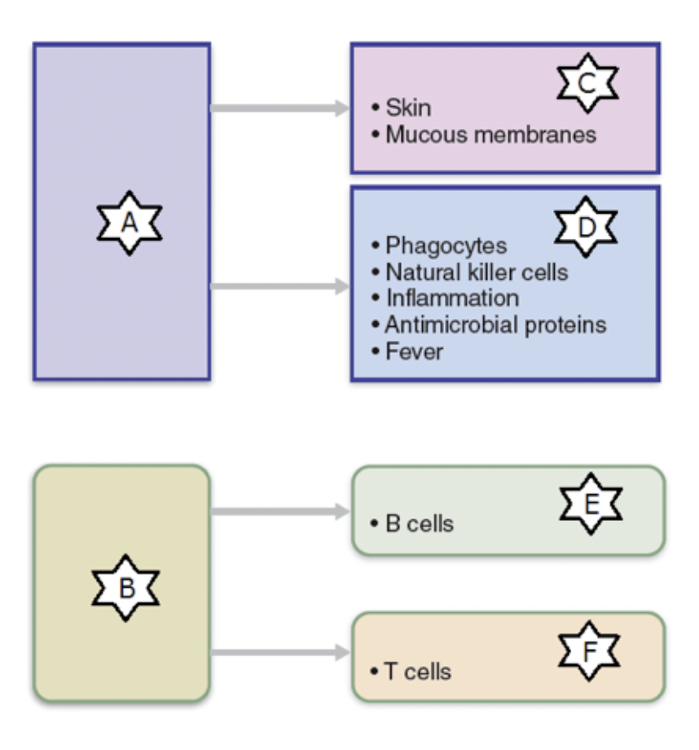
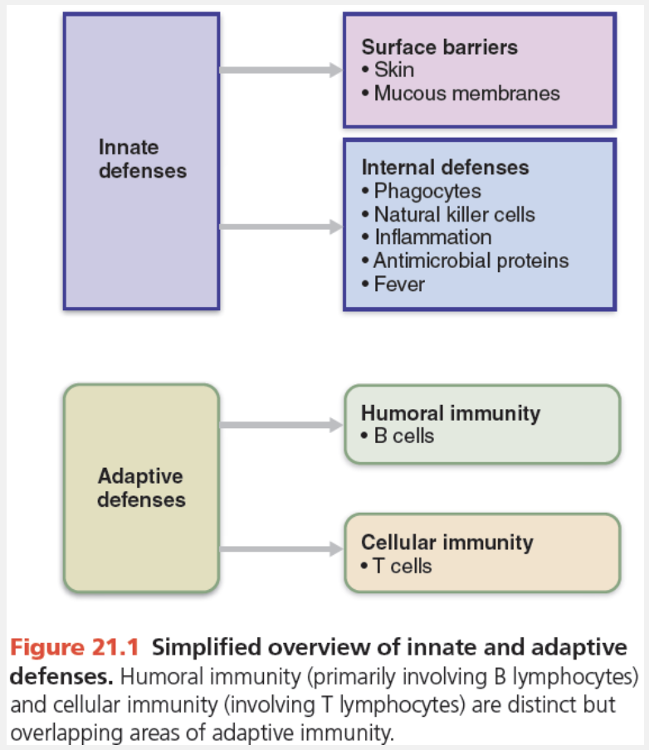
Identify the part of the immune system labelled as “C.”
- Surface barriers
- Internal defenses
- Innate defenses
- Cellular immunity
- Adaptive defenses
- Humoral immunity
Surface barriers
What is the definition of exudate?
- Increased blood flow due to vasodilation of blood vessels entering the injured area
- Fluid that seeps from the capillary containing clotting factors and antibodies during inflammation
- Caused by excess fluid pressing on adjacent nerve endings
- The process by which white blood cells are attracted to the site of an injury
Fluid that seeps from the capillary containing clotting factors and antibodies during inflammation
Ex.
Exudate is fluid that seeps from the capillary containing clotting factors and antibodies during inflammation.
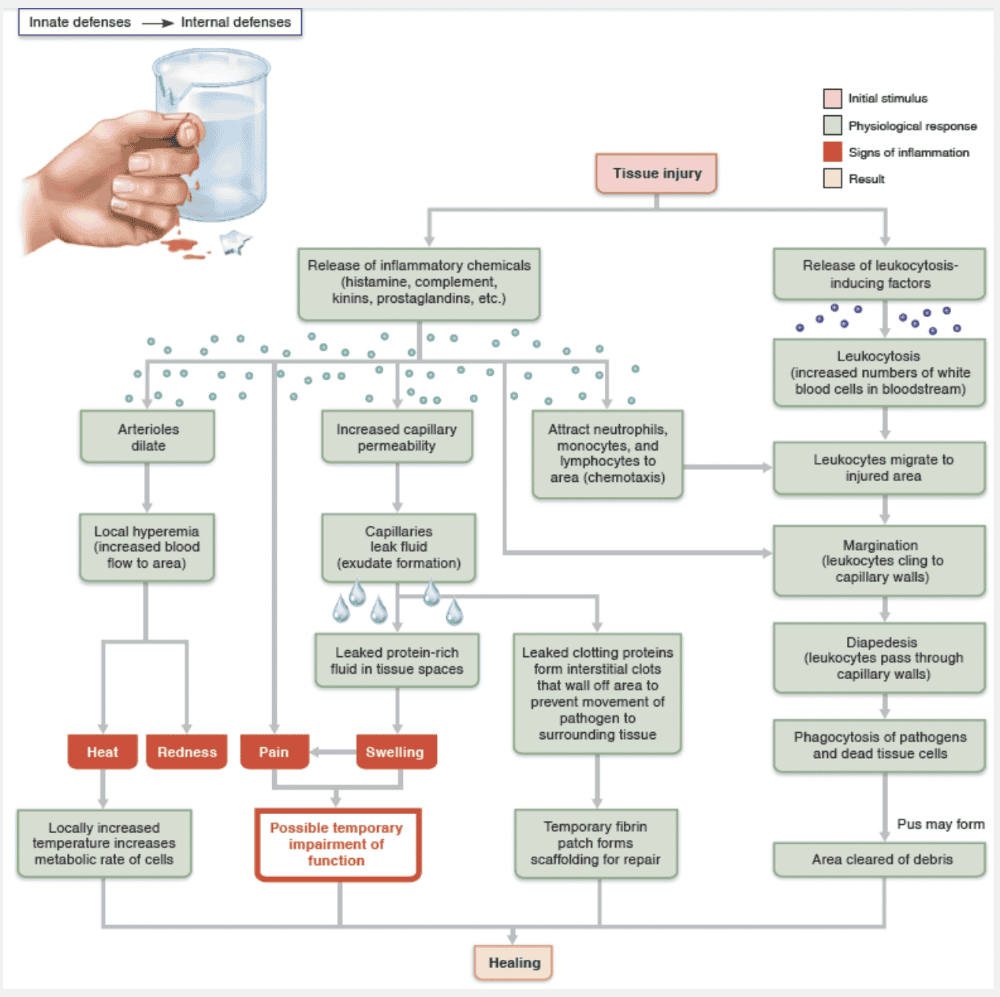
Inflammatory chemicals also increase the permeability of local capillaries. Consequently, exudate—fluid containing clotting factors and antibodies—seeps from the blood into the tissue spaces. This exudate causes the local swelling (edema) that presses on adjacent nerve endings, contributing to a sensation of pain. Pain also results from the release of bacterial toxins, and the sensitizing effects of released prostaglandins and kinins. Aspirin and some other anti-inflammatory drugs reduce pain by inhibiting prostaglandin synthesis.
Match the following term with its correct description: Leukocytosis.
- White blood cells migrate to the site of tissue damage
- Phagocytes squeeze through the capillary endothelium
- An increase in the number of white blood cells that are in circulation
- Clinging of phagocytic cells to the inner walls of the capillaries
An increase in the number of white blood cells that are in circulation
Ex.
Leukocytosis is an increase in the number of white blood cells that are in circulation.
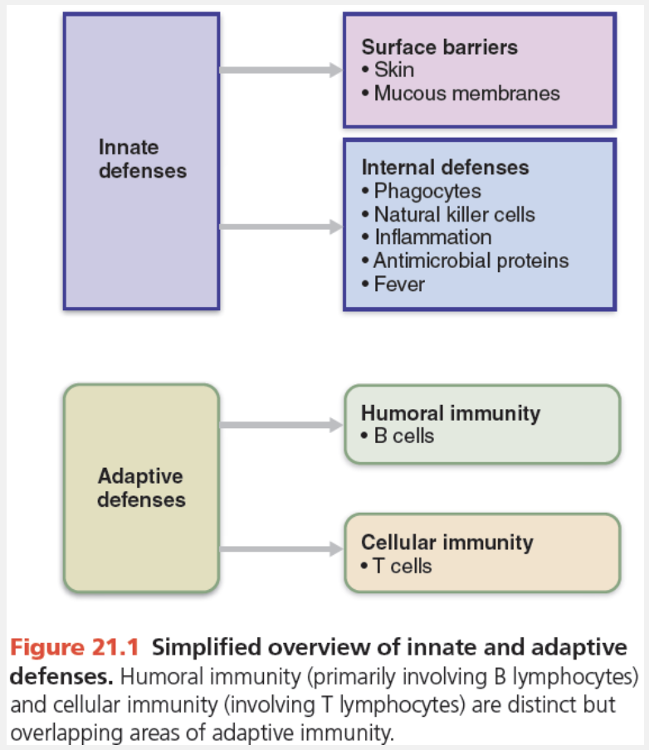
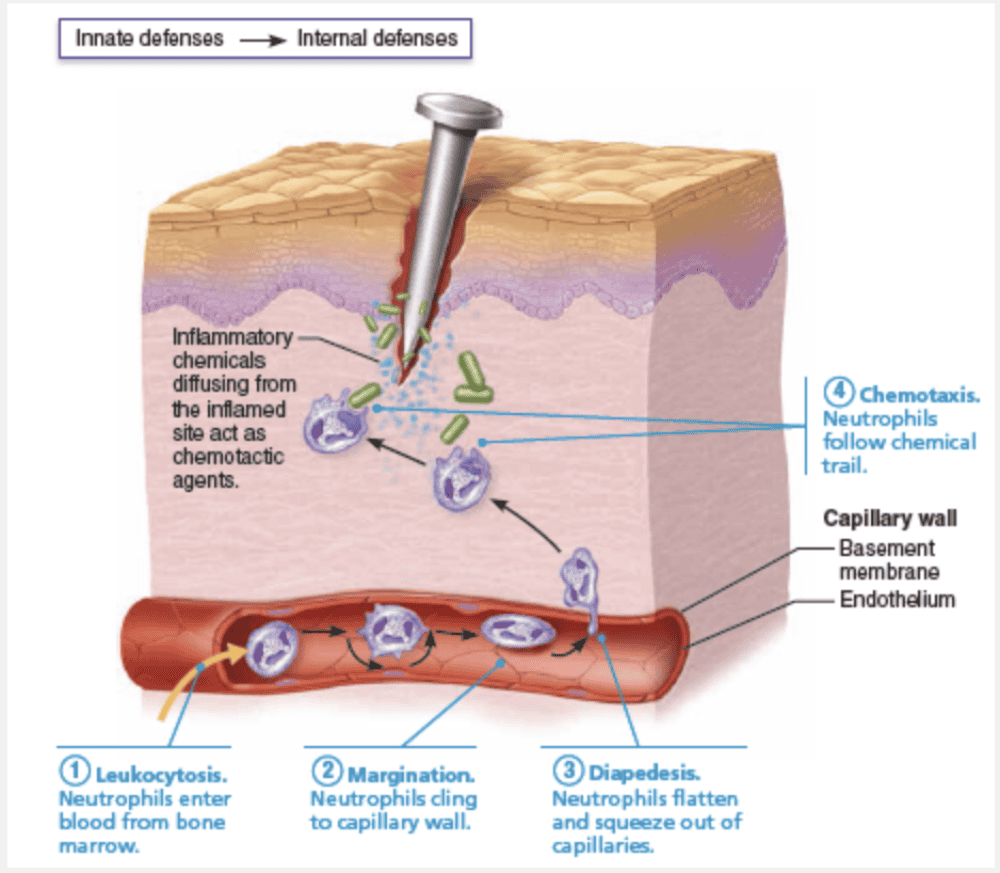
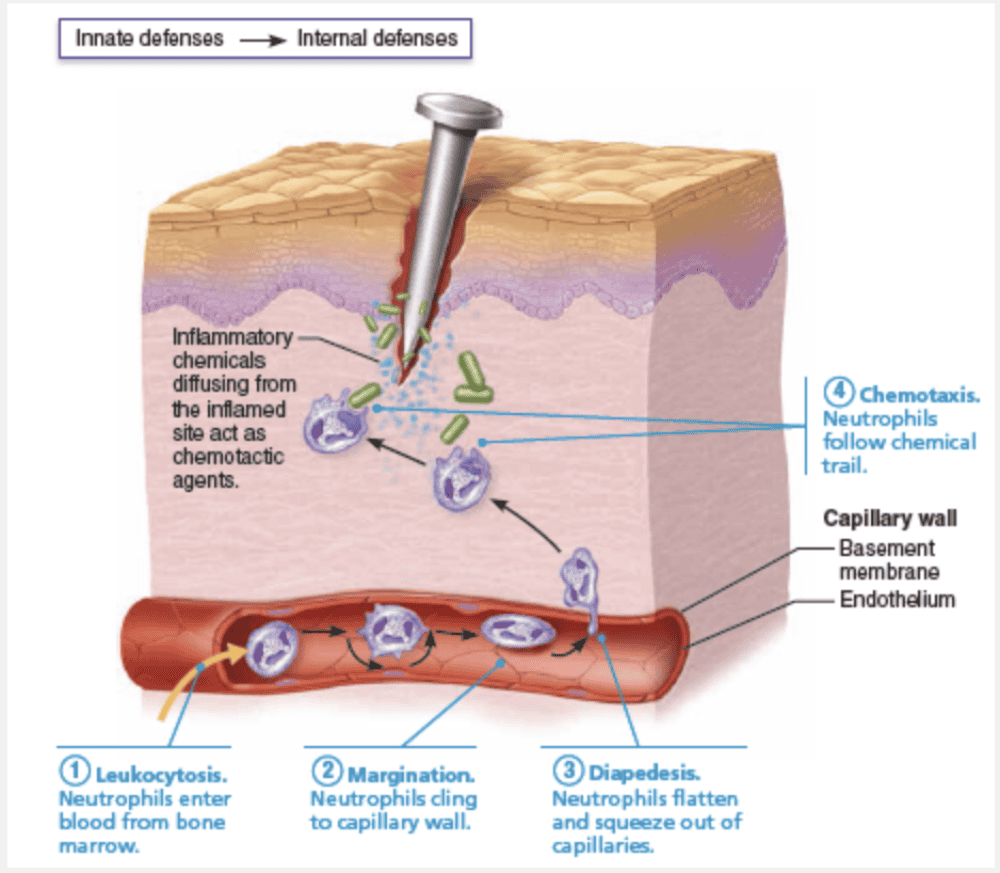
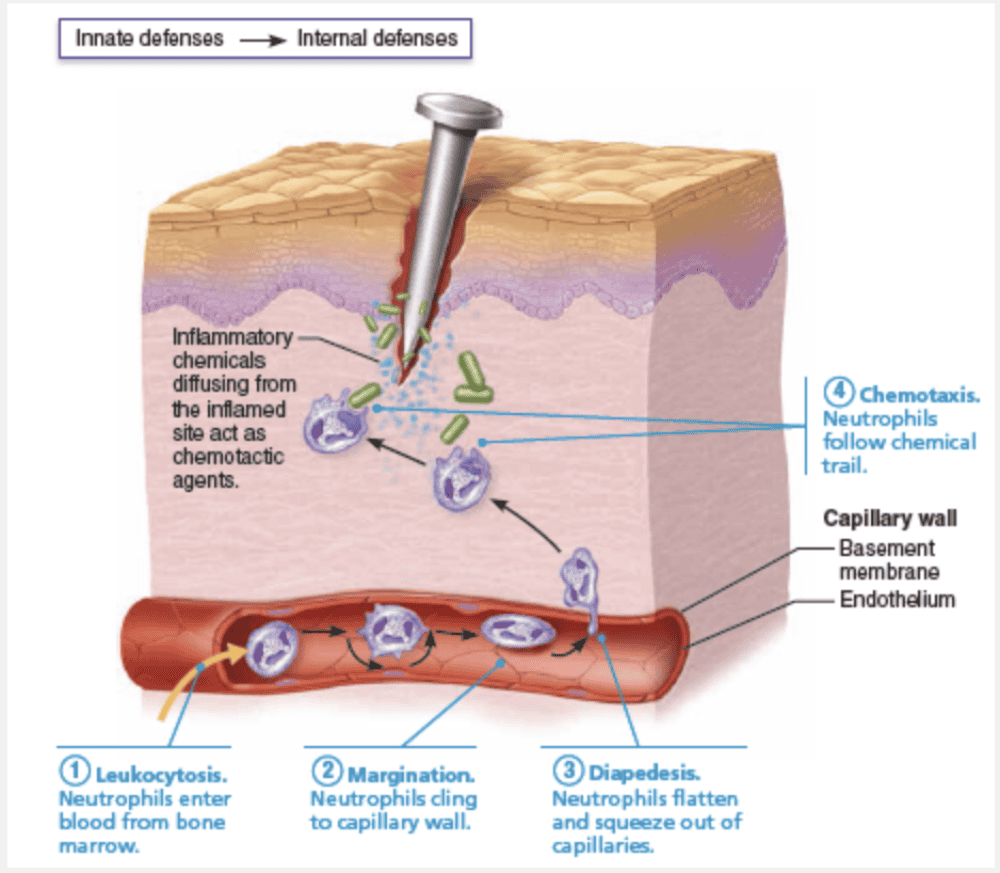
Leukocytosis. Injured cells release chemicals called leukocytosis-inducing factors. In response, neutrophils enter blood from red bone marrow and within a few hours, the number of neutrophils in blood increases four- to fivefold. This leukocytosis, the increase in white blood cells (WBCs), is characteristic of inflammation.
What fever inducing molecules are secreted by leukocytes and macrophages?
- Keratin
- Heparin
- Pyrogens
- Histamine
- Antibodies
Pyrogens
Ex.
Pyrogens are the molecules that are secreted by leukocytes and macrophages and result in a fever.
Inflammation is a localized response to infection, but sometimes the body’s response to the invasion of microorganisms is more widespread. Fever, an abnormally high body temperature, is a systemic response to invading microorganisms.
When leukocytes and macrophages are exposed to foreign substances in the body, they release chemicals called pyrogens (pyro = fire). These pyrogens act on the body’s thermostat—a cluster of neurons in the hypothalamus—raising the body’s temperature above normal [37°C (98.6°F)].
Fever is an adaptive response that seems to benefit the body, but exactly how it does so is unclear. Fever causes the liver and spleen to sequester iron and zinc, which may make them less available to support bacterial growth. Additionally, fever increases the metabolic rate of tissue cells, and may speed up repair processes.
Antibodies are secreted by plasma cells, while histamine and heparin are secreted by mast cells.
Keratin is a protein found in the skin.
All of the following describes interferons except that _____________.
- they can be released by lymphocytes to cause widespread immune mobilization.
- they are virus-specific
- they interfere with viral replication in cells neighboring an infected cell
- they mobilize natural killer cells
they are virus-specific
Ex.
Interferons are NOT virus-specific.
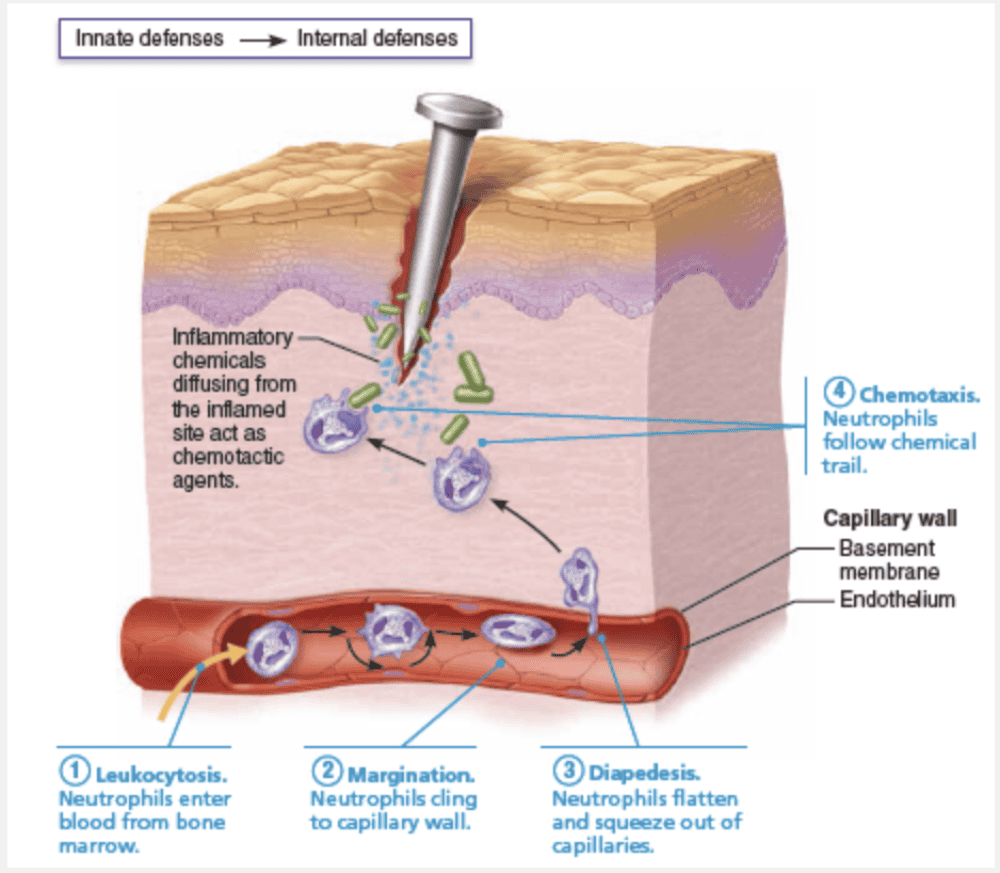
Viruses—essentially nucleic acids surrounded by a protein envelope—lack the cellular machinery to generate ATP or synthesize proteins. They do their “dirty work” in the body by invading tissue cells and taking over the cellular metabolic machinery needed to reproduce themselves.
Infected cells can do little to save themselves, but some can secrete small proteins called interferons (IFNs) (in”terfēr’ onz) to help protect cells that have not yet been infected. The IFNs diffuse to nearby cells, which they stimulate to synthesize proteins that “interfere” with viral replication in still-healthy cells by blocking protein synthesis and degrading viral RNA. Because IFN protection is not virus-specific, IFNs produced against a particular virus protect against other viruses, too.
The IFNs are a family of immune modulating proteins produced by a variety of body cells, each having a slightly different physiological effect. IFN alpha (α) and beta (β) have the antiviral effects that we’ve just described and also activate natural killer (NK) cells. Another interferon, IFN gamma (γ), or immune interferon, is secreted by lymphocytes and has widespread immune mobilizing effects, such as activating macrophages. Because both macrophages and NK cells can also act directly against cancerous cells, the interferons have an indirect role in fighting cancer. Genetically engineered IFNs are used to treat several disorders including hepatitis C, genital warts, and multiple sclerosis.
Select the description of chemotaxis.
- The process by which white blood cells are attracted to the site of an injury
- Seeps from the capillaries and contains clotting factors and antibodies
- Increased blood flow due to vasodilation of blood vessels entering the injured area
- Caused by excess blood flow to the injured area; helps to dilute harmful substances and brings in excess oxygen
The process by which white blood cells are attracted to the site of an injury
Ex.
Chemotaxis is the process by which white blood cells are attracted to the site of an injury.
Inflammatory chemicals act as homing devices, or more precisely chemotactic agents. Neutrophils and other white blood cells (WBCs) migrate up the gradient of chemotactic agents to the site of injury. Within an hour after the inflammatory response has begun, neutrophils have collected at the site and are devouring any foreign material present.
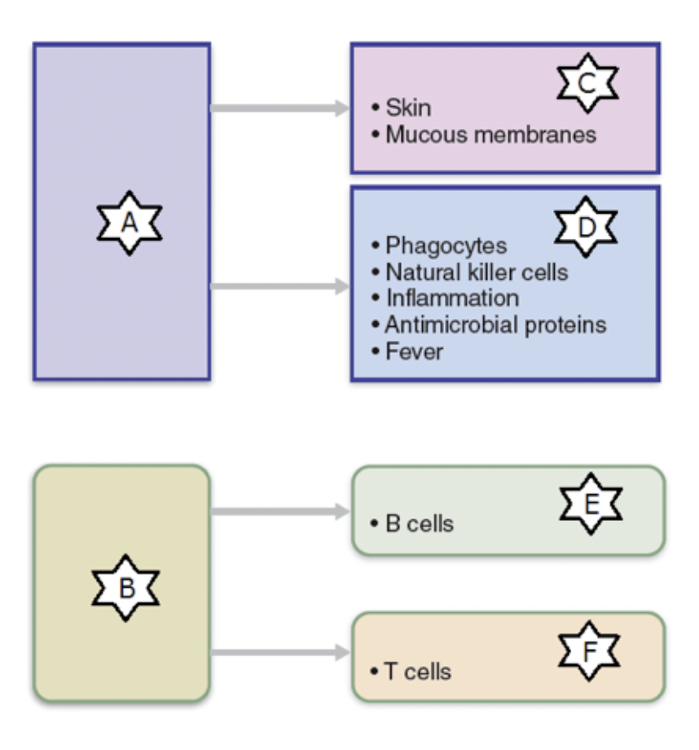
Identify the part of the immune system labelled as “A.”
- Humoral immunity
- Internal defenses
- Cellular immunity
- Surface barriers
- Innate defenses
- Adaptive defenses
Innate defenses
Select the enzyme in saliva and lacrimal fluids that destroys bacteria.
- Lysozyme
- Amylase
- Reverse transcriptase
- Pepsin
- Trypsin
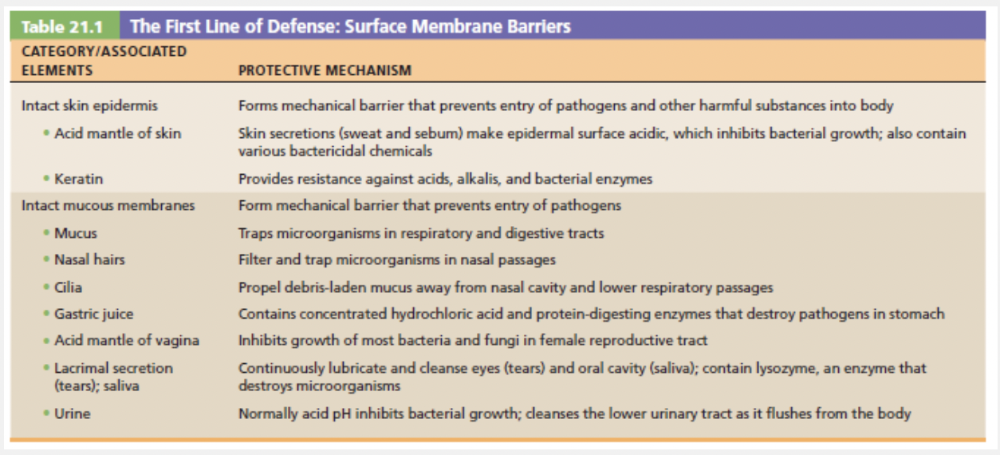
Lysozyme
Ex.
Lysozyme—found in saliva, respiratory mucus, and lacrimal fluid of the eye—destroys bacteria. Protein-digesting enzymes in the stomach kill many different microorganisms.
Amylase, trypsin, reverse trascriptase, and pepsin are enzymes with various functions, but are not found in lacrimal secretions, nor do they play a role in destroying bacteria as part of the innate responses.
Which of the following inflammatory processes attracts neutrophis to the injured area?
- Leukocytosis
- Diapedesis
- Margination
- Chemotaxis
Chemotaxis
Ex.
Chemotaxis is the process that attracts neutrophis to the injured area.
Neutrophils and other white blood cells (WBCs) migrate up the gradient of chemotactic agents to the site of injury. Within an hour after the inflammatory response has begun, neutrophils have collected at the site and are devouring any foreign material present.
Leukocytosis is an abnormally high number of leukocytes. Leukocytes in the vicinity of inflammation/injury will begin slowing down and marginating, and then cross the blood vessel wall by the process of diapedesis.
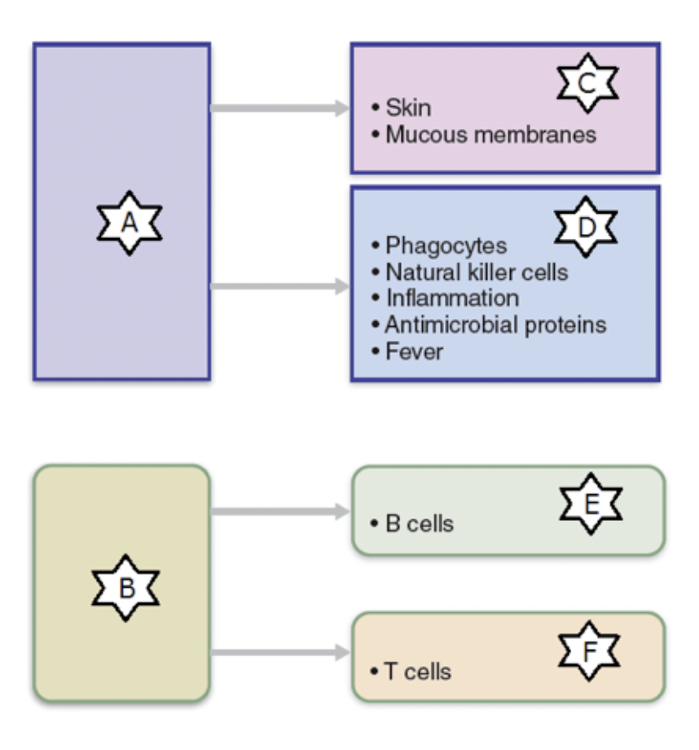
Identify the part of the immune system labelled as “F.”
- Innate defenses
- Humoral immunity
- Internal defenses
- Surface barriers
- Adaptive defenses
- Cellular immunity
Cellular immunity
Complement proteins work by __________.
- phagocytosis of target cells
- forming pores in the membranes of target cells
- creating an impermeable barrier
- neutralization of antigens
- producing antibodies
forming pores in the membranes of target cells
Ex.
Complement proteins work by forming pores in the membranes of target cells.
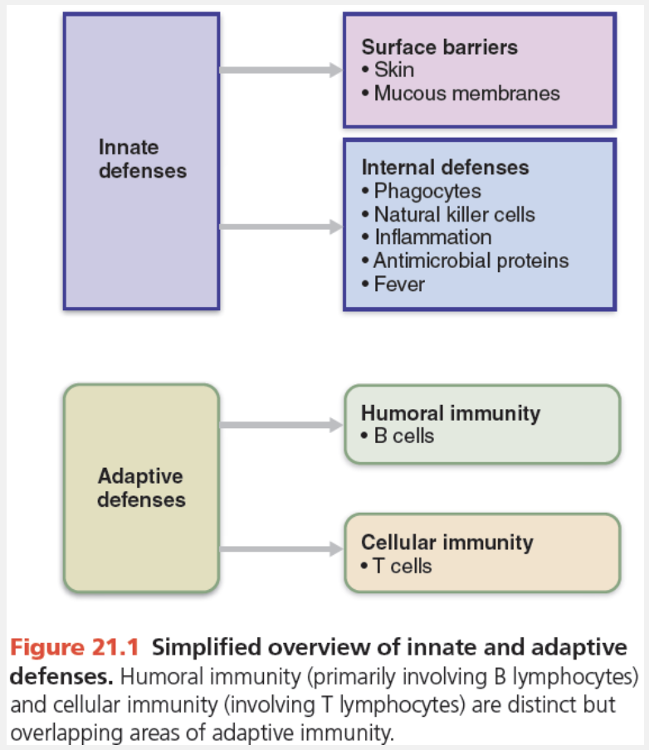
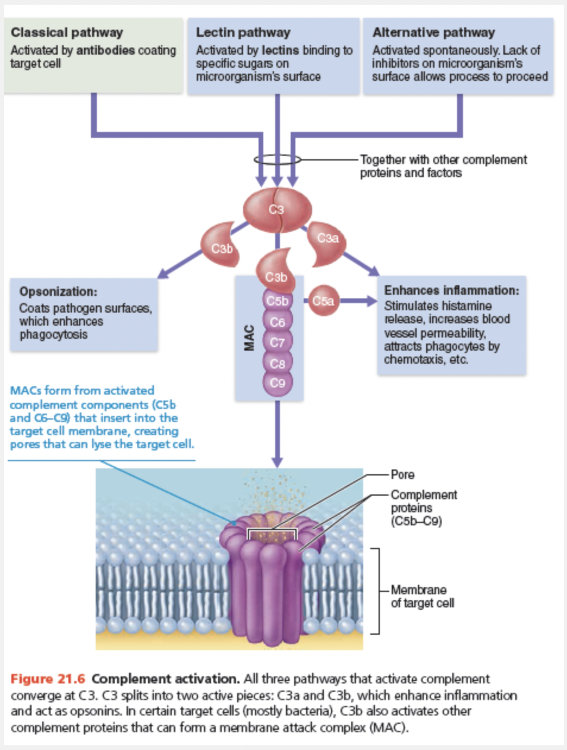
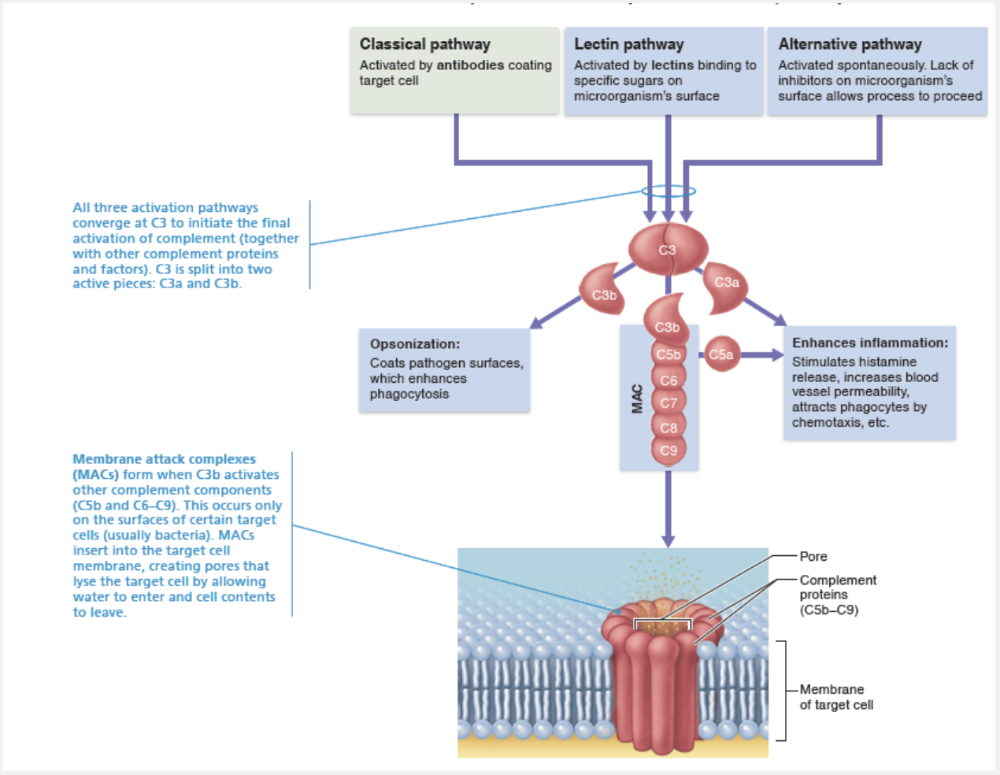
The term complement system, or simply complement, refers to a group of at least 20 plasma proteins that normally circulate in the blood in an inactive state. These proteins include C1 through C9, factors B, D, and P, plus several regulatory proteins.
Complement provides a major mechanism for destroying foreign substances in the body. Its activation unleashes inflammatory chemicals that amplify virtually all aspects of the inflammatory process. Activated complement also lyses and kills certain bacteria and other cell types. (Luckily our own cells are equipped with proteins that normally inhibit complement activation.) Although complement is a nonspecific defensive mechanism, it “complements” (enhances) the effectiveness of both innate and adaptive defenses.
The figure below outlines the three pathways by which complement can be activated:
- The classical pathway involves antibodies, water-soluble protein molecules that the adaptive immune system produces to fight off foreign invaders. When antibodies bind to pathogens, they can also bind complement components. This double binding, called complement fixation, is the first step in this complement activation pathway. (We describe this in more detail on pp. 790–791.)
- The lectin pathway involves lectins, water-soluble protein molecules that the innate immune system produces to recognize foreign invaders. When lectins bind specific sugars on the surface of microorganisms, they can then bind and activate complement.
- The alternative pathway is triggered when spontaneously activated C3 and other complement factors interact on the surface of microorganisms. These microorganisms lack the complement activation inhibitors our own cells have.
Like the blood clotting cascade, complement activation by any of these pathways involves a cascade in which proteins are activated in an orderly sequence—each step catalyzing the next. The three pathways converge at C3, which is split into C3a and C3b. Splitting C3 initiates a common terminal pathway that enhances inflammation, promotes phagocytosis, and can cause cell lysis.
Cell lysis begins when C3b binds to the target cell’s surface and triggers the insertion of a group of complement proteins called MAC (membrane attack complex) into the cell’s membrane. MAC forms and stabilizes a hole in the membrane that allows a massive influx of water, lysing the target cell.
The C3b molecules act as opsonins. As previously described, opsonins coat the microorganism, providing “handles” that receptors on macrophages and neutrophils can adhere to. This allows them to engulf the particle more rapidly. C3a and other cleavage products formed during complement fixation amplify the inflammatory response by stimulating mast cells and basophils to release histamine and by attracting neutrophils and other inflammatory cells to the area.
When collagen fibers are laid down to wall off a sac of pus, what structure is formed?
- Pustule
- An abscess
- Blisters
- Granulomas
An abscess
Ex.
Collagen fibers are laid down to wall off a sac of pus in the formation of an abscess.
In severely infected areas, the battle takes a considerable toll on both sides, and creamy yellow pus (a mixture of dead or dying neutrophils, broken-down tissue cells, and living and dead pathogens) may accumulate in the wound. If the inflammatory mechanism fails to clear the area of debris, collagen fibers may be laid down, which walls off the sac of pus, forming an abscess. The abscess may need to be surgically drained before healing can occur.
Which of the following defines opsonization?
- A process to increase the number of neutrophils
- A process of coating a pathogen to enhance phagocytosis.
- A process of releasing antibodies
- A process of coving the skin to limit bacterial growth
A process of coating a pathogen to enhance phagocytosis.
Ex.
Opsonization is a process of coating a pathogen to enhance phagocytosis.
Molecules released during complement activation tremendously amplify the inflammatory response and promote phagocytosis via opsonization. This sets into motion a positive feedback cycle that enlists more and more defensive elements.
When a localized area exhibits increased capillary filtration, hyperemia, and swelling, it is an indication that __________.
- an immune response is underway
- fever is developing
- antibodies are phagocytizing target cells
- inflammation is occurring
- antigens are present
inflammation is occurring
Ex.
When a localized area exhibits increased capillary filtration, hyperemia, and swelling, it is an indication that inflammation is occurring.
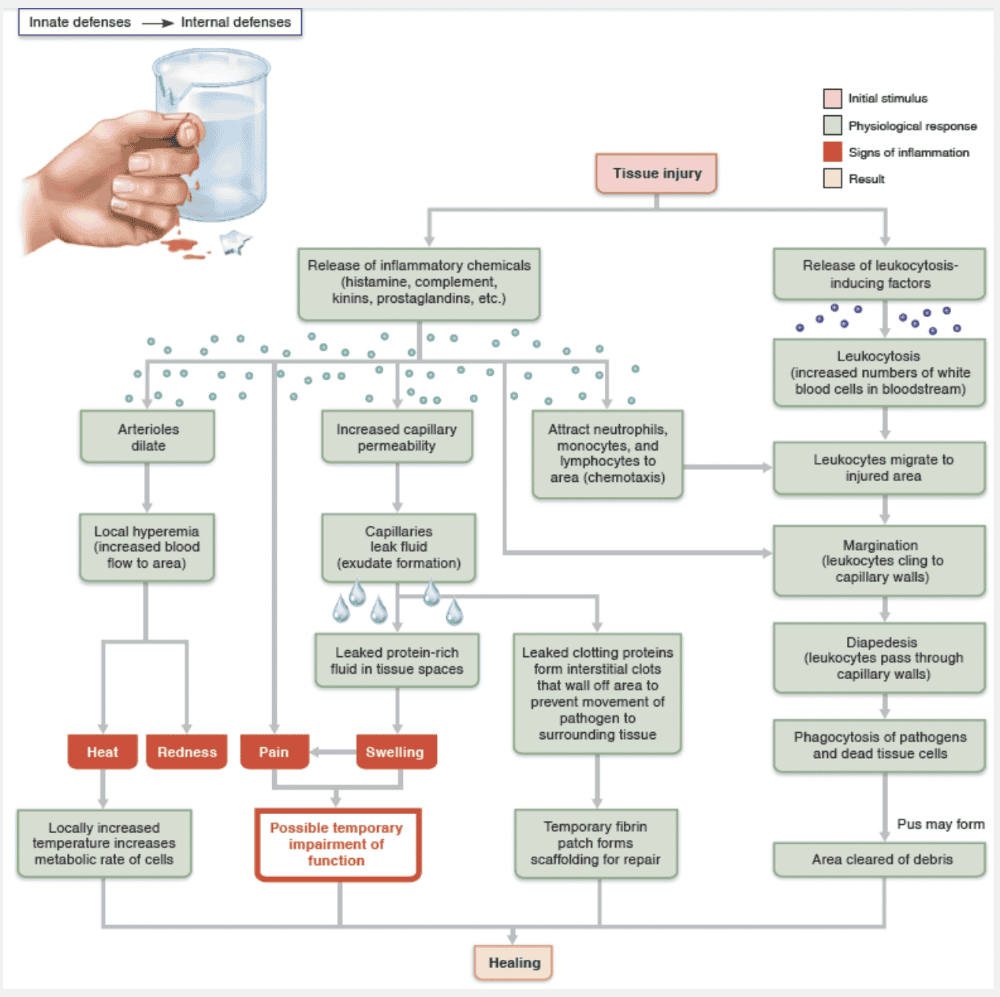
Inflammation is triggered whenever body tissues are injuredby physical trauma, intense heat, irritating chemicals, or infection by viruses, fungi, or bacteria. This inflammatory response to injury is summarized in the figure below. Inflammation has several beneficial effects:
- It prevents the spread of damaging agents to nearby tissues
- It disposes of cell debris and pathogens.
- It alerts the adaptive immune system.
- It sets the stage for repair.
The four cardinal signs of short-term, or acute, inflammation are redness, heat (inflam = set on fire), swelling, and pain. Some authorities consider impaired function to be a fifth cardinal sign. For instance, movement in an inflamed joint may be hampered temporarily, forcing it to rest, which aids healing.
Although antigens and antibodies may be present and an immune response may be occurring, an area that exhibits increased capillary filtration, hyperemia, and swelling, is a direct indication that inflammation is occurring.
Which nonspecific defense cells specialize in attacking cancer cells and virus-infected cells?
- Basophils
- Natural killer cells
- Helper T lymphocytes
- Plasma cells
- Macrophages
Natural killer cells
Ex.
Natural killer cells are defense cells that specialize in attacking cancer cells and virus-infected cells.
Natural killer (NK) cells, which “police” the body in blood and lymph, are a unique group of defensive cells that can lyse and kill cancer cells and virus-infected body cells before the adaptive immune system is activated. NK cells are part of a small group of large granular lymphocytes. Unlike lymphocytes of the adaptive immune system, which only recognize and react against specific virus-infected or tumor cells, NK cells are far less picky. They can eliminate a variety of infected or cancerous cells by detecting general abnormalities such as the lack of “self” cell-surface proteins called MHC. The name “natural” killer cells reflects their nonspecificity. NK cells are not phagocytic. They kill by directly contacting the target cell, inducing it to undergo apoptosis (programmed cell death). This is the same method used by cytotoxic T cells. NK cells also secrete potent chemicals that enhance the inflammatory response.
Basophils, helper T-cells, macrophages, and plasma cells do not directly attack and destroy cancer and virus-infected cells.
Identify the part of the immune system labelled as “E.”
- Innate defenses
- Humoral immunity
- Internal defenses
- Surface barriers
- Adaptive defenses
- Cellular immunity
Humoral immunity
Which of the following describes hyperemia?
- The process by which white blood cells are attracted to the site of an injury
- Caused by excess blood flow to the injured area; helps to dilute harmful substances and brings in excess oxygen
- Seeps from the capillaries and contains clotting factors and antibodies
- Increased blood flow due to vasodilation of blood vessels entering the injured area
Increased blood flow due to vasodilation of blood vessels entering the injured area
Ex.
Hyperemia is increased blood flow due to vasodilation of blood vessels entering the injured area.
Vasodilation accounts for two of the cardinal signs of inflammation. The redness and heat of an inflamed region are both due to local hyperemia (congestion with blood) that occurs when local arterioles dilate.
Excess blood flow to an area will cause local swelling, or edema. The fluid that seeps out of the blood vessels and contains clotting factors and antibodies, is called exudate. The white blood cells (leukocytes) that leave in exudate are attracted to the site of injury/inflammation by chemotaxis.
Which of the following describes edema?
- Caused by excess tissue fluid in the injured area; helps to dilute harmful substances and brings in excess oxygen
- The process by which white blood cells are attracted to the site of an injury
- Seeps from the capillaries and contains clotting factors and antibodies
- Increased blood flow due to vasodilation of blood vessels entering the injured area
Caused by excess tissue fluid in the injured area; helps to dilute harmful substances and brings in excess oxygen
Ex.
Edema is caused by excess blood flow to the injured area and helps to dilute harmful substances and brings in excess oxygen.
Inflammatory chemicals also increase the permeability of local capillaries. Consequently, exudate—fluid containing clotting factors and antibodies—seeps from the blood into the tissue spaces. This exudate causes the local swelling (edema) that presses on adjacent nerve endings, contributing to a sensation of pain. Pain also results from the release of bacterial toxins, and the sensitizing effects of released prostaglandins and kinins. Aspirin and some other anti-inflammatory drugs reduce pain by inhibiting prostaglandin synthesis.
Although edema may seem detrimental, it isn’t. The surge of protein-rich fluids into the tissue spaces sweeps foreign material into lymphatic vessels for processing in the lymph nodes. It also delivers important proteins such as complement and clotting factors to the interstitial fluid.
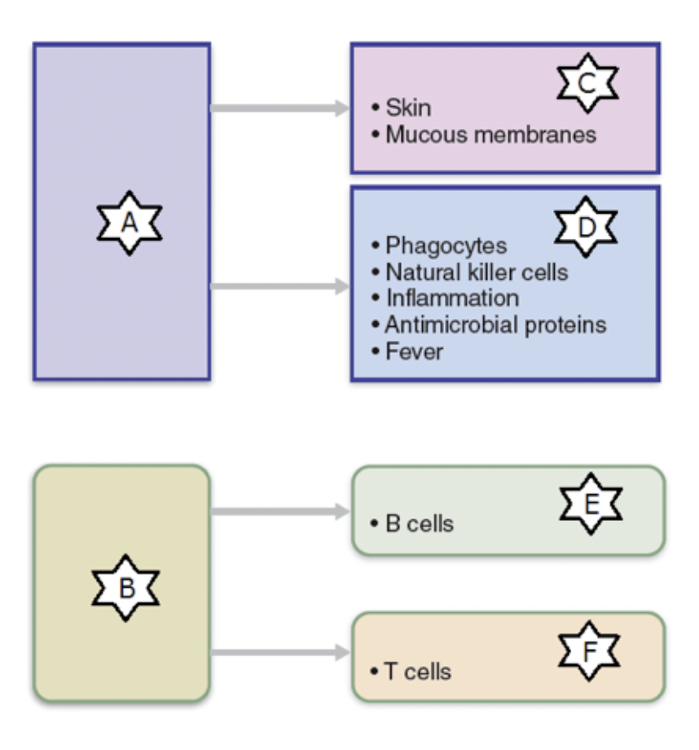
Identify the part of the immune system labelled as “D.”
- Adaptive defenses
- Cellular immunity
- Surface barriers
- Humoral immunity
- Innate defenses
- Internal defenses
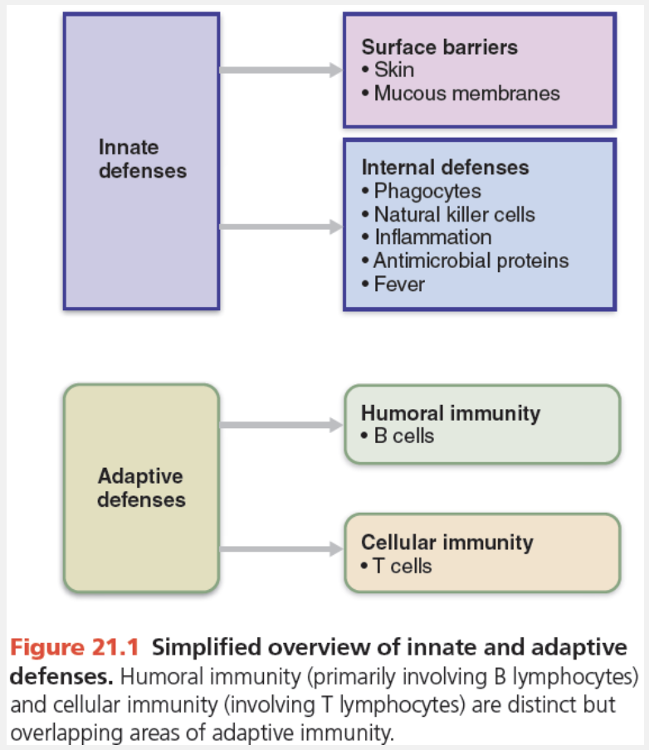
Internal defenses
Match the following cell of the immune system with its function: Neutrophils.
- Phagocytes; will migrate to the site of an infection within a few hours
- A small subgroup of lymphocytes that will attack cancerous cells
- Secrete antibodies
- Derived from circulating monocytes
Phagocytes; will migrate to the site of an infection within a few hours
Ex.
Neutrophils are phagocytes which will migrate to the site of an infection within a few hours.
Neutrophils, the most abundant type of white blood cell, become phagocytic on encountering infectious material in the tissues.
Neutrophils and other WBCs migrate up the gradient of chemotactic agents to the site of injury. Within an hour after the inflammatory response has begun, neutrophils have collected at the site and are devouring any foreign material present.
Macrophages are leukocytes derived from circulating monocytes.
Natural killer (NK) cells, part of the innate response, attack cancerous cells.
Plasma cells, derived from B lymphocytes, secrete antibodies.
Which of the following is not a surface barrier to pathogen influx?
- Mucous membranes
- Skin secretions
- Complement cascade
- Saliva and tears
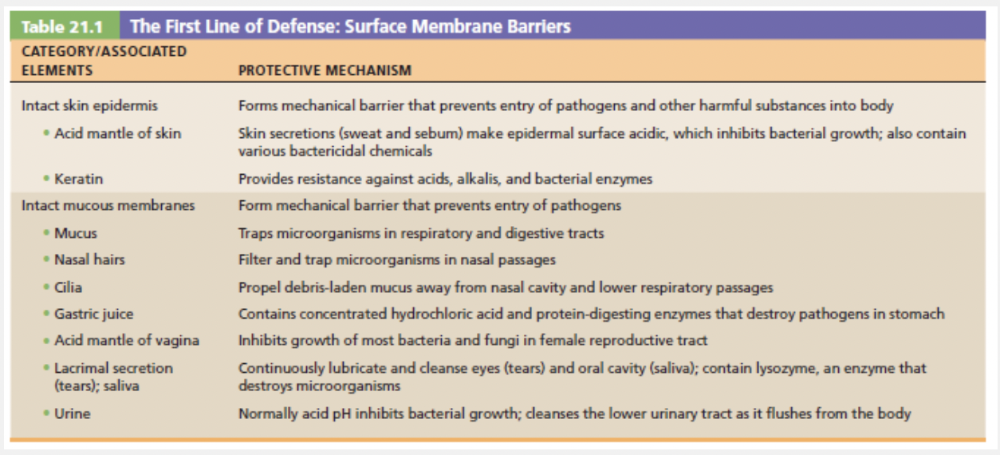
Complement cascade
Ex.
Complement cascade is not a surface barrier to pathogen influx.
As show in the table below, skin secretions, mucous membranes, and saliva/tears all contribute to surface membrane barriers while the complement cascade does not.
A person may harbor pathogens walled off in __________ for years without displaying any symptoms.
- an abscess
- granulomas
- pus
- blisters
granulomas
Ex.
A person may harbor pathogens walled off in granulomas for years without displaying any symptoms.
Some bacteria, such as tuberculosis bacilli, resist digestion by the macrophages that engulf them. They escape the effects of prescription antibiotics by remaining snugly enclosed within their macrophage hosts. In such cases, granulomas form. These tumorlike growths contain a central region of infected macrophages surrounded by uninfected macrophages and an outer fibrous capsule.
A person may harbor pathogens walled off in granulomas for years without displaying any symptoms. However, if the person’s resistance to infection is ever compromised, the bacteria may be activated and break free, leading to clinical disease symptoms.
Select the process in which neutrophils squeeze through walls of capillaries into the tissues.
- Chemotaxis
- Leukocytosis
- Diapedesis
- Margination
Diapedesis
Ex.
Diapedesis is the process whereby neutrophils squeeze through walls of capillaries into the tissues.
Soon after inflammation begins, phagocytes flood the damaged area. Neutrophils lead, followed by macrophages. If pathogens provoked the inflammation, a group of plasma proteins known as complement is activated and elements of adaptive immunity (lymphocytes and antibodies) also arrive at the injured site. The figure below illustrates the four steps in which phagocytes are mobilized to infiltrate the injured site.
- Leukocytosis. Injured cells release chemicals called leukocytosis-inducing factors. In response, neutrophils enter blood from red bone marrow and within a few hours, the number of neutrophils in blood increases four- to fivefold. This leukocytosis, the increase in white blood cells (WBCs), is characteristic of inflammation.
- Margination. Inflamed endothelial cells sprout cell adhesion molecules (CAMs) that signal “this is the place.” As neutrophils encounter these CAMs, they slow and roll along the surface, eventually achieving an initial foothold. When activated by inflammatory chemicals, CAMs on neutrophils bind tightly to endothelial cells. Margination refers to this phenomenon of phagocytes clinging to the inner walls (margins) of the capillaries and postcapillary venules.
- Diapedesis. Continued chemical signaling prompts the neutrophils to flatten and squeeze between the endothelial cells of the capillary walls—a process called diapedesis.
- Chemotaxis. Inflammatory chemicals act as homing devices, or more precisely chemotactic agents. Neutrophils and other WBCs migrate up the gradient of chemotactic agents to the site of injury. Within an hour after the inflammatory response has begun, neutrophils have collected at the site and are devouring any foreign material present.
Which of the following is not one of the cardinal signs of inflammation?
- Heat
- Redness
- Pain
- Swelling
- Opsonization
Opsonization
Ex.
Opsonization is not a cardinal signs of inflammation.
The four cardinal signs of short-term, or acute, inflammation are redness, heat (inflam = set on fire), swelling, and pain. Some authorities consider impaired function to be a fifth cardinal sign. For instance, movement in an inflamed joint may be hampered temporarily, forcing it to rest, which aids healing.
Opsonization is the process of coating a pathogen with antibodies to aid in clearing it from the body.
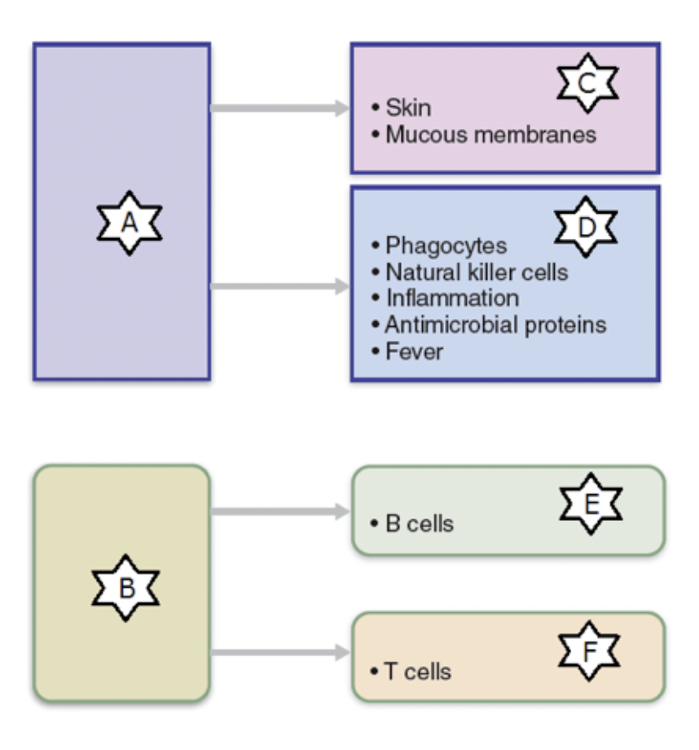
Identify the part of the immune system labelled as “B.”
- Innate defenses
- Cellular immunity
- Surface barriers
- Internal defenses
- Humoral immunity
- Adaptive defenses
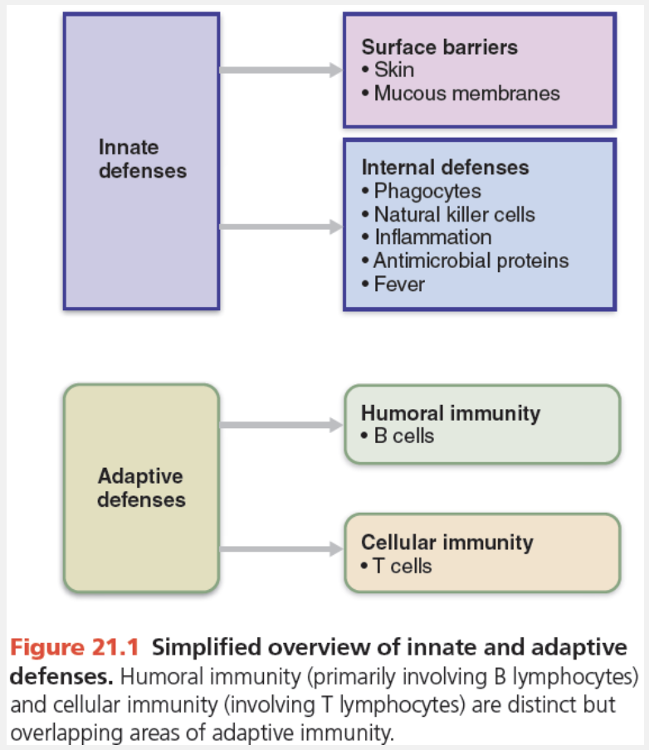
Adaptive defenses
Which of the following minerals needed for bacterial reproduction do both the liver and spleen sequester during a fever?
- Tin and aluminum
- Iron and zinc
- Sodium and potassium
- Selenium and cobalt
Iron and zinc
Ex.
Iron and zinc are minerals needed for bacterial reproduction that both the liver and spleen sequester during a fever.
Fever is an adaptive response that seems to benefit the body, but exactly how it does so is unclear. Fever causes the liver and spleen to sequester iron and zinc, which may make them less available to support bacterial growth. Additionally, fever increases the metabolic rate of tissue cells, and may speed up repair processes.
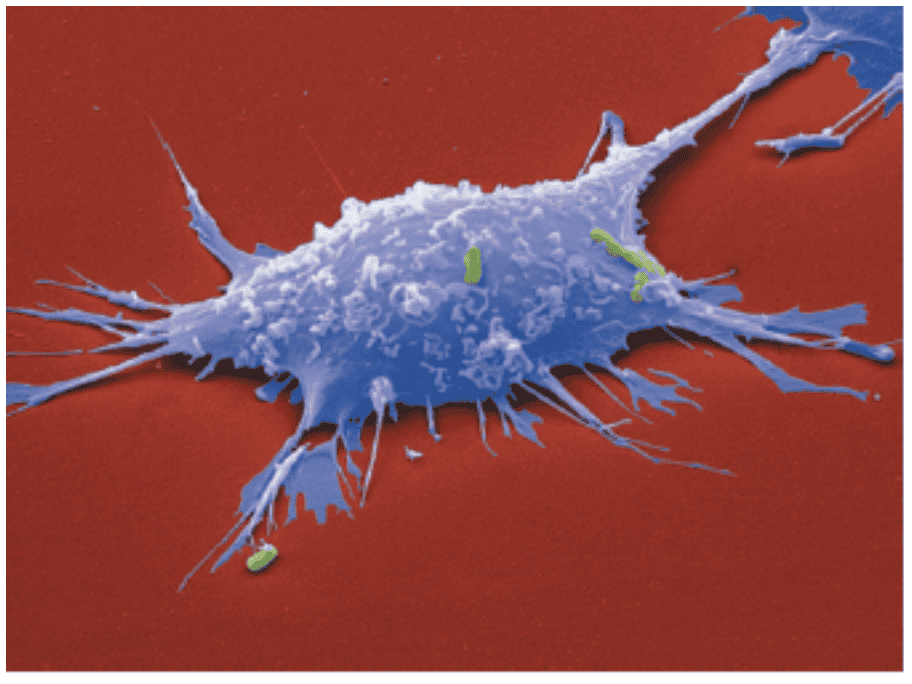
Identify the cell shown.
- Lymphocyte
- Natural killer cell
- Basophil
- Macrophage
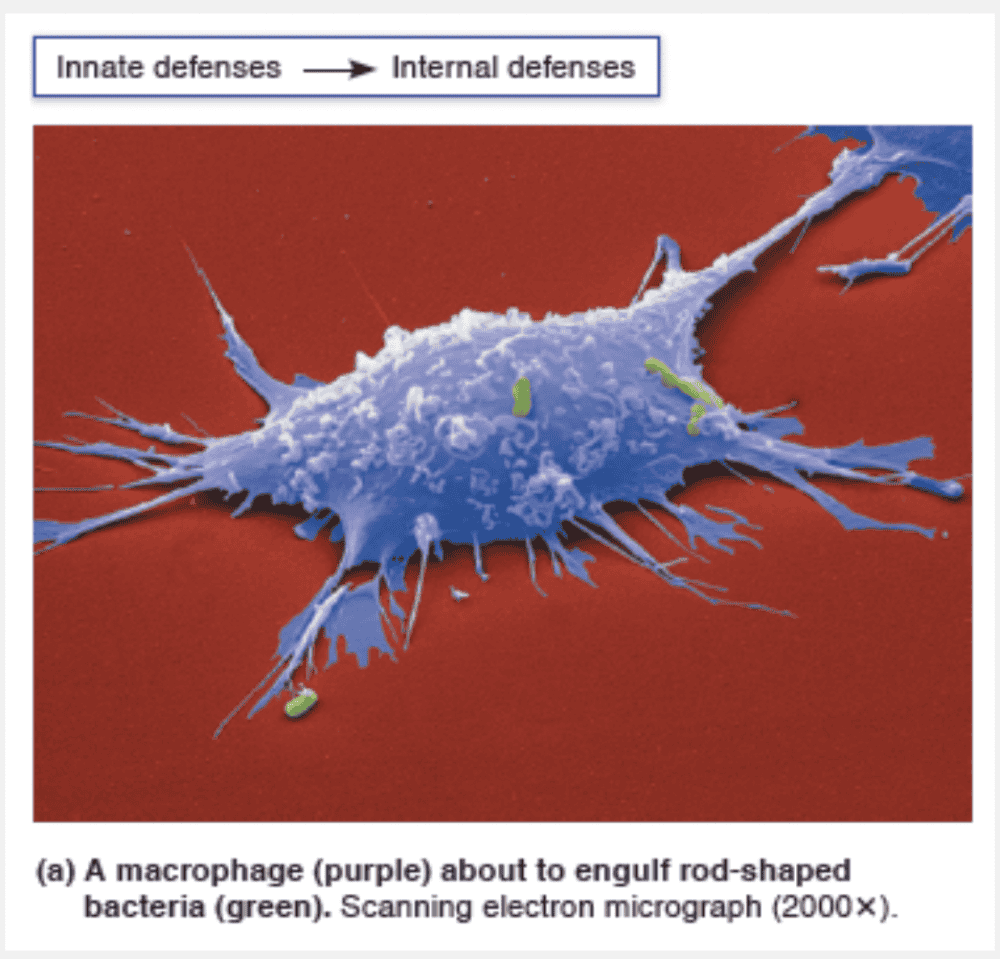
Macrophage
Ex.
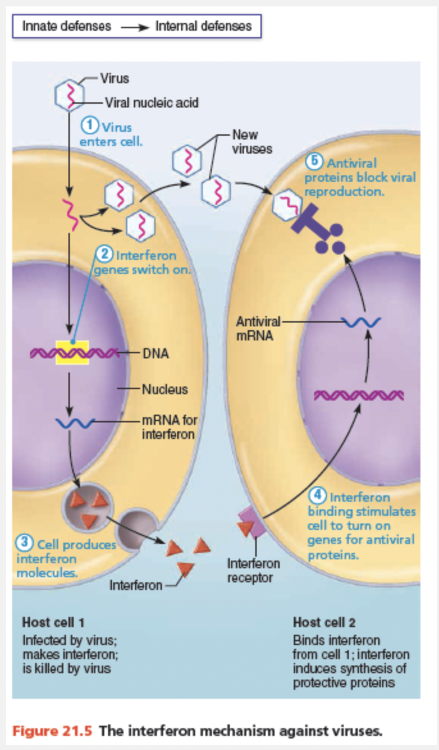
The most voracious phagocytes are macrophages (“big eaters”), which derive from white blood cells called monocytes that leave the bloodstream, enter the tissues, and develop into macrophages.
Match the following cell of the immune system with its function: Macrophages.
- Secrete antibodies
- Derived from circulating monocytes
- A small subgroup of lymphocytes that will attack cancerous cells
- First cell type to arrive at a site of injury
Derived from circulating monocytes
Ex.
Macrophages are derived from circulating monocytes.
The most voracious phagocytes are macrophages (“big eaters”), which derive from white blood cells called monocytes that leave the bloodstream, enter the tissues, and develop into macrophages.
Free macrophages wander throughout the tissue spaces in search of cellular debris or “foreign invaders.” Fixed macrophages, like stellate macrophages in the liver, are permanent residents of particular organs.
Neutrophils are the ‘first responders’ at sites of injury.
Nautral killer (NK) cells attack cancerous cells.
Plasma cells secrete antibodies.
Which of the following is a nonspecific barrier defense?
- Natural killer cells
- Mucous membranes
- Complements
- Antibodies
- Macrophages
Mucous membranes
Ex.
The mucous membranes are nonspecific barrier defenses.
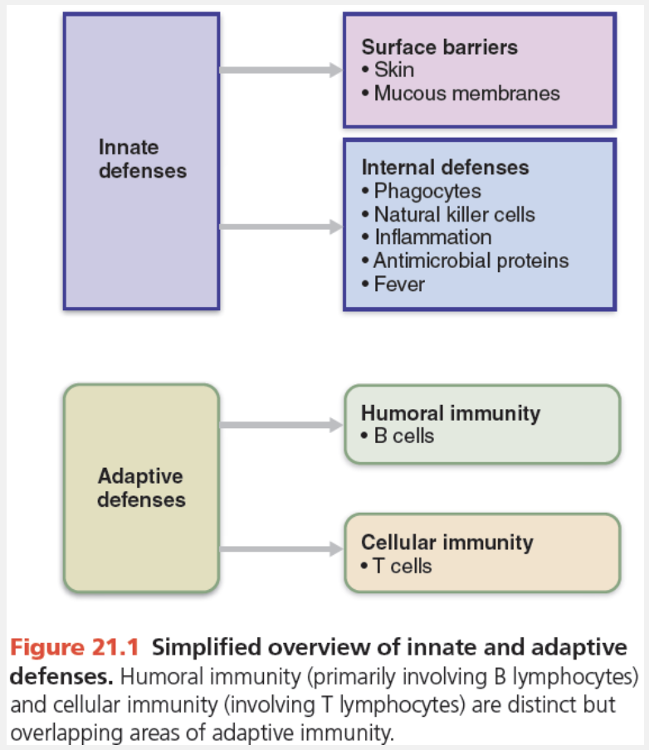
The innate (nonspecific) defense system, like a lowly foot soldier, is always prepared, responding within minutes to protect the body from foreign substances. This system has two “barricades.” The first line of defense is the external body membranes—intact skin and mucosae. The second line of defense, called into action whenever the first line has been penetrated, relies on internal defenses such as antimicrobial proteins, phagocytes, and other cells to inhibit the invaders’ spread throughout the body. The hallmark of the second line of defense is inflammation.
Match the defense cell with the correct characteristic: Macrophages.
- A common antigen presenting cell (APC)
- Invoke inflammation when IgE cross-links to them
- Coordinate humoral and cellular immune responses
- Produce immunoglobulins
A common antigen presenting cell (APC)
Ex.
Macrophages are common antigen-presenting cells (APCs).
Antigen-presenting cells (APCs) engulf antigens and then present fragments of them, like signal flags, on their own surfaces where T cells can recognize them. Naive T cells can only be activated by antigens that are presented to them on MHC proteins by APCs. In other words, APCs present antigens to the cells that will deal with the antigens. The major types of cells acting as APCs are dendritic cells, macrophages, and B lymphocytes.
Macrophages are widely distributed throughout the lymphoid organs and connective tissues. Although macrophages, like dendritic cells, can activate naive T cells, macrophages often present antigens to T cells for another reason—to be activated themselves. Certain effector T cells release chemicals that prod macrophages to become activated macrophages. Activated macrophages are true “killers”—insatiable phagocytes that also trigger powerful inflammatory responses and recruit additional defenses.
Many lymphocytes coordinate both humoral and cellular adaptive immune responses. B lymphocytes differentiate into plasma cells, which secrete immunoglobulins (antibodies).
Mast cells bind IgE produced by plasma cells in response to allergens, and cause inflammation when the IgE on the surface of the cell is cross-linked by an allergen.