What is shock?
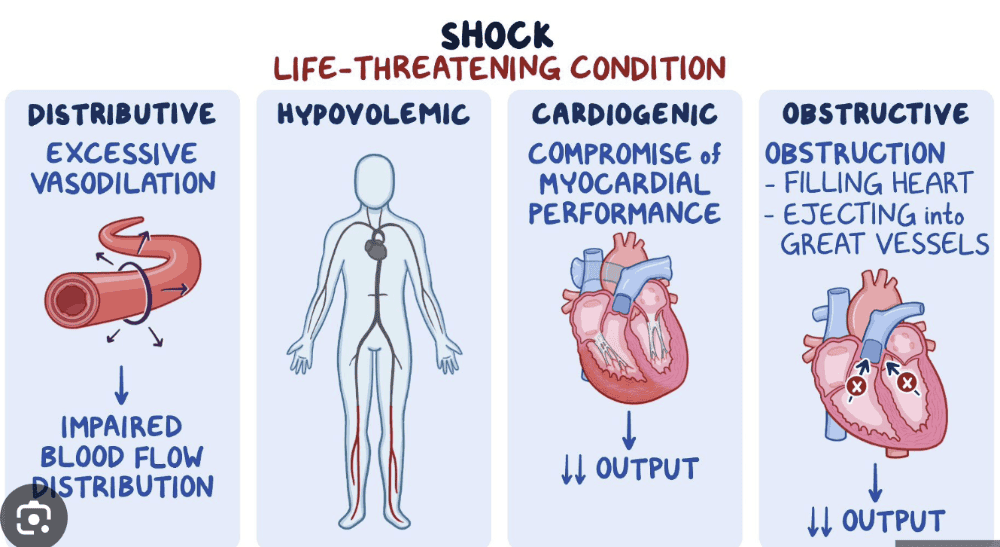
What are different classifications of Shock?
- Is a condition during which the cardiovascular system fails to perfuse the tissues adequately --> results in cellular hypoxia
- Causes general and widespread impairment of cellular metabolism
Types
- Cardiogenic (caused by heart failure)
- Hypovolemic (caused by insufficient intravascular fluid volume)
- Obstructive Shock
- Distributive Shock
- Neurogenic or vasogenic (caused by alterations in vascular smooth muscle tone)
- Anaphylactic (caused by hypersensitivity)
- Septic (caused by infection)
Pathophysiology of Shock :
IMPAIRMENT OF CELLULAR METABOLISM BY SHOCK
- Impairment of cellular metabolism
- Shift from aerobic to anaerobic metabolism
-
Loss of the ability to maintain an electrochemical gradient
- Accumulation of sodium and chloride in the cell
- Water follows, thus reducing the extracellular volume
- K exits cell
- Activation of coagulation pathway
- Impaired oxygen use, regardless of cause
- Impaired glucose delivery and use
- Impaired delivery or uptake
- Cells shifting to glycogenolysis, gluconeogenesis, lipolysis
- Gluconeogenesis causes proteins to be used for fuel, thus no longer available for maintaining cellular structure, function, repair, and replication
- Toxic ammonia and urea production
- Metabolic acidosis
- Glycogenolysis and lipolysis contribute to cellular failure
Clinical Manifestations of Shock
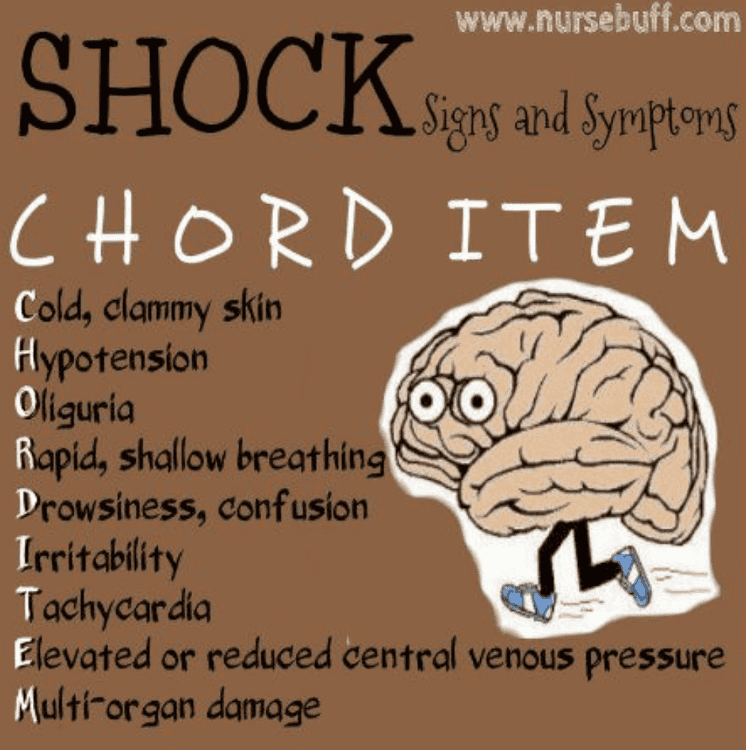
Clinical manifestations
- Weak, cold, hot, nauseated, dizzy, confused, afraid, thirsty, short of breath, and generally “feeling sick”
- Decreased blood pressure, cardiac output, and urinary output
- Increased respiratory rate
Treatment
- Oxygenation: Absolute necessity in all shock states
- Correct or remove underlying cause
- Provide supportive therapy
Cardiogenic Shock
What is failing?
Patients show low/decreased _____, ____, _____?
- "heart fails to pump blood"
- Inability of the heart to pump adequate blood to tissues and end organs from any cause
-
Patients with cardiogenic shock have decreased
- hypotension
- hypoperfusion
- cardiac output
Causes of Cardiogenic Shock

Cardiogenic shock may occur due to:
- Myocardial infarction (most common)
- Myocardial Ischemia
- Acute mitral valve regurgitation due to papillary muscle rupture
- Sustained arrhythmias/dysthymias
- Severe dilated cardiomyopathy
- Cardiac surgery
1. cardiomyopathy, sepsis, myocarditis, pericarditis, aneurysm, dysrhythmias, contusion, metabolic abnormalities, and papillary muscle rupture
2. impaired diastolic filling related to dysrhythmias
3. obstruction attributable to pulmonary embolism, cardiac
tamponade, valvular
disorders, tumors, and wall rupture or defects.
Dysrhythmias or conditions related to post–cardiopulmonary
resuscitation reduce
cardiac function and output
Cardiogenic Shock S/S?

- Chest pain
- Dyspnea
- Faintness
- along with feelings of impending doom
-
Classic hallmarks:
- Tachycardia
- Tachypnea
- Hypotension
- Jugular venous distention
- Dysrhythmia
- Low measured cardiac output
- cyanotic lips, nail beds, and skin
- Hypotension, oliguria, and cool skin Cyanosis; skin mottling
-
rapid, faint, or irregular pulses; low urine output; and
occasional
peripheral edema are additional signs and symptoms of end-organ
hypo perfusion - Pulmonary edema increases as volume accumulates and expands from the heart into the lungs as crackles wheezes
Treatment of Cardiogenic Shock
-
Medications
- Fluids
- Cardio supportive drug
- Fibrinolytic therapies: To disintegrate coronary thrombus
-
Assist the pump
- Pacemakers
- Internal defibrillator devices
- Implantable VADS
- Intra-aortic balloon pump (IABP) or percutaneous or ventricular assist devices (VADS)
-
Percutaneous interventions
- Balloon angioplasty
- Stent placement
- Thrombectomies
-
Surgery:
- Coronary artery bypass
- ventriculoplasty
- heart transplantation
What is Hypovolemic Shock?
- Insufficient intravascular fluid volume
Causes of Hypovolemic Shock
-
loss of whole blood
- Hemorrhage
-
plasma loss
- burns: increase in capillary permeability due to heat effect and damage causes plasma to leak out from capillaries to interstitial spaces
-
interstitial fluid loss
- emesis
- diuresis
- diaphoresis
- diabetes mellitus /insipidus
Hypovolemic Shock S/S?
"CHART"
- C: cool extremities, cyanosis. pale
- H: hypotension, High SVR (SVR increases due to the body’s attempt to compensate for the loss in volume)
- A: Altered LOC
- R: rapid/weak HR, reduced urine output
- T: thirst increased, tachycardia
- low systemic and pulmonary preloads
Hypovolemic Shock Compensatory Mechanism
- Compensatory vasoconstriction, increased systemic vascular resistance (SVR), and afterload
- To improve blood pressure and perfusion to core organs
SNS
- Heart rate and vasoconstriction increase as a result of catecholamine release by the adrenals
Liver and Spleen
- The liver and spleen add to blood volume by disgorging stored red blood cells and plasma
Kidney- RAAS
- In the kidneys, renin (through several intermediaries)
stimulates aldosterone release and the retention of sodium (and
hence water)
- Antidiuretic hormone (ADH, or vasopressin) from the posterior pituitary gland increases water retention.
Treatment of Hypovolemic Shock
Treatment
- Prompt control of hemorrhage
- Fluid replacement
What happens Distributive shock?
What are characteristics of Distributive Shock ?
aka vasodilatory shock
- distributive shock is a form of shock in which severe vasodilation despite normal blood volume results in improper distribution of blood flow
-
Characterized by
- loss of blood vessel tone
- enlargement of the peripheral vascular compartment (large diameter blood vessels)
- displacement of the vascular volume away from the heart and central circulation
- In distributive shock, the capacity of the vascular compartment expands.
Type of Distributive
- Neurogenic shock
- caused by decreased sympathetic
control of blood vessel tone due to a defect in the vasomotor center in the brain stem or the sympathetic outflow to the blood vessels (e.g. spinal cord injury)
- caused by decreased sympathetic
- Anaphylactic shock
- caused by a severe systemic allergic reaction.
- it is an immunologically mediated reaction
in which vasodilator substances such as histamine are
released into the blood
- Septic shock
- systemic immune response to severe
infection. It is the most common type of distributive shock
- systemic immune response to severe
- Patients with Distributive shock have blood vessel dilation and warm skin in contrast to other shock types
What is Neurogenic Shock?
What disbalance between systems is happening?
widespread and massive vasodilation that results from an imbalance between parasympathetic and sympathetic stimulation of vascular smooth muscle
Causes of Neurogenic Shock
- Trauma to the spinal cord
- Trauma to the medulla
(Lack of food and O2)
- conditions that interrupt the supply of oxygen to the medulla
- conditions that
deprive the medulla of glucose (e.g., insulin reactions) can
cause neurogenic shock
by interrupting sympathetic activity.
- Depressive drugs, anesthetic agents
- severe emotional stress and pain are other causes
of
neurogenic shock
Clinical Manifestation NS
Clinical hallmark of neurogenic shock is a very low SVR, bradycardia, fainting
Anaphylactic Shock
outcome of a widespread hypersensitivity to an allergen that triggers a reaction known as anaphylaxis.
-
caused by a severe systemic allergic reaction. It is an
immunologically
mediated reaction in which vasodilator substances such as histamine are released into the blood. - Production of mast cells, immunoglobulin E (IgE),
and
low-affinity IgE receptor (FceRI) is induced by cellular response to the
antigen - Physiologic alterations related to the inflammatory and immune response, similar to neurogenic shock, are massive; vasodilation, peripheral pooling, and relative hypovolemia lead to decreased tissue perfusion and impaired cellular metabolism
Clinical Manifestations of Anaphylactic Shock
Anaphylactic shock is often severe and has immediate symptoms:
- itchy rash
- throat swelling
- low blood
pressure: related to the massive vasodilation and
systemic
inflammation
Symptoms often affect multiple organ systems, including
- gastrointestinal (e.g., nausea, abdominal pain, vomiting, diarrhea)
- cutaneous (e.g., erythema, pruritus, urticaria, or angioedema),
- respiratory (e.g., shortness of breath, cough,
rhinorrhea, tightening of
throat, difficulty swallowing, wheezing) - cardiovascular (e.g., diaphoresis, pallor, hypotension), or hematologic (e.g., fever, hemolysis).
Treatment of Anaphylactic Shock
- Treatment begins with removal of the antigen (if possible).
- Epinephrine is administered to decrease
mast
cell and basophil degranulation, cause vasoconstriction, and reverse
airway constriction - Volume expanders (e.g., lactated Ringer solution) are given intravenously to reverse the relative hypovolemia
- antihistamines and corticosteroids
are given to stop the
inflammatory reaction
Septic Shock
disease process begins with infection entering the bloodstream and causing bacteremia.
Sepsis Criteria
-
SIRS has
4 criteria: -Temp > 38 or Temp < 36
-Heart rate > 90
-RR > 20 or PaCO2 < 32
-WBC >12,000 or WBC < 4,000 or >10% Bands - The patient must have a suspected/proven infection and fulfill at least 2 of the SIRS criteria to be defined as septic.
Important Notes of Sepsis
Two main mechanisms contribute to lactic acid accumulation in sepsis:
- tissue hypoxia
- epinephrine-induced stimulation of aerobic glycolysis.
- The patient with sepsis is at risk of developing shock through the loss of systemic vascular resistance
- A patient has severe sepsis if they fulfill sepsis criteria and have organ dysfunction, hypotension, lactic acidosis, oliguria, or mental status changes.
- Elevated procalcitonin (PCT)
level indicates a nonspecific
proinflammatory response seen in bacterial infection - C-reactive protein (CRP) is an
acute
phase reactant protein produced by the liver, mainly in response to
interleukin-6 produced by inflammation of any type. CRP is most
sensitive to acute phase reactants; consequently, its level rises rapidly
during inflammation. Similarly to PCT, CRP is nonspecific to types of
inflammation, but may be used to trend severity of infection and
response to treatment, especially in occult and resistant infections,
such as osteomyelitis.
Treatment of Sepsis
- Pharmacologic hemodynamic support and adjunctive therapy
to
maintain tissue perfusion include vasoactive agents. - Norepinephrine is now considered the initial vasopressor of choice
- Dopamine, epinephrine, phenylephrine, and vasopressin
are alternatives;
however, these are less preferred because of potential tachycardia,
dysrhythmias, or reduction in splanchnic blood flow. - Pharmacologic hemodynamic support and adjunctive therapy to maintain tissue perfusion include vasoactive agents.
- Norepinephrine is now considered the initial vasopressor of choice
- Dopamine, epinephrine, phenylephrine, and vasopressin are alternatives; however, these are less preferred because of potential tachycardia, dysrhythmias, or reduction in splanchnic blood flow
Complications of Shock
- Acute lung injury/acute respiratory distress syndrome
(ALI/ARDS)
- Rapid and profound onset of dyspnea that can be caused by shock.
- Acute kidney injury (AKI)
- Impaired renal perfusion that occurs in response to decreased intravascular volume.
- Gastrointestinal complications
- Patients may develop gastrointestinal ulcers and bleeding.
- Disseminated intravascular coagulation
- Widespread activation of the coagulation system with resulting clots and thrombotic occlusion of vessels as well as bleeding.
- More commonly occurs as a consequence of gram-negative (bacteria) sepsis
- Multiple organ
dysfunction syndrome
- Malfunctioning of multiple organ systems as a consequence of shock
MODS
organ injury is directly associated with a
specific insult, most
often ischemia or impaired perfusion from an
episode of shock or
trauma, thermal injury, soft tissue necrosis, or
invasive infection
Obstructive Shock
- Obstructive shock occurs due to mechanical obstruction of the blood flow through the circulation
Causes of Obstructive Shock
- Obstructive shock can be due to:
- Pulmonary embolism (most common)
- Cardiac tamponade
- Pneumothorax
- Dissecting aortic aneurysm