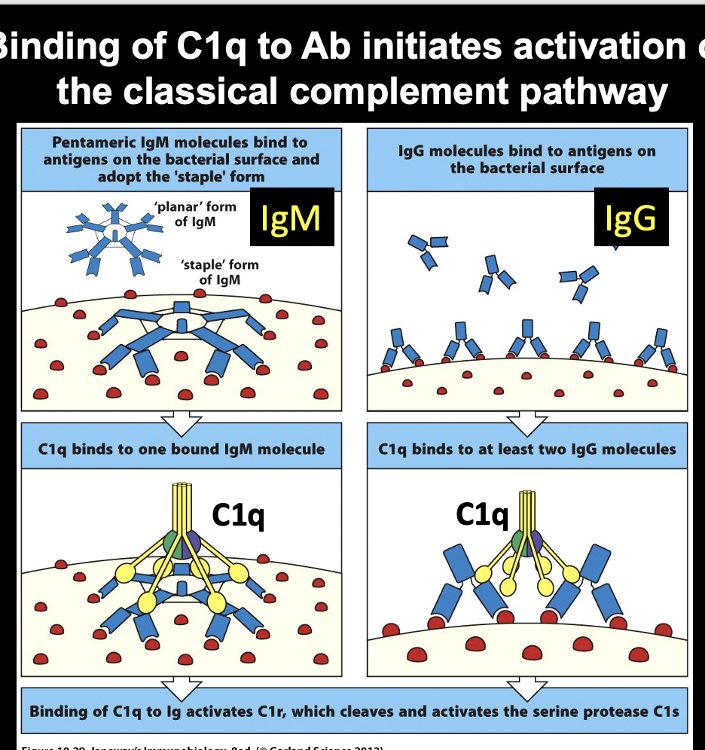
pentameric IgM molecules bind to antigens on the bacterial surface and adopt the "staple" form
-> C1q binds to one bound IgM molecule
-> binding of C1q to Ig activates C1r, which cleaves + activates the serine protease C1s
IgG molecules bind to antigens on the bacterial surface
-> C1q binds to at least 2 IgG molecules
-> binding of C1q to Ig activates C1r, which cleaves + activates the serine protease C1s
Antibodies can bind to targets that have multiple binding sites -> recruit binding + activation of complement
Important: IgM (despite poor affinity) overcomes the deficit by having multiple binding sites -> create complex that is good for activating complement
Same thing achieved by IgG.
HE WILL ASK ABOUT ON TEST:
2 functions of antbodies that are independent of other cells
answer: 1.Neutralize toxins 2.Activate complement
which 2 Ab functions can be performed without the help of other immune cells?
pause for activity
*** EXAM QUESTION ***
1- Toxin neutralization
2. Complement fixation (activation)
inhibition of BCR and FcR signaling
Immune system response can be destructive
Don’t want it to go on for longer than needed, would cause more disease than pathogen would
- excessive/prolonged immune response is BAD and cause many problems
Then how do u calm active immune response?
- mechanisms to turn off response – we will discuss this in terms of B cells
FcRs activate innate cells
ITAM, immunoreceptor tyrosine based activation motif
Fc receptord activcate innate cells bc they have ITAM In their cytoplasm
- very potent
B cells express FcR that inhibit B cell activation
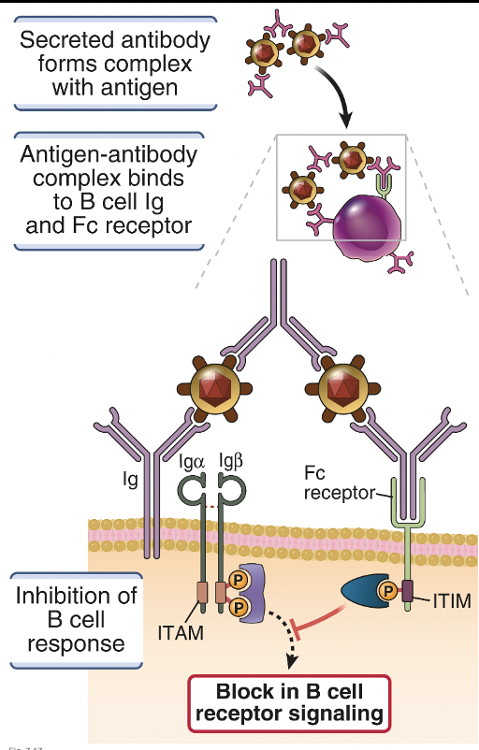
ITAM, Immunoreceptor Tyrosine Based Activation Motif
ITI(?)M, Immunoreceptor Tyrosine Based Inhibition Motif
Antibody bound to target
Specific clone of B cell also has same specificity
So these floating complexes w/ Fc come back and bind Fc receptor on B cell
Antibody bring antigen to bind to original B cell receptor, and antibody is bound to Fc receptor
- Fc receptor carries inhibitory motif (ITAM)
usually tyrosine kinase is necessary for activation in the cells by phosphorylation, initiating signaling cascade to activate B cell
ITIM motif has activity to recruit phosphatase – disrupts the process of activation and phosphorylation is STOPPED
Presence of Fc gamma receptor on B cells bind to antibodies the B cell made(??? Idk what he was saying),
When they find B cells, they attenuate process of activation
- temper/reduce b cell actvation and can no longer be activated
FcR mediate Ab feedback inhibition of B cell activation
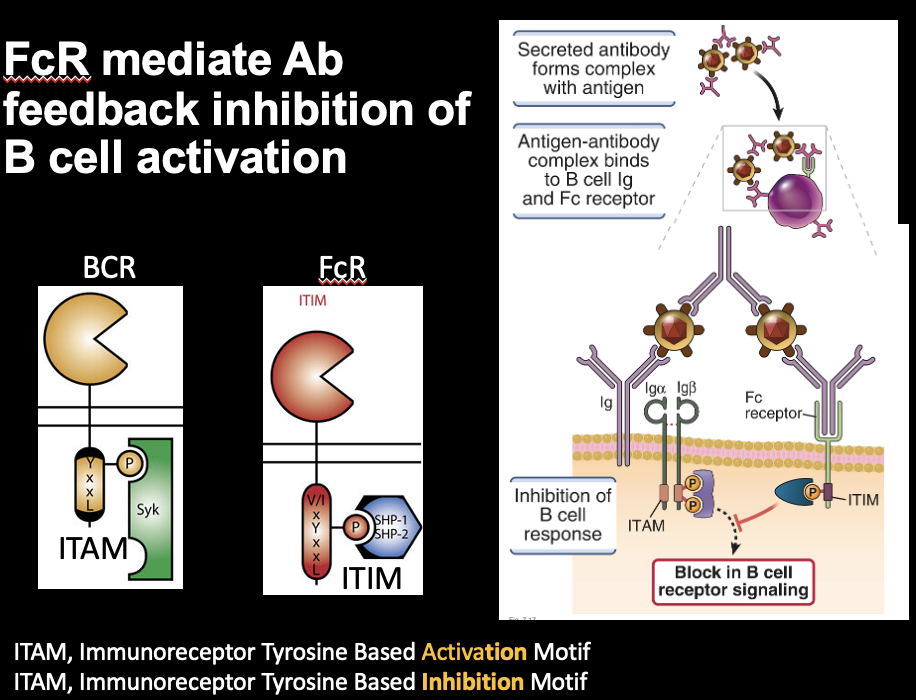
BCR activated motifs
FCR has inhibitory motifs?
Idk
How prevent excessive inflammation
Excessive inflammation causes most of damage
distribution and functions of immunoglobulin classes
- Antibodies of different classes operate in distinct places and have distinct effector functions.
- Transport proteins that bind to the Fc regions of antibodies carry particular isotypes across epithelial barriers.
- High-affinity IgG and IgA antibodies can neutralize bacterial toxins.
- High-affinity IgG and IgA antibodies can inhibit the infectivity of viruses.
- Antibodies can block the adherence of bacteria to host cells.
- Antibody:antigen complexes activate the classical pathway of complement by binding to Complement.
- Antibodies inhibit BCR activation signaling through inhibitory Fc receptors