What is the definition of: Enzyme
reduces the activation energy of a reaction. Acts as a catalyst. (The Lock)
a protein that decreases the activation energy of a reaction
What is the definition of: Isoenzyme
:specific form of an enzyme, different isoenzymes can perform the same exact function, they just look a little different, or they may go about it in a slightly different manner. (The color of the lock, or how the lock looks)
What is the definition of: Cofactor
: non-protein molecule necessary for enzyme activity (Tumblers inside the lock)
- inorganic and organic compounds that are required for full enzyme function
What is the definition of: Holoenzyme
The complete form of a functional enzyme unit complete with cofactors (Lock with the tumblers)
What is the definition of: Apoenzyme :
The enzyme portion of a Holoenzyme, may or may not be active (The casing around the lock. looks like a lock, but does it lock?
an inactive enzyme without its cofactor
What is the definition of: Coenzyme :
an organic cofactor, AKA prosthetic group. (The metal key guard that you rotate to the side to insert the key)
- organic cofactors that commonly have a structure related to vitamins
What is the definition of: Oxidoreductases
- Oxidize or Reduce substrates
What is the definition of: Transferases -
Transfer side groups (e.g. NH 3 ) between substrates
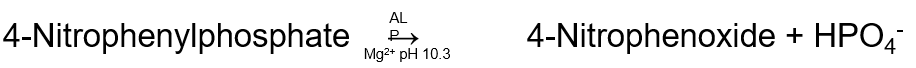
What is the definition of: Hydrolases -
Add water to break apart a substrate
What is the definition of: Lyases
- Breaks apart chemical bonds of a substrate
What is the definition of: Isomerases
- Interconvert between forms of a substrate (think transforming)
What is the definition of: Ligases
- Join together two organic substrates into one
Under what classification is thyroid peroxidase considered in a reaction which oxidizes iron?
Oxidoreductase
What is the summed up equation for enzyme.
S + E → ES → E + P
S = Substrate E = Enzyme P = Product
What is the primary function of enzymes?
To reduce the activation energy of a reaction. This will subsequently increase the likelihood that this reaction will occur, and the amount of product that is being formed.
What is the definition of zero order kinetics?
All of the enzyme binding sites are full and the enzyme is working at maximum capacity. A further increase in substrate concentration will NOT be able to increase the reaction speed.
What type of inhibition can be overcome by an increase in substrate concentration?
Competitive inhibition
What is the unit which we measure enzyme activity?
International Units
CYP450 Phase I metabolism has what predominant effect on drugs?
Simple reactions like hydroxylation, oxidation, or reduction to make the drug more water soluble.
A 23-year-old male living in Arizona is given a bottle of Ketoconazole for a coccidioidomycosis infection. He is also taking Phenytoin for his epilepsy that he has had since childhood. Ketoconazole is known to inhibit CYP450 enzymes in the liver. What effect would the addition of Ketoconazole likely result in for this patient?
A. Cause increased phenytoin activity
B. Render
phenytoin ineffective
C. Create a subtherapeutic phenytoin
level
D. Create a toxic phenytoin level
The correct answer is D) This is caused because it
is
metabolized by the CYP450 enzyme system. If Ketoconazole
inhibits this enzyme, then less phenytoin will be metabolized and more
will remain in circulation, causing more drug to be in the blood than
calculated. The Ketoconazole does NOT cause the phenytoin
to
become more active (A), nor does it render the phenytoin
ineffective (B), or create a subtherapeutic level of the drug (C).
Where do we want to measure enzyme concentration at on the
Michaelis-Menten curve?
A. With low substrate concentration on
the left
B. With low substrate concentration on the right
C.
With high substrate concentration on the left
D. With high
substrate concentration on the right
The correct answer is D) . When we have
an excess of substrate,
and we know how much enzyme we put in the reaction, we know exactly
how fast the reaction can go at different concentrations of enzyme.
With this knowledge, we then can compare the unknown sample to a
reference reaction speed to infer the concentration. All of the
available binding sites on the enzymes are occupied and the enzyme is
working as fast as it can. The rate is dependent upon how
much
enzyme there is in the reaction.
A patient’s enzyme kinetic assay is interpreted by your lab and you
see the Lineweaver-Burk plot. It appears that the patient has an
inhibitor to the enzyme in question. This inhibitor has decreased just
the Vmax, but not the K m . What is the inhibitor type?
A.
Competitive inhibitor
B. Irreversible inhibitor
C.
Noncompetitive inhibitor
D. Uncompetitive inhibitor
The correct answer is C) . The total Vmax is decreased, which
basically means that the inhibitor renders the bound enzyme obsolete
in catalyzing the reaction. Noncompetitive inhibitors bind to sites on
the enzyme other than the active site for the substrate, therefore,
they do not compete for the binding site. When
these
Noncompetitive inhibitors bind, they usually cause a
conformational change in the enzyme, which will block the substrate
from binding and the reaction from being
catalyzed. This effect
may be a permanent disfiguration of the enzyme or it may just be a
temporary one. This deformed shape may improve when the noncompetitive inhibitor
dissociates.
A male bodybuilder has an elevated Total CK value. Is this expected?
Yes, CK is positively correlated with muscle mass.
What is the subunits for: LD-1
HHHH
heart, RBCs, kidney. Are elevated in heart attacks
What is the subunits for:LD-2
HHHM
lungs, RBCs
What is the subunits for:LD-3
HHMM
spleen, lungs, and many tissues
What is the subunits for:LD-4
HMMM
liver and skeleton
What is the subunits for:LD-5
MMMM
liver and skeleton
What is the primary tissues and High-Yield defects which cause elevation for the following isoenzyme:LD-1
Primary tissues: Heart, RBCs
High-Yield defects which cause elevation: Myocardial infarction, hemolytic anemia
What is the primary tissues and High-Yield defects which cause elevation for the following isoenzyme:LD-2
Primary tissues: Heart, RBCs
High-Yield defects which cause elevation: Myocardial infarction
What is the primary tissues and High-Yield defects which cause elevation for the following isoenzyme:LD-3
Primary tissues: Lung, Lymphocytes, Pancreas
High-Yield defects which cause elevation:
Acute pancreatitis, pneumonia
What is the primary tissues and High-Yield defects which cause elevation for the following isoenzyme:LD-4
Primary tissues: Liver
High-Yield defects which cause elevation: Hepatic injury
What is the primary tissues and High-Yield defects which cause elevation for the following isoenzyme:LD-5
Primary tissues: Liver, Skeletal Muscle
High-Yield defects which cause elevation:
Hepatic injury, skeletal muscle injury
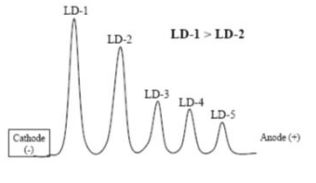
Edwin, a 42-year-old software engineer, falls into his double bacon cheeseburger, fries, and a shake at lunch and is unresponsive. He has no pulse and is rushed to the ER where he is diagnosed with a myocardial infarction. What would his LD isoenzymes look like?
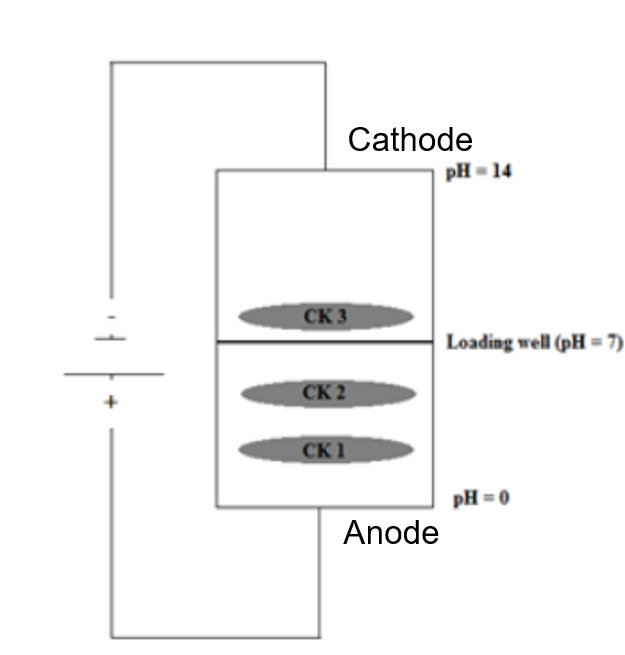
His LD isoenzyme panel would show the 1,2 Flip. LD-1 is higher than LD-2. This is a stereotypical pattern for patients with myocardial infarctions.
What are the 4 tissues that have the highest LD concentrations?
Kidney, Liver, Muscle, and RBCs
What is a common cause of elevated AST in a normal patient?
Hemolysis in the tube
What tissue is ALT found in primarily?
Liver
A 15-year-old African boy is taking medications after he was diagnosed with malaria last week. He now has hemolytic anemia. What genetic deficiency does he likely have?
G6PD deficiency
A 47-year-old anxious, obese female is complaining of shortness of
breath. She has had a strange sensation in her upper abdomen which
woke her up from sleep 3 days ago. She is concerned about the
possibility of gastric ulcers. From her online research over the past
3 days, she learned about this scary thing called ulcerative colitis
and thinks she has it. While these both could be possible, the astute
ER physician rapidly orders a CK-MB which comes back as slightly
elevated, but not alarming at all. What assay could her physician
order to help determine if she had a heart attack almost 4 days
ago?
A. CK-MB
B. Lactate Dehydrogenase
C.
Myoglobin
D. Total CK
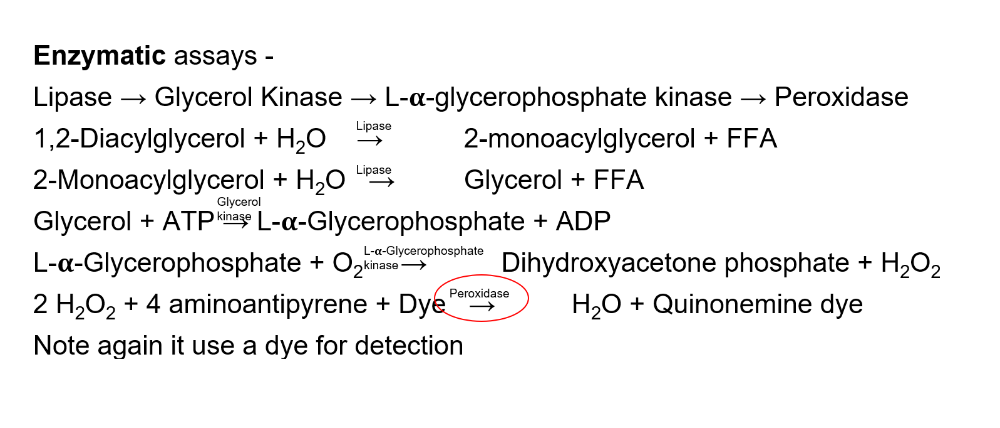
The correct answer is B) Other cardiac biomarkers that would help out
in this scenario would be any of the troponins, Tn-I, Tn-C, or Tn-T.
Remember that these biomarkers stay elevated for a long time after the
other acute biomarkers have dropped off in concentration. Tn elevates
quickly and remains elevated for a long time, that makes this marker
the most specific marker when we are trying to determine a distant
heart attack. LD can come from many sources, so it is not as specific
to the heart.
An elevation in LD should probably be followed up
with a more specific marker, like Tn.
A 28-year old female comes into the ED and is confused. She is
afebrile, floridly jaundiced and unaccompanied by any of her family or
friends. Upon further questioning, the patient reveals a family
history of lupus, Graves’ disease, autoimmune hepatitis, and type 1
diabetes. She said that she was at a bar with her friends, but does
not remember how she got to the hospital. The ED physician gets the
following results from the tests ordered:
INR: 2.9 AST: 7x the
upper limit of normal ALT: 5x the upper limit of normal
What is
the most likely cause of this condition?
A. Alcoholic
hepatitis
B. Autoimmune hepatitis
C. Hepatitis D
infection
D. Bacterial hepatitis
The correct answer is B) There’s a lot going on in this
question,
so let’s break it down a little bit at a time. What I
wanted you to pick up on, is that she only has one suggestion that
she’s here for alcoholic hepatitis, but the AST/ALT ratio is only 1.4,
so it means that she might have been drinking tonight, but she maybe
does it
once a year or so, not often enough to cause lasting
liver damage, because her DeRitis ratio is less than 2. Her clinical
history is quite suspicious for an autoimmune disease. First, she’s a
female, and females get them a lot more often than males do. Next,
she
has a family history of autoimmune diseases, which places her
at an increased risk. Next is the prognostic sign of the productive
capacity of the liver. We create most of our clotting factors in our
liver, and if our liver is damaged, then we can’t produce as many of
them. Likewise, the more damaged our livers are, then the more
impaired our clotting factor production will be. This will lead to an
increase in clotting times and probably an INR >2.
A)
Long-term alcoholic hepatitis would be suggested if her AST/ALT ratio
were above 2.
C) Hepatitis D infections are fairly rare, and
require a coinfection with Hepatitis B.
D) Bacterial hepatitis
may be possible, but she has no systemic signs of infection, just
liver failure
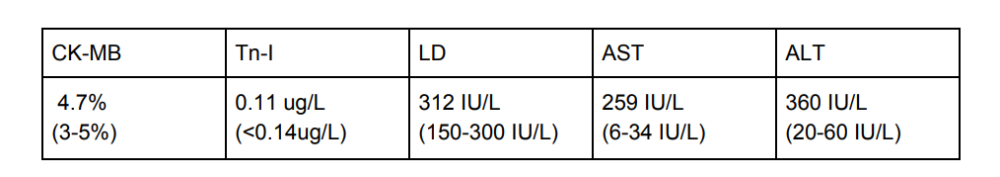
A 67-year-old male presents to the hospital via ambulance. He is brought to the hospital miraculously less than 2 hours after observers saw him go unconscious. He is slightly jaundiced. As the team began ruling out all life-threatening causes of his loss of consciousness, they order these tests with the following results:
He is diagnosed with liver disease because of the timeline.
What would the LD isoenzyme electrophoresis show?
A. Elevated
LD-1 and LD-3
B. Elevated LD-2
C. Elevated LD-4 and
LD-5
D. 1,2 Flipped pattern
The correct answer is C) These isoenzymes are fairly specific
to
the liver. Not enough time has elapsed for CK-MB, Tn-I, LD, or AST to
be elevated from the cardiac source. So they will have to keep him in
the hospital for about 8 hours to rule out the myocardial infarction.
Bone disease is one that can commonly cause elevation in LD-5, but it
does not result in an increased LD-4. this allows for fairly
easy
differentiation between the two. D) The 1,2 Flip is seen in
a myocardial infarction, where LD-1 raises above the level of the LD-2
peak. B) LD-2 should be higher than all of the other isoenzyme peaks,
but you can get into the specifics if you decide to do a
Masters
or Doctoral program. A) Elevated LD-1 and LD-3 do not
usually go together
Where is the ALP enzyme most prominent in the body?
Biliary tract, placenta, bone, kidney, liver
A 57-year-old male patient with benign prostatic hypertrophy and an elevated PSA has a total serum ACP value of 5 ng/mL. After tartrate inhibition, the serum ACP value dropped to 1 ng/mL. What is the total amount of prostatic ACP present?
4 ng/mL. 5 - 1 = 4. Remember, prostatic ACP is susceptible to tartrate.
What is the greatest source of ACP in the human body?
Prostatic secretions
A pregnant 28-year-old female has an elevated alkaline phosphatase.
What enzyme would tell the physician that the source of the ALP is NOT biliary?
.
If GGT were low, then that would rule-out a hepatobiliary source of the ALP
AMY ( pancreatic amylase )has one job, what is it?
Destroy α-1, 4 glycosidic linkages
How many free fatty acids are created from lipase, 12 triglycerides, and water?
24, 2 from every triglyceride and 12 monoglycerides
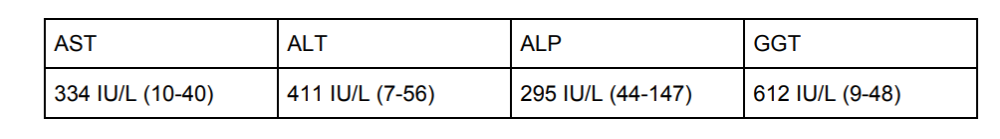
A 44-year-old obese female who is the mother of 12 kids has episodic right upper quadrant abdominal pain after eating fatty meals. Lab results are as follows:
What is the likely cause of her condition?
A.
Hepatitis
B. Gallstone (Choledocholithiasis)
C. Kidney
stone (Urolithiasis)
D. Heart attack (Myocardial infarction)
The correct answer is B) Gallstone (Choledocholithiasis). AST and ALT
will be elevated if there is liver damage so with this question stem,
I am really only thinking about answers A and B. Remember that ALP and
GGT are seen in extremely high concentrations in the bile ducts and
that they will be increased in just about any bile
duct
pathology, especially if you try to jam a stone through the
pipe! The elevated ALP and GGT at these levels are NOT consistent with
a diagnosis of A) hepatitis. The increased ALT value pretty much rules
out the possibility of a C) Kidney stone or a D) Heart attack.
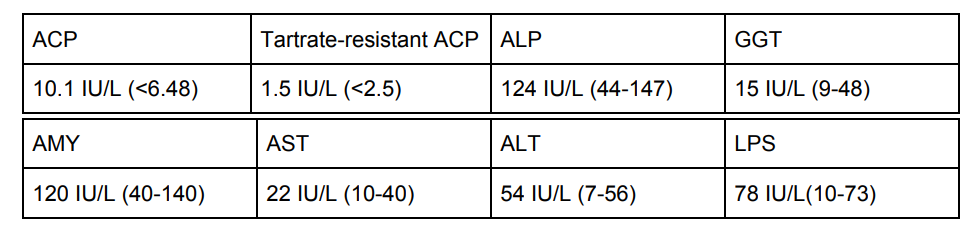
A 62-year old male presents to the physician with groin pain. His
groin pain radiates into his back and points to where his kidneys are
located and is exacerbated when he jumps. It is not associated with
passive movement but he has noticed an inability to completely
evacuate his bladder upon urination. He has also noticed a dull,
painful sensation in his lower back and right anterior thigh. This
pain is associated with movement and is NOT always present.
Upon
questioning, he says that the pain resides when he has an
alcoholic beverage. His physician orders the following panel of tests:
Where is the likely source of this patient’s medical
problem?
A. Liver
B. Muscle
C. Pancreas
D. Prostate
The correct answer is D) This is a long question stem with some great
clinical pearls hidden within the question stem. Let’s go through them
first and then we’ll go through the lab results. The groin pain
radiating to his back sounds like a musculoskeletal thing or
testicular torsion to me. The inability for complete evacuation of the
bladder during urination is a hallmark for benign prostatic
hypertrophy. We notice that this patient’s ALP is normal, so there is
likely not a skeletal disease causing this issue. Pain relief with
alcohol consumption is a typical finding. Alcohol not only dulls the
nerves which dulls the pain, it also dulls the neurons in your brain
to receive that pain.
All the results are normal except for the
ACP, TRAP, and LPS. Who knows what happened with LPS. But he is NOT
complaining of symptoms at this point that would lead me to think that
there is a problem with absorbance of fat soluble vitamins or an
energy deficiency. So this is likely NOT causing a problem and this
patient might just fall out of the normal range since his value is
barely elevated. The values that I want to look at are the elevated
ACP and the low TRAP. Let’s calculate the prostatic portion of
ACP:
10.1 - 1.5 = 8.6. The normal range for prostatic ACP is less
than 4.08 IU/L. This is about double that value. That’s about double
the value! No wonder he is having a problem peeing.
A 24-year-old female patient with pancreatitis presents to her
physician with weight loss, foul-smelling stool, jaundice, and
abdominal pain. What are the most likely pancreatic
enzymatic
deficiencies causing this clinical picture?
A.
Amylase
B. Glucagon
C. Insulin
D. Lipase
The correct answer is D) This enzymatic deficiency causes
steatorrhea, which leads to what the experts call “foul-smelling
stool” (as if poop didn’t normally smell bad). The jaundice is often
caused by hepatocellular damage and inability to conjugate the
bilirubin to excrete it. The weight loss comes from the inability to
absorb fats. They’re all lost in the stool. We really only have one
enzyme that would cause all of these fat-related issues, LPS! A)
Amylase breaks down starches and carbohydrate chains. B) Glucagon is
released
from the
What is the definition of: Substrate -
the substance that is used up in the reaction
What is the definition of: Product
- the substance that is formed in the reaction
What is the definition of: Inhibitor
- a substance that prevents or inhibits a reaction from taking place
What is the definition of: Kinetic assay
- the change of absorbance is measured on a spectrophotometer to assess the reaction rate . Have to do with speed
What is the definition of: Endpoint assay -
the change in absorbance is measured at the end of the reaction.
What is the definition of: International unit -
a unit of activity or potency for many substances defined individually in terms of the activity of a standard solution.
What is the definition of: Vmax
- the maximum velocity of an enzymatic reaction
What is the definition of: Km -
the concentration of substrate which allows the enzyme to achieve half Vmax
What is the definition of: Activation energy -
the energy required to get the reaction started. Kind of like finding the energy required to get yourself off the couch on a lazy day
What is the definition of: First order reaction -
The reaction rate is dependent upon substrate and enzyme concentrations
What is the definition of: Zero order reaction -
The reaction rate is constant and dependent upon only the enzyme concentration
What is the definition of: Prosthetic Groups
- coenzymes covalently bound to the enzyme
What is the definition of: Holoenzyme
- is the apoenzyme and coenzyme in one catalytically active unit
What is the definition of: Metalloenzyme
- enzymes that have a metallic ion in them
What is the ratio for First Order Kinetics for the Michaelis-Menten Constant (Km)
- a 1:1 relationship between substrate and velocity
What is Zero Order Kinetics -
the reaction reaches an asymptote, all enzyme sites are occupied and the reaction velocity cannot be increased by addition of substrate
what is the Michaelis-Menten Constant (Km)?
is the substrate concentration at which the reaction rate is half of Vmax
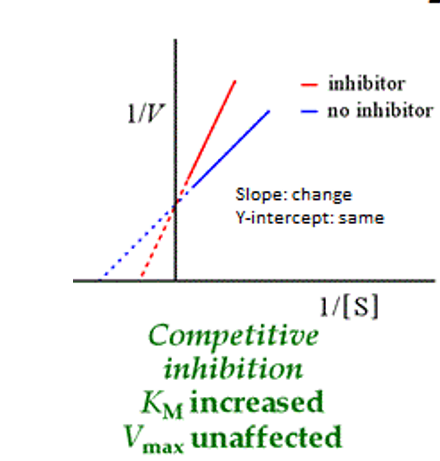
what should about Competitive inhibitor and Vmax and Km
Same Vmax
different Km
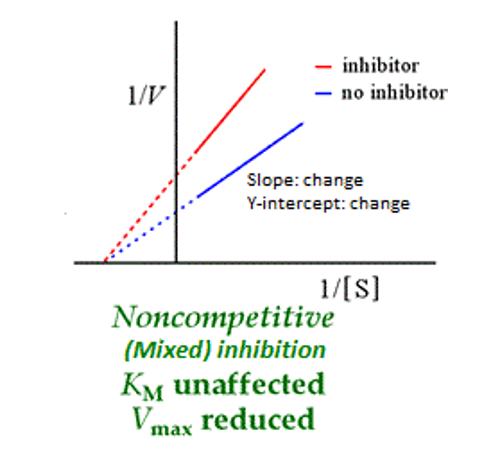
what should about noncompetitive inhibitor and Vmax and Km
Same Km
Different vmax
What does the Lineweaver Burk plots for competitive inhibition look like?
What does the Lineweaver Burk plots for noncompetitive(mixed) inhibition look like?
In healthy individuals what is the order of the isoenzymes for Lactate Dehydrogenase?
LD2 > LD1 > LD3 > LD4 > LD5
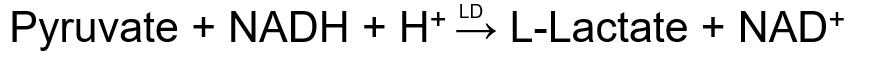
In Lactate Dehydrogenase what does Oxidoreductase do ?
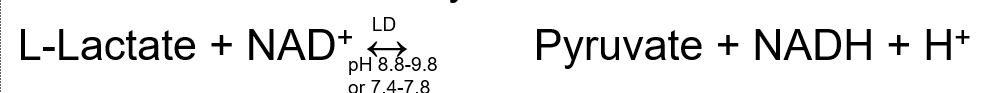
catalyzes the conversion of L-lactate to pyruvate and NADH
For LD methodology what is the Wacker procedure

For LD methodology what is the Wroblewski and LaDue reaction
What is the clinical significance of LD1>LD2 ?
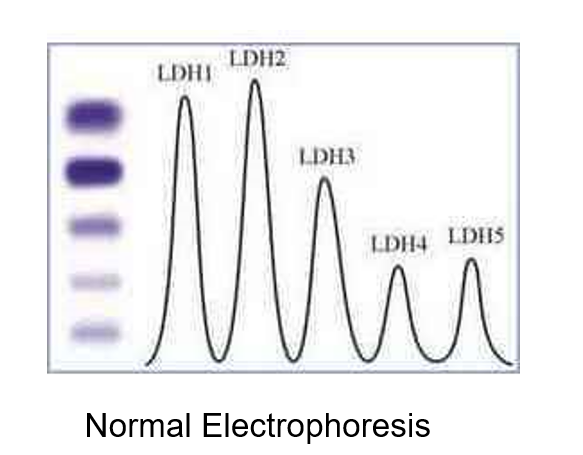
“Flipped pattern” indicative of MI, shock, myocarditis, or CHF
LD Peaks between 48 and 72 hours and stays elevated for 7-14 days
What is the clinical significance of LD5>LD4
Liver disease increases LD4 and LD5
What is important to know about LD reference ranges?
No clinically significant gender differences
Ranges are significantly different based upon the method used
Children have much higher LD values than adults
Hemolysis causes a gigantic spike in the LD levels
LD cannot be frozen! Activity is lost when frozen
What are the four tissue types that have the highest LD concentrations?
Kidney, Liver, Muscle, and RBCs
What are the refence ranges for Creatine Kinase (CK) in males?
= 52 - 236 U/L
What are the refence ranges for Creatine Kinase (CK) in females?
38 - 176 U/L
The conditions for CK to be stable are?
CK activity is unstable and lost during storage, light sensitive
Only stable for 4 hours at RT, 48 hours at 4˚C, and 1 month at -20˚C
The clinical significant of: CK-MB
It doesn’t peak for 24 hours. I t’s used to assess heart attacks
The clinical significant of: CK-MM
It is elevated in Duchenne muscular dystrophy, seizures, trauma, and “extreme” exercise
The clinical significant of: CK-BB
is elevated in brain injury, and is used as a tumor marker with Prostate and Small Cell Carcinoma of the lung
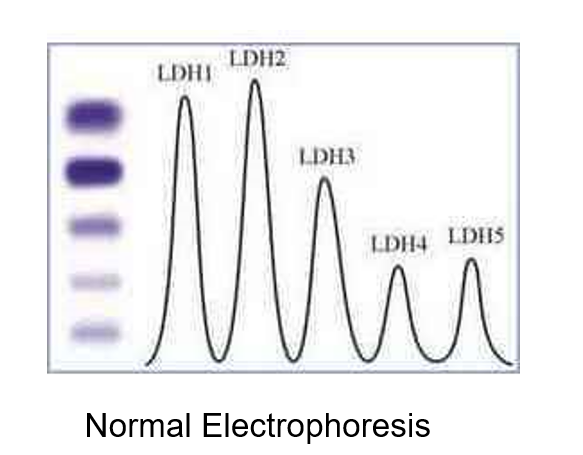
In CK Electrophoresis where can CK1 = CK-BB be found?
travels the furthest
In CK Electrophoresis where can CK2 = CK-MB be found?
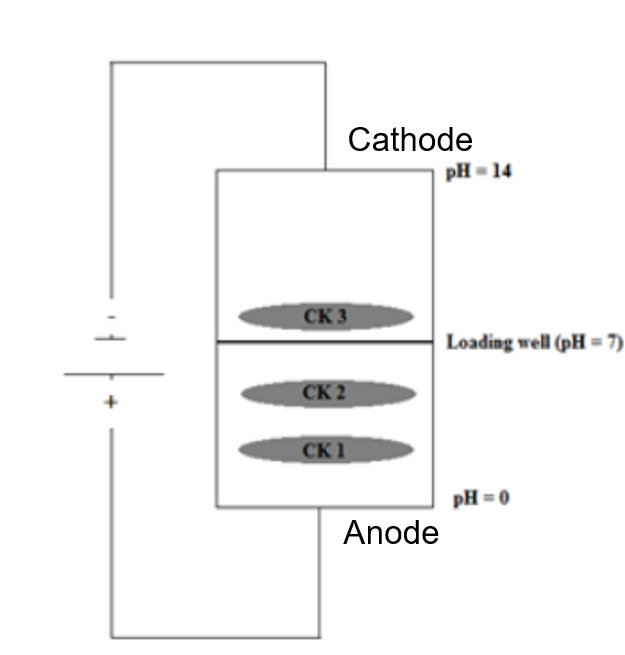
travelest the 2nd furthest
In CK Electrophoresis where can CK3 = CK-MM be found?
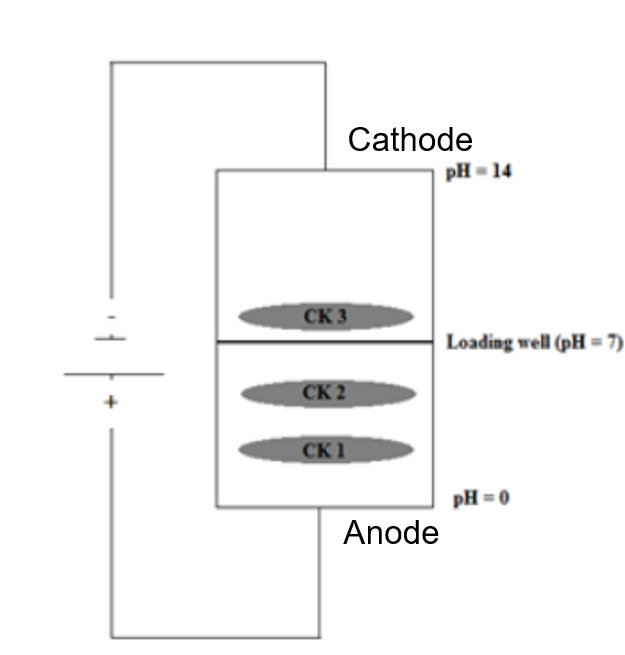
travels backward
What is the most common reason for AST to be elevated in the blood of a normal patient?
Hemolysis in the tube
in CK Isoenzyme Methodologies what is Immunoinhibition -
specific antibody against the CK-M subunit, old method and has been replaced by mass assay
in CK Isoenzyme Methodologies what is a Mass assay
- Primary anti-M antibody
Antibody attached to a solid phase,
Then a labeled secondary anti-B antibody
Signal is detected and directly proportional to CK-MB
For CK Isoenzyme Reference Range. What CK-BB does indicate?
absent or trace amount
For CK Isoenzyme Reference Range. What CK-MB does indicate?
≤6% of total CK, ≥6% is a fairly specific indicator of MI, myocardial infarction
For CK Isoenzyme Reference Range. What does CK-MM indicate?
94-100%
For CK Isoenzyme Reference Range.Relative Index CK-MB (ug/L x 100) / total CK (U/L) indicate?
<3% = noncardiac source
4-5% = gray area
>6% = cardiac source
The greatest source of CK-MB in the normal serum is cardiac muscle
What should you know about Aspartate Aminotransferase (AST)?
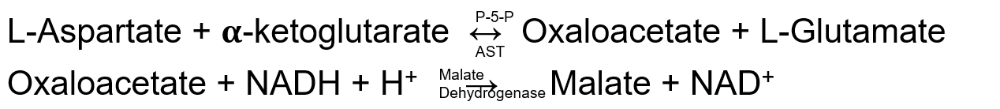
Catalyzes deamination
Measured by the Karmen method. Think hemolysis and hepatitis
Present in red blood cells, heart, liver, skeletal muscle, and kidney
AST is the most sensitive enzyme to alcoholic liver injury
The Aspartate Aminotransferase AST Reference Ranges are
Range at 37˚C is 5-30 U/L
No clinically significant gender differences
Hemolysis jeopardizes sample accuracy (because AST is found in high concentrations in RBCs) these are un acceptable for testing
What should you know about Alanine Aminotransferase (ALT)?
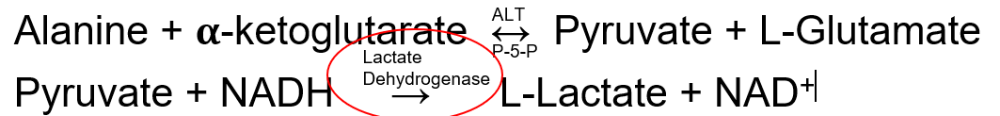
Catalyzes the deamination
Measured by the modified Wroblewski and LaDue method
Uses Lactate Dehydrogenase as an indicator reaction
Found primarily in the cytoplasm of cells
Mostly a liver specific transaminase
What is the clinical significance of Alanine Aminotransferase ALT?
DeRitis ratio (AST/ALT ratio)
Alcoholic liver disease produces a ratio >2 s = s auced and l = l osing l iver
Other hepatitis's can cause an AST/ALT ratio <1
The reference range for ALT?
Reference Range at 37˚C is 6-37 U/L
Hemolysis jeopardizes sample accuracy
Where can Acid Phosphatase ACP be found?
Osteoclasts , increases in bone disease,
normal serum
Prostate is the tissue with the highest concentration
RBCs are have high intracellular concentrations
Note: can’t be performed on a hemolysed sample
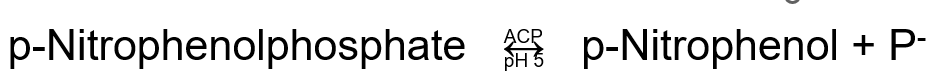
What is Acid Phosphatase ACP Methodology?
Addition of tartrate inhibits Prostatic
serum is derived from osteoclasts
The purpose of Amylase (AMS) is
Hydrolase that catalyzes the hydrolysis of starches (breaks down starch into individual glucose molecules)
1.Salivary Amylase - secreted in the saliva, active at a pH of about 6.8
2.Pancreatic Amylase - secreted from the pancreas, active at the same pH
Why do we need two types of virtually identical enzymes?
Increased in pancreatitis, alcoholism, parotitis
Macroamylasemia, not medically interesting, but can cause hyperamylasemia
SENSITIVE marker for pancreatitis
Pancreatic amylase is activated by the chloride in gastric acid
The purpose of lipase is?
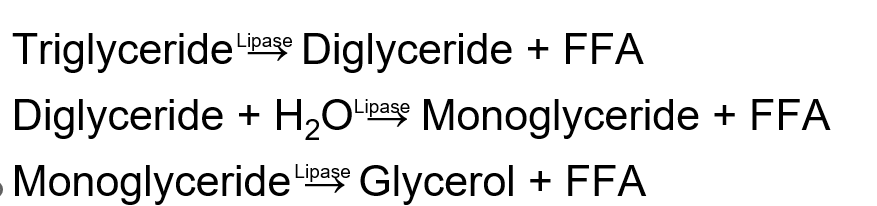
Hydrolyzes glycerol esters to produce glycerol and free fatty acids
Breaks down Triglyceride into 3 fatty acid chains and a gycerol back bone
The clinical significance of lipase?
Produced by the Pancreatic Acinar Cells
Peaks after 24 hours from the insult and remains elevated for 8-14 days
SPECIFIC marker for pancreatitis
What is the methodology for Lipase?
The reference ranges for lipase is?
Lipase is stable at RT for one week, 3˚C for 3 weeks, -20˚C for years
The significance of Cholinesterase (CHE)?
deficiency for anesthesiologists because it causes patients to remain paralyzed for a prolonged period of time after neuromuscular blocking agents are given for surgery
Cholinesterase Methodologies reference ranges for males are
40-78 U/L
note :5-MNBA is measured at 410 nm
Cholinesterase Methodologies reference ranges for females are
33-76 U/L
note :5-MNBA is measured at 410 nm
A man comes in to the clinic 4 days after a suspected heart attack. What is the best cardiac biomarker to order in this scenario?
Tn-I or Tn-T
The markers for Myocardial Infarction are?
What is the mainstay for diagnosis of hepatitis?
AST and ALT
note:ALT is more specific to liver tissue, whereas AST is found in many other tissues
GGT and LD will also increase, but they are not commonly-tested in the setting of hepatitis
The Tests that measure hepatocyte integrity are?
- AST
- ALT
The Tests that measure hepatocyte function?
- Serum Albumin
- PT/PTT
The Tests that assess the biliary tract?
- GGT
- ALP
- 5’-NT
What is Alkaline Phosphatase (ALP) associated with?
Associated with gallstones (choledocholithiasis)
Refrigeration causes activity to decrease
The formula for Bowers and McComb Reaction is?
A pregnant 28-year-old female has an elevated alkaline phosphatase. What enzyme would tell the physician that the source of the ALP is NOT biliary?
If GGT were low, then that would rule-out a hepatobiliary source of the ALP.
The disease that is association with this enzyme malignancies is: ACP
Prostate Cancer
The disease that is association with this enzyme malignancies is: ALP - ones
Lung, colon, ovarian, breast, uterine cancers, and lymphomas
Possibly more to come, these are the high-yield
Name the enzymes that you want to look for when you think the diagnosis could be pancreatitis?
1.Amylase
2.Lipase
If these two enzymes are not elevated, then it’s going to be hard to convince anyone that the diagnosis is pancreatitis
In Lineweaver-Burke Plots. what type of competition happens when: Lines cross on the Y, axis forming an X
Competitive inhibition,
The Vmax is the same, which means
that you can overcome this
type of inhibition by
increasing the substrate concentration
Note: X intercept = -1/Km, Y intercept = 1/Vmax
In Lineweaver-Burke Plots. what type of competition happens when: Lines meet at the X axis forming a V
Noncompetitive inhibition,
The Km is the same and the Vmax is reduced, which means that
there
are fewer available active binding sites for the substrate
to undergo the reaction
Note: X intercept = -1/Km, Y intercept = 1/Vmax
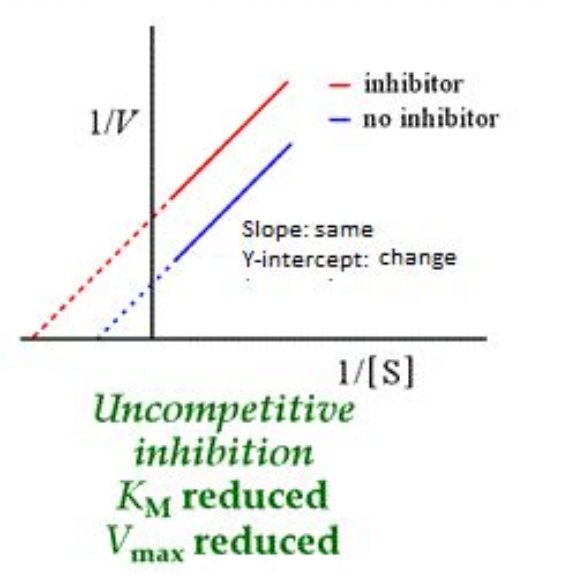
In Lineweaver-Burke Plots. what type of competition happens when: Lines do not cross, forming parallel lines
Uncompetitive inhibition,
This inhibitor binds to the enzyme-substrate complex, therefore the
reaction has a very difficult time getting going at all. Both the Km
and
Vmax are affected.
Note: X intercept = -1/Km, Y intercept = 1/Vmax
In Michaelis-Menten Curve what type of competition happens when: Km is increased, but Asymptote stays the same
Competitive inhibition
The maximum velocity can still be reached, bit the
enzyme and
substrate must overcome the effects of the inhibitor, this means that
it will take a higher concentration of the substrate to reach Vmax and
1/2 Vmax (or Km) will be increased
note: Asymptote = Vmax, 1/2 Vmax = Km
In Michaelis-Menten Curve what type of competition happens when: Asymptote is decreased, but Km stays the same
Noncompetitive inhibition
The maximum velocity is decreased because there are less
active
sites available for the substrate to bind to undergo the
reaction.
The Km will still be the same, because it will take
just as much concentration of the substrate to reach 1/2 Vmax
note: Asymptote = Vmax, 1/2 Vmax = Km
In Michaelis-Menten Curve what type of competition happens when: Lines do not cross, forming parallel lines
Uncompetitive inhibition
This inhibitor binds to the enzyme-substrate complex, therefore the
reaction has a very difficult time getting going at all. Both the Km
and
Vmax are affected
note: Asymptote = Vmax, 1/2 Vmax = Km
What does the Lineweaver Burk plots for uncompetitive inhibition look like?