Match the following: Pleurisy.
- Decreased natural resilience of the lungs
- Such strong bronchoconstriction that pulmonary ventilation almost completely stops, regardless of the pressure gradient
- Collapse of alveoli due to little surfactant
- Inflammation of the serous membranes or serosa surrounding the lungs
Inflammation of the serous membranes or serosa surrounding the lungs
Ex.
Pleurisy (ploo’rĭ-se), inflammation of the pleurae, in flammation of the serous membranes or serosa surrounding the lungs.
Inflamed pleurae become rough, resulting in friction and stabbing pain with each breath. As the disease progresses, the pleurae may produce excessive amounts of fluid. This increased fluid relieves the pain caused by pleural surfaces rubbing together, but may exert pressure on the lungs and hinder breathing movements.
Other fluids that may accumulate in the pleural cavity include blood (leaked from damaged blood vessels) and blood filtrate (the watery fluid that oozes from the lung capillaries when leftsided heart failure occurs). The term for fluid accumulation in the pleural cavity is pleural effusion.
Collapse of the alveoli due to a decreased amount of surfactant can cause infant respiratory distress syndrome.
Asthma can result in a strong enough constriction of the bronchioles that air flow is dramatically reduced.
Decreased natural resilience of the lungs results in a decrease in lung compliance, requiring more energy to breathe.
Match the following term with its correct description: External respiration.
- Movement of oxygen from the lungs to the blood, and of carbon dioxide from the blood to the lungs
- Movement of air into and out of the lungs so that gases are continuously changed and refreshed
- Movement of oxygen from the blood to tissue cells, and of carbon dioxide from tissue cells to blood
- The actual site of gas exchange in the lungs
- The fairly rigid conduits for air to reach the gas exchange sites in the lungs
- Transport of oxygen from lungs to body cells and carbon dioxide from tissue cells to lungs
Movement of oxygen from the lungs to the blood, and of carbon dioxide from the blood to the lungs
Ex.
External respiration is the movement of oxygen from the lungs to the blood, and of carbon dioxide from the blood to the lungs.
Pulmonary ventilation causes movement of air into and out of the lungs so that gases are continuously changed and refreshed.
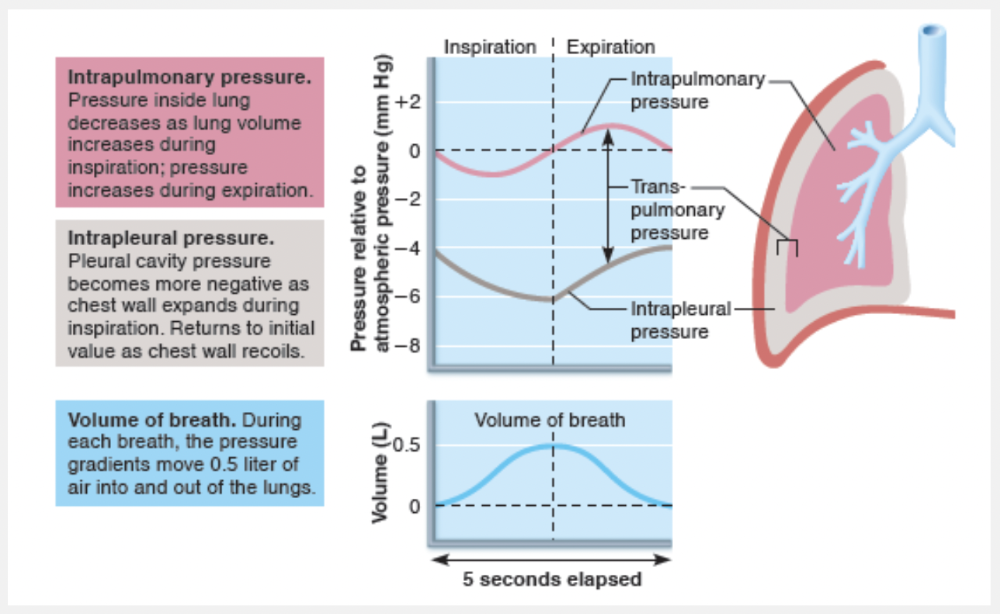
Pulmonary ventilation, consisting of inspiration and expiration, is a mechanical process that depends on volume changes in the thoracic cavity. A rule to keep in mind is that volume changes lead to pressure changes, and pressure changes lead to the flow of gases to equalize the pressure.
Transport of oxygen from lungs to body cells and carbon dioxide from tissue cells to lungs is a transport function of the cardiovascular system.
Movement of oxygen from the blood to tissue cells, and of carbon dioxide from tissue cells to blood is internal respiration.
The fairly rigid conduits for air to reach the gas exchange sites in the lungs are the respiratory passages that are part of the conducting zone.
What value(s) would be affected by a restrictive disorder?
- VC, TLC, FRC, and RV decline
- VC, TLC, FRC, and RV increase
- Only TLC
- Only TV
VC, TLC, FRC, and RV decline
Ex.
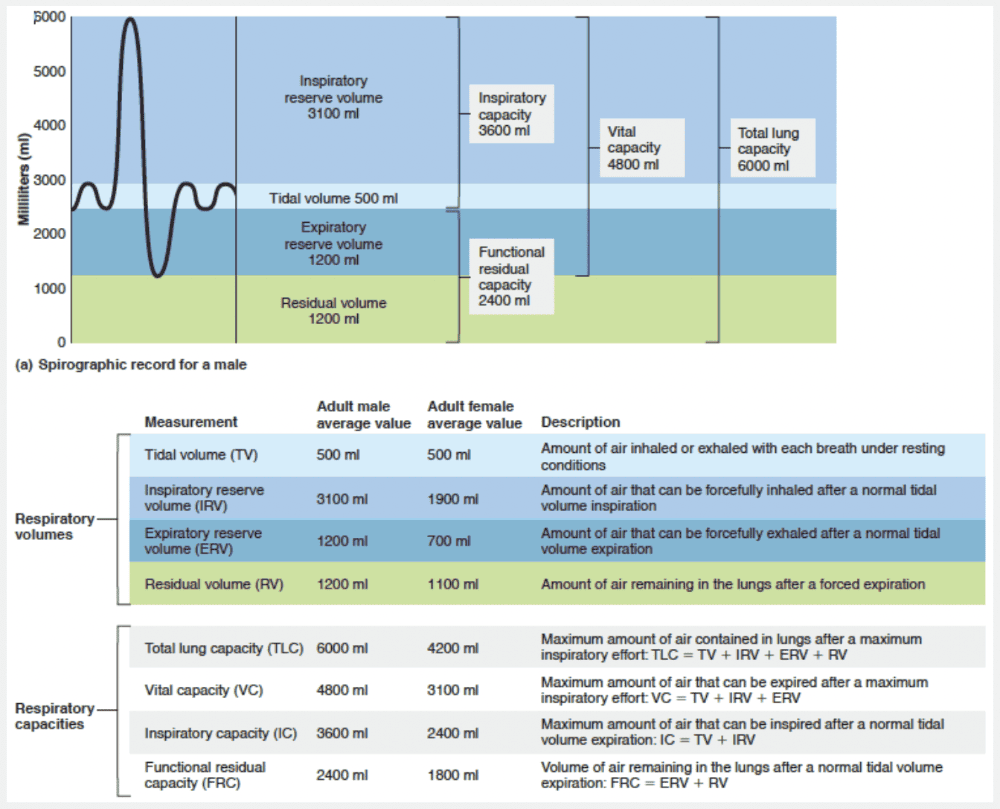
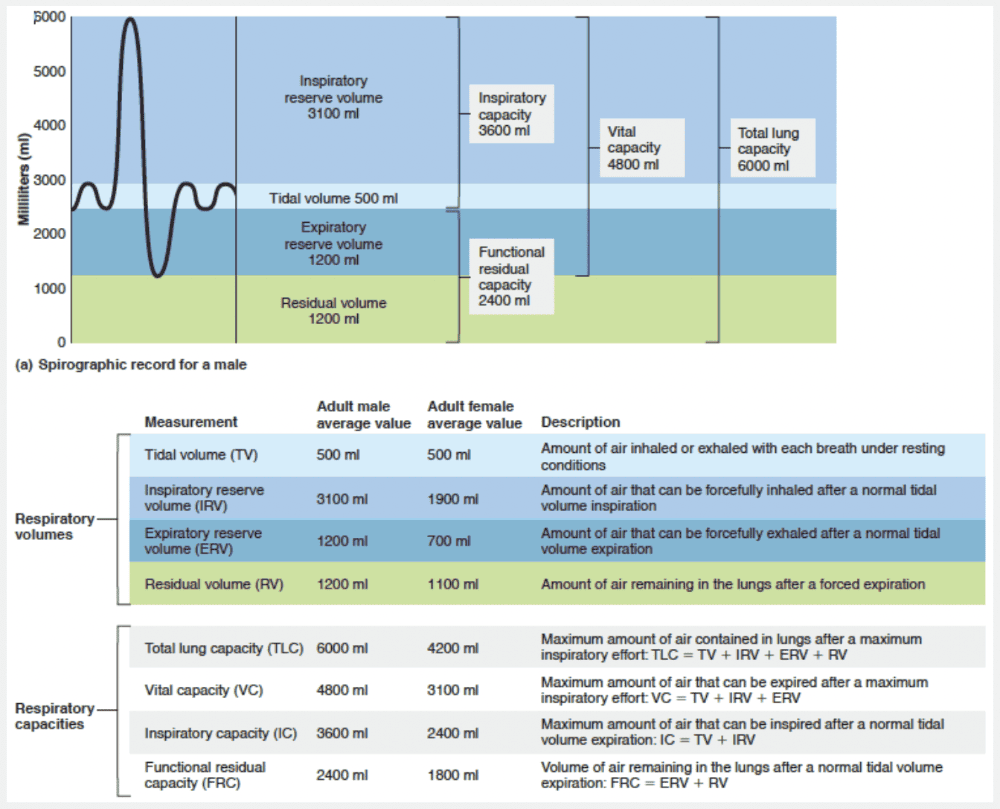
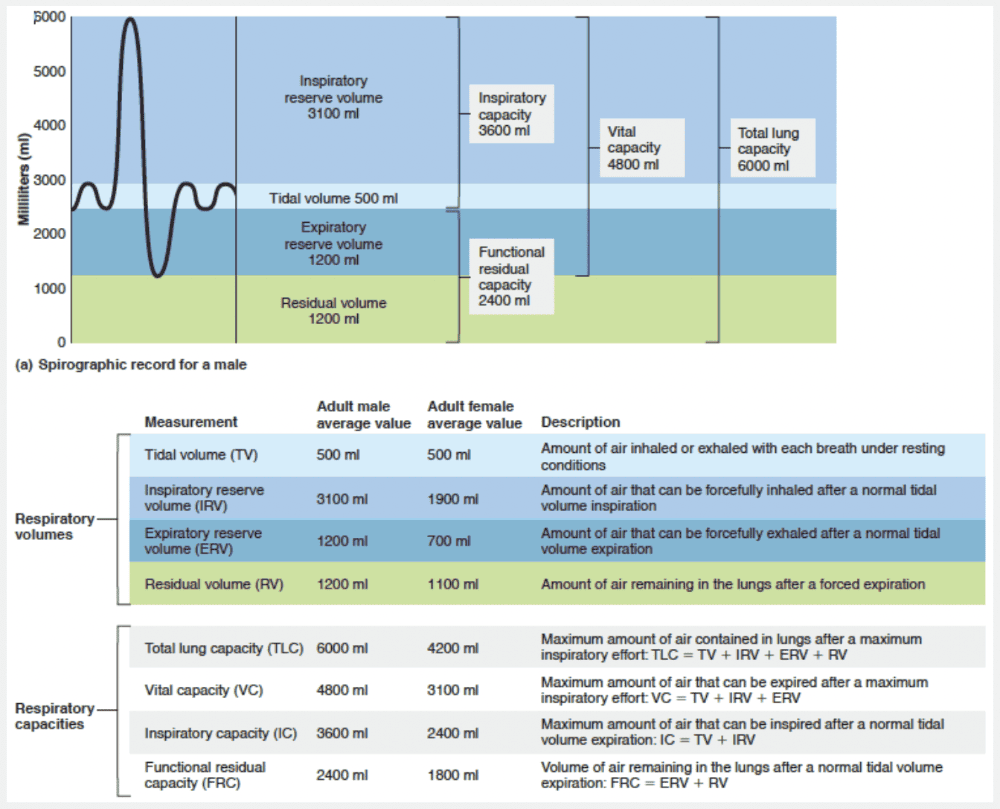
In restrictive diseases, VC, TLC, FRC, and RV decline because lung expansion is limited, whereas in obstructive diseases, TLC, FRC, and RV may increase because the lungs hyperinflate.
Match the following gas law to the appropriate respiratory event: Boyle's law.
- Pressure and volume have an inverse relationship. Inspiration increases lung volume by enlarging all of its dimensions; this lowers gas pressure inside the lungs.
- The more a lung expands for a given rise in transpulmonary pressure, the greater its compliance.
- When a mixture of gases is in contact with a liquid, each gas will dissolve in the liquid in proportion to its partial pressure; this affects the movement of oxygen gas from the lungs into fluids in the tissues.
- Each gas in a mixture has a partial pressure (pp) that is proportional to the percentage of that gas in the gas mixture; therefore, if the pp of oxygen is higher in the blood than in the cells, it will diffuse from the blood into the cells.
Pressure and volume have an inverse relationship. Inspiration increases lung volume by enlarging all of its dimensions; this lowers gas pressure inside the lungs.
Ex.
Boyles law describes how pressure and volume have an inverse relationship. Inspiration increases lung volume by enlarging all of its dimensions; this lowers gas pressure inside the lungs.
Boyle’s law gives the relationship between the pressure and volume of a gas: At constant temperature, the pressure of a gas varies inversely with its volume. That is,
P1V1 = P2V2
where P is the pressure of the gas, V is its volume, and subscripts 1 and 2 represent the initial and resulting conditions, respectively.
Gases always fill their container. Consequently, in a large container, the molecules in a given amount of gas will be far apart and the pressure will be low. But if the volume of the container is reduced, the gas molecules will be forced closer together and the pressure will rise.
A good example is an inflated automobile tire. The tire is hard and strong enough to bear the weight of a car because air is compressed to about one-third of its atmospheric volume inside the tire, providing high pressure.
Partial pressures of a gas are defined by Dalton’s law, which states that the total pressure exerted by a mixture of gases is the sum of the pressures exerted independently by each gas in the mixture.
The amount of gas dissolved in solution is given by Henry’s law, which states that when a gas is in contact with a liquid, the gas will dissolve in the liquid in proportion to its partial pressure.
The more a lung expands for a given rise in transpulmonary pressure, the greater its compliance is the relationship called lung compliance.
Match the following term with its correct description: Pulmonary ventilation.
- Movement of oxygen from the lungs to the blood, and of carbon dioxide from the blood to the lungs
- Transport of oxygen from lungs to body cells and carbon dioxide from tissue cells to lungs
- Movement of air into and out of the lungs so that gases are continuously changed and refreshed
- The fairly rigid conduits for air to reach the gas exchange sites in the lungs
- The actual site of gas exchange in the lungs
- Movement of oxygen from the blood to tissue cells, and of carbon dioxide from tissue cells to blood
Movement of air into and out of the lungs so that gases are continuously changed and refreshed
Ex.
Pulmonary ventilation causes movement of air into and out of the lungs so that gases are continuously changed and refreshed.
Pulmonary ventilation (commonly called breathing): Air is moved into and out of the lungs (during inspiration and expiration) so the gases there are continuously changed and refreshed.
Pulmonary ventilation, consisting of inspiration and expiration, is a mechanical process that depends on volume changes in the thoracic cavity. A rule to keep in mind is that volume changes lead to pressure changes, and pressure changes lead to the flow of gases to equalize the pressure.
Transport of oxygen from lungs to body cells and carbon dioxide from tissue cells to lungs is a transport function of the cardiovascular system.
Movement of oxygen from the blood to tissue cells, and of carbon dioxide from tissue cells to blood is internal respiration.
The fairly rigid conduits for air to reach the gas exchange sites in the lungs are the respiratory passages that are part of the conducting zone.
Match the following: “A.”
- Amount of air remaining in the lungs after a forced expiration
- Volume of air remaining in the lungs after a normal tidal volume expiration
- Maximum amount of air that can be expired after a maximum inspiratory effort
- Maximum amount of air that can be inspired after a normal tidal volume expiration
- Amount of air inhaled or exhaled with each breath under resting conditions
- Maximum amount of air contained in lungs after a maximum inspiratory effort
Amount of air inhaled or exhaled with each breath under resting conditions
Ex.
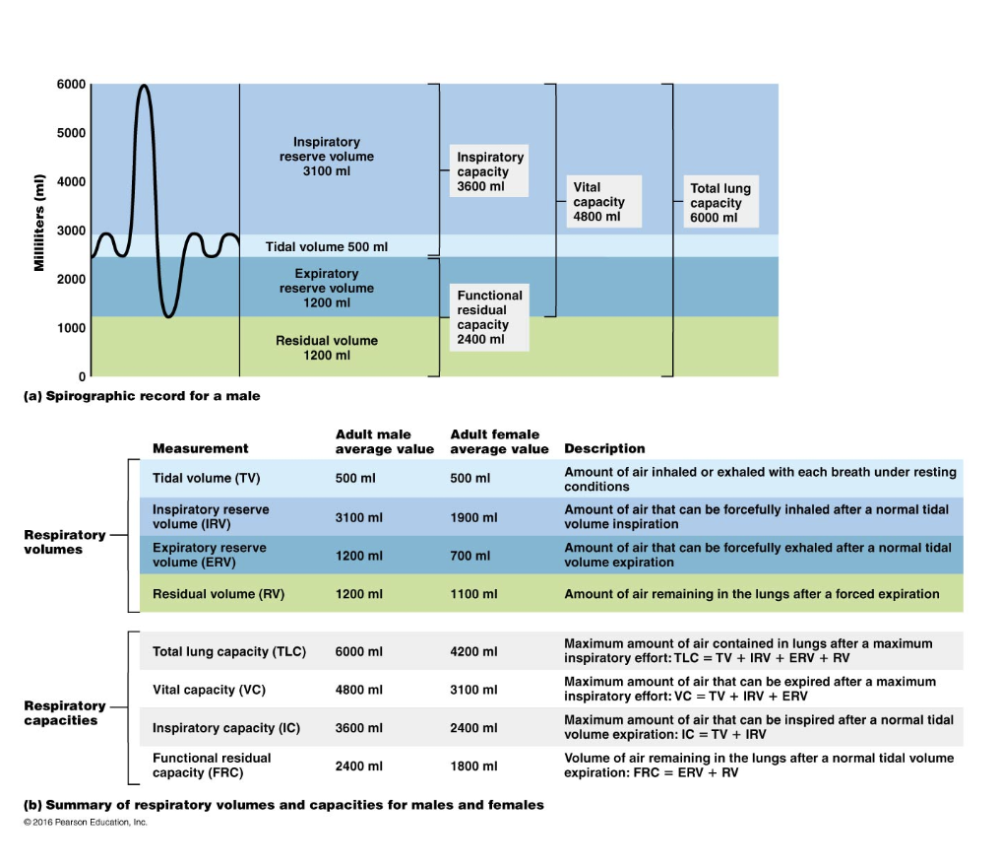
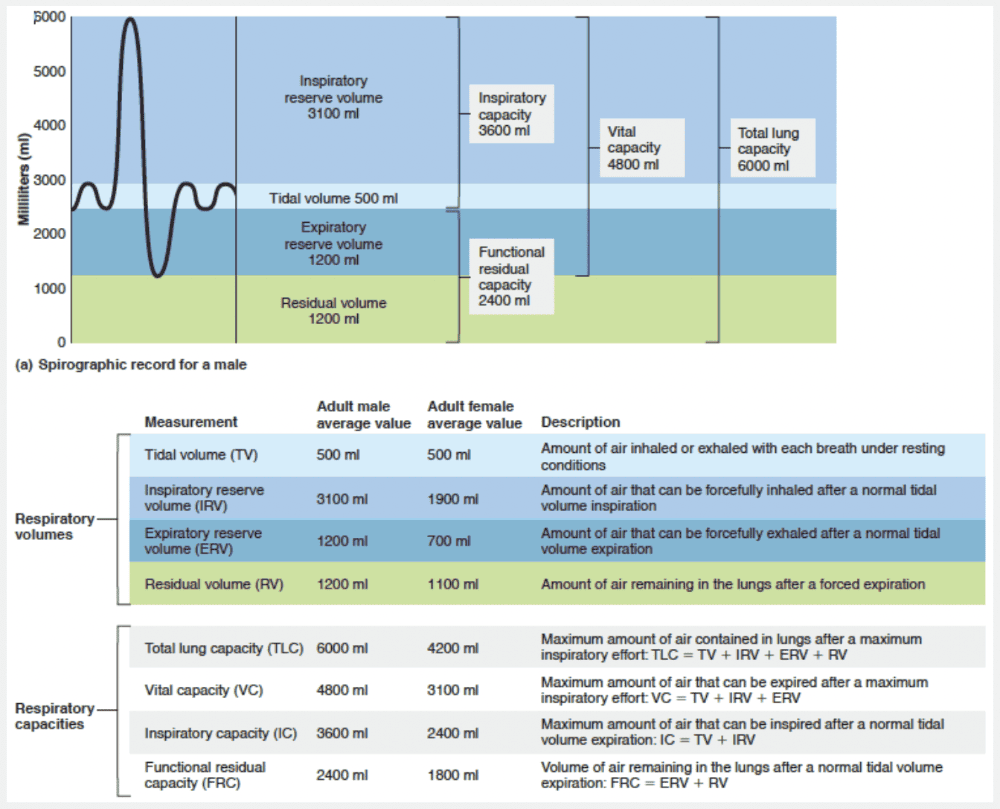
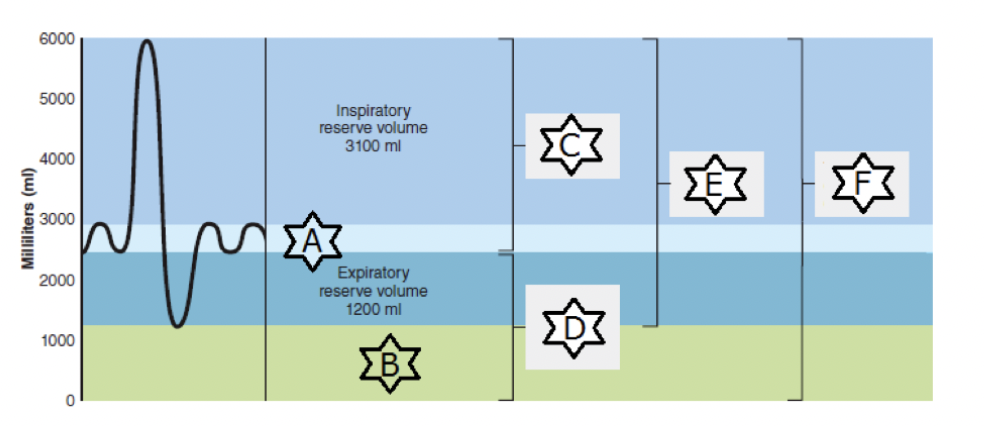
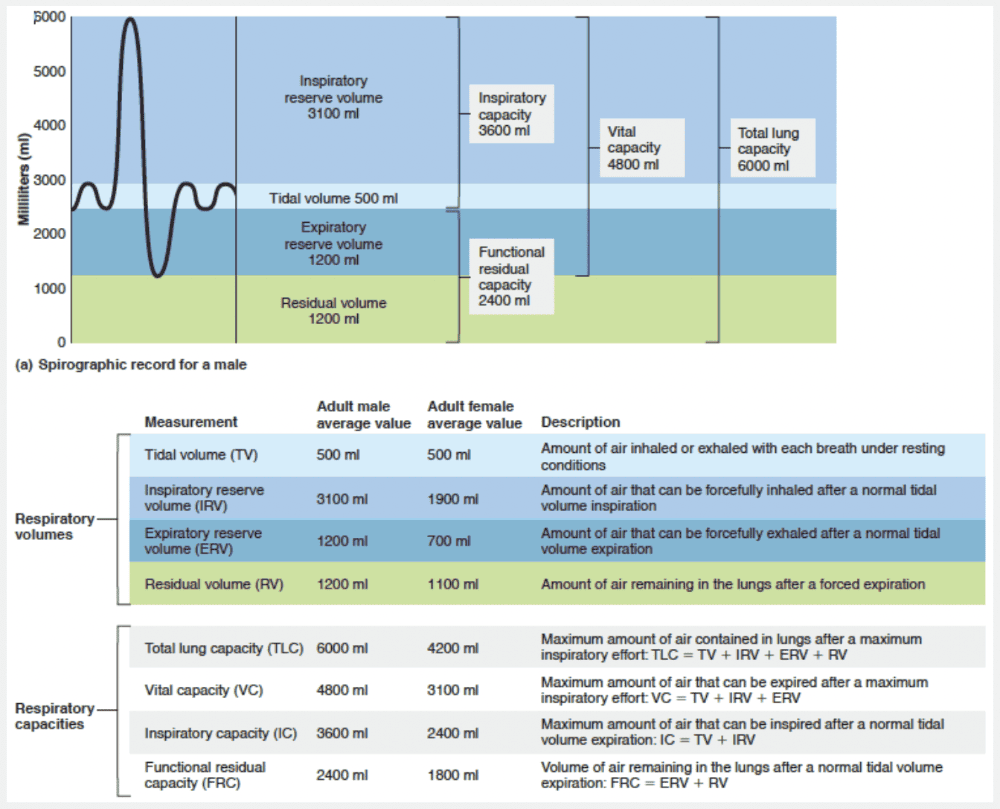
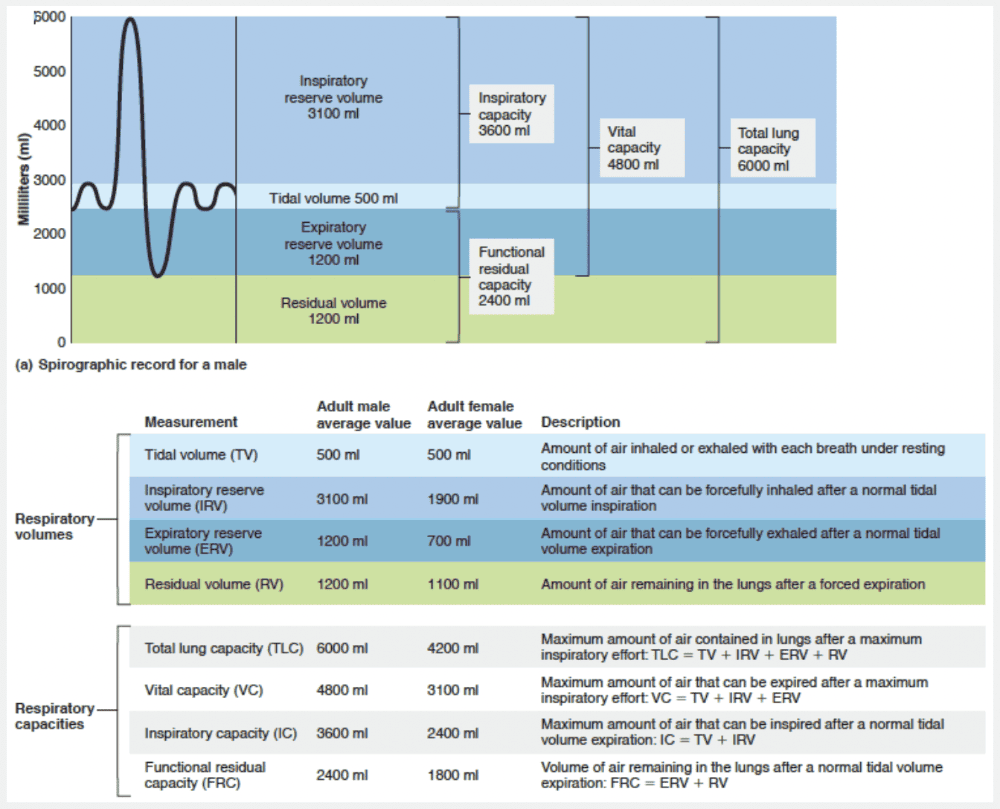
“A” represents tidal volume, the amount of air inhaled or exhaled with each breath under resting conditions.
Match the following volume or capacity to its correct description: Vital capacity.
- About 6000 ml in an average male
- Volume that can be forced in after a tidal inhalation
- Volume of air in lungs after normal tidal expiration
- About 500 ml
- Maximum volume of air that can be exhaled after maximum inhalation
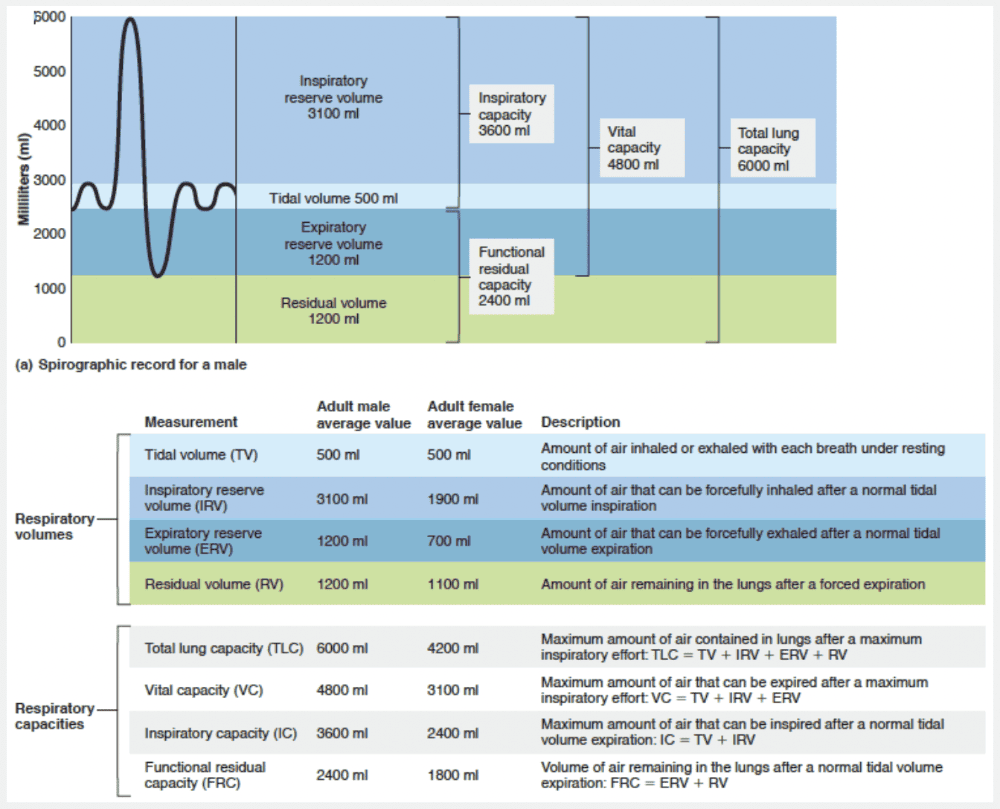
Maximum volume of air that can be exhaled after maximum inhalation
Ex.
Vital capacity is the maximum volume of air that can be exhaled after maximum inhalation.
The respiratory capacities include inspiratory, functional residual, vital, and total lung capacities. The respiratory capacities always consist of two or more lung volumes.
- Inspiratory capacity (IC) is the total amount of air that can be inspired after a normal tidal volume expiration, so it is the sum of TV and IRV.
- Functional residual capacity (FRC) represents the amount of air remaining in the lungs after a normal tidal volume expiration and is the combined RV and ERV.
- Vital capacity (VC) is the total amount of exchangeable air. It is the sum of TV, IRV, and ERV.
- Total lung capacity (TLC) is the sum of all lung volumes. Lung volumes and capacities (with the possible exception of TV) tend to be smaller in women than in men because of women’s smaller size.
The maximum amount of air that can be inhaled after a normal inspiration is the inspiratory reserve volume.
6000 ml is the typical total lung volume in an average adult male.
In the alveoli, the partial pressure of oxygen is __________.
- lower than the PO2 of venous blood
- much higher than the PO2 of arterial blood
- equal to that in the tissues
- about 104 mm Hg
- the same as the PO2 of venous blood.
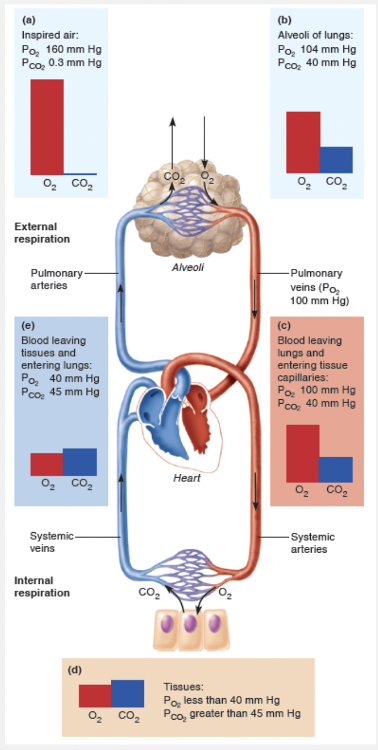
about 104 mm Hg
Ex.
In the alveoli, the partial pressure of oxygen is about 104 mm Hg.
Partial pressure gradients of O2 and CO2 drive the diffusion of these gases across the respiratory membrane. A steep oxygen partial pressure gradient exists across the respiratory membrane because the PO2 of deoxygenated blood in the pulmonary arteries is only 40 mm Hg, as opposed to a PO2 of approximately 104 mm Hg in the alveoli. As a result, O2 diffuses rapidly from the alveoli into the pulmonary capillary blood.
The movement of air into and out of the lungs is called __________.
- cellular respiration
- internal respiration
- external respiration
- oxidative phosphorylation
- pulmonary ventilation
pulmonary ventilation
Ex.
The movement of air into and out of the lungs is called pulmonary ventilation.
Pulmonary ventilation, consisting of inspiration and expiration, is a mechanical process that depends on volume changes in the thoracic cavity. A rule to keep in mind is that volume changes lead to pressure changes, and pressure changes lead to the flow of gases to equalize the pressure.
During external respiration oxygen diffuses from the lungs to the blood, and carbon dioxide diffuses from the blood to the lungs.
During internal respiration oxygen diffuses from blood to tissue cells, and carbon dioxide diffuses from tissue cells to blood.
Oxidative phosphorylation is used during the process of cellular respiration to produce ATP within the mitochondria.
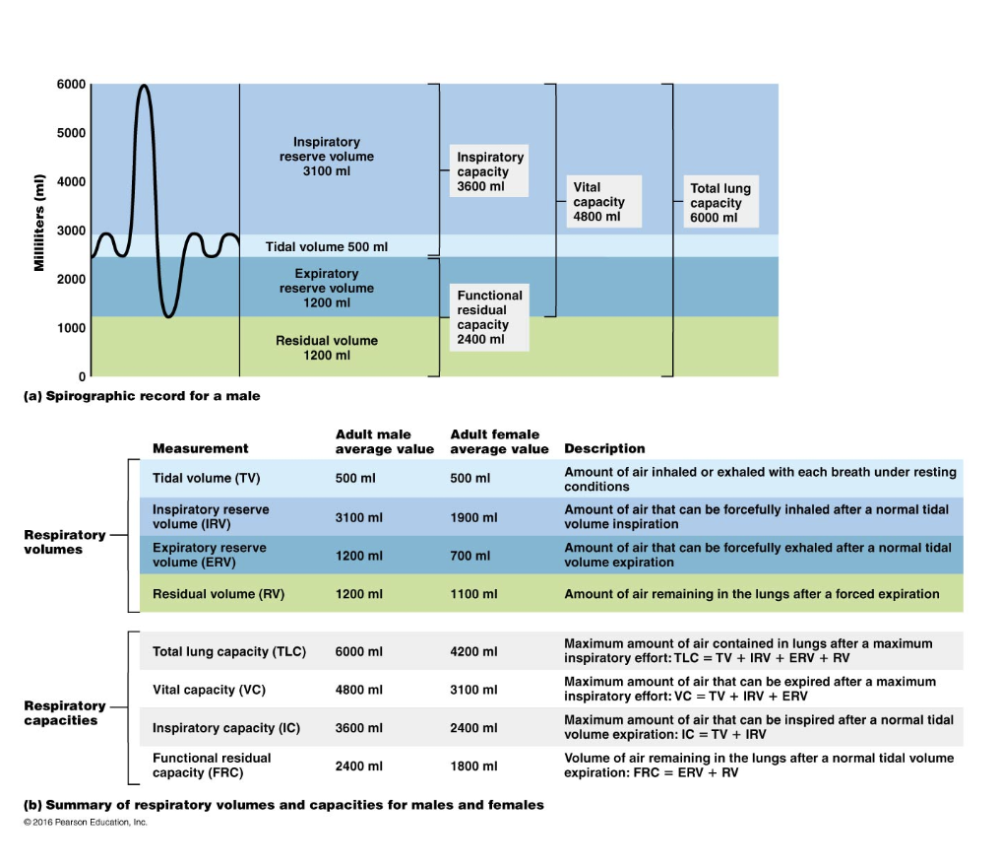
What value(s) would be affected by an obstructive disorder?
- TLC and FRC alone
- FRC
- Only TLC
- TLC, FRC, and RV may increase
- Tidal volume
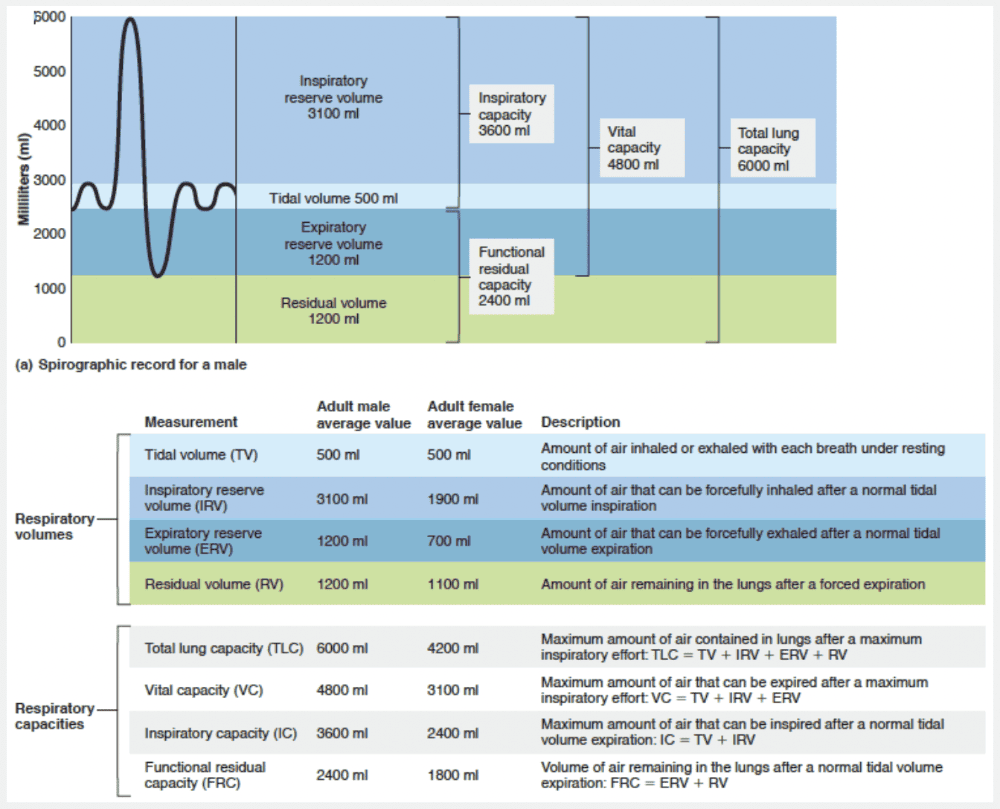
TLC, FRC, and RV may increase
Ex.
In obstructive diseases, TLC, FRC, and RV may increase because the lungs hyperinflate, whereas in restrictive diseases, VC, TLC, FRC, and RV decline because lung expansion is limited.
Air moves into the lungs because __________.
- the gas pressure in the lungs becomes lower than the outside pressure as the diaphragm contracts
- contraction of the diaphragm decreases the volume of the pleural cavity
- the volume of the lungs decreases with inspiration
- the thorax is muscular
- the internal intercostal muscles decrease the thoracic cavity volume
the gas pressure in the lungs becomes lower than the outside pressure as the diaphragm contracts
Ex.
Air moves into the lungs because the gas pressure in the lungs becomes lower than the outside pressure as the diaphragm contracts.
As the thoracic dimensions increase during inspiration, the lungs are stretched and the intrapulmonary volume increases. As a result, Ppul drops about 1 mm Hg relative to Patm. Anytime the intrapulmonary pressure is less than the atmospheric pressure (Ppul < Patm), air rushes into the lungs along the pressure gradient. Inspiration ends when Ppul = Patm. During the same period, Pip declines to about −6 mm Hg relative to Patm.
Which of the following is false?
- AVR drops dramatically during rapid shallow breathing because most of the inspired air never reaches the exchange sites.
- The minute ventilation is the total amount of gas that flows into or out of the respiratory tract in 1 minute.
- Because anatomical dead space is constant in a particular individual, increasing the volume of each inspiration (breathing depth) enhances AVR and gas exchange more than raising the respiratory rate.
- Minute ventilation values are the best way to assess respiratory efficiency.
Minute ventilation values are the best way to assess respiratory efficiency.
Ex.
It would be false to say that minute ventilation values are the best way to assess respiratory efficiency.
The minute ventilation is the total amount of gas that flows into or out of the respiratory tract in 1 minute. During normal quiet breathing, the minute ventilation in healthy people is about 6 L/min (500 ml per breath multiplied by 12 breaths per minute). During vigorous exercise, the minute ventilation may reach 200 L/min.
Minute ventilation values provide a rough yardstick for assessing respiratory efficiency, but the alveolar ventilation rate (AVR) is a better index of effective ventilation. The AVR takes into account the volume of air wasted in the dead space and measures the flow of fresh gases in and out of the alveoli during a particular time interval. We can compute AVR using this equation:
AVR = frequency × (TV − dead space)
(ml/min) (breaths/min) (ml/breath)
In healthy people, AVR is usually about 12 breaths per minute times the difference of 500 − 150 ml per breath, or 4200 ml/min.
Because anatomical dead space is constant in a particular individual, increasing the volume of each inspiration (breathing depth) enhances AVR and gas exchange more than raising the respiratory rate. AVR drops dramatically during rapid shallow breathing because most of the inspired air never reaches the exchange sites. Furthermore, as tidal volume approaches the dead space value, effective ventilation approaches zero, regardless of how fast a person is breathing.
Match the following volume or capacity to its correct description: Tidal volume.
- About 500 ml
- Volume of air in lungs after normal tidal expiration
- About 6000 ml in an average male
- Maximum volume of air that can be exhaled after maximum inhalation
- Volume that can be forced in after a tidal inhalation
About 500 ml
Ex.
Tidal volume is about 500 ml.
The respiratory capacities include inspiratory, functional residual, vital, and total lung capacities. The respiratory capacities always consist of two or more lung volumes.
- Inspiratory capacity (IC) is the total amount of air that can be inspired after a normal tidal volume expiration, so it is the sum of TV and IRV.
- Functional residual capacity (FRC) represents the amount of air remaining in the lungs after a normal tidal volume expiration and is the combined RV and ERV.
- Vital capacity (VC) is the total amount of exchangeable air. It is the sum of TV, IRV, and ERV. It is the maximum amount of air that can be exhaled after a maximum inhalation.
- Total lung capacity (TLC) is the sum of all lung volumes. Lung volumes and capacities (with the possible exception of TV) tend to be smaller in women than in men because of women’s smaller size.
6000 ml is the typical total lung capacity for an average adult male.
Which of the following movements would not ventilate the alveoli?
- Crying
- Yawning
- Hiccups
- Sneezing
- Burping
Burping
Ex.
Burping does not ventilate the alveoli.
Many processes other than breathing move air into or out of the lungs, altering the normal respiratory rhythm. These non-respiratory air movements occur whenever you cough, sneeze, cry, laugh, hiccup, or yawn. Some can be produced voluntarily, but some (such as sneezing and hiccups) are reflexive.
Which respiratory measurement is normally the greatest?
- Expiratory reserve volume
- Tidal volume
- Vital capacity
- Residual volume
- Inspiratory capacity
Vital capacity
Ex.
Vital capacity is the greatest of the volumes given.
The respiratory capacities include inspiratory, functional residual, vital, and total lung capacities. The respiratory capacities always consist of two or more lung volumes.
- Inspiratory capacity (IC) is the total amount of air that can be inspired after a normal tidal volume expiration, so it is the sum of TV and IRV.
- Functional residual capacity (FRC) represents the amount of air remaining in the lungs after a normal tidal volume expiration and is the combined RV and ERV.
- Vital capacity (VC) is the total amount of exchangeable air. It is the sum of TV, IRV, and ERV. It is the maximum amount of air that can be exhaled after a maximum inhalation.
- Total lung capacity (TLC) is the sum of all lung volumes. Lung volumes and capacities (with the possible exception of TV) tend to be smaller in women than in men because of women’s smaller size.
The transpulmonary pressure is the difference between the __________ and the __________ pressure.
- atmospheric; intrapleural
- intrapulmonary; intrapleural
- intrapleural; andatmospheric
- intrapulmonary; atmospheric
intrapulmonary; intrapleural
Ex.
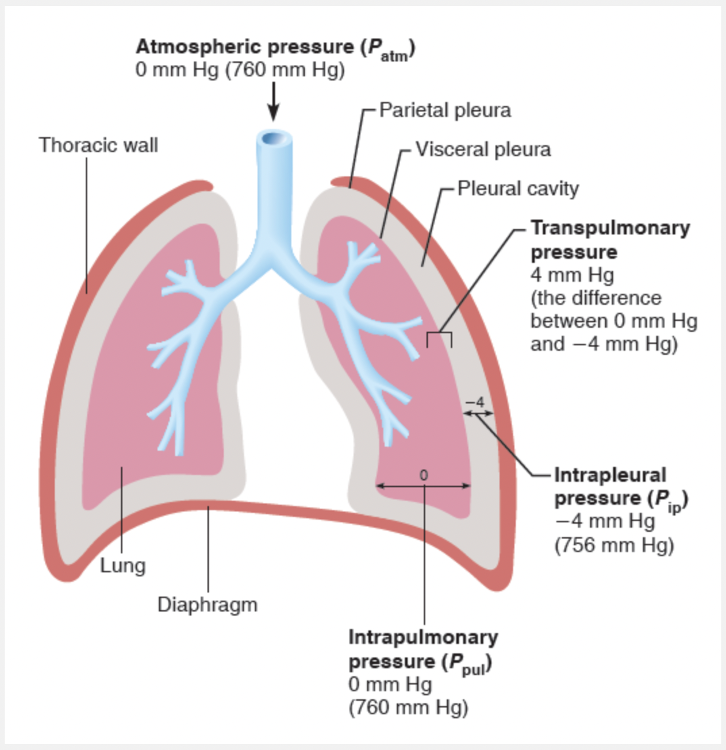
The transpulmonary pressure is the difference between the intrapulmonary and intrapleural pressures (Ppul – Pip).
It is this pressure that keeps the air spaces of the lungs open or, phrased another way, keeps the lungs from collapsing. Moreover, the size of the transpulmonary pressure determines the size of the lungs at any time—the greater the transpulmonary pressure, the larger the lungs. We cannot overemphasize the importance of negative pressure in the intrapleural space and the tight coupling of the lungs to the thorax wall. Any condition that equalizes Pip with the intrapulmonary (or atmospheric) pressure causes immediate lung collapse.
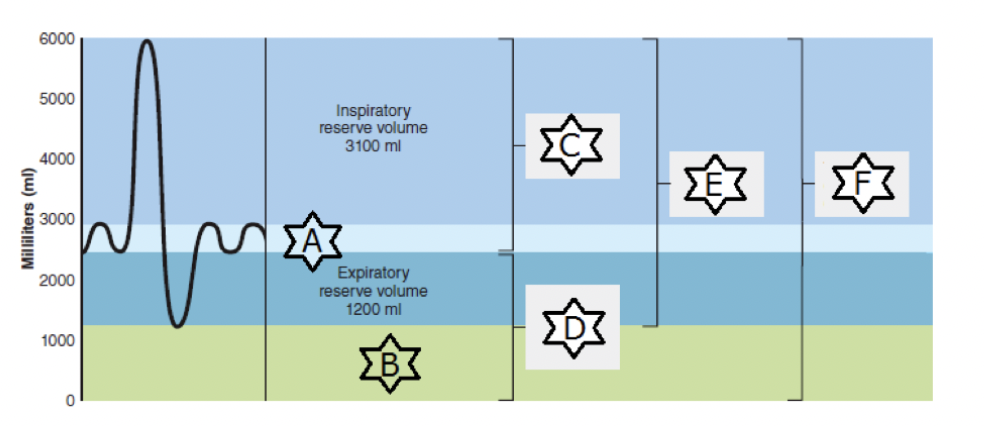
Match the following: “F.”
- Maximum amount of air contained in lungs after a maximum inspiratory effort
- Amount of air remaining in the lungs after a forced expiration
- Maximum amount of air that can be expired after a maximum inspiratory effort
- Volume of air remaining in the lungs after a normal tidal volume expiration
- Maximum amount of air that can be inspired after a normal tidal volume expiration
- Amount of air inhaled or exhaled with each breath under resting conditions
Maximum amount of air contained in lungs after a maximum inspiratory effort
Ex.
“F” represents total lung capacity, the maximum amount of air contained in lungs after a maximum inspiratory effort.
FEV1 can be used to diagnose what condition?
- Infection in the lung
- Restrictive pulmonary disorders
- Obstructive pulmonary disorders
Obstructive pulmonary disorders
Ex.
FEV1 can be used to diagnose obstructive pulmonary disorders.
The volume exhaled during the first second is FEV1. Those with healthy lungs can exhale about 80% of the forced vital capacity (FVC) within 1 second. Those with obstructive pulmonary disease exhale considerably less than 80% of the FVC within 1 second, while those with restrictive disease can exhale 80% or more of FVC in 1 second even though their FVC is reduced.
Which of the following conditions would not cause atelectasis?
- Rupture of the visceral pleura
- Increased atmospheric pressure
- Pneumonia
- Air entering the pleural cavity
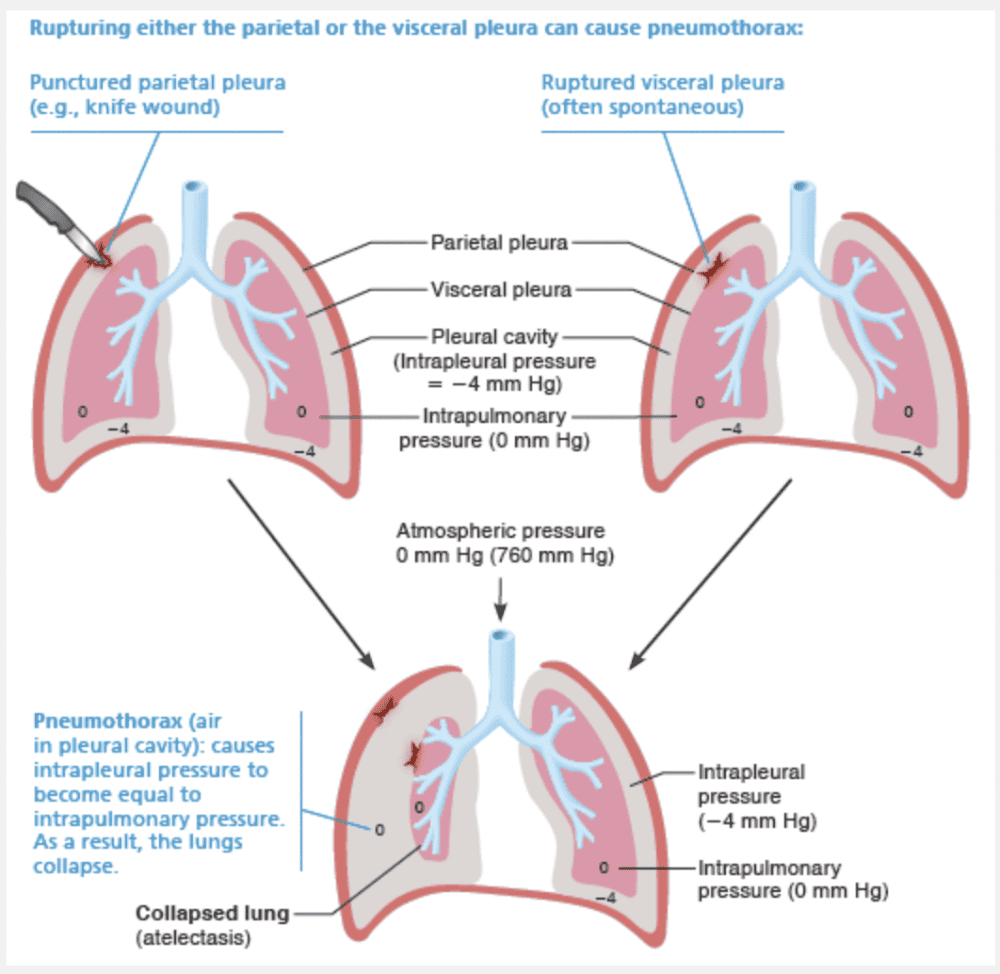
Increased atmospheric pressure
Ex.
Increased atmospheric pressure would not cause atelectasis.
Atelectasis (at”ĕ-lik’tah-sis), or lung collapse, occurs when a bronchiole becomes plugged (as may follow pneumonia). Its associated alveoli then absorb all of their air and collapse. Atelectasis can also occur when air enters the pleural cavity either through a chest wound or a rupture of the visceral pleura, which allows air from the respiratory tract to enter the pleural cavity. The presence of air in the pleural cavity is referred to as a pneumothorax (nu”mo-tho’raks; “air thorax”), and is reversed by drawing air out of the intrapleural space with chest tubes. This procedure allows the pleurae to heal and the lung to re-inflate and resume normal function.
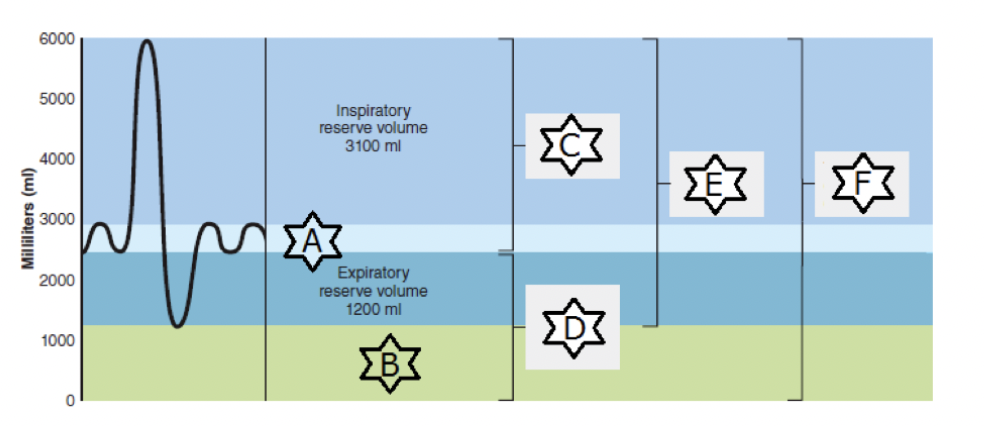
Match the following: “D.”
- Maximum amount of air that can be inspired after a normal tidal volume expiration
- Maximum amount of air contained in lungs after a maximum inspiratory effort
- Volume of air remaining in the lungs after a normal tidal volume expiration
- Maximum amount of air that can be expired after a maximum inspiratory effort
- Amount of air inhaled or exhaled with each breath under resting conditions
- Amount of air remaining in the lungs after a forced expiration
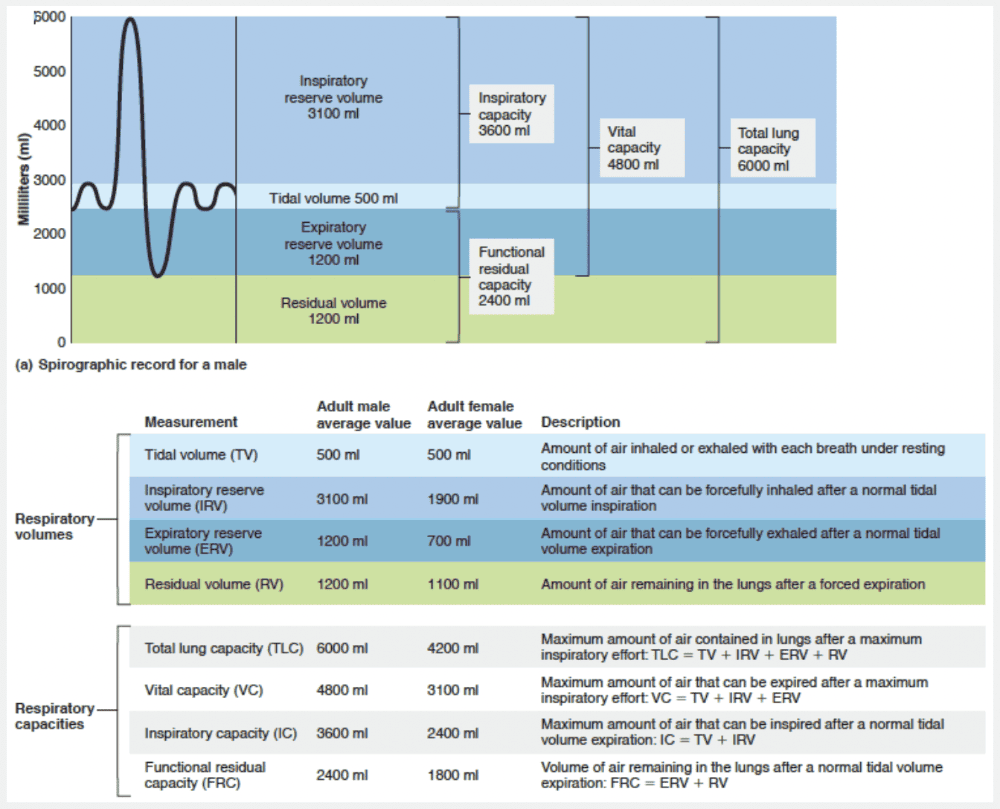
Volume of air remaining in the lungs after a normal tidal volume expiration
Ex.
“D” represents functional residual capacity, the volume of air remaining in the lungs after a normal tidal volume expiration.
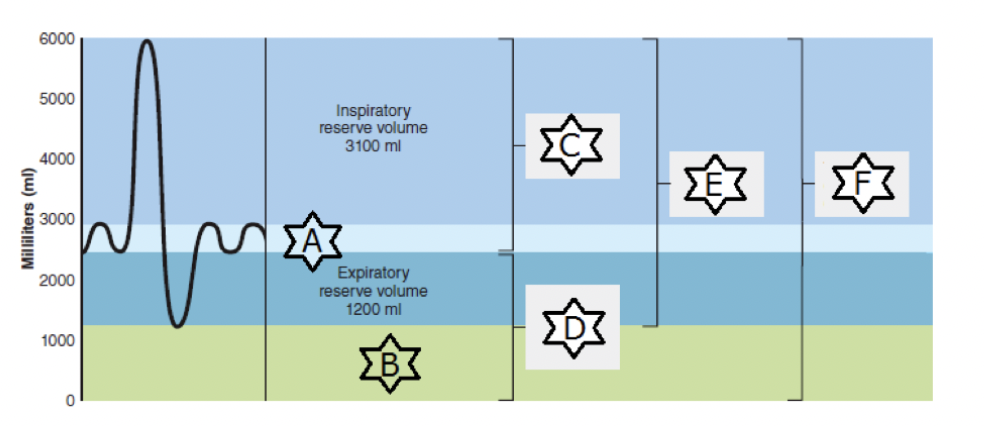
Match the following: “C.”
- Maximum amount of air contained in lungs after a maximum inspiratory effort
- Volume of air remaining in the lungs after a normal tidal volume expiration
- Maximum amount of air that can be expired after a maximum inspiratory effort
- Amount of air inhaled or exhaled with each breath under resting conditions
- Amount of air remaining in the lungs after a forced expiration
- Maximum amount of air that can be inspired after a normal tidal volume expiration
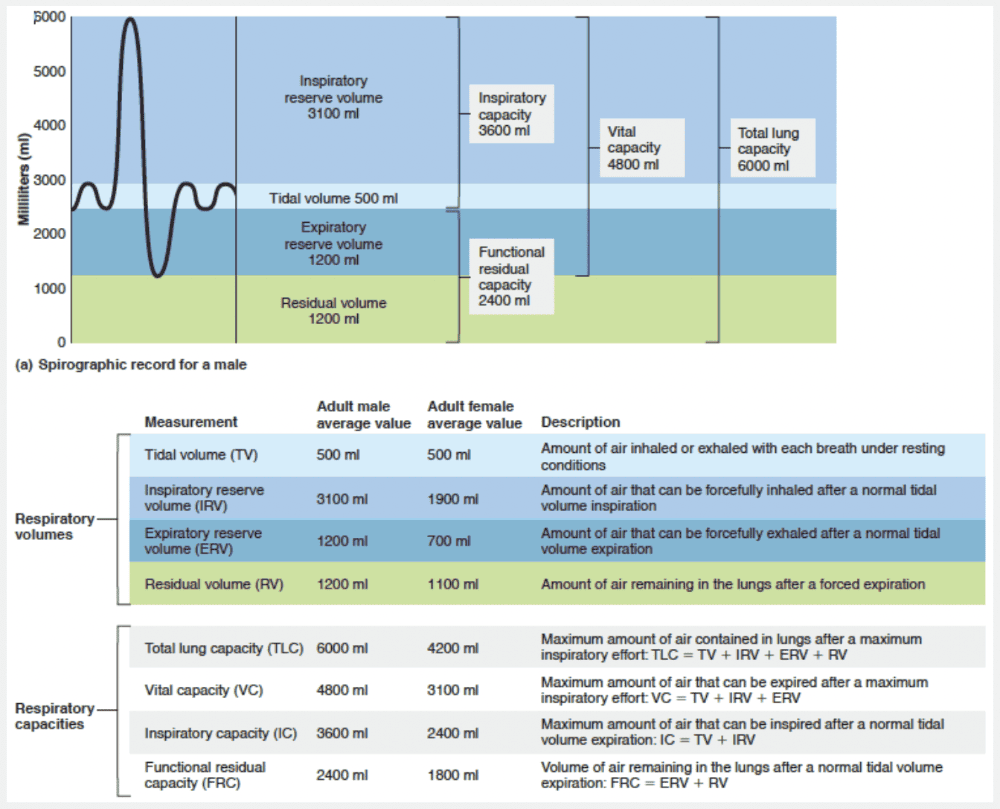
Maximum amount of air that can be inspired after a normal tidal volume expiration
Ex.
“C” represents inspiratory capacity, the maximum amount of air that can be inspired after a normal tidal volume expiration.
Match the following volume or capacity to its correct description: Total lung capacity.
- About 500 ml
- Maximum volume of air that can be exhaled after maximum inhalation
- Volume of air in lungs after normal tidal expiration
- Volume that can be forced in after a tidal inhalation
- About 6000 ml in an average male
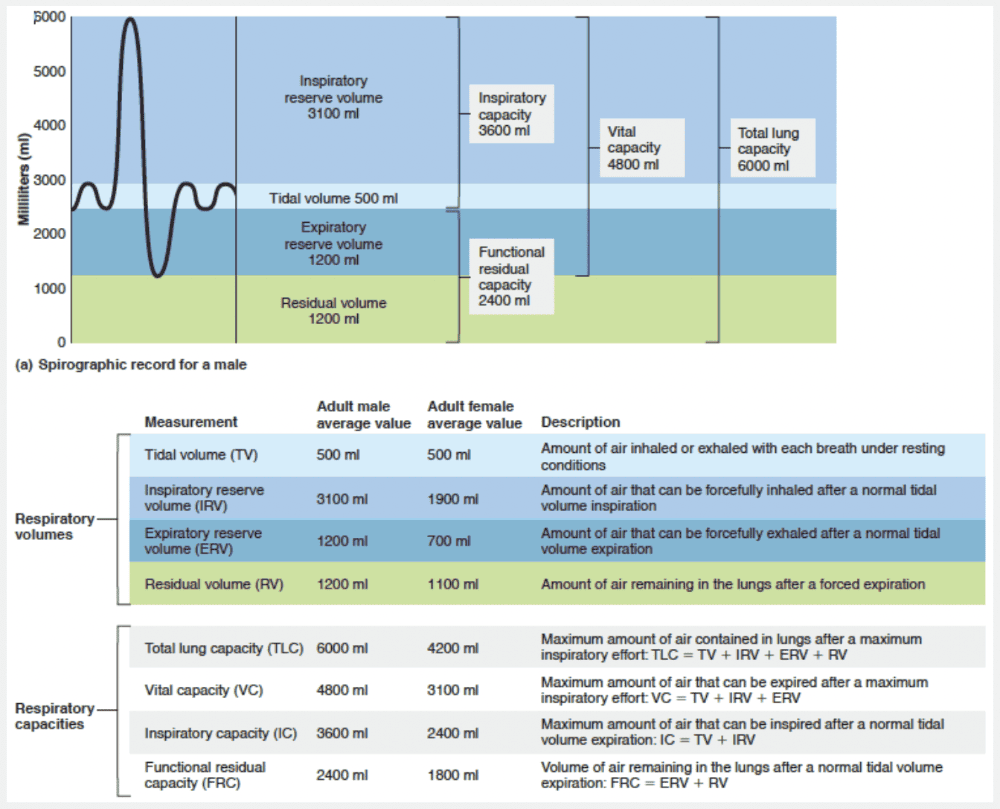
About 6000 ml in an average male
Ex.
Total lung capacity is about 6000 ml in an average male.
The respiratory capacities include inspiratory, functional residual, vital, and total lung capacities. The respiratory capacities always consist of two or more lung volumes.
- Inspiratory capacity (IC) is the total amount of air that can be inspired after a normal tidal volume expiration, so it is the sum of TV and IRV.
- Functional residual capacity (FRC) represents the amount of air remaining in the lungs after a normal tidal volume expiration and is the combined RV and ERV.
- Vital capacity (VC) is the total amount of exchangeable air. It is the sum of TV, IRV, and ERV. It is the maximum amount of air that can be exhaled after a maximum inhalation.
- Total lung capacity (TLC) is the sum of all lung volumes. Lung volumes and capacities (with the possible exception of TV) tend to be smaller in women than in men because of women’s smaller size.
The maximum amount of air that can be inhaled after a normal inspiration is the inspiratory reserve volume.
500 ml is the typical tidal volume.
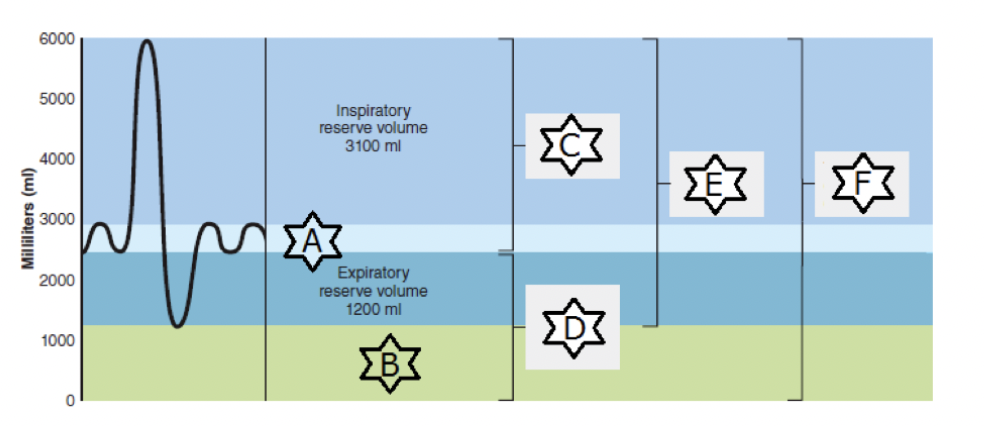
Match the following: “B.”
- Maximum amount of air that can be expired after a maximum inspiratory effort
- Volume of air remaining in the lungs after a normal tidal volume expiration
- Amount of air remaining in the lungs after a forced expiration
- Maximum amount of air that can be inspired after a normal tidal volume expiration
- Amount of air inhaled or exhaled with each breath under resting conditions
- Maximum amount of air contained in lungs after a maximum inspiratory effort
Amount of air remaining in the lungs after a forced expiration
Ex.
“B” represents residual volume, the amount of air remaining in the lungs after a forced expiration.
Match the following: IRDS.
- Such strong bronchoconstriction that pulmonary ventilation almost completely stops, regardless of the pressure gradient
- Often results from pneumonia
- Collapse of alveoli due to little surfactant
- Inflammation of the pleurae
Collapse of alveoli due to little surfactant
Ex.
IRDS, Infant Resiratory Distress Syndrome, is collapse of alveoli due to little surfactant.
When too little surfactant is present, surface tension can collapse the alveoli. Once this happens, the alveoli must be completely reinflated during each inspiration, an effort that uses tremendous amounts of energy. This is the problem faced by newborns with infant respiratory distress syndrome (IRDS), a condition common in premature babies. Since fetal lungs do not produce adequate amounts of surfactant until the last two months of development, babies born prematurely often are unable to keep their alveoli inflated between breaths.
IRDS is treated by spraying natural or synthetic surfactant into the newborn’s respiratory passageways. In addition, devices that maintain positive airway pressure throughout the respiratory cycle can keep the alveoli open between breaths. Severe cases require mechanical ventilators.
Many IRDS survivors suffer from bronchopulmonary dysplasia, a chronic lung disease, during childhood and beyond. This condition is believed to result from inflammatory injury caused by mechanically ventilating the premature newborn’s delicate respiratory zone structures.
Inflammation of the pleurae, called pleurisy, often results from pneumonia.
Asthma can result in a strong enough constriction of the bronchioles that air flow is dramatically reduced.
__________ pressure keeps the air spaces in the lung open.
- Transpulmonary pressure
- Atmospheric pressure
- Pleural pressure
- Intrapulmonary pressure
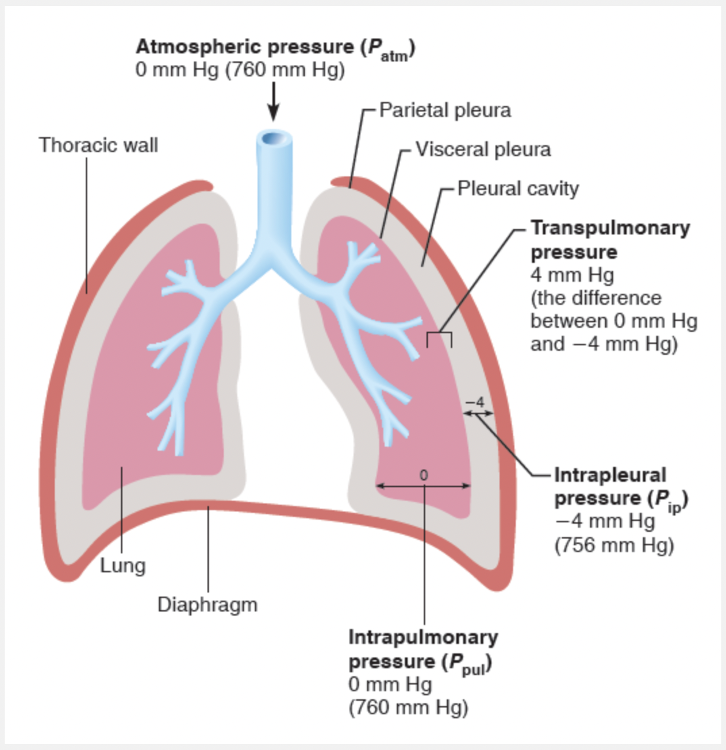
Transpulmonary pressure
Ex.
Transpulmonary pressure keeps the air spaces in the lung open.
The transpulmonary pressure is the difference between the intrapulmonary and intrapleural pressures (Ppul – Pip). It is this pressure that keeps the air spaces of the lungs open or, phrased another way, keeps the lungs from collapsing. Moreover, the size of the transpulmonary pressure determines the size of the lungs at any time—the greater the transpulmonary pressure, the larger the lungs. We cannot overemphasize the importance of negative pressure in the intrapleural space and the tight coupling of the lungs to the thorax wall. Any condition that equalizes Pip with the intrapulmonary (or atmospheric) pressure causes immediate lung collapse.
Intrapulmonary pressure is the pressure inside the lung.
Match the following: Asthma.
- Such strong bronchoconstriction that pulmonary ventilation almost completely stops, regardless of the pressure gradient
- Often results from pneumonia
- Collapse of the lungs due to plugging of bronchioles
- Collapse of alveoli due to little surfactant
Such strong bronchoconstriction that pulmonary ventilation almost completely stops, regardless of the pressure gradient
Ex.
Asthma causes such strong bronchoconstriction that pulmonary ventilation almost completely stops, regardless of the pressure gradient.
Smooth muscle of the bronchiolar walls is exquisitely sensitive to neural controls and certain chemicals. For example, inhaled irritants activate a reflex of the parasympathetic division of the nervous system that causes vigorous constriction of the bronchioles and dramatically reduces air passage diameters. During an acute asthma attack, histamine and other inflammatory chemicals can cause such strong bronchoconstriction that pulmonary ventilation almost completely stops, regardless of the pressure gradient. Conversely, epinephrine released during sympathetic nervous system activation or administered as a drug dilates bronchioles and reduces airway resistance. Local accumulations of mucus, infectious material, or solid tumors in the passageways are important sources of airway resistance in those with respiratory disease.
Whenever airway resistance rises, breathing movements become more strenuous, but such compensation has its limits. When the bronchioles are severely constricted or obstructed, even the most extreme respiratory efforts cannot restore ventilation to life-sustaining levels.
Collapse of the alveoli due to decreased surfactant occurs in infant respiratory distress syndrome.
Pleurisy, inflammation of the pleurae, often results from pneumonia.
Collapse of the lungs due to plugged bronchioles is called atelectasis.
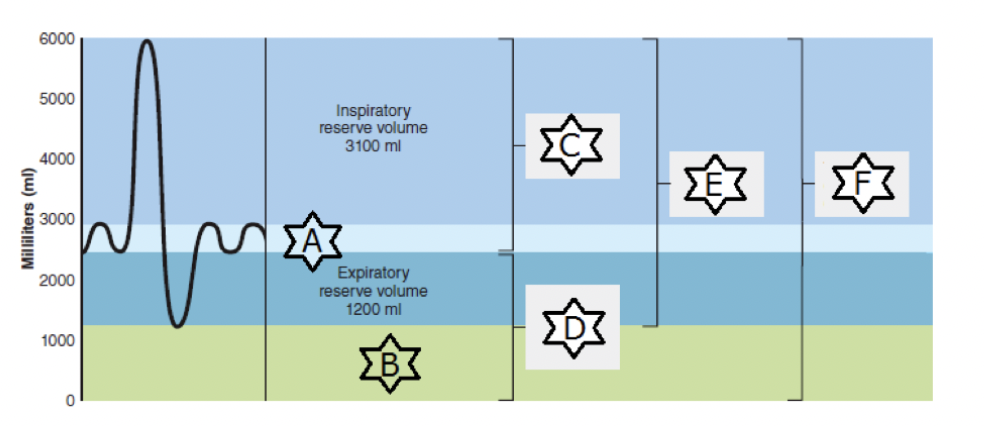
Match the following: “E.”
- Volume of air remaining in the lungs after a normal tidal volume expiration
- Amount of air inhaled or exhaled with each breath under resting conditions
- Amount of air remaining in the lungs after a forced expiration
- Maximum amount of air that can be inspired after a normal tidal volume expiration
- Maximum amount of air that can be expired after a maximum inspiratory effort
- Maximum amount of air contained in lungs after a maximum inspiratory effort
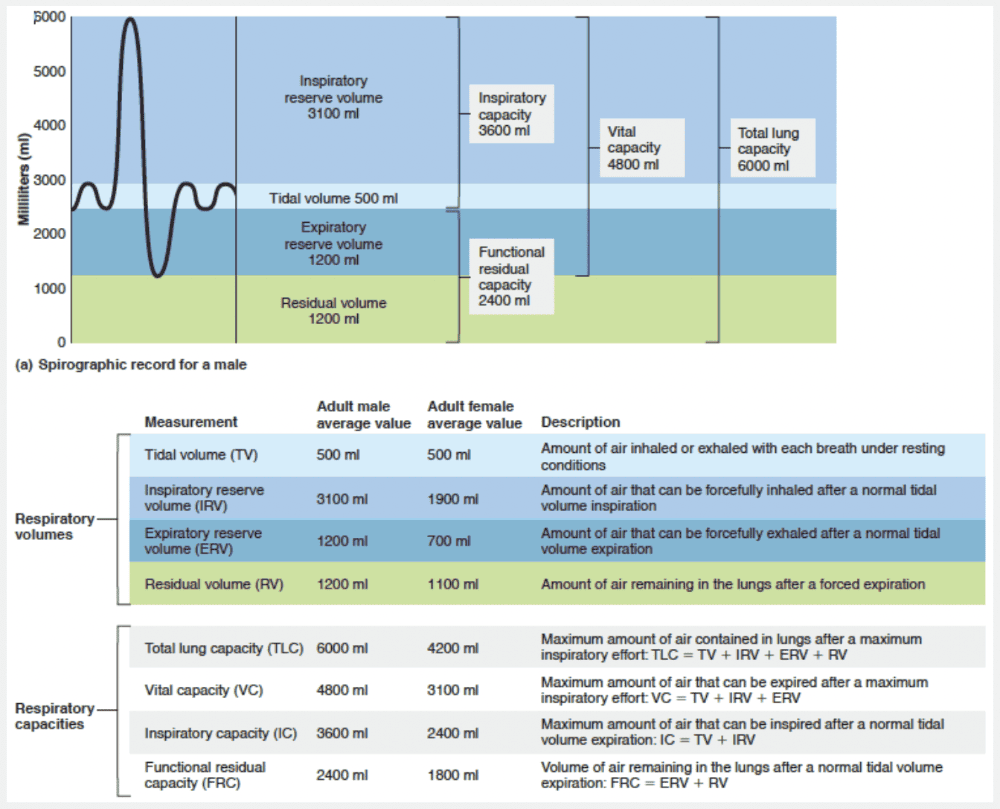
Maximum amount of air that can be expired after a maximum inspiratory effort
Ex.
“E” represents vital capacity, the maximum amount of air that can be expired after a maximum inspiratory effort.