10/19
TB therapeutics
1882-1950
post germ/pre therapy era of TB
- "huge commercial system of quakery and posion"
- post germ - we know what causes the disease + took years before relief a couple generations later
-
"cures" for TB always were around, even
pre germ
- there were cures that didnt work (like
"quackery")
- ex: like the pink pills
- there were cures that didnt work (like
"quackery")
on the lake - movie assigned to watch. this is the slide that he discusses it
thinking of time - thought sanitariums could slow things down + relieve symptoms (area/air cound help fight it or something)
some ppl thought TB was hereditary
microbacterium - can start in lungs + spread to rest of body if immune system cannot keep it localized in lungs - rely on immune system to keep it localized
everyone was getting the disease - many things determined treatment would recieve (like racial status, etc.)
TB was and is the biggest infectious disease killer in the world (except for the time of covid)
mycobacterium tuberculosis and lung pathology
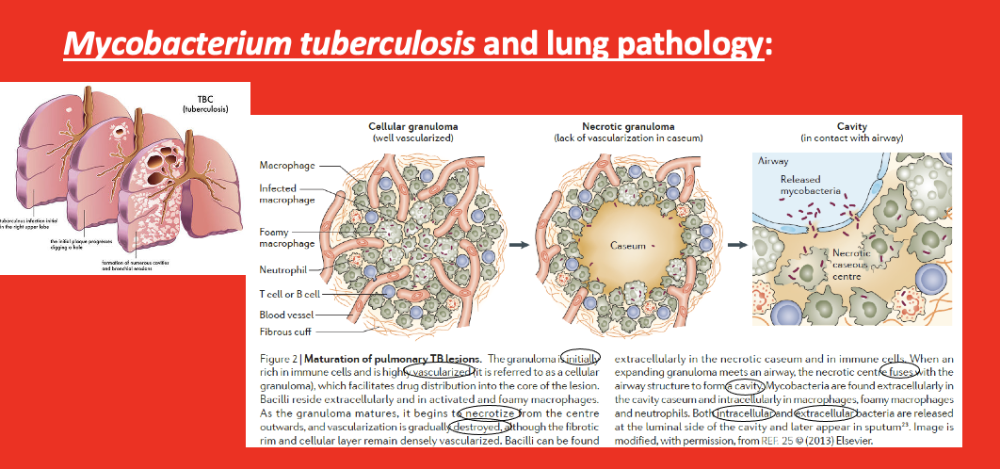
CRUCIAL SLIDE
- 2 nd pic from left – granulomas – form in lung when infected with mycobacterium TB
-
granuloma =
general term – any collection of mutant cells(immune cells? I
think he may have said immune cells not mutant cells)
- young and mature granulomas (one seen in pic is
young – just formed)
- key in young granuloma = well/highly vascularized
- as granuloma matures – w/ time the center of it – cells start to die = caseum (dead cells in center)
- the center loses blood supply ( vascularilzation becomes gradually destroyed)
- * vascularization is KEY – if LOSE it (if granuloma less vascularized), then cannot reach the granuloma with IMMUNE SYSTEM (no blood to reach it thru) and DRUGS (drugs cannot reach it thru blood) if no blood flow
- *** this is present in ¼ earth’s population – live mycobacterium TB – will have for rest of their life (stable, mycobacterium stays contained in granuloma). Same granuloma may remain for decades
- young and mature granulomas (one seen in pic is
young – just formed)
*** 90% of these ¼ population will NEVER suffer from this – will remain asymptomatic for rest of their lives
*** other 10% who have this -> go to next stage (can happen at any time, decades later, etc.)
- granulomas begin to fuse w/ airways -> form cavities (right pic) = bacteria are intra and extra cellular ->extracellular bacteria releases on luminal side of the cavity – the side that is continuous with outside atmosphere
- everytime person coughs – releasing mycobacterium into environment
(latent infection, 90% of ppl with it = noninfectious. ONLY the 10% discussed can spread it / are infectious)
- Know in the 10% of ppl who have advanced TB, its not that they get bigger, but the granulomas begin to fuse w/ airways/ airsacs = pathway to infect others thru cough
LTBI and "active" TB
a spectrum of pathology and clinical symptoms
asymptomatic -> symptomatic
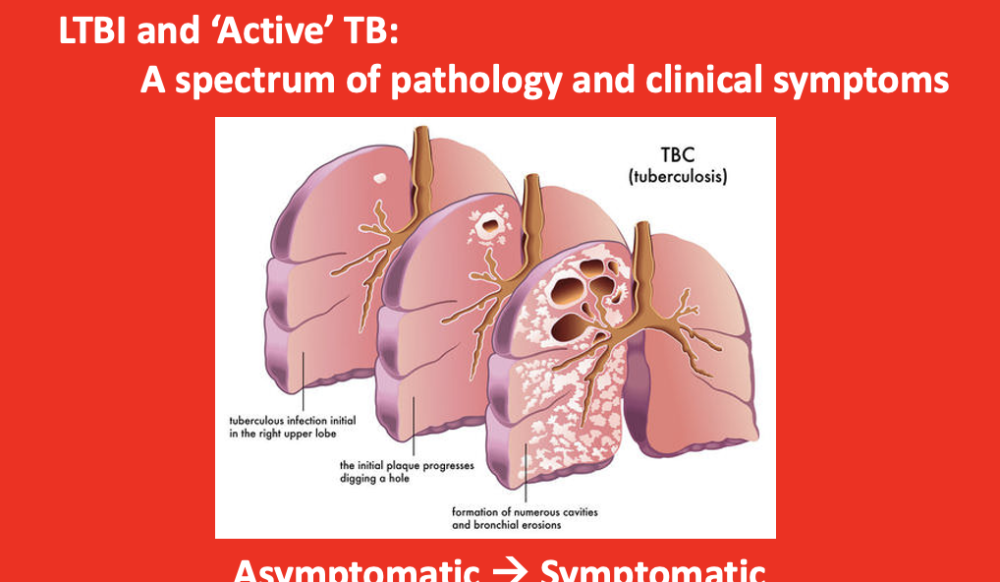
Latent TB infecion – LTBI
Active TB – have symptoms, like coughing
- if the 10%, granulomas grow + fuse w/ airways = cavities form = promote spread of pathogen within the lung and to others (infectious)
- here is where person feels sick (leave asymptomatic stage + become symptomatic w/ disease)
TB therapy history
coincidence - 2 discoveries / breakthroughs in mid 40s - drug active could kil mycobacterium in test tube (in vitro)
- SM - killed it pretty well
- natural compound made by bacteria named
- in sweden made drug (PAS) man
made (synthetic) drug
- discovered it was very active, specifically to kill mycobacterium TB in test tube
1944: streptomycin (SM) discovered by selman waksman
- produced by soil bacterium streptomyces griseus
- targets prokaryotic ribosome (interferes w/ protein synthesis)
1944: antimycobacterial activity of para-amino salycylic acid (PAS)
- discovered by jorgen lehmann
- synthetic compound
- mechanism of action only recently described
para-aminosalisylic acid is a prodrug targeting dihydrofolate reductase in mycobacterium TB
Found out completely how drug works (mechanism) only about 10 years ago
- complicated
1882 - 1950s
- post-germ / pre therapy era of TB (palliative)
post 1950s
- therapeutic era of TB (curative)
later in 40s - 2 drugs were used in clinical studies - assess if could help ppl suffering from TB
- could it slow down progression of TB?
- in 1950 -
published paper w/ results - found ppl treated w/ combination
responded the best
- if treated w/ both together - best outcome in terms of slowing down progression of TB in ppl
- finding in paper - recognized as bringing world into therapeutic stage of TB (curative)
- could not cure ppl right away - took at least a decade
to figure out right drug combinations
- but this was the start
- at this point - not only treatable but have curative drugs
TB therapy history
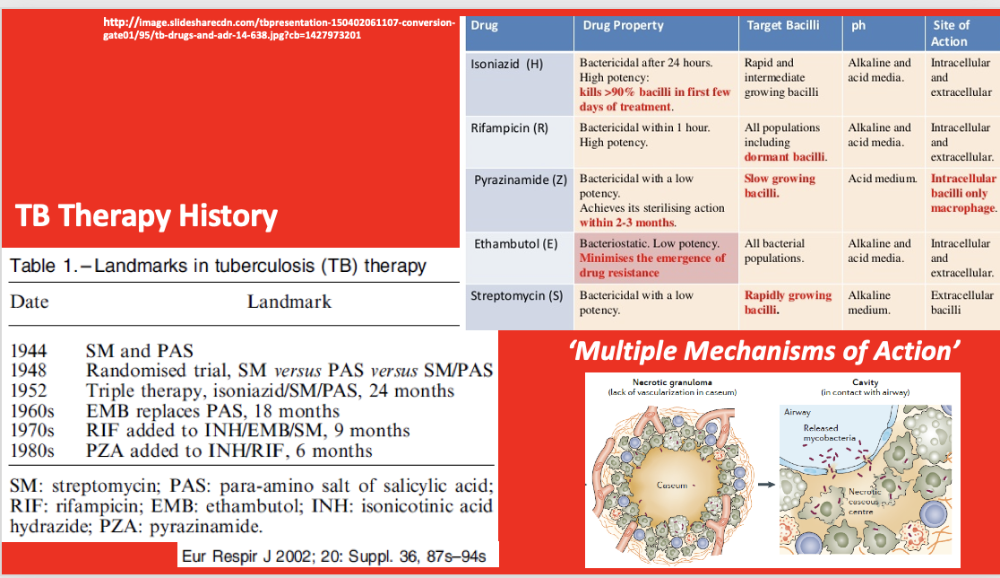
HOWEVER - even WITH drugs - is NOT easy to cure TB
timeline in pic
- came up w/ 4 "fronline drugs" for TB
- even
with these drugs - not easy to treat someone with TB
- no blood supply - HIGH DOSE + LONG TIME OF TREATMENT
- even
with these drugs - not easy to treat someone with TB
current drug treatment regimen for "active" TB
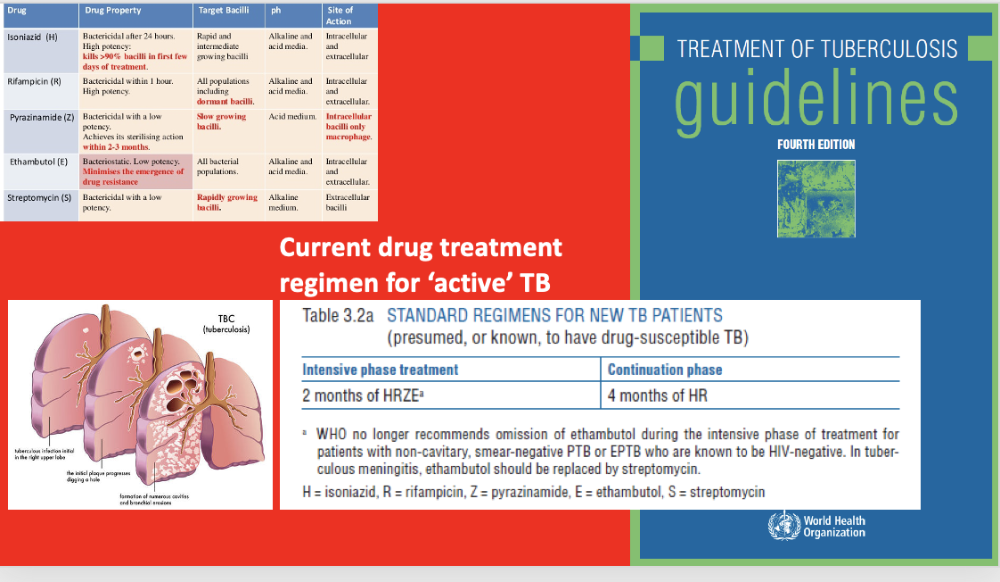
drug regimen for active TB (for ppl symptomatic)
- 2 months of the 4 drugs
- after that, continue with 2 of the drugs for 4 months
the drugs are intense - take a toll on body
- takes a lot to get rid of mycobacterium
LTBI and "active" TB
a spectrum of pathology and clinical symptoms
if NOT active (asymptomatic) - dont have to be as brutal in treatment
diff treatment for latent TB - state of persistent immune response to stimulation by mycobacterium TB antigens without evidence of clinically manifested active TB
- (see in slide)
- direc measurement toll for M. TB infection in humans is currently unavailable
- majority of infected persons have no signs or symptoms of TB but are at risk for developing active TB disease
- this can be averted by preventative treatment
another thing abt granuloma - mystery of TB latent infections - very few bacteria in granulomas
- in the granulomas - cant find mycobacterium even though know theyre there
current drug treatment regiment for LTBI
Current treatment for latent TB
- active TB only has 1 option
- latent has options
why hasnt TB been eradicated?
- LTBI is silent
- compliance
- drug resistance (generally true for all pathogens)
how does mycobactetia/TB resemble/differ from HIV/AIDS in this regard?
Pulled up WHO list of essential medicines
For active TB: the 4 frontline drugs used are: ethambutol +isoniazid + pyrazinamide + rifampicin
Certain drugs for drug-resistant mycobacterium
Fixed doses = options for latent TB
- leprosy caused by diff species of mycobacterium
In theory – could eradicate TB bc have curative drugs
- so then why still have it in world?
Because:
- LTBI is silent – ppl wont get tested if feel fine, and if test +, ppl not motivated to treat it bc they feel fine
- Compliance – how can keep ppl to take the treatment? Ppl do not stay on treatment always
- Drug resistance – eventually strains are resistant to the antibiotic
How differ form HIV/AIDS – cureative . Although there are some of same challenges (like compliance, etc.)
resistance strain classifications
- multi drug resistant TB (MDR-TB)
- at minimum - resistant to isoniazid (H) and rifampicin (R)
- extensively drug resistant TB (XDR-TB)
- MDR-TB plus resistant to second-line TB drugs
- If TB bacteria are found in the sputum, the diagnosis of TB can be made in a day or two, but this finding will not be able to distinguish between drug-susceptible and drug-resistant TB. To evaluate drug susceptibility, the bacteria need to be cultivated and tested in a suitable laboratory. Final diagnosis in this way for TB, and especially for XDR-TB, may take from 6 to 16 weeks.
XDR – extensively resistant TB – pick up additional resistance to second line drugs (2 nd line of defense)
Way resistance can
Challenge in public health – how do you know you are dealing with antibiotic resistance mycobacterium?
- even difficult in the lab
russia suffering particularly from TB drug resistant TB
...
rifampicin (R) activity and how mycobacteria can become resistant to it
1 way how mycobacterium can become resistant (general way can occur in various bacterium)
- rifampicin – interferes w/ gene expression – blocks ability of mycobacterium to express the genes
Can mutate enzyme in way antibiotic can no longer bind to it
- genetic mutation on gene encoding enzyme – altered form makes so no longer bound/targeted by antibiotic
This is ONE way bacteria can become resistant to antibiotics
immune directed approaches
- bacillus calmette-guerin (BCG) vaccine
- The most controversial aspect of BCG is the variable efficacy found in different clinical trials, which appears to depend on geography. Trials conducted in the UK have consistently shown a protective effect of 60 to 80%, but those conducted elsewhere have shown no protective effect, and efficacy appears to fall the closer one gets to the equator.
- Like HIV, we only have limited success in terms of vaccines w/ TB BCG – strain of mycobacterium (attenuated – doesn’t cause disease) – is a live vaccine that is used to try to obtain immunity - problem – limited efficacy – doesn’t work all the time - don’t understand why vaccine works in some parts of world better than other parts of the world - not used in many countries where TB is not a threat (like the US)
anti-microbial drugs and antibiotics (from nature) remain the most effective approach against TB
LTBI and active TB
a spectrum of pathology and clinical symptoms
Like HIV, this is best fought w/ drugs / antibiotics – no strong vaccine