Which answer choice refers to the pressure exerted by filtrate in the glomerular capsule?
- Glomerular hydrostatic pressure
- Hydrostatic pressure in the capsular space
- Colloid osmotic pressure
- Net filtration pressure
Hydrostatic pressure in the capsular space
Ex.
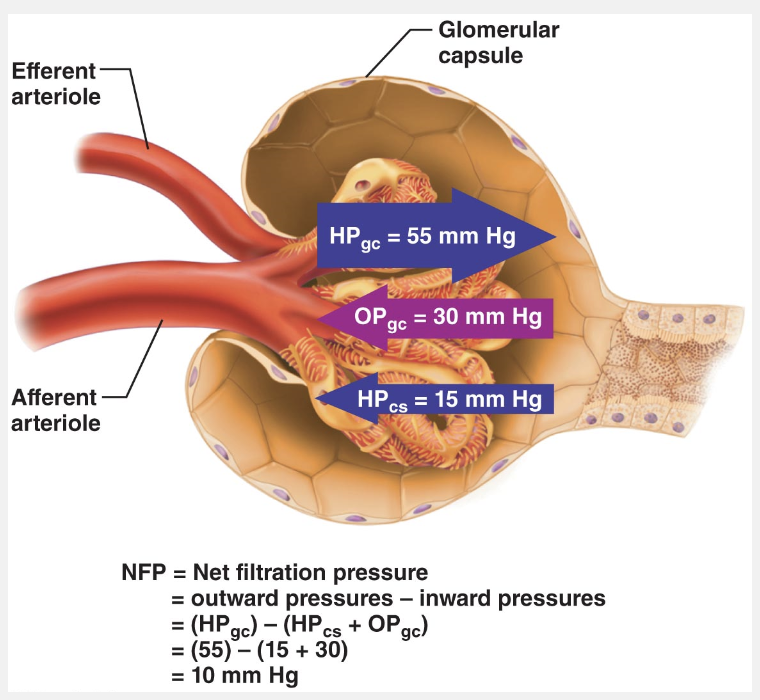
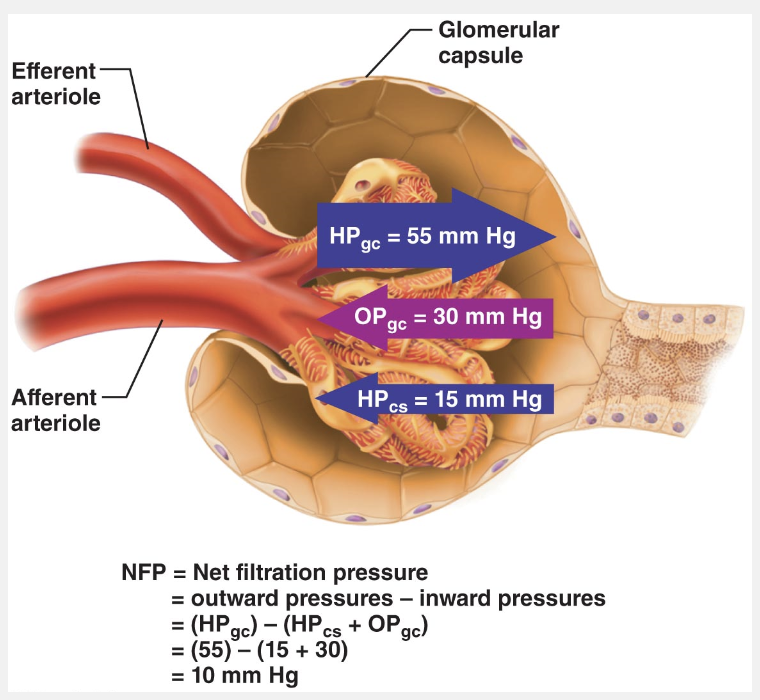
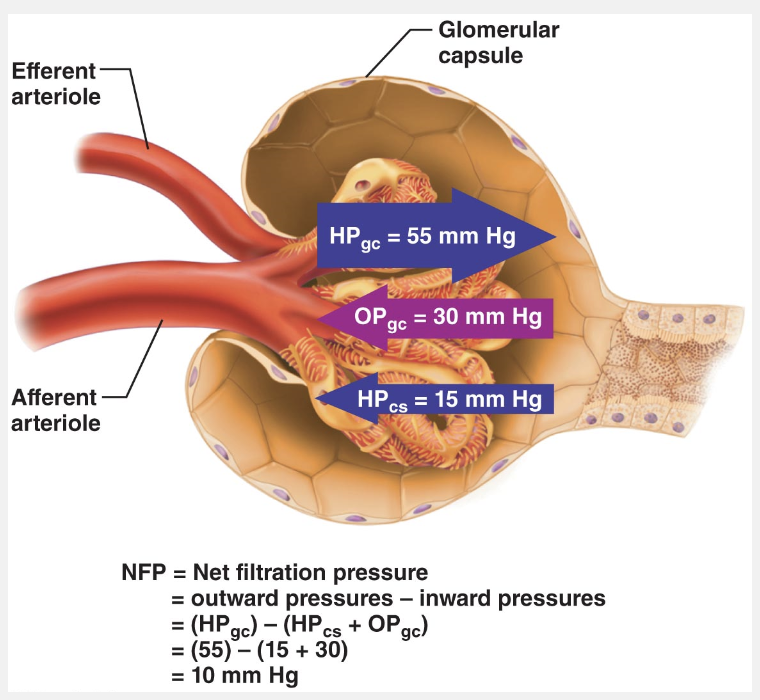
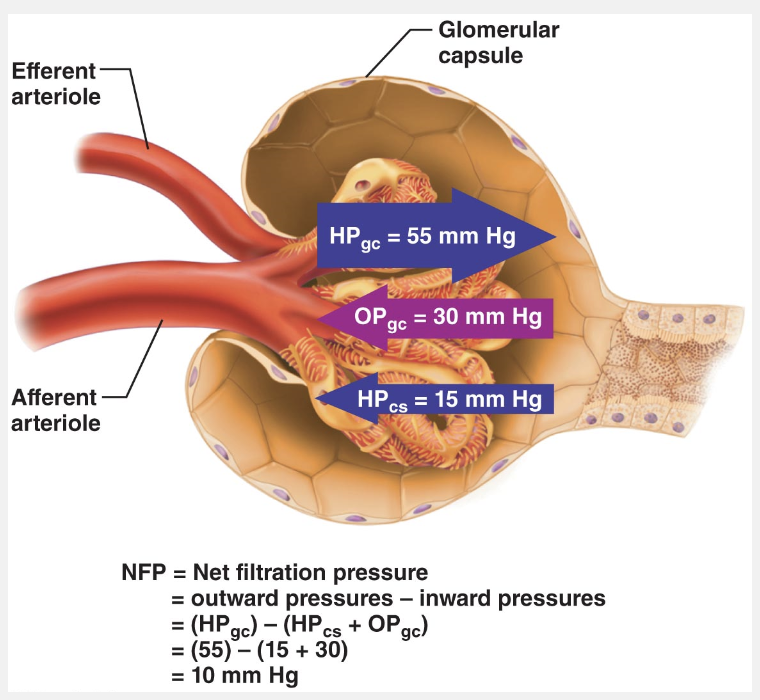
The hydrostatic pressure in the capsular space (HPcs) is the pressure exerted by filtrate in the glomerular capsule. HPcs is much higher than hydrostatic pressure surrounding most capillaries because filtrate is confined in a small space with a narrow outlet.
Which answer choice refers to the force of blood against the walls of the glomerular capillaries?
- Colloid osmotic pressure (OPgc)
- Capsular hydrostatic pressure (HPcs)
- Net filtration pressure (NFP)
- Glomerular hydrostatic pressure (HPgc)
Glomerular hydrostatic pressure (HPgc)
Ex.
Glomerular hydrostatis pressure (HPgc) refers to the force of blood against the walls of the glomerular capillaries.
The hydrostatic pressure in glomerular capillaries (HPgc) is essentially glomerular blood pressure. It is the chief force pushing water and solutes out of the blood and across the filtration membrane. The blood pressure in the glomerulus is extraordinarily high (approximately 55 mm Hg compared to an average of 26 mm Hg or so in other capillary beds) and it remains high across the entire capillary bed. This is because the glomerular capillaries are drained by a high-resistance efferent arteriole whose diameter is smaller than the afferent arteriole that feeds them. As a result, filtration occurs along the entire length of each glomerular capillary and reabsorption does not occur as it would in other capillary beds.
The energy needed for secondary active transport is provided by the __________.
- concentration gradient established by Cl-
- H+ pump
- passive transport
- concentration gradient established by Na+
concentration gradient established by Na+
Ex.
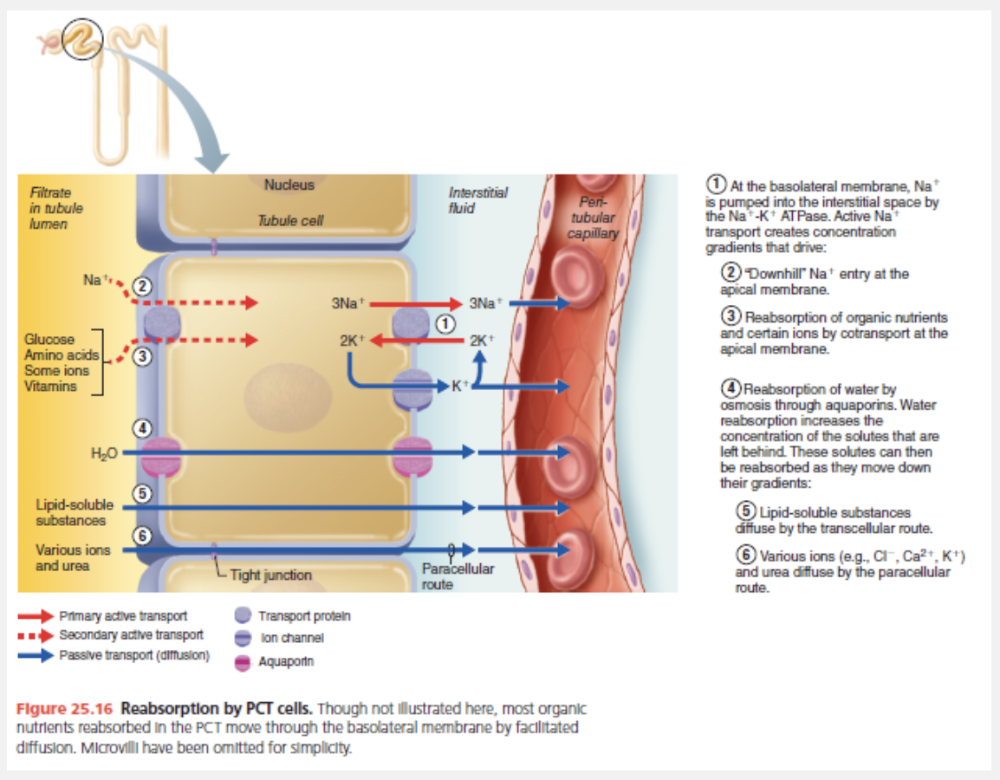
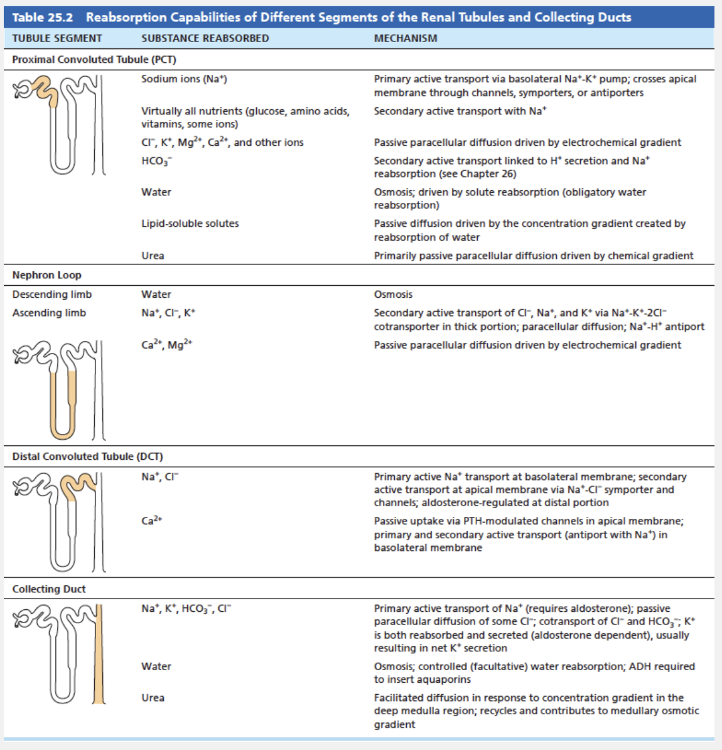
The energy needed for secondary active transport is provided by the concentration gradient established by Na+.
Active pumping of Na+ from the tubule cells results in a strong electrochemical gradient that favors its entry at the apical face via secondary active transport (cotransport) carriers or via facilitated diffusion through channels. This occurs because (1) the pump maintains the intracellular Na+ concentration at low levels, and (2) the K+ pumped into the tubule cells almost immediately diffuses out into the interstitial fluid via leakage channels, leaving the interior of the tubule cell with a net negative charge.
Because each tubule segment plays a slightly different role in reabsorption, the precise mechanism by which Na+ is reabsorbed at the apical membrane varies.
Match the following hormone with its action on the urinary system: ADH.
- Promotes reabsorption of sodium at the distal convoluted tubule
- Enzyme that catalyzes the formation of angiotensin I
- A powerful vasoconstrictor that also stimulates the secretion of aldosterone
- Regulates water reabsorption at the collecting duct
Regulates water reabsorption at the collecting duct
Ex.
ADH regulates water reabsorption at the collecting duct.
As its name reveals, ADH inhibits diuresis (di″u-re′sis), or urine output. ADH makes the principal cells of the collecting ducts more permeable to water by causing aquaporins to be inserted into their apical membranes. The amount of ADH determines the number of aquaporins, and thus the amount of water that is reabsorbed there. When the body is overhydrated, extracellular fluid osmolality decreases, decreasing ADH secretion by the posterior pituitary and making the collecting ducts relatively impermeable to water. ADH also increases urea reabsorption by the collecting ducts, as we will describe later.
Which of the following glomerular regulators responds to filtrate NaCl concentrations?
- Renin-angiotensin system
- Sympathetic branch
- Tubuloglomerular feedback mechanism
- Myogenic mechanism
Tubuloglomerular feedback mechanism
Ex.
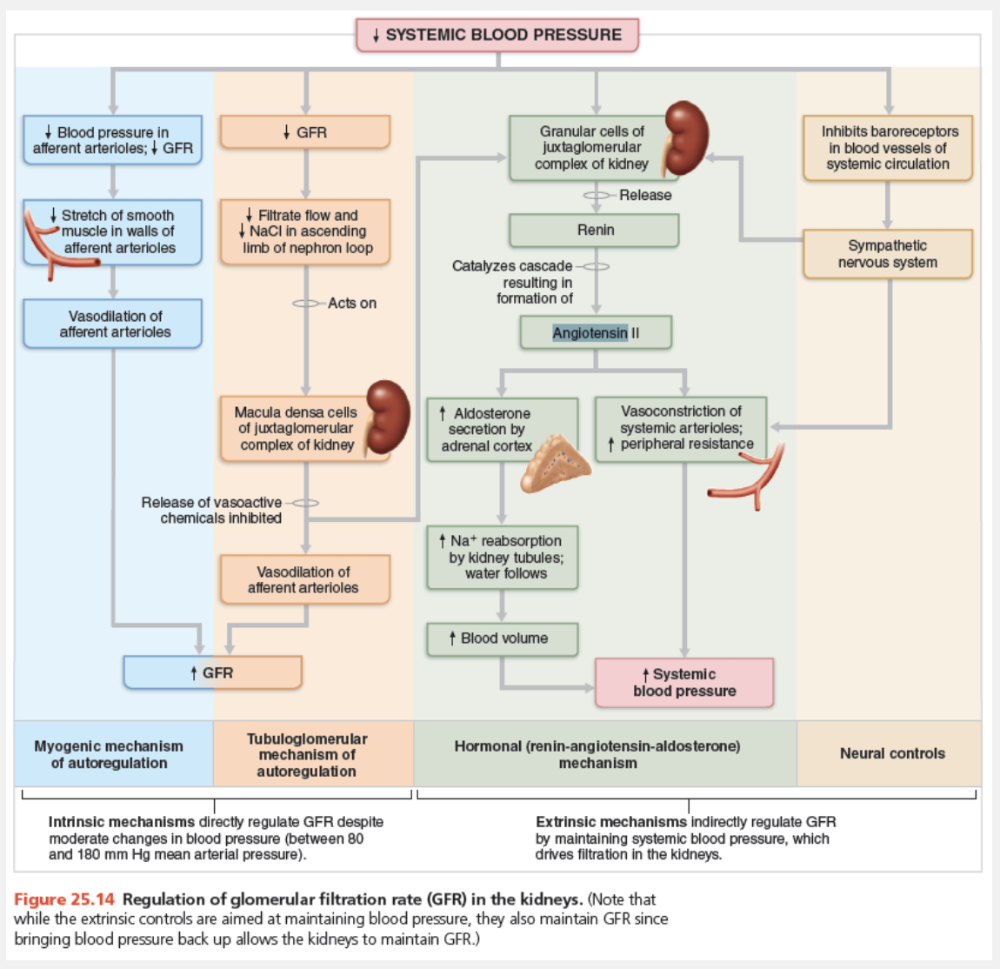
The tubuloglomerular feedback mechanism responds to filtrate NaCl concentrations.
Autoregulation by the flow-dependent tubuloglomerular feedback mechanism is “directed” by the macula densa cells of the juxtaglomerular complex. These cells, located in the walls of the ascending limb of the nephron loop, respond to filtrate NaCl concentration (which varies directly with filtrate flow rate). When GFR increases, there is not enough time for reabsorption and the concentration of NaCl in the filtrate remains high. The macula densa cells respond to high levels of NaCl in filtrate by releasing vasoconstrictor chemicals (ATP and others) that cause intense constriction of the afferent arteriole, reducing blood flow into the glomerulus. This drop in blood flow decreases the NFP and GFR, slowing the flow of filtrate and allowing more time for filtrate processing (NaCl reabsorption).
In contrast, the low NaCl concentration of slowly flowing filtrate inhibits ATP release from macula densa cells, causing vasodilation of the afferent arterioles. This allows more blood to flow into the glomerulus, thus increasing NFP and GFR.
Which of the following mechanisms involves an enzyme that is produced by the kidney when systemic blood pressure drops?
- Sympathetic nervous system controls
- Renin-angiotensin-aldosterone mechanism
- Myogenic mechanism
- Tubuloglomerular feedback mechanism
Renin-angiotensin-aldosterone mechanism
Ex.
The renin-angiotensin-aldosterone mechanism involves the enzyme renin, produced by the kidney when systemic blood pressure drops.
The renin-angiotensin-aldosterone mechanism is the body’s main mechanism for increasing blood pressure. Without adequate blood pressure (as might be due to hemorrhage, dehydration, etc.), glomerular filtration is not possible, so this mechanism regulates GFR indirectly.
Low blood pressure causes the granular cells of the juxtaglomerular complex to release renin. There are three pathways that stimulate granular cells:
- Sympathetic nervous system. As part of the baroreceptor reflex, renal sympathetic nerves activate β1-adrenergic receptors that cause the granular cells to release renin.
- Activated macula densa cells. Low blood pressure or vasoconstriction of the afferent arterioles by the sympathetic nervous system reduces GFR, slowing down the flow of filtrate through the renal tubules. When macula densa cells sense the low NaCl concentration of this sluggishly flowing filtrate, they signal the granular cells to release renin. They may signal by releasing less ATP (also thought to be the tubuloglomerular feedback messenger), by releasing more of the prostaglandin PGE2, or both.
- Reduced stretch. Granular cells act as mechanoreceptors. A drop in mean arterial blood pressure reduces the tension in the granular cells’ plasma membranes and stimulates them to release more renin.
Which pressure is exerted by the proteins in the blood that “sucks” water into the capillary?
- Colloid osmotic pressure (OPgc)
- Capsular hydrostatic pressure (HPcs)
- Glomerular hydrostatic pressure (HPgc)
- Net filtration pressure (NFP)
Colloid osmotic pressure (OPgc)
Ex.
The colloid osmotic pressure in glomerular capillaries (OPgc) is the pressure exerted by the proteins in the blood that “sucks” water into the capillary.
- The hydrostatic pressure in the capsular space (HPcs) is the pressure exerted by filtrate in the glomerular capsule. HPcs is much higher than hydrostatic pressure surrounding most capillaries because filtrate is confined in a small space with a narrow outlet.
- The colloid osmotic pressure in glomerular capillaries (OPgc) is the pressure exerted by the proteins in the blood. As shown in the figure below, the above pressures determine the net filtration pressure (NFP). NFP largely determines the glomerular filtration rate, which we consider next.
Anuria may be caused by all of the following except __________.
- transfusion reactions
- hypertension
- crush injuries
- acute nephritis
hypertension
Ex.
Hypertension would likely not lead to anuria.
Abnormally low urinary output (less than 50 ml/day), called anuria (ah-nu′re-ah), may indicate that glomerular blood pressure is too low to cause filtration. Renal failure and anuria can also result from situations in which the nephrons stop functioning, including acute nephritis, transfusion reactions, and crush injuries.
The most important factor affecting the net filtration pressure in the glomerulus is __________.
- blood osmotic pressure
- negative pressure
- capsular osmotic pressure
- capsular hydrostatic pressure
- hydrostatic pressure in the glomerulus
hydrostatic pressure in the glomerulus
Ex.
The most important factor affecting the net filtration pressure in the glomerulus is glomerular hydrostatic pressure.
NFP is the main controllable factor that determines GFR. Of the pressures determining NFP, the most important is hydrostatic pressure in the glomerulus. This pressure can be controlled by changing the diameter of the afferent (and sometimes the efferent) arterioles.
Which of the regions of the nephron do not absorb Na+ by primary active transport?
- Nephron loop, ascending limb
- Collecting duct
- Nephron loop, descending limb
- Distal convoluted tubule
Nephron loop, descending limb
Ex.
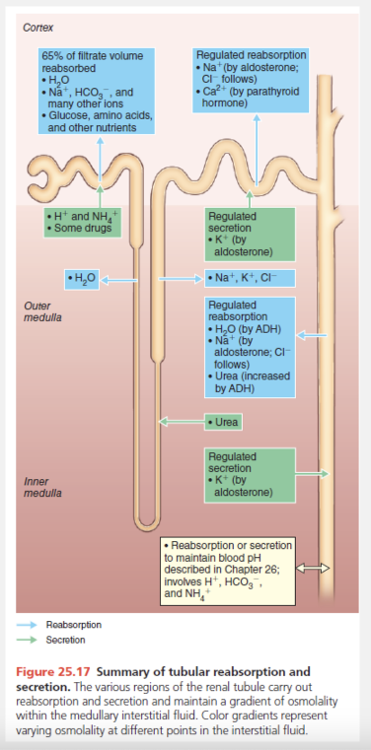
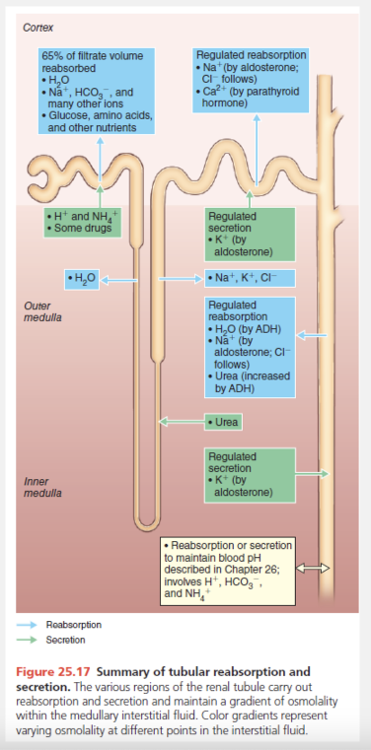
As shown in the table, the proximal convoluted tubule, the distal convoluted tubule, and the collecting duct all use primary active transport to reabsorb Na+. The descending limb of the nephron loop does not transport Na+ by primary active transport.
Which part of the nephron is influenced by hormones to absorb sodium and water?
- Nephron loop, ascending limb
- Nephron loop, descending limb
- Proximal convoluted tubule
- Distal convoluted tubule
Distal convoluted tubule
Ex.
Sodium and water are reabsorbed under hormonal influence in the distal convoluted tubule.
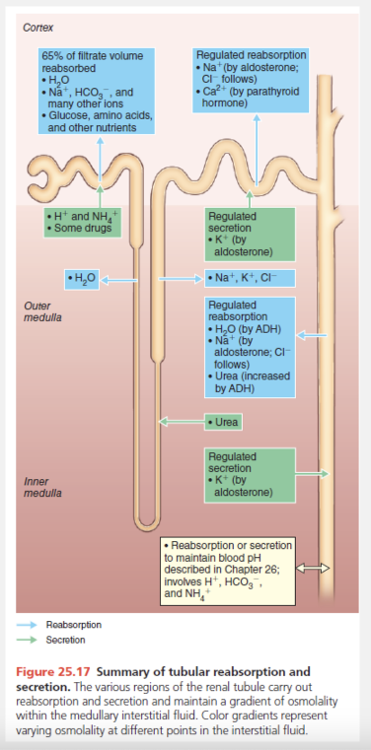
While reabsorption in the PCT and nephron loop does not vary with the body’s needs, hormones fine-tune reabsorption in the DCT and collecting duct. Because most of the filtered water and solutes have been reabsorbed by the time the DCT is reached, only a small amount of the filtered load is subject to this fine tuning (e.g., about 10% of the originally filtered NaCl and 25% of the water). These hormones include:
- Antidiuretic hormone (ADH). As its name reveals, ADH inhibits diuresis (di″u-re′sis), or urine output. ADH makes the principal cells of the collecting ducts more permeable to water by causing aquaporins to be inserted into their apical membranes. The amount of ADH determines the number of aquaporins, and thus the amount of water that is reabsorbed there. When the body is overhydrated, extracellular fluid osmolality decreases, decreasing ADH secretion by the posterior pituitary and making the collecting ducts relatively impermeable to water. ADH also increases urea reabsorption by the collecting ducts, as we will describe later.
- Aldosterone. Aldosterone fine-tunes reabsorption of the remaining Na+. Decreased blood volume or blood pressure, or high extracellular K+ concentration (hyperkalemia), can cause the adrenal cortex to release aldosterone to the blood. Except for hyperkalemia (which directly stimulates the adrenal cortex to secrete aldosterone), these conditions promote the renin-angiotensin-aldosterone mechanism. Aldosterone targets the principal cells of the collecting ducts and cells of the distal portion of the DCT (prodding them to synthesize and retain more apical Na+ and K+ channels, and more basolateral Na+-K+ ATPases). As a result, little or no Na+ leaves the body in urine. In the absence of aldosterone, these segments reabsorb much less Na+ and about 2% of Na+ filtered daily can be lost—an amount incompatible with life. Physiologically, aldosterone’s role is to increase blood volume, and therefore blood pressure, by enhancing Na+ reabsorption. In general, water follows Na+ if aquaporins are present. Aldosterone also reduces blood K+ concentrations because aldosterone-induced reabsorption of Na+ is coupled to K+ secretion in the principal cells of the collecting duct. That is, as Na+ enters the cell, K+ moves into the lumen.
- Atrial natriuretic peptide (ANP). In contrast to aldosterone, which acts to conserve Na+, ANP reduces blood Na+, thereby decreasing blood volume and blood pressure. Released by cardiac atrial cells when blood volume or blood pressure is elevated, ANP exerts several effects that lower blood Na+ content, including direct inhibition of Na+ reabsorption at the collecting ducts.
- Parathyroid hormone (PTH). Acting primarily at the DCT, PTH increases the reabsorption of Ca2+.
How would afferent arteriole dilation in response to a fall in blood pressure affect the GFR?
- Decreases GFR
- Effect on GFR cannot be determined
- GFR does not change
- Increases GFR
Increases GFR
Ex.
The afferent arterioles dilate in response to a fall in blood pressure and increases GFR.
The myogenic mechanism (mi″ojen′ ik) reflects a property of vascular smooth muscle—it contracts when stretched and relaxes when not stretched. Rising systemic blood pressure stretches vascular smooth muscle in the arteriolar walls, causing the afferent arterioles to constrict. This constriction restricts blood flow into the glomerulus and prevents glomerular blood pressure from rising to damaging levels. Declining systemic blood pressure causes dilation of afferent arterioles and raises glomerular hydrostatic pressure. Both responses help maintain normal NFP and GFR.
All of the following would stimulate the release of renin from granular cells, except __________.
- hemorrhaging or dehydration
- reduced stretching of the granular cells
- inhibition by the macula densa cells
- stimulation of the granular cells by the sympathetic nervous system
inhibition by the macula densa cells
Ex.
All of the responses would stimulate the release of renin from granular cells, except inhibition by the macula densa cells.
The renin-angiotensin-aldosterone mechanism is the body’s main mechanism for increasing blood pressure. Without adequate blood pressure (as might be due to hemorrhage, dehydration, etc.), glomerular filtration is not possible,so this mechanism regulates GFR indirectly.Low blood pressure causes the granular cells of the juxtaglomerular complex to release renin. There are three pathways that stimulate granular cells:
- Sympathetic nervous system.
- Renal sympathetic nerves cause the granular cells to release renin.
- Activated macula densa cells.
When macula densa cells sense the low NaCl concentration of sluggishly flowing filtrate, they signal the granular cells to release renin. Reduced stretch. Granular cells act as mechanoreceptors. Adrop in mean arterial blood pressure reduces the tension in the granular cells’ plasma membranes and stimulates them to release more renin.
Which substance would not normally be expected in urine?
- Sodium
- Nitrogenous waste
- Water
- Protein
- Chloride
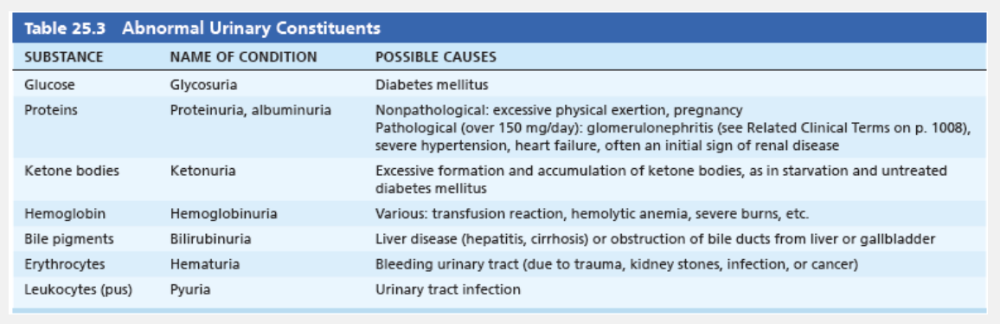
Protein
Ex.
Unusually high concentrations of any solute, or the presence of abnormal substances such as blood proteins, WBCs (pus), or bile pigments, may indicate pathology.
Which answer choice uses neural signals to override autoregulatory mechanisms?
- Sympathetic nervous system
- Renin-angiotensin system
- Myogenic mechanism
- Tubuloglomerular feedback mechanism
Sympathetic nervous system
Ex.
The sympathetic nervous system provides neural control that may overcome the renal autoregulatory mechanisms.
Neural renal controls serve the needs of the body as a whole—sometimes to the detriment of the kidneys. When the volume of the extracellular fluid is normal and the sympathetic nervous system is at rest, the renal blood vessels are dilated and renal autoregulation mechanisms prevail. However, when the extracellular fluid volume is extremely low (as in hypovolemic shock during severe hemorrhage), it is necessary to shunt blood to vital organs, and neural controls may override autoregulatory mechanisms. This could reduce renal blood flow to the point of damaging the kidneys.
When blood pressure falls, norepinephrine released by sympathetic nerve fibers (and epinephrine released by the adrenal medulla) causes vascular smooth muscle to constrict, increasing peripheral resistance and bringing blood pressure back up toward normal. This is the baroreceptor reflex we discussed in Chapter 19. As part of this reflex, the afferent arterioles also constrict. Constriction of the afferent arterioles decreases GFR and so helps restore blood volume and blood pressure to normal.
Which of the following is not part of the filtration membrane?
- Basement membrane
- Podocytes
- Endothelium
- Extraglomerular mesangial cells
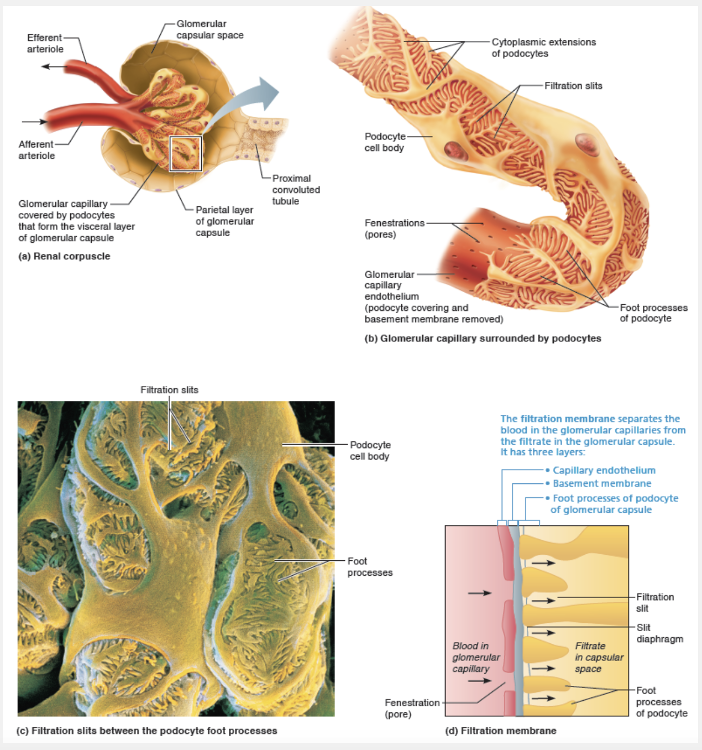
Extraglomerular mesangial cells
Ex.
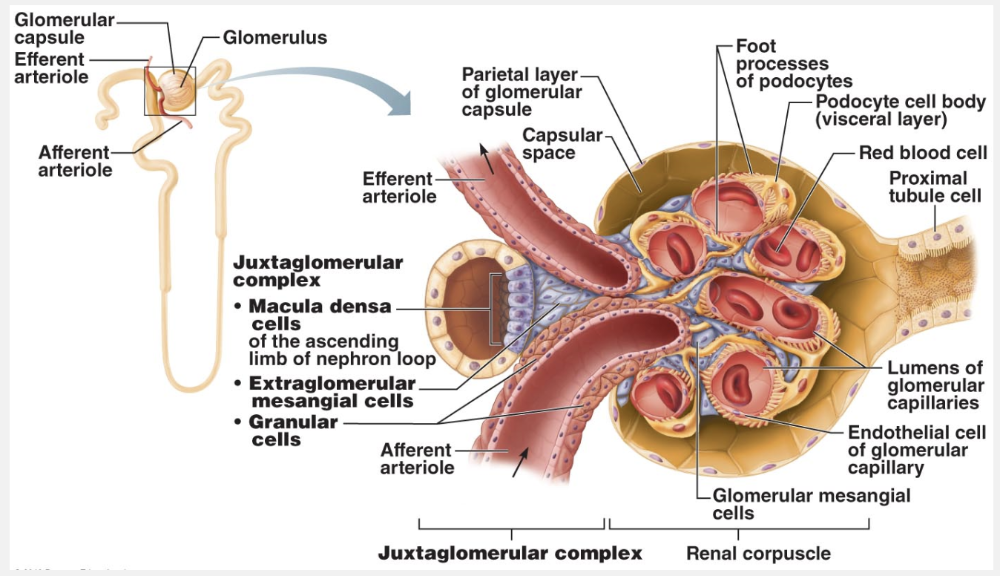
Extraglomerular mesangial cells are not part of the filtration membrane. Extraglomerular mesangial cells lie between the arteriole and tubule cells, and are interconnected by gap junctions. These cells may pass regulatory signals between macula densa and granular cells.
The filtration membrane lies between the blood and the interior of the glomerular capsule. It is a porous membrane that allows free passage of water and solutes smaller than plasma proteins. As the figure below shows, its three layers are:
- Fenestrated endothelium of the glomerular capillaries. The fenestrations (capillary pores) allow all blood components except blood cells to pass through.
- Basement membrane. The basement membrane lies between the other two layers and is composed of their fused basal laminae. It forms a physical barrier that blocks all but the smallest proteins while still permitting most other solutes to pass. The glycoproteins of the gel-like basement membrane give it a negative charge. As a result, the basement membrane electrically repels many negatively charged macromolecular anions such as plasma proteins, reinforcing the blockade based on molecular size.
- Foot processes of podocytes of the glomerular capsule. The visceral layer of the glomerular capsule is made of podocytes that have filtration slits between their foot processes. If any macromolecules manage to make it through the basement membrane, slit diaphragms—thin membranes that extend across the filtration slits—prevent almost all of them from traveling farther.
Macromolecules that get “hung up” in the filtration membrane are engulfed by specialized pericytes called glomerular mesangial cells.
All of the following functions are carried out in the renal tubules, except __________.
- filtration
- reabsorption
- All of these functions occur in the renal tubules.
- secretion
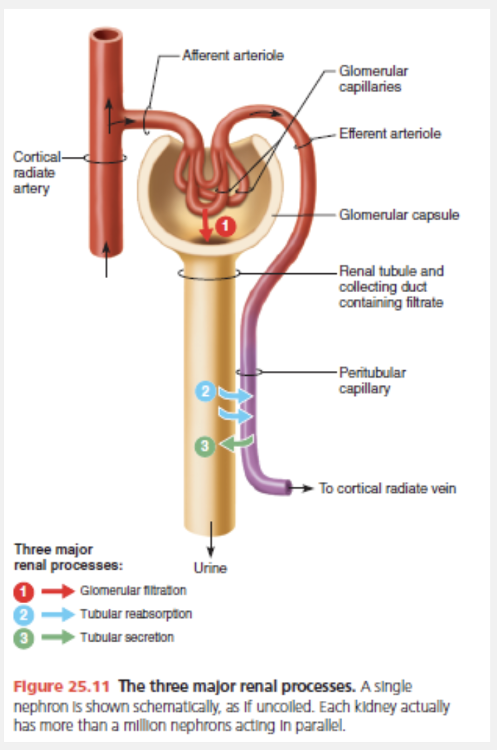
filtration
Ex.
All of the following functions are carried out in the renal tubules, except filtration.
Urine formation and the adjustment of blood composition involve three processes:
- Glomerular filtration. Glomerular filtration (“dumping into the waste container”) takes place in the renal corpuscle and produces a cell- and protein-free filtrate.
- Tubular reabsorption. Tubular reabsorption (“reclaiming what the body needs to keep”) is the process of selectively moving substances from the filtrate back into the blood. It takes place in the renal tubules and collecting ducts. Tubular reabsorption reclaims almost everything filtered—all of the glucose and amino acids, and some 99% of the water, salt, and other components. Anything that is not reabsorbed becomes urine.
- Tubular secretion. Tubular secretion (“selectively adding to the waste container”) is the process of selectively moving substances from the blood into the filtrate. Like tubular reabsorption, it occurs along the length of the tubule and collecting duct.
Select the description of macula densa cells.
- Long nephrons that deeply invade the medulla
- Specialized chemoreceptors
- Anchor kidneys to surrounding structures
- Prevent infection from other areas spreading to the kidney
- Specialized mechanoreceptors
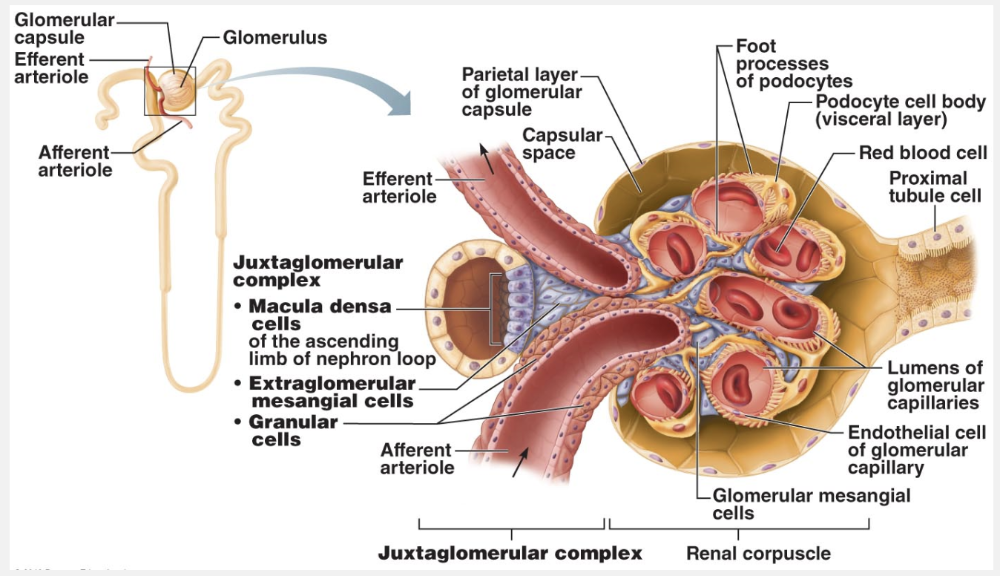
Specialized chemoreceptors
Ex.
Macula densa cells are specialized chemoreceptors.
The macula densa (mak′u-lah den′sah; “dense spot”) is a group of tall, closely packed cells in the ascending limb of the nephron loop that lies adjacent to the granular cells. The macula densa cells are chemoreceptors that monitor the NaCl content of the filtrate entering the distal convoluted tubule.
Match the following hormone with its action on the urinary system: Angiotensin II.
- Promotes reabsorption of sodium at the distal convoluted tubule
- Enzyme that catalyzes the formation of angiotensin I
- Regulates water reabsorption at the collecting duct
- A powerful vasoconstrictor that also stimulates the secretion of aldosterone
A powerful vasoconstrictor that also stimulates the secretion of aldosterone
Ex.
Angiotensin II is a powerful vasoconstrictor that also stimulates the secretion of aldosterone.
As shown in the figure below, angiotensin II stimulates aldosterone secretion by the adrenal cortex and stimulates vasoconstriction of systemic arterioles to increase peripheral resistance.
If the afferent arteriole constricts while the efferent arteriole remains unchanged, the glomerular filtration rate __________.
- decreases
- cannot be determined
- increases
- does not change
decreases
Ex.
If the afferent arteriole constricts while the efferent arteriole remains unchanged, the glomerular filtration rate decreases.
The myogenic mechanism (mi″ojen′ ik) reflects a property of vascular smooth muscle—it contracts when stretched and relaxes when not stretched. Rising systemic blood pressure stretches vascular smooth muscle in the arteriolar walls, causing the afferent arterioles to constrict. This constriction restricts blood flow into the glomerulus and prevents glomerular blood pressure from rising to damaging levels. Declining systemic blood pressure causes dilation of afferent arterioles and raises glomerular hydrostatic pressure. Both responses help maintain normal NFP and GFR.
How is Na+ reabsorbed?
- By receptor-mediated endocytosis
- By osmosis
- By facilitated diffusion
- By diffusion
- By active transport using ATP
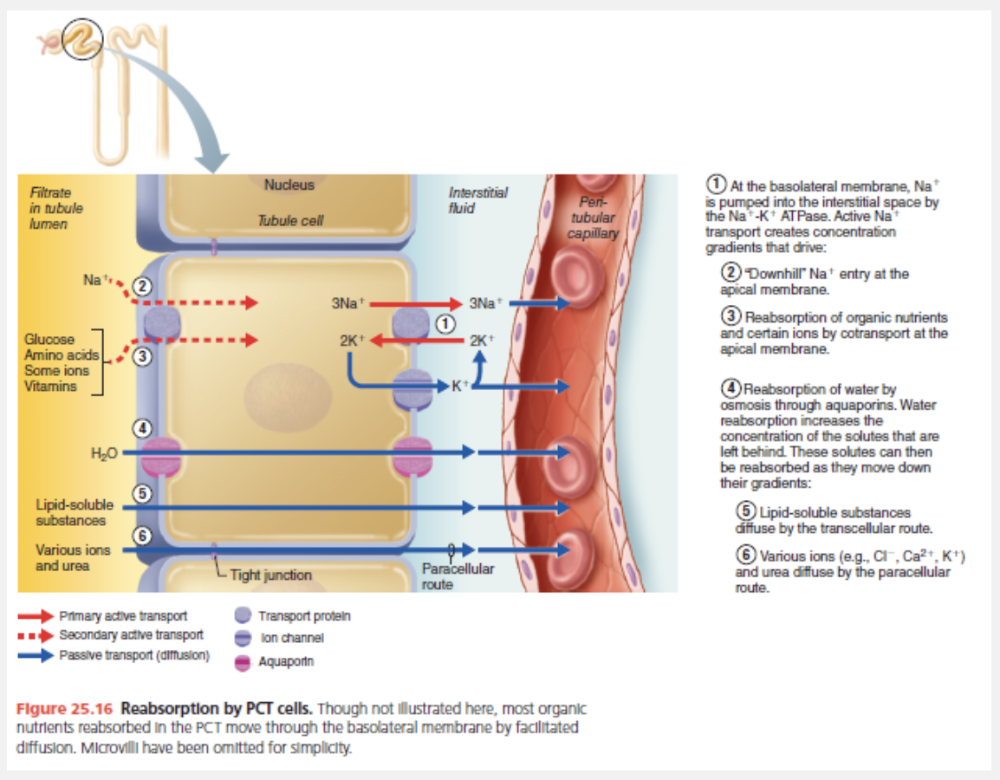
By active transport using ATP
Ex.
Na+ is reabsorbed by active transport using ATP.
Na+ is actively transported out of the tubule cell by primary active transport—a Na+-K+ ATPase pump in the basolateral membrane. From there, the bulk flow of water sweeps Na+ into adjacent peritubular capillaries. This bulk flow of water and solutes into the peritubular capillaries is rapid because the blood there has low hydrostatic pressure and high osmotic pressure (remember, most proteins remain in the blood instead of filtering out into the tubule).
Which pressure in or around the glomerulus is the result of all pressures and is responsible for filtrate formation?
- Net filtration pressure
- Capsular hydrostatic pressure
- Glomerular hydrostatic pressure
- Colloid osmotic pressure
Net filtration pressure
Ex.
The net filtration pressure in or around the glomerulus is the result of all pressures and is responsible for filtrate formation.
Usually about 10 mm Hg, the net filtration pressure (NFP) is determined by the relationship between forces favoring filtration (glomerular hydrostatic pressure) and forces that oppose it (capsular hydrostatic pressure and blood colloid osmotic pressure).
Which of the following homeostatic imbalances suggests that glomerular blood pressure may be too low to cause filtration?
- Anuria
- Pyelonephritis
- Diuresis
- Incontinence
Anuria
Ex.
Abnormally low urinary output (less than 50 ml/day), called anuria (ah-nu′re-ah), may indicate that glomerular blood pressure is too low to cause filtration. Renal failure and anuria can also result from situations in which the nephrons stop functioning, including acute nephritis, transfusion reactions, and crush injuries.
Urinary incontinence is the inability to control urination.
Pyelonephritis refers to infections or inflammations that affect the kidney.
Diuresis is increased production of urine.
When the concentration of ADH increases, __________.
- less urine is produced
- more urine is produced
- the specific gravity of the urine decreases
- less water is reabsorbed by the nephron and collecting duct
- more salt is secreted by the nephron
less urine is produced
Ex.
When the concentration of ADH increases, less urine is produced.
As its name reveals, ADH inhibits diuresis (di″u-re′sis), or urine output. ADH makes the principal cells of the collecting ducts more permeable to water by causing aquaporins to be inserted into their apical membranes. The amount of ADH determines the number of aquaporins, and thus the amount of water that is reabsorbed there. When the body is overhydrated, extracellular fluid osmolality decreases, decreasing ADH secretion by the posterior pituitary and making the collecting ducts relatively impermeable to water. ADH also increases urea reabsorption by the collecting ducts, as we will describe later.
Select the mechanism in which rising systemic blood pressure stretches vascular smooth muscle in the arteriolar walls, causing the afferent arterioles to constrict.
- Myogenic mechanism
- Sympathetic nervous system
- Renin-angiotensin system
- Tubuloglomerular feedback mechanism
Myogenic mechanism
Ex.
In the myogenic mechanism rising systemic blood pressure stretches vascular smooth muscle in the arteriolar walls, causing the afferent arterioles to constrict.
The myogenic mechanism (mi″ojen′ ik) reflects a property of vascular smooth muscle—it contracts when stretched and relaxes when not stretched. Rising systemic blood pressure stretches vascular smooth muscle in the arteriolar walls, causing the afferent arterioles to constrict. This constriction restricts blood flow into the glomerulus and prevents glomerular blood pressure from rising to damaging levels. Declining systemic blood pressure causes dilation of afferent arterioles and raises glomerular hydrostatic pressure. Both responses help maintain normal NFP and GFR.
Which of the following substances is typically used to measure the GFR?
- Glucose
- Protein
- Inulin
- Drug metabolites
Inulin
Ex.
Because it is freely filtered and neither reabsorbed nor secreted by the kidneys, inulin (in′u-lin) is the substance typically used to determine the GFR. Inulin is a plant polysaccharide that has a renal clearance value equal to the GFR. When inulin is infused such that its plasma concentration is 1 mg/ml (P = 1 mg/ml), then generally U = 125 mg/ml, and V = 1 ml/min. Therefore, its renal clearance is C = (125 × 1)/1 = 125 ml/min, meaning that in 1 minute the kidneys have cleared all the inulin present in 125 ml of plasma.
Glomerular filtration is based on particle _______.
- size
- solubility
- pressure
- charge
size
Ex.
Glomerular filtration is based on particle size.
Molecules smaller than 3 nm in diameter—such as water, glucose, amino acids, and nitrogenous wastes—pass freely from the blood into the glomerular capsule. As a result, these substances usually have similar concentrations in the blood andthe glomerular filtrate. Larger molecules pass with greater difficulty,and those larger than 5 nm are generally barred from entering the tubule. The presence of large proteins or blood cells in the urine usually indicates a problem with the filtration membrane.
Which process results in increased blood pressure in response to hormone release?
- Tubuloglomerular response
- Adrenergic response
- Renin-angiotensin-aldosterone mechanism
- Countercurrent mechanism
- Myogenic mechanism
Renin-angiotensin-aldosterone mechanism
Ex.
The renin-angiotensin-aldosterone mechanism increases blood pressure in response to hormone release.
The renin-angiotensin-aldosterone mechanism is the body’s main mechanism for increasing blood pressure. Without adequate blood pressure (as might be due to hemorrhage, dehydration, etc.), glomerular filtration is not possible, so this mechanism regulates GFR indirectly.
Low blood pressure causes the granular cells of the juxtaglomerular complex to release renin. There are three pathways that stimulate granular cells:
- Sympathetic nervous system. As part of the baroreceptor reflex, renal sympathetic nerves activate β1-adrenergic receptors that cause the granular cells to release renin.
- Activated macula densa cells. Low blood pressure or vasoconstriction of the afferent arterioles by the sympathetic nervous system reduces GFR, slowing down the flow of filtrate through the renal tubules. When macula densa cells sense the low NaCl concentration of this sluggishly flowing filtrate, they signal the granular cells to release renin. They may signal by releasing less ATP (also thought to be the tubuloglomerular feedback messenger), by releasing more of the prostaglandin PGE2, or both.
- Reduced stretch. Granular cells act as mechanoreceptors. A drop in mean arterial blood pressure reduces the tension in the granular cells’ plasma membranes and stimulates them to release more renin.
Match the following hormone with its action on the urinary system: Aldosterone.
- Regulates water reabsorption at the collecting duct
- Enzyme that catalyzes the formation of angiotensin I
- Promotes reabsorption of sodium at the distal convoluted tubule
- A powerful vasoconstrictor that also stimulates the secretion of aldosterone
Promotes reabsorption of sodium at the distal convoluted tubule
Ex.
Aldosterone promotes reabsorption of sodium at the distal convoluted tubule.
Aldosterone fine-tunes reabsorption of the remaining Na+. Decreased blood volume or blood pressure, or high extracellular K+ concentration (hyperkalemia), can cause the adrenal cortex to release aldosterone to the blood. Except for hyperkalemia (which directly stimulates the adrenal cortex to secrete aldosterone), these conditions promote the renin-angiotensin-aldosterone mechanism. Aldosterone targets the principal cells of the collecting ducts and cells of the distal portion of the DCT (prodding them to synthesize and retain more apical Na+ and K+ channels, and more basolateral Na+-K+ ATPases). As a result, little or no Na+ leaves the body in urine. In the absence of aldosterone, these segments reabsorb much less Na+ and about 2% of Na+ filtered daily can be lost—an amount incompatible with life.
Physiologically, aldosterone’s role is to increase blood volume, and therefore blood pressure, by enhancing Na+ reabsorption. In general, water follows Na+ if aquaporins are present. Aldosterone also reduces blood K+ concentrations because aldosterone-induced reabsorption of Na+ is coupled to K+ secretion in the principal cells of the collecting duct. That is, as Na+ enters the cell, K+ moves into the lumen.
Which of the following substances is typically used to measure the GFR?Aldosterone-induced reabsorption of Na+ is coupled with ____________.
- Ca2+ secretion
- None of these is correct.
- K+ reabsorption
- K+ secretion
- Ca2+ reabsorption
K+ secretion
Ex.
Aldosterone-induced reabsorption of Na+ is coupled with K+ secretion.
Aldosterone-induced reabsorption of Na+ is coupled with to K+ secretion in the principal cells of the collecting duct. That is, as Na+ enters the cell, K+ moves into the lumen. Acting primarily at the DCT, PTH increases the reabsorption of Ca2+.