A nurse assesses several clients who have a history of respiratory disorders. Which client would the nurse assess first?
A. A 66-year-old client with a barrel chest and clubbed fingernails
B. A 48-year-old client with an oxygen saturation level of 92% at rest
C. A 35-year-old client who reports orthopnea in bed
D. A 27-year-old client with a heart rate of 120 beats/min
D
Tachycardia can indicate hypoxemia as the body tries to circulate the oxygen that is available. A barrel chest is not an emergency finding. Likewise, a pulse oximetry level of 92% is not considered an acute finding. Orthopnea at night in bed is breathlessness when lying down but is not an acute finding at this moment.
A nurse cares for a client with arthritis who reports frequent asthma attacks. What action would the nurse take first?
A. Review the client’s pulmonary function test results.
B. Ask about medications the client is currently taking.
C. Assess how frequently the client uses a bronchodilator.
D. Consult the primary health care provider and request arterial blood gases.
B
Aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs) can trigger asthma in some people. This results from increased production of leukotriene when aspirin or NSAIDs suppress other inflammatory pathways and is a likely culprit given the client’s history. Reviewing pulmonary function test results will not address the immediate problem of frequent asthma attacks. This is a good time to review response to bronchodilators, but assessing triggers is more important. Questioning the client about the use of bronchodilators will address interventions for the attacks but not their cause. Reviewing arterial blood gas results would not be of use in a client between attacks because many clients are asymptomatic when not having attacks.
After teaching a client who is prescribed a long-acting beta2 agonist medication, a nurse assesses the client’s understanding. Which statement indicates that the client comprehends the teaching?
A. “I will carry this medication with me at all times in case I need it.”
B. “I will take this medication when I start to experience an asthma attack.”
C. “I will take this medication every morning to help prevent an acute attack.”
D. “I will be weaned off this medication when I no longer need it.”
C
Long-acting beta2 agonist medications will help prevent an acute asthma attack because they are long acting. The client will take this medication every day for best effect. The client does not have to always keep this medication with him or her because it is not used as a rescue medication. This is not the medication the client will use during an acute asthma attack because it does not have an immediate onset of action. The client will not be weaned off this medication because this is likely to be one of his or her daily medications.
After teaching a client how to perform diaphragmatic breathing, the nurse assesses the client’s understanding. Which action demonstrates that the client correctly understands the teaching?
A. The client lies on his or her side with knees bent.
B. The client places his or her hands on the abdomen.
C. The client lies in a prone position with straight.
D. The client places his or her hands above the head.
B
To perform diaphragmatic breathing correctly, the client would place his or her hands on the abdomen to create resistance. This type of breathing cannot be performed effectively while lying on the side or with hands over the head. This type of breathing would not be as effective lying prone.
A nurse cares for a client who has developed esophagitis after undergoing radiation therapy for lung cancer. Which diet selection would the nurse provide for this client?
A. Spaghetti with meat sauce, ice cream
B. Chicken soup, grilled cheese sandwich
C. Omelet, soft whole-wheat bread
D. Pasta salad, custard, orange juice
C
Side effects of radiation therapy may include inflammation of the esophagus. Clients would be taught that bland, soft, high-calorie foods are best, along with liquid nutritional supplements. Tomato sauce may prove too spicy for a client with esophagitis. A grilled cheese sandwich is too difficult to swallow with this condition, and orange juice and other foods with citric acid are too caustic.
After teaching a client who is prescribed salmeterol, the nurse assesses the client’s understanding. Which statement by the client indicates a need for additional teaching?
A. “I will be certain to shake the inhaler well before I use it.”
B. “It may take a while before I notice a change in my asthma.”
C. “I will use the drug when I have an asthma attack.”
D. “I will be careful not to let the drug escape out of my nose and mouth.”
C
Salmeterol is a long-acting beta2 agonist designed to prevent an asthma attack; it does not relieve or reverse symptoms. Salmeterol has a slow onset of action; therefore, it would not be used as a rescue drug. The drug must be shaken well because it has a tendency to separate easily. Poor technique on the client’s part allows the drug to escape through the nose and mouth.
A nurse cares for a client with chronic obstructive pulmonary disease (COPD). The client states that going out with friends is no longer enjoyable. How would the nurse respond?
A. There are a variety of support groups for people who have COPD.
B. “I will ask your primary health care provider to prescribe an antianxiety agent.”
C. “I’d like to hear about thoughts and feelings causing you to limit social activities.”
D. “Friends can be a good support system for clients with chronic disorders.”
C
Many clients with moderate to severe COPD become socially isolated because they are embarrassed by frequent coughing and mucus production. They also can experience fatigue, which limits their activities. The nurse needs to encourage the client to verbalize thoughts and feelings so that appropriate interventions can be selected. Joining a support group would not decrease feelings of social isolation if the client does not verbalize feelings. Antianxiety agents will not help the client with social isolation. While friends can be good sources of support, the client specifically is discussing going out of the home.
A nurse is teaching a client who has cystic fibrosis (CF). Which statement would the nurse include in this client’s teaching?
A. “Take an antibiotic each day.”
B. “You should get genetic screening.”
C. “Eat a well-balanced, nutritious diet.”
D. “Plan to exercise for 30 minutes every day.”
C
Clients with CF often are malnourished due to vitamin deficiency and pancreatic malfunction. Maintaining nutrition is essential. Daily antibiotics and daily exercise are not essential actions. Genetic screening might be an option; however, the nurse would not just tell the client to do something like that.
While assessing a client who is 12 hours postoperative after a thoracotomy for lung cancer, a nurse notices that the chest tube is dislodged. Which action by the nurse is best?
A. Assess for drainage from the site.
B. Cover the insertion site with sterile gauze.
C. Contact the primary health care provider.
D. Reinsert the tube using sterile technique.
B
Immediately covering the insertion site helps prevent air from entering the pleural space and causing a pneumothorax. The area will not reseal quickly enough to prevent air from entering the chest. The nurse would not leave the client to obtain a suture kit. An occlusive dressing may cause a tension pneumothorax. The nurse does not need to assess the site at this moment. The primary health care provider would be called to reinsert the chest tube or prescribe other treatment options.
A nurse assesses a client who is prescribed fluticasone and notes oral lesions. What action would the nurse take?
A. Encourage oral rinsing after fluticasone administration.
B. Obtain an oral specimen for culture and sensitivity.
C. Start the client on a broad-spectrum antibiotic.
D. Document the finding as a known side effect.
A
The drug reduces local immunity and increases the risk for local infection, especially Candida albicans. Rinsing the mouth after using the inhaler will decrease the risk for developing this infection. Use of mouthwash and broad-spectrum antibiotics is not warranted in this situation. The nurse would document the finding, but the best action to take is to have the client start rinsing his or her mouth after using fluticasone. An oral specimen for culture and sensitivity is not necessary to care for this client.
A nurse cares for a client who had a chest tube placed 6 hours ago and refuses to take deep breaths because of the pain. What action would the nurse take?
A. Ambulate the client in the hallway to promote deep breathing.
B. Auscultate the client’s anterior and posterior lung fields.
C. Encourage the client to take shallow breaths to help with the pain.
D. Administer pain medication and encourage the client to take deep breaths.
D
A chest tube is placed in the pleural space and may be uncomfortable for a client. The nurse would provide pain medication to minimize discomfort and encourage the client to take deep breaths. The other responses do not address the client’s discomfort and need to take deep breaths to prevent complications.
The nurse is caring for a client who has cystic fibrosis (CF). The client asks for information about gene therapy. What response by the nurse is best?
A. “Unfortunately, gene therapy is only provided to children upon diagnosis.”
B. “Do you know that you will have to have genetic testing?”
C. “There is a good treatment for the most common genetic defect in CF.”
D. “Gene therapy will only help improve your pulmonary symptoms.”
C
The drug ivacaftor/lumacaftor is effective as therapy for patients whose CF is caused by the F508del (also known as the Phe508del) mutation, the most common mutation involved in CF, even in patients who are homozygous for the mutation with both alleles being affected. The nurse would provide that information as the best response. Asking if the client understands he or she will have to undergo genetic testing is a correct statement, but is a yes/no question which is not therapeutic and might sound paternalistic. It also does not provide any information on the therapy itself. The drug is not limited to children and helps move chloride closer to the membrane surfaces so it would have an effect on any organ compromised by CF.
A nurse cares for a client with a 40-year smoking history who is experiencing distended neck veins and dependent edema. Which physiologic process would the nurse correlate with this client’s history and clinical signs and symptoms?
A. Increased pulmonary pressure creating a higher workload on the right side of the heart
B. Exposure to irritants resulting in increased inflammation of the bronchi and bronchioles
C. Increased number and size of mucous glands producing large amounts of thick mucus
D. Left ventricular hypertrophy creating a decrease in cardiac output
A
Smoking increases pulmonary hypertension, resulting in cor pulmonale, or right-sided heart failure. Increased pressures in the lungs make it more difficult for blood to flow through the lungs. Blood backs up into the right side of the heart and then into the peripheral venous system, creating distended neck veins and dependent edema. Inflammation in bronchi and bronchioles creates an airway obstruction which manifests as wheezes. Thick mucus in the lungs has no impact on distended neck veins and edema. Left ventricular hypertrophy is associated with left-heart failure and is not directly caused by a 40-year smoking history.
A nurse cares for a client with chronic obstructive pulmonary disease (COPD) who appears thin and disheveled. Which question would the nurse ask first?
A. “Do you have a strong support system?”
B. “What do you understand about your disease?”
C. “Do you experience shortness of breath with basic activities?”
D. “What medications are you prescribed to take each day?”
C
Clients with severe COPD may not be able to perform daily activities, including bathing and eating, because of excessive shortness of breath. The nurse would ask the client if shortness of breath is interfering with basic activities. Although the nurse would need to know about the client’s support systems, current knowledge, and medications, these questions do not address the client’s appearance.
A clinic nurse is reviewing care measures with a client who has asthma, Step 3. What statement by the client indicates the need to review the information?
A. “I still will use my rapid-acting inhaler for an asthma attack.”
B. “I will always use the spacer with my dry powder inhaler.”
C. “If I am stable for 3 months, I might be able to reduce my drugs.”
D. “My inhaled corticosteroid must be taken regularly to work well.”
B
Dry powder inhalers are not used with a spacer. The other statements are accurate.
A pulmonary nurse cares for clients who have chronic obstructive pulmonary disease (COPD). Which client would the nurse assess first?
A. A 46 year old with a 30–pack-year history of smoking
B. A 52 year old in a tripod position using accessory muscles to breathe
C. A 68 year old who has dependent edema and clubbed fingers
D. A 74 year old with a chronic cough and thick, tenacious secretions
B
The client who is in a tripod position and using accessory muscles is working to breathe. This client must be assessed first to establish how effectively the client is breathing and provide interventions to minimize respiratory distress. The other clients are not in acute distress.
A nurse cares for a client who has a pleural chest tube. What action would the nurse take to ensure safe use of this equipment?
A. Strip the tubing to minimize clot formation and ensure patency.
B. Secure tubing junctions with clamps to prevent accidental disconnections.
C. Connect the chest tube to wall suction as prescribed by the primary health care provider.
D. Keep padded clamps at the bedside for use if the drainage system is interrupted.
D
Padded clamps would be kept at the bedside for use if the drainage system becomes dislodged or is interrupted. The nurse would never strip the tubing. Tubing junctions would be taped, not clamped. Wall suction would be set at the level indicated by the device’s manufacturer, not the primary health care provider.
A nurse cares for a client who has a family history of cystic fibrosis. The client asks, “Will my children have cystic fibrosis?” How would the nurse respond?
A. “Since many of your family members are carriers, your children will also be carriers of the gene.”
B. “Cystic fibrosis is an autosomal recessive disorder. If you are a carrier, your children will have the disorder.”
C. “Since you have a family history of cystic fibrosis, I would encourage you and your partner to be tested.”
D. “Cystic fibrosis is caused by a protein that controls the movement of chloride. Adjusting your diet will decrease the spread of this disorder.”
C
Cystic fibrosis is an autosomal recessive disorder in which both gene alleles must be mutated for the disorder to be expressed. The nurse would encourage both the client and partner to be tested for the abnormal gene. The other statements are not true.
A nurse administers medications to a client who has asthma. Which medication classification is paired correctly with its physiologic action?
A. Bronchodilator—stabilizes the membranes of mast cells and prevents the release of inflammatory mediators.
B. Cholinergic antagonist—causes bronchodilation by inhibiting the parasympathetic nervous system.
C. Corticosteroid—relaxes bronchiolar smooth muscles by binding to and activating pulmonary beta2
D. Cromone—disrupts the production of pathways of inflammatory mediators.
B
Cholinergic antagonist drugs cause bronchodilation by inhibiting the parasympathetic nervous system. This allows the sympathetic nervous system to dominate and release norepinephrine that activates beta2 receptors. Bronchodilators relax bronchiolar smooth muscles by binding to and activating pulmonary beta2 receptors. Corticosteroids disrupt the production of pathways of inflammatory mediators. Cromones stabilize the membranes of mast cells and prevent the release of inflammatory mediators.
A nurse evaluates the following arterial blood gas and vital sign results for a client with chronic obstructive pulmonary disease (COPD):
Arterial Blood Gas Results:
pH = 7.32
PaCO2 = 62 mm Hg
PaO2 = 46 mm Hg
HCO3 = 28 mEq/L (28 mmol/L)
Vitals:
Heart rate = 110 beats/min
Respiratory rate = 12 breaths/min
Blood pressure = 145/65 mm Hg
Oxygen saturation = 76%
What action would the nurse take first?
A. Administer a short-acting beta2 agonist inhaler.
B. Document the findings as normal for a client with COPD.
C. Teach the client diaphragmatic breathing techniques.
D. Initiate oxygenation therapy to increase saturation to 88% to 92%.
D
Oxygen would be administered to a client who is hypoxic even if the client has COPD and is a carbon dioxide retainer. The other interventions do not address the client’s hypoxia, which is the major issue. There is no indication the client needs an inhaler. Diaphragmatic breathing techniques would not be taught to a client in distress. These findings are not normal for all clients with COPD.
A nurse assesses a client with asthma and notes bilateral wheezing, decreased pulse oxygen saturation, and suprasternal retraction on inhalation. What actions by the nurse are best?
(Select all that apply.)
A. Administer prescribed salmeterol inhaler.
B. Assess the client for a tracheal deviation.
C. Administer oxygen and place client on an oximeter.
D. Perform peak expiratory flow readings
E. Administer prescribed albuterol inhaler.
F. Assess the client’s lung sounds after administering the inhaler.
C, E, F
Suprasternal retraction caused by inhalation usually indicates that the client is using accessory muscles and is having difficulty moving air into the respiratory passages because of airway narrowing. Wheezing indicates a narrowed airway; a decreased pulse oxygen saturation also supports this finding. The asthma is becoming unstable, and intervention is needed.
Administration of a rescue inhaler is indicated, probably along with administration of oxygen. The nurse would reassess the lung sounds after the rescue inhaler. The nurse would not do a peak flow reading at this time, nor would a code be called. The nurse could assess for tracheal deviation after administering oxygen and albuterol.
A nurse teaches a client who has chronic obstructive pulmonary disease. Which statements related to nutrition would the nurse include in this client’s teaching? (Select all that apply.)
A. “Avoid drinking fluids just before and during meals.”
B. “Rest before meals if you have dyspnea.”
C. “Have about six small meals a day.”
D. “Eat high-fiber foods to promote gastric emptying.”
E. “Use pursed-lip breathing during meals.”
F. “Choose soft, high-calorie, high-protein foods.”
A, B, C, E, F
Clients with COPD often are malnourished for several reasons. The nurse would teach the client not to drink fluids before and with meals to avoid early satiety. The client needs to rest before eating, and eat smaller frequent meals: 4 to 6 a day. Pursed-lip breathing will help control dyspnea. Food that is easy to eat will be less tiring and the client should choose high-calorie, high-protein foods.
A client, who has become increasingly dyspneic over a year, has been diagnosed with pulmonary fibrosis. What information would the nurse plan to include in teaching this client?
(Select all that apply.)
A. The need to avoid large crowds and people who are ill
B. Safety measures to take if home oxygen is needed
C. Information about appropriate use of the drug nintedanib
D. Genetic therapy to stop the progression of the disease
E. Measures to avoid fatigue during the day
F. The possibility of receiving a lung transplant if infection-free for a year
A, B, C, E
Pulmonary fibrosis is a progressive disorder with no cure. Therapy focuses on slowing progression and managing dyspnea. Clients need to avoid contracting infections so should be taught to stay away from large crowds and sick people. Home oxygen is needed and the nurse would teach safety measures related to oxygen. The drug nintedanib has shown to improve cellular regulation and slow progression of the disease. Gene therapy is not available. Energy conservation measures are also an important topic. Lung transplantation is an unlikely option due to selection criteria.
A nurse working in a geriatric clinic sees clients with “cold” symptoms and rhinitis. The primary health care provider (PHCP) often leaves a prescription for diphenhydramine. What action by the nurse is best?
A. Teach the client about possible drowsiness.
B. Instruct the client to drink plenty of water.
C. Consult with the PHCP about the medication.
D. Encourage the client to take the medication with food.
C
First-generation antihistamines are not appropriate for use in the older population. These drugs include chlorpheniramine, diphenhydramine, and hydroxyzine. The nurse would consult with the PHCP and request a different medication. Diphenhydramine does cause drowsiness, but the nurse would request a different medication. Drinking plenty of fluids is appropriate for the condition and is not related to the medication. Antihistamines can be taken without regard to food.
A nurse in a family practice clinic is preparing discharge instructions for a client reporting facial pain that is worse when bending over, tenderness across the cheeks, and postnasal discharge. What instruction will be most helpful?
A. “Ice packs may help with the facial pain.”
B. “Limit fluids to dry out your sinuses.”
C. “Try warm, moist heat packs on your face.”
D. “We will schedule a computed tomography scan this week.”
C
This client has rhinosinusitis. Comfort measures for this condition include humidification, hot packs, nasal saline irrigations, sleeping with the head elevated, increased fluids, and avoiding cigarette smoke. The client does not need a CT scan.
A client is in the family practice clinic reporting a severe “cold” that started 4 days ago. On examination, the nurse notes that the client also has a severe headache and muscle aches.
What action by the nurse is best?
A. Educate the client on oseltamivir.
B. Facilitate admission to the hospital.
C. Instruct the client to have a flu vaccine.
D. Teach the client to sneeze in the upper sleeve.
D
Sneezing and coughing into one’s sleeve helps prevent the spread of upper respiratory infections. The client does have symptoms of the flu (influenza), but it is too late to start antiviral medications; to be effective, they must be started within 24 to 48 hours of symptom onset. The client does not need hospital admission. The client would be instructed to have a flu vaccination, but now that he or she has the flu, vaccination will have to wait until next year.
A client admitted for pneumonia has been tachypneic for several days. When the nurse starts an IV to give fluids, the client questions this action, saying “I have been drinking tons of water. How am I dehydrated?” What response by the nurse is best?
A. “Breathing so quickly can be dehydrating.”
B. “Everyone with pneumonia is dehydrated.”
C. “This is really just to administer your antibiotics.”
D. “Why do you think you are so dehydrated?”
A
Tachypnea and mouth breathing (from increased work of breathing), both seen in pneumonia, increase insensible water loss and can lead to a degree of dehydration. The other options do not give the client useful information that addresses this specific concern.
An older adult is brought to the emergency department by a family member, who reports a moderate change in mental status and mild cough. The client is afebrile. The primary health care provider orders a chest x-ray. The family member questions why this is needed since the symptoms seem so vague. What response by the nurse is best?
- “Chest x-rays are always ordered when we suspect pneumonia.”
- “Older people often have vague symptoms, so an x-ray is essential.”
- “The x-ray can be done and read before laboratory work is reported.”
- “We are testing for any possible source of infection in the client.”
B
It is essential to obtain an early chest x-ray in older adults suspected of having pneumonia because symptoms are often vague. Waiting until definitive signs and symptoms are present to obtain the x-ray leads to a costly delay in treatment. Stating that chest x-rays are always ordered does not give the family definitive information. The x-ray can be done while laboratory values are still pending, but this also does not provide specific information about the importance of a chest x-ray in this client. The client has symptoms of pneumonia, so the staff is not testing for any possible source of infection but rather is testing for a suspected disorder.
A client has been diagnosed with tuberculosis (TB). What action by the nurse takes highest
priority?
A. Educating the client on adherence to the treatment regimen
B. Encouraging the client to eat a well-balanced diet
C. Informing the client about follow-up sputum cultures
D. Teaching the client ways to balance rest with activity
A
The treatment regimen for TB often ranges from 26 weeks, but can be up to 2 years, making adherence problematic for many people. The nurse would stress the absolute importance of following the treatment plan for the entire duration of prescribed therapy. The other options are appropriate topics to educate this client on but do not take priority.
A client has been admitted for suspected inhalation anthrax infection. What question by the nurse is most important?
A. “Are any family members also ill?”
B. “Have you traveled recently?”
C. “How long have you been ill?”
D. “What is your occupation?”
D
Inhalation anthrax is rare and is an occupational hazard among people who work with animal wool, bone meal, hides, and skin, such as taxidermists and veterinarians. Inhalation anthrax seen in someone without an occupational risk is considered a bioterrorism event and must be reported to authorities immediately. The other questions are appropriate for anyone with an infection.
A charge nurse is rounding on several older clients on ventilators in the Intensive Care Unit whom the nurse identifies as being at high risk for ventilator-associated pneumonia. To reduce this risk, what activity would the nurse delegate to the assistive personnel (AP)?
A. Encourage between-meal snacks
B. Monitor temperature every 4 hours.
C. Provide oral care every 4 hours.
D. Report any new onset of cough.
C
Oral colonization by gram-negative bacteria is a risk factor for health care–associated pneumonia. Good, frequent oral care can help prevent this from developing and is a task that can be delegated to the AP. Encouraging good nutrition is important, but this will not prevent pneumonia. Monitoring temperature and reporting new cough in clients are important to detect the onset of possible pneumonia but do not prevent it.
The emergency department (ED) manager is reviewing client charts to determine how well the staff perform when treating clients with community-acquired pneumonia. What outcome demonstrates that goals for this client type have been met?
A. Antibiotics started before admission.
B. Blood cultures obtained within 20 minutes.
C. Chest x-ray obtained within 30 minutes.
D. Pulse oximetry obtained on all clients.
A
Goals for treatment of community-acquired pneumonia include initiating antibiotics prior to inclient admission or within 6 hours of presentation to the ED. Timely collection of blood cultures, chest x-ray, and pulse oximetry are important as well but do not coincide with established goals.
A client seen in the emergency department reports fever, fatigue, and dry cough but no other upper respiratory symptoms. A chest x-ray reveals mediastinal widening. What action by the nurse is best?
A. Collect a sputum sample for culture by deep suctioning.
B. Inform the client that oral antibiotics will be needed for 60 days.
C. Place the client on Airborne Precautions immediately.
D. Tell the client that directly observed therapy is needed.
B
This client has signs and symptoms of early inhalation anthrax. For treatment, after IV antibiotics are finished, oral antibiotics are continued for at least 60 days. Sputum cultures are not needed. Anthrax is not transmissible from person to person, so Standard Precautions are adequate. Directly observed therapy is often used for tuberculosis.
A client has been hospitalized with tuberculosis (TB). The client’s spouse is fearful of entering the room where the client is in isolation and refuses to visit. What action by the nurse is best?
A. Ask the spouse to explain the fear of visiting in further detail.
B. Inform the spouse that the precautions are meant to keep other clients safe.
C. Show the spouse how to follow the Isolation Precautions to avoid illness.
D. Tell the spouse that he or she has already been exposed, so it’s safe to visit.
A
The nurse needs to obtain further information about the spouse’s specific fears so they can be addressed. This will decrease stress and permit visitation, which will be beneficial for both client and spouse. Precautions for TB prevent transmission to all who come into contact with the client. Explaining Isolation Precautions and what to do when entering the room will be helpful, but this is too narrow in scope to be the best answer. Telling the spouse that it’s safe to visit is demeaning of the spouse’s feelings.
A client is being discharged on long-term therapy for tuberculosis (TB). What referral by the nurse is most appropriate?
A. Community social worker for Meals on Wheels
B. Occupational therapy for job retraining
C. Physical therapy for homebound therapy services
D. Visiting nurses for directly observed therapy
D
Directly observed therapy is often utilized for managing clients with TB in the community. Meals on Wheels, job retraining, and home therapy may or may not be appropriate.

A client is admitted with suspected pneumonia from the emergency department. The client went to the primary health care provider a “few days ago” and shows the nurse the results of what the client calls “an allergy test,” as shown below:
The reddened area is firm. What action by the nurse is best?
A. Assess the client for possible items to which he or she is allergic.
B. Call the primary health care provider’s office to request records.
C. Immediately place the client on Airborne PRecautions.
D. Prepare to begin administration of intravenous antibiotics.
C
This “allergy test” is actually a positive tuberculosis test. The client would be placed on Airborne Precautions immediately. The other options do not take priority over preventing the spread of the disease.
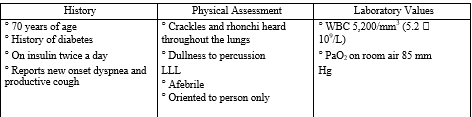
A nurse admits a client from the emergency department. Client data are listed below:
What action by the nurse is the priority?
A. Administer oxygen at 4 L per nasal cannula.
B. Begin broad-spectrum antibiotics.
C. Collect a sputum sample for culture.
D. Start an IV of normal saline at 50 mL/hr.
A
All actions are appropriate for this client who has signs and symptoms of pneumonia. However, airway and breathing come first, so begin oxygen administration and titrate it to maintain saturations greater than 95%. Start the IV and collect a sputum culture, and then begin antibiotics.
A client is taking ethambutol for tuberculosis. What instructions does the nurse provide the client regarding this drug? (Select all that apply.)
A. Contact the primary health care provider if preexisting gout becomes worse.
B. Report any changes in vision immediately to the health care provider.
C. Avoid drinking alcoholic beverages due to the chance of liver damage.
D. Do not take antacids or eat within 2 hours after taking this medication.
E. You will take this medication along with some others for 8 weeks.
F. Take this medicine with a full glass of water.
A, B, E, F
The nurse would teach the client that preexisting gout may get worse and the client should report this as medications for gout may need to be adjusted. The nurse would also inform the client about the multi-drug routine used for TB. Optic neuritis can occur with this drug so the client needs to report visual changes right away. The medication should be taken with a full glass of water. Drinking while taking ethambutol causes severe nausea and vomiting.
Avoiding antacids and food (within 2 hours) is a precaution with isoniazid.
A nurse assesses a client who had a myocardial infarction and has a blood pressure of 88/58 mm Hg. Which additional assessment finding would the nurse expect?
A. Heart rate of 120 beats/min
B. Cool, clammy skin
C. Oxygen saturation of 90%
D. Respiratory rate of 8 breaths/min
A
When a client experiences hypotension, baroreceptors in the aortic arch sense a pressure decrease in the vessels. The parasympathetic system responds by lessening the inhibitory effect on the sinoatrial node. This results in an increase in heart rate and respiratory rate. This tachycardia is an early response and is seen even when blood pressure is not critically low. An increased heart rate and respiratory rate will compensate for the low blood pressure and maintain oxygen saturation and perfusion. The client may not be able to compensate for long and decreased oxygenation and cool, clammy skin will occur later.
A nurse assesses a client after administering a prescribed beta blocker. Which assessment would the nurse expect to find?
A. Blood pressure increased from 98/42 to 132/60 Mm Hg.
B. Respiratory rate decreased from 25 to 14 breaths/min.
C. Oxygen saturation increased from 88% to 96%.
D. Pulse decreased from 100 to 80 beats/min.
D
Beta blockers block the stimulation of beta1-adrenergic receptors. They block the sympathetic (fight-or-flight) response and decrease the heart rate (HR). The beta blocker will decrease HR and blood pressure, increasing ventricular filling time. It usually does not have effects on beta2-adrenergic receptor sites. Cardiac output may drop because of decreased HR, but slowing the rate may allow for better filling and better cardiac output.
A nurse assesses clients on a medical-surgical unit. Which client would the nurse identify as having the greatest risk for cardiovascular disease?
A. An 86-year-old man with a history of asthma.
B. A 32-year-old man with colorectal cancer.
C. A 65-year-old woman with diabetes mellitus.
D. A 53-year-old postmenopausal woman who takes bisphosphonates.
C
Of the options, the client with diabetes has a two- to four-fold increase in risk for death due to cardiovascular disease. Advancing age also increases risk, but not as much. Asthma, colorectal cancer, and bisphosphonate therapy do not increase the risk for cardiovascular disease.
A nurse assesses an older adult client who has multiple chronic diseases. The client’s heart rate is 48 beats/min. What action would the nurse take first?
A. Document the finding in the chart.
B. Initiate external pacing.
C. Assess the client’s medications.
D. Administer 1 mg of atropine.
C
Pacemaker cells in the conduction system decrease in number as a person ages, potentially resulting in bradycardia. However, the nurse would first check the medication reconciliation for medications that might cause such a drop in heart rate, and then would inform the primary health care provider. Documentation is important, but it is not the first action. The heart rate is not low enough for atropine or an external pacemaker to be needed unless the client is symptomatic, which is not apparent.
A nurse obtains the health history of a client who is newly admitted to the medical unit.
Which statement by the client would alert the nurse to the presence of edema?
A. “I wake up to go to the bathroom at night.”
B. “My shoes fit tighter by the end of the day.”
C. “I seem to be feeling more anxious lately.”
D. “I drink at least eight glasses of water a day.”
B
Weight gain can result from fluid accumulation in the interstitial spaces. This is known as edema. The nurse would note whether the client feels that his or her shoes or rings are tight, and would observe, when present, an indentation around the leg where the socks end. The other answers do not describe edema.
A nurse assesses female client who is experiencing a myocardial infarction. Which clinical manifestation would the nurse expect?
A.Excruciating pain on inspiration
B. Left lateral chest wall pain
C. Fatigue and shortness of breath
D. Numbness and tingling of the arm
C
In women, fatigue, shortness of breath, and indigestion may be the major symptoms of myocardial infarction caused by poor cardiac output. Chest pain is the classic symptom of myocardial infarction and can be present in women. Pain on inspiration may be related to a pleuropulmonary cause. Numbness and tingling of the arm could also be related to the myocardial infarction, but are not known to be specific symptoms for women having and MI.
A nurse assesses a client 2 hours after a cardiac angiography via the left femoral artery. The nurse notes that the left pedal pulse is weak. What action would the nurse take next?
A. Elevate the leg and apply a sandbag to the entrance site.
B. Increase the flow rate of intravenous fluids.
C. Assess the color and temperature of the left leg.
D. Document the finding as “left pedal pulse of +1/4.”
C
Loss of a pulse distal to an angiography entry site is serious, indicating a possible arterial obstruction. The left pulse would be compared with the right, and pulses would be compared with previous assessments, especially before the procedure. Assessing color (pale, cyanosis) and temperature (cool, cold) will identify a decrease in circulation. Once all peripheral and vascular assessment data are acquired, the primary health care provider would be notified. Simply documenting the findings is inappropriate. The leg would be positioned below the level of the heart to increase blood flow to the distal portion of the leg. Increasing intravenous fluids will not address the client’s problem.
A nurse assesses a client who is recovering after a left-sided cardiac catheterization. Which assessment finding requires immediate intervention?
A. Urinary output less than intake
B. Bruising at the insertion site
C. Slurred speech and confusion
D. Discomfort in the left leg
C
A left-sided cardiac catheterization specifically increases the risk for a cerebral vascular accident. A change in neurologic status needs to be acted on immediately. Discomfort and bruising are not unexpected at the site. Urinary output less than intake may or may not be significant.
A nurse assesses a client who is scheduled for a cardiac catheterization. Which assessment would the nurse complete as the priority prior to this procedure?
A. Client’s level of anxiety
B. Ability to turn self in bed
C. Cardiac rhythm and heart rate
D. Allergies to iodine-based agents
D
Before the procedure, the nurse would ascertain whether the client has an allergy to iodine-containing preparations, such as seafood or local anesthetics. The contrast medium used during the procedure is iodine based. This allergy can cause a life-threatening reaction, so it is a high priority. It is important for the nurse to assess anxiety, mobility, and baseline cardiac status, but allergies take priority for client safety.
A nurse cares for a client who is prescribed magnetic resonance imaging (MRI) of the heart. The client’s health history includes a previous myocardial infarction and pacemaker implantation. What action would the nurse take?
A. Schedule an electrocardiogram just before the MRI.
B. Notify the primary health care provider before scheduling the MRI.
C. Request lab for cardiac enzymes from the primary health care provider.
D. Instruct the client to increase fluid intake the day before the MRI.
B
The magnetic fields of the MRI can deactivate the pacemaker. The nurse would call the primary health care provider and report that the client has a pacemaker so that he or she can order other diagnostic tests. The client does not need an electrocardiogram, cardiac enzymes, or increased fluids. Some newer MRI scanners have eliminated the possibility of complications due to implants, but the nurse needs to notify the primary health care provider.
A nurse assesses a client who is recovering from a myocardial infarction. The client’s blood pressure is 140/88 mm Hg. What action would the nurse take first?
A. Compare the results with previous blood pressure readings.
B. Increase the intravenous fluid rate because these readings are low.
C. Immediately notify the primary health care provider of the elevated blood pressure.
D. Document the finding in the client’s chart as the only action.
A
The most recent range for normal blood pressure is less than 140 mm Hg systolic and less than 90mm Hg diastolic. This client’s blood pressure is at the upper range of acceptable, so the nurse would compare the client’s current reading with those previously recorded before doing anything else. The reading is not low, so the nurse would not increase IV fluids, nor would the nurse necessarily notify the primary health care provider. Documentation is important, but the nurse first checks previous readings.
A nurse teaches a client with diabetes mellitus and a body mass index of 42 who is at high risk for coronary artery disease. Which statement related to nutrition would the nurse include in this client’s teaching?
A. “The best way to lose weight is a high-protein, low-carbohydrate diet.”
B. “You should balance weight loss with consuming necessary nutrients.”
C. “A nutritionist will provide you with information about your new diet.”
D. “If you exercise more frequently, you won’t need to change your diet.”
B
Clients at risk for cardiovascular diseases should follow the American Heart Association guidelines to combat obesity and improve cardiac health. The nurse would encourage the client to eat vegetables, fruits, unrefined whole-grain products, and fat-free dairy products while losing weight. High-protein food items are often high in fat and calories. Although the nutritionist can assist with client education, the nurse would include nutrition education and assist the client to make healthy decisions. Exercising and eating nutrient-rich foods are both important components in reducing cardiovascular risk.
A nurse cares for a client who has advanced cardiac disease and states, “I am having trouble breathing while I’m sleeping at night.” What is the nurse’s best response?
A. “I will consult your primary health care provider to prescribe a sleep study.”
B. “You become hypoxic while sleeping; oxygen therapy via nasal cannula will help.”
C. “A continuous positive airway pressure, or CPAP, breathing mask will help you breathe at night.”
D. “Use pillows to elevate your head and chest while you are sleeping.”
D
The client is experiencing orthopnea (shortness of breath while lying flat). The nurse would teach the client to elevate the head and chest with pillows or sleep in a recliner. A sleep study is not necessary to diagnose this client. Oxygen and CPAP will not help a client with orthopnea.
A nurse cares for a client who is recovering from a myocardial infarction. The client states, “I will need to stop eating so much chili to keep that indigestion pain from returning.” What is the nurse’s best response?
A. “Chili is high in fat and calories; it would be a good idea to stop eating it.”
B. “The primary health care provider has prescribed an antacid every morning.”
C. “What do you understand about what happened to you?”
D. “When did you start experiencing this indigestion?”
C
Clients who experience myocardial infarction often respond with denial, which is a defense mechanism. The nurse would ask the client what he or she thinks happened, or what the illness means to him or her. The other responses do not address the client’s misconception about recent pain and the cause of that pain.
A nurse prepares a client for cardiac catheterization. The client states, “I am afraid I might die.” What is the nurse’s best response?
A. “This is a routine test and the risk of death is very low.”
B. “Would you like to speak with a chaplain prior to test?”
C. “Tell me more about your concerns about the test.”
D. “What support systems do you have to assist you?”
C
The nurse would discuss the client’s feelings and concerns related to the cardiac catheterization. The nurse would not provide false hope or push the client’s concerns off on the chaplain. The nurse would address support systems after addressing the client’s current issue.
An emergency department nurse triages clients who present with chest discomfort. Which client would the nurse plan to assess first?
A. Client who describes pain as a dull ache.
B. Client who reports moderate pain that is worse on inspiration.
C. Client who reports cramping substernal pain.
D. Client who describes intense squeezing pressure across the chest.
D
All clients who have chest pain would be assessed more thoroughly. To determine which client would be seen first, the nurse must understand common differences in pain descriptions. Intense stabbing and viselike (squeezing) substernal pain or pressure that spreads through the client ’s chest, arms, jaw, back, or neck are indicatives of a myocardial infarction. The nurse would plan to see this client first to prevent cardiac cell death. A dull ache, pain that gets worse with inspiration, and cramping pain are not usually associated with myocardial infarction.
A nurse cares for a client who is recovering from a right-sided heart catheterization. For which complications of this procedure would the nurse assess? (Select all that apply.)
A. Thrombophlebitis
B. Stroke
C. Pulmonary embolism
D. Myocardial infarction
E. Cardiac tamponade
F. Dysrhythmias
A, C, E
Complications from a right-sided heart catheterization include thrombophlebitis, pulmonary embolism, and vagal response. Cardiac tamponade is a risk of both right- and left-sided heart catheterizations. Stroke, myocardial infarction, and dysrhythmias are complications of left-sided heart catheterizations.
A nurse assesses clients on a cardiac unit. Which client would the nurse identify as being at greatest risk for the development of left-sided heart failure?
A. A 36-year-old woman with aortic stenosis
B. A 42-year-old man with pulmonary hypertension
C. A 59-year-old woman who smokes cigarettes dAily
D. A 70-year-old man who had a cerebral vascular accident
A
Causes of left ventricular failure include mitral or aortic valve disease, coronary artery disease, and hypertension. Pulmonary hypertension and chronic cigarette smoking are risk factors for right ventricular failure. A cerebral vascular accident does not increase the risk of heart failure.
A nurse assesses a client in an outpatient clinic. Which statement alerts the nurse to the possibility of left-sided heart failure?
A. “I have been drinking more water than usual.”
B. “I am awakened by the need to urinate at night.”
C. “I must stop halfway up the stairs to catch my bReath.”
D. “I have experienced blurred vision on several occasions.”
C
Clients with left-sided heart failure report weakness or fatigue while performing normal activities of daily living, as well as difficulty breathing, or “catching their breath.” This occurs as fluid moves into the alveoli. Nocturia is often seen with right-sided heart failure. Thirst and blurred vision are not related to heart failure.
A nurse assesses a client admitted to the cardiac unit. Which statement by the client alerts the nurse to the possibility of right-sided heart failure?
A. “I sleep with four pillows at night.”
B. “My shoes fit really tight lately.”
C. “I wake up coughing every night.”
D.“I have trouble catching my breath.”
B
Signs of systemic congestion occur with right-sided heart failure. Fluid is retained, pressure builds in the venous system, and peripheral edema develops. Left-sided heart failure symptoms include respiratory symptoms. Orthopnea, coughing, and difficulty breathing all could be results of left-sided heart failure.
While assessing a client on a cardiac unit, a nurse identifies the presence of an S3 What action would the nurse take next?
A. Assess for symptoms of left-sided heart failure.
B. Document this as a normal finding.
C. Call the primary health care provider immediately.
D. Transfer the client to the intensive care unit.
A
The presence of an S3 gallop is an early diastolic filling sound indicative of increasing left ventricular pressure and left ventricular failure. The other actions are not warranted.
A nurse cares for a client with right-sided heart failure. The client asks, “Why do I need to weigh myself every day?” How would the nurse respond?
A. “Weight is the best indication that you are gaining or losing fluid.”
B. “Daily weights will help us make sure that you’re eating properly.”
C. “The hospital requires that all clients be weighed daily.”
D. “You need to lose weight to decrease the incidence of heart failure.”
A
Daily weights are needed to document fluid retention or fluid loss. One liter of fluid equals 2.2 lb (1 kg). Weight changes are the most reliable indicator of fluid loss or gain. The other responses do not address the importance of monitoring fluid retention or loss.
A nurse is teaching a client with heart failure who has been prescribed enalapril. Which statement would the nurse include in this client’s teaching?
A. “Avoid using salt substitutes.”
B. “Take your medication with food.”
C. “Avoid using aspirin-containing products.”
D. “Check your pulse daily.”
A
Angiotensin-converting enzyme (ACE) inhibitors such as enalapril inhibit the excretion of potassium. Hyperkalemia can be a life-threatening side effect, and clients should be taught to limit potassium intake. Salt substitutes are composed of potassium chloride. ACE inhibitors do not need to be taken with food and have no impact on the client’s pulse rate. Aspirin is often prescribed in conjunction with ACE inhibitors and is not contraindicated.
After administering the first dose of captopril to a client with heart failure, the nurse implements interventions to decrease complications. Which intervention is most important for the nurse to implement?
A. Provide food to decrease nausea and aid in absorption.
B. Instruct the client to ask for assistance when rising from bed.
C. Collaborate with assistive personnel to bathe the client.
D. Monitor potassium levels and check for symptoms of hypokalemia.
ANS: B
Hypotension is a side effect of ACE inhibitors such as captopril. Clients with a fluid volume deficit should have their volume replaced or start at a lower dose of the drug to minimize this effect. The nurse would instruct the client to seek assistance before arising from bed to prevent injury from postural hypotension. ACE inhibitors do not need to be taken with food. Collaboration with assistive personnel to provide hygiene is not a priority. The client would be encouraged to complete activities of daily living as independently as possible. The nurse would monitor for hyperkalemia, not hypokalemia, especially if the client has renal insufficiency secondary to heart failure.
A nurse assesses a client after administering the first dose of a nitrate. The client reports a headache. What action would the nurse take?
A. Initiate oxygen therapy.
B. Hold the next dose.
C. Instruct the client to drink water.
D. Administer PRN acetaminophen.
D
The vasodilating effects of nitrates frequently cause clients to have headaches during the initial period of therapy. The nurse would inform the client about this side effect and offer a mild analgesic, such as acetaminophen. The client’s headache is not related to hypoxia or dehydration; therefore, applying oxygen and drinking water would not help. The client needs to take the medication as prescribed to prevent angina; the medication would not be held.
A nurse teaches a client who is prescribed digoxin therapy. Which statement would the nurse include in this client’s teaching?
A. “Avoid taking aspirin or aspirin-containing products.”
B. “Increase your intake of foods that are high in potassium.”
C. “Hold this medication if your pulse rate is below 80 beats/min.”
D. “Do not take this medication within 1 hour of taking an antacid.”
D
Gastrointestinal absorption of digoxin is erratic. Many medications, especially antacids, interfere with its absorption. Clients are taught to hold their digoxin for bradycardia; a heart rate of 80 beats/min is too high for this cutoff. Potassium and aspirin have no impact on digoxin absorption.
A nurse teaches a client who has a history of heart failure. Which statement would the nurse include in this client’s discharge teaching?
A. “Avoid drinking more than 3 quarts (3 L) of liquids each day.”
B. “Eat six small meals daily instead of three larger meals.”
C. “When you feel short of breath, take an additional diuretic.”
D. “Weigh yourself daily while wearing the same amount of clothing.”
D
Clients with heart failure are instructed to weigh themselves daily to detect worsening heart failure early, and thus avoid complications. Other signs of worsening heart failure include increasing dyspnea, exercise intolerance, cold symptoms, and nocturia. Fluid overload increases symptoms of heart failure. The client would be taught to eat a heart-healthy diet, balance intake and output to prevent dehydration and overload, and take medications as prescribed. The most important discharge teaching is daily weights as this provides the best data related to fluid retention.
A nurse admits a client who is experiencing an exacerbation of heart failure. What action would the nurse take first?
A. Assess the client’s respiratory status.
B. Draw blood to assess the client’s serum electrolytes.
C. Administer intravenous furosemide.
D. Ask the client about current medications.
A
Assessment of respiratory and oxygenation status is the most important nursing intervention for the prevention of complications. Monitoring electrolytes, administering diuretics, and asking about current medications are important but do not take precedence over assessing respiratory status.
A nurse cares for a client recovering from prosthetic valve replacement surgery. The client asks, “Why will I need to take anticoagulants for the rest of my life?” What is the best response by the nurse?
A. “The prosthetic valve places you at greater risk for a heart attack.”
B. “Blood clots form more easily in artificial replacement valves.”
C. “The vein taken from your leg reduces circulation in the leg.”
D. “The surgery left a lot of small clots in your heart and lungs.”
B
Synthetic valve prostheses and scar tissue provide surfaces on which platelets can aggregate easily and initiate the formation of blood clots. The other responses are inaccurate.
After teaching a client who is being discharged home after mitral valve replacement surgery, the nurse assesses the client’s understanding. Which client statement indicates a need for additional teaching?
A. “I’ll be able to carry heavy loads after 6 months of rest.”
B. “I will have my teeth cleaned by my dentist in 2 weeks.”
C. “I must avoid eating foods high in vitamin K, like spinach.”
D. “I must use an electric razor instead of a straight razor to shave.”
B
Clients who have defective or repaired valves are at high risk for endocarditis. The client who has had valve surgery should avoid dental procedures for 6 months because of the risk for endocarditis. When undergoing a mitral valve replacement surgery, the client needs to be placed on anticoagulant therapy to prevent vegetation forming on the new valve. Clients on anticoagulant therapy would be instructed on bleeding precautions, including using an electric razor. If the client is prescribed warfarin, the client should avoid foods high in vitamin K. Clients recovering from open-heart valve replacements should not carry anything heavy for 6 months while the chest incision and muscle heal.
A nurse cares for a client with infective endocarditis. Which infection control precautions would the nurse use?
A. Standard Precautions
B. Bleeding Precautions
C. Reverse isolation
D. Contact isolation
A
The client with infective endocarditis does not pose any specific threat of transmitting the causative organism. Standard Precautions would be used. Bleeding Precautions, reverse isolation, or Contact Precautions are not necessary.
A nurse assesses a client with pericarditis. Which assessment finding would the nurse expect to find?
A. Heart rate that speeds up and slows down.
B. Friction rub at the left lower sternal border.
C. Presence of a regular gallop rhythm.
D. Coarse crackles in bilateral lung bases.
B
The client with pericarditis may present with a pericardial friction rub at the left lower sternal border. This sound is the result of friction from inflamed pericardial layers when they rub together. The other assessments are not related.
After teaching a client who is recovering from a heart transplant to change positions slowly, the client asks, “Why is this important?” How would the nurse respond?
A. “Rapid position changes can create shear and friction forces, which can tear out your internal vascular sutures.”
B. “Your new vascular connections are more sensitive to position changes, leading to increased intravascular pressure and dizziness.”
C. “Your new heart is not connected to the nervous system and is unable to respond to decreases in blood pressure caused by position changes.”
D. “While your heart is recovering, blood flow is diverted away from the brain, increasing the risk for stroke when you stand up.”
C
Because the new heart is denervated, the baroreceptor and other mechanisms that compensate for blood pressure drops caused by position changes do not function. This allows orthostatic hypotension to persist in the postoperative period. The other options are false statements and do not correctly address the client’s question.
A nurse is providing discharge teaching to a client recovering from a heart transplant. Which statement would the nurse include?
A. “Use a soft-bristled toothbrush and avoid flossing.”
B. “Avoid large crowds and people who are sick.”
C. “Change positions slowly to avoid hypotension.”
D. “Check your heart rate before taking the medication.”
B
Clients who have had heart transplants must take immunosuppressant therapy for the rest of their lives. The nurse would teach this client to avoid crowds and sick people to reduce the risk of becoming ill him- or herself. These medications do not place clients at risk for bleeding, orthostatic hypotension, or changes in heart rate. Orthostatic hypotension from the denervated heart is generally only a problem in the immediate postoperative period.
A nurse cares for a client with end-stage heart failure who is awaiting a transplant. The client appears depressed and states, “I know a transplant is my last chance, but I don’t want to become a vegetable.” How would the nurse respond?
A. “Would you like to speak with a priest or chaplain?”
B. “I will arrange for a psychiatrist to speak with you.”
C. “Do you want to come off the transplant list?”
D. “Would you like information about advance directives?”
D
The client is verbalizing a real concern or fear about negative outcomes of the surgery. This anxiety itself can have a negative effect on the outcome of the surgery because of sympathetic stimulation. The best action is to allow the client to verbalize the concern and work toward a positive outcome without making the client feel as though the concerns are not valid. The client needs to feel that he or she has some control over the future. The nurse personally provides care to address the client’s concerns instead of immediately calling for the chaplain or psychiatrist. The nurse would not jump to conclusions and suggest taking the client off the transplant list, which is the best treatment option.
A nurse assesses a client who has a history of heart failure. Which question would the nurse ask to assess the extent of the client’s heart failure?
A. “Do you have trouble breathing or chest pain?”
B. “Are you still able to walk upstairs without fatigue?”
C. “Do you awake with breathlessness during the night?”
D. “Do you have new-onset heaviness in your legs?”
B
Clients with a history of heart failure generally have negative findings, such as shortness of breath and fatigue. The nurse needs to determine whether the client’s activity is the same or worse, or whether the client identifies a decrease in activity level. Trouble breathing, chest pain, breathlessness at night, and peripheral edema are symptoms of heart failure, but do not provide data that can determine the extent of the client’s heart failure.
A nurse cares for an older adult client with heart failure. The client states, “I don’t know what to do. I don’t want to be a burden to my daughter, but I can’t do it alone. Maybe I should die.” What is the best response by the nurse?
A. “I can stay if you would you like to talk more about this.”
B. “You are lucky to have such a devoted daughter.”
C. “It is normal to feel as though you are a burden.”
D. “Would you like to meet with the chaplain?”
A
Depression can occur in clients with heart failure, especially older adults. Having the client talk about his or her feelings will help the nurse focus on the actual problem. Open-ended statements allow the client to respond safely and honestly. The other options minimize the client’s concerns and do not allow the nurse to obtain more information to provide client-centered care.
A nurse teaches a client with heart failure about energy conservation. Which statement would the nurse include in this client’s teaching?
A. “Walk until you become short of breath, and then walk back home.”
B. “Begin walking 200 feet a day three times a week.”
C. “Do not lift heavy weights for 6 months.”
D. “Eat plenty of protein to build your strength.”
B
A client who has heart failure would be taught to conserve energy and given an exercise plan. The client should begin walking 200-400 feet a day at home three times a week. The client should not walk until becoming short of breath because he or she may not make it back home. The lifting restriction is specifically for clients after valve replacements. Protein does help build strength, but this direction is not specific to heart failure.
A nurse is caring for a client with acute pericarditis who reports substernal precordial pain that radiates to the left side of the neck. Which nonpharmacologic comfort measure would the nurse implement?
A. Apply an ice pack to the client’s chest.
B. Provide a neck rub, especially on the left side.
C. Allow the client to lie in bed with the lights down.
D. Sit the client up with a pillow to lean forward on.
D
Pain from acute pericarditis may worsen when the client lays supine. The nurse would position the client in a comfortable position, which usually is upright and leaning slightly forward. An ice pack and neck rub will not relieve this pain. Dimming the lights will also not help the pain.
A nurse assesses a client who has mitral valve regurgitation. For which cardiac dysrhythmia would the nurse assess?
A. Preventricular contractions
B. Atrial fibrillation
C. Symptomatic bradycardia
D. Sinus tachycardia
B
Atrial fibrillation is a clinical manifestation of mitral valve regurgitation and stenosis. Preventricular contractions and bradycardia are not associated with valvular problems. These are usually identified in clients with electrolyte imbalances, myocardial infarction, and sinus node problems. Sinus tachycardia is a manifestation of aortic regurgitation due to a decrease in cardiac output.
A nurse is assessing a client with left-sided heart failure. For which clinical manifestations would the nurse assess? (Select all that apply.)
A. Pulmonary crackles
B. Confusion
C. Pulmonary hypertension
D. Dependent edema
E. Cough that worsens at night
F. Jugular venous distention
A, B, E
Left-sided heart failure occurs with a decrease in contractility of the heart or an increase in afterload. Most of the signs will be noted in the respiratory system. These include crackles, confusion (due to decreased oxygenation), and cough. Right ventricular failure is associated with pulmonary hypertension, edema, and jugular venous distention.
A nurse assesses clients on a cardiac unit. Which clients would the nurse identify as at greatest risk for the development of acute pericarditis? (Select all that apply.)
A 36-year-old woman with systemic lupus erythematosus (SLE)
B. A 42-year-old man recovering from coronary artery bypass graft surgery
C. A 59-year-old woman recovering from a hysterectomy
D. An 80-year-old man with a bacterial infection of the respiratory tract
E. An 88-year-old woman with a stage III sacral ulcer
A,B, D
Acute pericarditis is most commonly associated with acute exacerbations of systemic connective tissue disease, including SLE; with Dressler syndrome, or inflammation of the cardiac sac after cardiac surgery or a myocardial infarction; and with infective organisms, including bacterial, viral, and fungal infections. Abdominal and reproductive surgeries and pressure injuries do not increase clients’ risk for acute pericarditis.
After teaching a client with congestive heart failure (CHF), the nurse assesses the client’s understanding. Which client statements indicate a correct understanding of the teaching related to nutritional intake? (Select all that apply.)
A. “I’ll read the nutritional labels on food items for salt content.”
B. “I will drink at least 3 L of water each day.”
C. “Using salt in moderation will reduce the workload of my heart.”
D. “I will eat oatmeal for breakfast instead of ham and eggs.”
E. “Substituting fresh vegetables for canned ones will lower my salt intake.”
F. “Salt substitutes are a good way to cut down on sodium in my diet.”
A, D, E
Nutritional therapy for a client with CHF is focused on decreasing sodium and water retention to decrease the workload of the heart. The client would be taught to read nutritional labels on all food items, omit table salt and foods high in sodium (e.g., ham and canned foods), and limit water intake to a normal 2 L/day. Salt substitutes typically contain potassium, so although they are not strictly banned, clients would have to have their renal function and serum potassium monitored while using them. It would be safer to avoid them.
A nurse collaborates with assistive personnel (AP) to provide care for a client with congestive heart failure. Which instructions would the nurse provide to the AP when delegating care for this client? (Select all that apply.)
A. “Reposition the client every 2 hours.”
B. “Teach the client to perform deep-breathing exercises.”
C. “Accurately record intake and output.”
D. “Use the same scale to weigh the client each morning.”
E. “Place the client on oxygen if the client becomes short of breath.”
A, C, D
The AP should reposition the client every 2 hours to improve oxygenation and prevent atelectasis. The AP can also accurately record intake and output, and use the same scale to weigh the client each morning before breakfast. APs are not qualified to teach clients or assess the need for and provide oxygen therapy.
A nurse is assessing the peripheral vascular system of an older adult. What action by the nurse would cause the supervising nurse to intervene?
A. Assessing blood pressure in both upper extremities
B. Auscultating the carotid arteries for any bruits
C. Classifying capillary filling of 4 seconds as normal
D. Palpating both carotid arteries at the same time
D
The nurse would not compress both carotid arteries at the same time to avoid brain ischemia. Blood pressure would be taken and compared in both arms. Prolonged capillary filling is considered to be greater than 5 seconds in an older adult, so classifying refill of 4 seconds as normal would not require intervention. Bruits would be auscultated.
A nurse is working with a client who takes clopidogrel. The client’s recent laboratory results include a blood urea nitrogen (BUN) of 33 mg/dL and creatinine of 2.8 mg/dL. What action by the nurse is best?
A. Ask if the client eats grapefruit.
B. Assess the client for dehydration.
C. Facilitate admission to the hospital.
D. Obtain a random urinalysis.
A
There is a drug–food interaction between clopidogrel and grapefruit that can lead to acute kidney failure. This client has elevated renal laboratory results, indicating some degree of kidney involvement. The nurse would assess if the client eats grapefruit or drinks grapefruit juice. Dehydration can cause the BUN to be elevated, but the elevation in creatinine is more specific for a kidney injury. The client does not necessarily need to be admitted. A urinalysis may or may not be ordered.
A client asks what “essential hypertension” is. What response by the registered nurse is best?
A. “It means it is caused by another disease.”
B. “It means it is ‘essential’ that it be treated.”
C. “It is hypertension with no specific cause.”
D. “It refers to severe and life-threatening hypertension.”
C
Essential hypertension is the most common type of hypertension and has no specific cause such as an underlying disease process. Hypertension that is due to another disease process is called secondary hypertension. A severe, life-threatening form of hypertension is malignant hypertension.
A nurse is interested in providing community education and screening on hypertension. In order to reach a priority population, to what target audience would the nurse provide this service?
A. African-American churches
B. Asian-American groceries
C. High school sports camps
D. Women’s health clinics
A
African Americans in the United States have one of the highest rates of hypertension in the world. The nurse has the potential to reach this priority population by providing services at African-American churches. Although hypertension education and screening are important for all groups, African Americans are the priority population for this intervention.
A client has hypertension and high risk factors for cardiovascular disease. The client is overwhelmed with the recommended lifestyle changes. What action by the nurse is best?
A. Assess the client’s support system.
B. Assist in finding one change the client can control.
C. Determine what stressors the client faces in daily life.
D. Inquire about delegating some of the client’s obligations.
B
All options are appropriate when assessing stress and responses to stress. However, this client feels overwhelmed by the suggested lifestyle changes. Instead of looking at all the needed changes, the nurse would assist the client in choosing one the client feels optimistic about controlling. Once the client has mastered that change, he or she can move forward with another change. Determining support systems, daily stressors, and delegation opportunities does not directly impact the client’s feelings of control.
The nurse is caring for four hypertensive clients. Which drug–laboratory value combination would the nurse report immediately to the health care provider?
A. Furosemide/potassium: 2.1 mEq/L
B. Hydrochlorothiazide/potassium: 4.2 mEq/L
C. Spironolactone/potassium: 5.1 mEq/L
D. Torsemide/sodium: 142 mEq/L
A
Furosemide is a loop diuretic and can cause hypokalemia. A potassium level of 2.1 mEq/L is quite low and would be reported immediately. Spironolactone is a potassium-sparing diuretic that can cause hyperkalemia. A potassium level of 5.1 mEq/L is on the high side, but it is not as critical as the low potassium with furosemide. The other two laboratory values are normal.
A nurse is assessing a client with peripheral artery disease (PAD). The client states that walking five blocks is possible without pain. What question asked next by the nurse will give the best information?
A. “Could you walk further than that a few months ago?”
B. “Do you walk mostly uphill, downhill, or on flat surfaces?”
C. “Have you ever considered swimming instead of walking?”
D. “How much pain medication do you take each day?”
ANS: A
As PAD progresses, it takes less oxygen demand to cause pain. Needing to cut down on activity to be pain free indicates that the client’s disease is worsening. The other questions are useful, but not as important.
An older client with peripheral vascular disease (PVD) is explaining the daily foot care regimen to the family practice clinic nurse. What statement by the client may indicate a barrier to proper foot care?
A. “I nearly always wear comfy sweatpants and house shoes.”
B. “I’m glad I get energy assistance so my house isn’t so cold.”
C. “My daughter makes sure I have plenty of lotion for my feet.”
D. “My hands shake when I try to do things requiring coordination.”
D
Clients with PVD need to pay special attention to their feet. Toenails need to be kept short and cut straight across. The client whose hands shake may cause injury when trimming toenails. The nurse would refer this client to a podiatrist. Comfy sweatpants and house shoes are generally loose and not restrictive, which is important for clients with PVD. Keeping the house at a comfortable temperature makes it less likely the client will use alternative heat sources, such as heating pads, to stay warm. The client should keep the feet moist and soft with lotion.
A client is taking warfarin and asks the nurse if taking St. John’s wort is acceptable. What response by the nurse is best?
A. “No, it may interfere with the warfarin.”
B. “There isn’t any information about that.”
C. “Why would you want to take that?”
D. “Yes, it is a good supplement for you.”
A
Many foods and drugs interfere with warfarin, St. John’s wort being one of them. The nurse would advise the client against taking it. The other answers are not accurate.
A nurse is teaching a female client about alcohol intake and how it affects hypertension. The client asks if drinking two beers a night is an acceptable intake. What answer by the nurse is best?
A. “No, women should only have one beer a day as a general rule.”
B. “No, you should not drink any alcohol with hypertension.”
C. “Yes, since you are larger, you can have more alcohol.”
D. “Yes, two beers per day is an acceptable amount of alcohol.”
A
Alcohol intake should be limited to two drinks a day for men and one drink a day for women. A “drink” is classified as one beer, 1.5 ounces of hard liquor, or 5 ounces of wine. Limited alcohol intake is acceptable with hypertension. The woman’s size does not matter.
A nurse is caring for four clients. Which one would the nurse see first?
A. Client who needs a beta blocker, and has a blood pressure of 98/58 mm Hg.
B. Client who had a first dose of captopril and needs to use the bathroom.
C. Hypertensive client with a blood pressure of 188/92 mm Hg.
D. Client who needs pain medication prior to a dressing change of a surgical wound.
B
Angiotensin-converting enzyme inhibitors such as captopril can cause hypotension, especially after the first dose. The nurse would see this client first to prevent falling if the client decides to get up without assistance. The two blood pressure readings are abnormal but not critical. The nurse would check on the client with higher blood pressure next to assess for problems related to the reading. The nurse can administer the beta blocker as standards state to hold it if the systolic blood pressure is below 90 to 100 mm Hg. The client who needs pain medication prior to the dressing change is not a priority over client safety and assisting the other client to the bathroom.
A client had a percutaneous angioplasty for renovascular hypertension 3 months ago. What assessment finding by the nurse indicates that an important outcome for this client has been met?
A. Client is able to decrease blood pressure medications.
B. Insertion site has healed without redness or tenderness.
C. Most recent lab data show BUN: 19 mg/dL and creatinine 1.1 mg/dL.
D. Verbalizes understanding of postprocedure lifestyle changes.
A
Hypertension can be caused by renovascular disease. Opening up a constricted renal artery can lead to decreased blood pressure, manifested by the need for less blood pressure medication. The other findings are normal and desired, but not specifically related to hypertension caused by renal disease.
A client is 4 hours postoperative after a femoral-popliteal bypass. The client reports throbbing leg pain on the affected side, rated as 7/10. What action by the nurse is most important?
A. Administer pain medication as ordered.
B. Assess distal pulses and skin color.
C. Document the findings in the client’s chart.
D. Notify the surgeon immediately.
B
Once perfusion has been restored or improved to an extremity, clients can often feel a throbbing pain due to the increased blood flow. However, it is important to differentiate this pain from ischemia. The nurse would assess for other signs of perfusion, such as distal pulses and skin color/temperature. Administering pain medication is done once the nurse determines that the client’s perfusion status is normal. Documentation needs to be thorough. Notifying the surgeon is not necessary.
A client had a femoral-popliteal bypass graft with a synthetic graft. What action by the nurse is most important to prevent wound infection?
A. Appropriate hand hygiene before giving care
B. Assessing the client’s temperature every 4 hours
C. Clean technique when changing dressings
D. Monitoring the client’s daily white blood cell count
A
Hand hygiene is the best way to prevent infections in hospitalized clients. Dressing changes would be done with sterile technique. Assessing vital signs and white blood cell count will not prevent infection.
A client is receiving an infusion of alteplase for an intra-arterial clot. The client begins to mumble and is disoriented. What action by the nurse is most important?
A. Assess the client’s neurologic status.
B. Notify the Rapid Response Team.
C. Prepare to administer vitamin K.
D. Turn down the infusion rate.
B
Clients on fibrinolytic therapy are at high risk of bleeding. The sudden onset of neurologic signs may indicate that the client is having a hemorrhagic stroke. The nurse does need to complete a thorough neurologic examination, but would first call the Rapid Response Team based on the client’s manifestations. Vitamin K is not the antidote for this drug. Turning down the infusion rate will not be helpful if the client is still receiving any of the drug.
A new nurse is caring for a client with an abdominal aneurysm. What action by the new nurse requires the nurse’s mentor to intervene?
A. Assesses the client for back pain.
B. Auscultates over abdominal bruit.
C. Measures the abdominal girth.
D. Palpates the abdomen in four quadrants.
D
Abdominal aneurysms should never be palpated as this increases the risk of rupture. The nurse mentoring the new nurse would intervene when the new nurse attempts to do this. The other actions are appropriate.
A nurse is caring for a client with a deep vein thrombosis (DVT). What nursing assessment indicates that an important outcome has been met?
A. Ambulates with assistance
B. Oxygen saturation of 98%
C. Pain of 2/10 after medication
D. Verbalizing risk factors
B
A critical complication of DVT is pulmonary embolism. A normal oxygen saturation indicates that this has not occurred. The other assessments are also positive, but not as important.
A client has a deep vein thrombosis (DVT). What comfort measure does the nurse delegate to the assistive personnel (AP)?
A. Ambulate the client.
B. Apply a warm moist pack.
C. Massage the client’s leg.
D. Provide an ice pack.
B
Warm moist packs will help with the pain of a DVT. Ambulation is not a comfort measure. Massaging the client’s legs is contraindicated to prevent complications such as pulmonary embolism. Ice packs are not recommended for DVT.
A nurse is assessing an obese client in the clinic for follow-up after an episode of deep vein thrombosis. The client has lost 20 lb (9.09 Kg) since the last visit. What action by the nurse is best?
A. Ask if the weight loss was intended.
B. Encourage a high-protein, high-fiber diet.
C. Measure for new compression stockings.
D. Review a 3-day food recall diary.
C
Compression stockings must fit correctly in order to work. After losing a significant amount of weight, the client would be remeasured and new stockings ordered if needed. The other options are appropriate, but not the most important.
A nurse wants to provide community service that helps meet the goals of Healthy People 2020 (HP2020) related to cardiovascular disease and stroke. What activity would best meet this goal?
A. Teach high school students heart-healthy living.
B. Participate in blood pressure screenings at the mall.
C. Provide pamphlets on heart disease at the grocery store.
D. Set up an “Ask the nurse” booth at the pet store.
B
An important goal of HP2020 is to increase the proportion of adults who have had their blood pressure measured within the preceding 2 years and can state whether their blood pressure was normal or high. Participating in blood pressure screening in a public spot will best help meet that goal. The other options are all appropriate but do not specifically help meet a goal.
A client has been diagnosed with a deep vein thrombosis and is to be discharged on warfarin. The client is adamant about refusing the drug because “it’s dangerous.” What action by the nurse is best?
A. Assess the reason behind the client’s fear.
B. Remind the client about laboratory monitoring.
C. Tell the client that drugs are safer today than before.
D. Warn the client about consequences of noncompliance.
A
The first step is to assess the reason behind the client’s fear, which may be related to the experience of someone the client knows who took warfarin or misinformation. If the nurse cannot address the specific rationale, teaching will likely be unsuccessful. Laboratory monitoring once every few weeks may not make the client perceive the drug to be safe. General statements like “drugs are safer today” do not address the root cause of the problem. Warning the client about possible consequences of not taking the drug is not therapeutic and is likely to lead to an adversarial relationship.
A client with a history of heart failure and hypertension is in the clinic for a follow-up visit. The client is on lisinopril and warfarin. The client reports new-onset cough. What action by the nurse is most appropriate?
A. Assess the client’s lung sounds and oxygenation.
B. Instruct the client on another antihypertensive.
C. Obtain a set of vital signs and document them.
D. Remind the client that cough is a side effect of lisinopril.
A
This client could be having an exacerbation of heart failure or experiencing a side effect of lisinopril (and other angiotensin-converting enzyme inhibitors). The nurse would assess the client’s lung sounds and other signs of oxygenation first. The client may or may not need to switch antihypertensive medications. Vital signs and documentation are important, but the nurse would assess the respiratory system first. If the cough turns out to be a side effect, reminding the client is appropriate, but then more action needs to be taken.
A nurse is caring for a client with a nonhealing arterial lower leg ulcer. What action by the nurse is best?
A. Consult with the wound care nurse.
B. Give pain medication prior to dressing changes.
C. Maintain sterile technique for dressing changes.
D. Prepare the client for eventual amputation.
A
A nonhealing wound needs the expertise of the wound care nurse. Premedicating prior to painful procedures and maintaining sterile technique are helpful, but if the wound is not healing, more needs to be done. The client may need an amputation, but other options need to be tried first.
A client has peripheral arterial disease (PAD). What statement by the client indicates misunderstanding about self-management activities?
A. “I can use a heating pad on my legs if it’s set on low.”
B. “I should not cross my legs when sitting or lying down.”
C. “I will go out and buy some warm, heavy socks to wear.”
D. “It’s going to be really hard but I will stop smoking.”
A
Clients with PAD should never use heating pads as skin sensitivity is diminished and burns can result. The other statements show good understanding of self-management.

The nurse is assessing a client on admission to the hospital. The client’s leg appears as shown below:
What action by the nurse is best?
A. Assess the client’s ankle-brachial index.
B. Elevate the client’s leg above the heart.
C. Obtain an ice pack to provide comfort.
D. Prepare to teach about heparin sodium.
A
This client has dependent rubor, a classic finding in peripheral arterial disease. The nurse would measure the client’s ankle-brachial index. Elevating the leg above the heart will further impede arterial blood flow. Ice will cause vasoconstriction, also impeding circulation and perhaps causing tissue injury. Heparin sodium is not the drug of choice for this condition.
What nonpharmacologic comfort measures would the nurse include in the plan of care for a client with severe varicose veins? (Select all that apply.)
A. Administering mild analgesics for pain
B. Applying elastic compression stockings
C. Elevating the legs when sitting or lying
D. Reminding the client to do leg exercises
E. Teaching the client about surgical options
F. Encouraging participation in high impact aerobic activity
ANS: B, C, D
The three Es of care for varicose veins include elastic compression hose, exercise, and elevation. Mild analgesics are not a nonpharmacologic measure. Teaching about surgical options is not a comfort measure. High impact aerobics is not encouraged and is not a comfort measure.
A client has been bedridden for several days after major abdominal surgery. What action does the nurse delegate to the assistive personnel (AP) for deep vein thrombosis (DVT) prevention?
(Select all that apply.)
A. Apply compression stockings.
B. Assist with ambulation.
C. Encourage coughing and deep breathing.
D. Offer fluids frequently.
E. Teach leg exercises.
A, B ,D
The AP can apply compression stockings, assist with ambulation, and offer fluids frequently to help prevent DVT. The AP can also encourage the client to do pulmonary exercises, but these do not decrease the risk of DVT. Teaching is a nursing function.
A nurse is caring for a client on IV infusion of heparin. What actions does this nurse include in the client’s plan of care? (Select all that apply.)
A. Assess the client for bleeding.
B. Monitor the daily activated partial thromboplastin time (aPTT) results.
C. Stop the IV for aPTT above baseline.
D. Use an IV pump for the infusion.
E. Weigh the client daily on the same scale.
A, B, D
Assessing for bleeding, monitoring aPTT, and using an IV pump for the infusion are all important safety measures for heparin to prevent injury from bleeding. The aPTT needs to be 1.5 to 2.5 times normal in order to demonstrate that the heparin is therapeutic. Weighing the client is not related.
A client with a known abdominal aortic aneurysm reports dizziness and severe abdominal pain. The nurse assesses the client’s blood pressure at 82/40 mm Hg. What actions by the nurse are most important? (Select all that apply.)
A. Administer pain medication.
B. Assess distal pulses every 10 minutes.
C. Have the client sign a surgical consent.
D. Notify the Rapid Response Team.
E. Take vital signs every 10 minutes.
B, D, E
This client may have a ruptured/rupturing aneurysm. The nurse would notify the Rapid Response team and perform frequent client assessments. Giving pain medication will lower the client’s blood pressure even further. The nurse cannot have the client sign a consent until the surgeon has explained the procedure.
A client presents to the emergency department with a thoracic aortic aneurysm. Which findings are most consistent with this condition? (Select all that apply.)
A. Abdominal tenderness
B. Difficulty swallowing
C. Changes in bowel habits
D. Shortness of breath
E. Hoarseness
B, E
Signs of a thoracic aortic aneurysm include shortness of breath, hoarseness, and difficulty swallowing. Pain is often rated as a 10 on a 10-point scale. Bowel habits are not related.
The nurse is reviewing risk factors in a client who has atherosclerosis. Which findings are most concerning? (Select all that apply.)
A. Elevated low-density lipoprotein (LDL-C)
B. Decreased levels of high-density lipoprotein cholesterol (HDL-C)
C. Asian ethnicity
D. History of smoking
E. Blood pressure: 142/92 mm Hg on one occasion
A, B, D
Elevated levels of lipids (fats) such as low-density lipoprotein cholesterol (LDL-C) and decreased levels of high-density lipoprotein cholesterol can cause chemical damage to blood vessel walls. Smoking can cause endothelial damage in addition to increasing a client’s carbon monoxide levels. African American and Hispanic ethnicities carry an increased risk for atherosclerosis. Hypertension does increase atherosclerosis risk, but an elevated reading on one occasion is not classified as hypertension.
A nurse is teaching a client with diabetes mellitus who asks, “Why is it necessary to maintain my blood glucose levels no lower than about 60 mg/dL (3.3 mmol/L)?” How would the nurse respond?
A. “Glucose is the only fuel used by the body to produce the energy that it needs.”
B. “Your brain needs a constant supply of glucose because it cannot store it.”
C. “Without a minimum level of glucose, your body does not make red blood cells.”
D. “Glucose in the blood prevents the formation of lactic acid and prevents acidosis.”
B
Because the brain cannot synthesize or store significant amounts of glucose, a continuous supply from the body’s circulation is needed to meet the fuel demands of the central nervous system. The nurse would want to educate the patient to prevent hypoglycemia. The body can use other sources of fuel, including fat and protein, and glucose is not involved in the production of red blood cells. Glucose in the blood will encourage glucose metabolism but is not directly responsible for lactic acid formation.
The nurse is assessing a client for risk of developing metabolic syndrome. Which risk factor is associated with this health condition?
A. Hypotension
B. Hyperthyroidism
C. Abdominal obesity
D. Hypoglycemia
D
The client at risk for metabolic syndrome typically has hypertension, abdominal obesity, hyperlipidemia, and hyperglycemia.
After teaching a young adult client who is newly diagnosed with type 1 diabetes mellitus, the nurse assesses the client’s understanding. Which statement made by the client indicates a correct understanding of the need for eye examinations?
A. “At my age, I should continue seeing the ophthalmologist as I usually do.”
B. “I will see the eye doctor when I have a vision problem and yearly after age 40.”
C. “My vision will change quickly. I should see the ophthalmologist twice a year.
D. “Diabetes can cause blindness, so I should see the ophthalmologist yearly.”
D
Diabetic retinopathy is a leading cause of blindness in North America. All clients with diabetes, regardless of age, should be examined by an ophthalmologist (rather than an optometrist or optician) at diagnosis and at least yearly thereafter.
A nurse assesses a client who has a 15-year history of diabetes and notes decreased tactile sensation in both feet. What action would the nurse take first?
A. Document the finding in the client’s chart.
B. Assess tactile sensation in the client’s hands.
C. Examine the client’s feet for signs of injury.
D. Notify the primary health care provider.
C
Diabetic neuropathy is common when the disease is of long duration. The client is at great risk for injury in any area with decreased sensation because he or she is less able to feel injurious events. Feet are common locations for neuropathy and injury, so the nurse would inspect them for any signs of injury. After assessment, the nurse would document findings in the client’s chart. Testing sensory perception in the hands may or may not be needed. The primary health care provider can be notified after assessment and documentation have been completed.
A nurse cares for a client who has a family history of diabetes mellitus. The client states, “My father has type 1 diabetes mellitus. Will I develop this disease as well?” How would the nurse respond?
A. “Your risk of diabetes is higher than the general population, but it may not occur.”
B. “No genetic risk is associated with the development of type 1 diabetes mellitus.”
C. “The risk for becoming a diabetic is 50% because of how it is inherited.”
D. “Female children do not inherit diabetes mellitus, but male children will.”
A
Risk for type 1 diabetes is determined by inheritance of genes coding for HLA-DR and HLA-DQ tissue types. Clients who have one parent with type 1 diabetes are at increased risk for its development. Diabetes (type 1) seems to require interaction between inherited risk and environmental factors, so not everyone with these genes develops diabetes. The other statements are not accurate.
A nurse teaches a client who is diagnosed with diabetes mellitus. Which statement would the nurse include in this client’s plan of care to delay the onset of microvascular and macrovascular complications?
A. “Maintain tight glycemic control and prevent hyperglycemia.”
B. “Restrict your fluid intake to no more than 2 L a day.”
C. “Prevent hypoglycemia by eating a bedtime snack.”
D. “Limit your intake of protein to prevent ketoacidosis.”
A
Hyperglycemia is a critical factor in the pathogenesis of long-term diabetic complications. Maintaining tight glycemic control will help delay the onset of complications. Restricting fluid intake is not part of the treatment plan for patients with diabetes. Preventing hypoglycemia and ketosis, although important, is not as important as maintaining daily glycemic control.
A nurse teaches a patient about self-monitoring of blood glucose levels. Which statement would the nurse include in this client’s teaching to prevent bloodborne infections?
A. “Wash your hands after completing each test.”
B. “Do not share your monitoring equipment.”
C. “Blot excess blood from the strip with a cotton ball.”
D. “Use gloves when monitoring your blood glucose.”
B
Small particles of blood can adhere to the monitoring device, and infection can be transported from one user to another. Hepatitis B in particular can survive in a dried state for about a week. The client would be taught to avoid sharing any equipment, including the lancet holder. The client would also be taught to wash his or her hands before testing. He or she would not need to blot excess blood away from the strip or wear gloves.
A nurse teaches a client with type 2 diabetes mellitus who is prescribed glipizide (Glucotrol).
Which statement would the nurse include in this client’s teaching?
A.“Change positions slowly when you get out of bed.”
B. “Avoid taking nonsteroidal anti-inflammatory drugs (NSAIDs).”
C. “If you miss a dose of this drug, you can double the next dose.”
D. “Discontinue the medication if you develop a urinary infection.”
B
NSAIDs potentiate the hypoglycemic effects of sulfonylurea agents. Glipizide is a sulfonylurea. The other statements are not applicable to glipizide.
After teaching a patient with type 2 diabetes mellitus who is prescribed nateglinide, the nurse assesses the client’s understanding. Which statement made by the patient indicates a correct understanding of the prescribed therapy?
A. “I’ll take this medicine during each of my meals.”
B. “I must take this medicine in the morning when I wake.”
C. “I will take this medicine before I go to bed.”
D. “I will take this medicine immediately before I eat.”
D
Nateglinide is an insulin secretagogue that is designed to increase meal-related insulin secretion. It should be taken immediately before each meal. The medication should not be taken without eating as it will decrease the client’s blood glucose levels causing hypoglycemia. The medication should be taken before meals instead of during meals.
The nurse is caring for a client who has diabetes mellitus type 1 and is experiencing hypoglycemia. Which assessment findings will the nurse expect? (Select all that apply.)
A. Warm, dry skin
B. Nervousness
C. Rapid deep respirations
D. Dehydration
E. Ketoacidosis
F. Blurred vision
B, F
The client who has hypoglycemia is often anxious, nervous, and possibly confused. Due to lack of glucose, vision may be blurred or the client may report diplopia (double vision). Clients who have hyperglycemia from diabetes mellitus type 1 have warm skin, Kussmaul respirations that are rapid and deep, dehydration due to elevated blood glucose, and ketoacidosis.
A nurse teaches a client with diabetes mellitus about foot care. Which statements would the nurse include in this client’s teaching? (Select all that apply.)
A. “Do not walk around barefoot.”
B. “Soak your feet in a tub each evening.”
C. “Trim toenails straight across with a nail clipper.”
D.“Treat any blisters or sores with Epsom salts.”
E. “Wash your feet every other day.”
A, C
Clients who have diabetes mellitus are at high risk for wounds on the feet secondary to peripheral neuropathy and poor arterial circulation. The client would be instructed to not walk around barefoot or wear sandals with open toes. These actions place the client at higher risk for skin breakdown of the feet. The client would be instructed to trim toenails straight across with a nail clipper. Feet should be washed daily with lukewarm water and soap, but feet should not be soaked in the tub. The client should contact the primary health care provider immediately if blisters or sores appear and should not use home remedies to treat these wounds.
A nurse assesses a patient who is experiencing diabetic ketoacidosis (DKA). For which assessment findings would the nurse monitor the client? (Select all that apply.)
A. Deep and fast respirations
B. Decreased urine output
C. Tachycardia
D. Dependent pulmonary crackles
E. Orthostatic hypotension
A, C, E
DKA leads to dehydration, which is manifested by tachycardia and orthostatic hypotension. Usually, patients have Kussmaul respirations, which are fast and deep. Increased urinary output (polyuria) is severe. Because of diuresis and dehydration, peripheral edema and crackles do not occur.
A nurse assesses adults at a health fair. Which adults would the nurse counsel to be tested for diabetes? (Select all that apply.)
A. A 56-year-old African-American male
B. A 22-year-old female with a 30-lb (13.6 kg) weight gain during pregnancy
C. A 60-year-old male with a history of liver trauma
D. A 48-year-old female with a sedentary lifestyle
E. A 50-year-old male with a body mass index greater than 25 kg/m2
F. A 28-year-old female who gave birth to a baby weighing 9.2 lb (4.2 kg)
A, D, E, F
Risk factors for type 2 diabetes include certain ethnic/racial groups (African Americans, American Indians, and Hispanics), obesity and physical inactivity, and giving birth to large babies. Liver trauma and a 30-lb (13.6 kg) gestational weight gain are not risk factors.
The nurse is caring for a newly admitted client who is diagnosed with hyperglycemic-hyperosmolar state (HHS). What is the nurse’s priority action at this time?
A. Assess the client’s blood glucose level.
B. Monitor the client’s urinary output every hour.
C. Establish intravenous access to provide fluids.
D. Give regular insulin per agency policy.
C
The first priority in caring for a client with HHS is to increase blood volume to prevent shock or severe hypotension from dehydration. The nurse would monitor vital signs, urinary output, and blood glucose to determine if interventions were effective. Regular insulin is also indicated but not as the first priority action.
The nurse is caring for a newly admitted older adult who has a blood glucose of 300 mg/dL (16.7 mmol/L), a urine output of 185 mL in the past 8 hours, and a blood urea nitrogen (BUN) of 44 mg/dL (15.7 mmol/L). What diabetic complication does the nurse suspect?
A. Diabetic ketoacidosis (DKA)
B. Severe hypoglycemia
C. Chronic kidney disease (CKD)
D. Hyperglycemic-hyperosmolar state (HHS)
D
The client most likely has diabetes mellitus type 2 and has a high blood glucose causing increased blood osmolarity and dehydration, as evidenced by an insufficient urinary output and increased BUN. Older adults are at the greatest risk for dehydration due to age-related physiologic changes.
A nurse reviews laboratory results for a client with diabetes mellitus who is prescribed an intensified insulin regimen:
- Fasting blood glucose: 75 mg/dL (4.2 mmol/L)
- Postprandial blood glucose: 200 mg/dL (11.1 mmol/L)
- Hemoglobin A1C level: 5.5%
How would the nurse interpret these laboratory findings?
A. Increased risk for developing ketoacidosis
B. Good control of blood glucose
C. Increased risk for developing hyperglycemia
D. Signs of insulin resistance
B
The client is maintaining blood glucose levels within the defined ranges for goals in an intensified regimen. Because the client’s glycemic control is good, he or she is not at higher risk for ketoacidosis or hyperglycemia and is not showing signs of insulin resistance.
After teaching a client who is newly diagnosed with type 2 diabetes mellitus, the nurse assesses the client’s understanding. Which statement made by the client indicates a need for additional teaching?
A. “I should increase my intake of vegetables with higher amounts of dietary fiber.”
B. “My intake of saturated fats should be no more than 10% of my total calorie intake.”
C. “I should decrease my intake of protein and eliminate carbohydrates from my diet.”
D. “My intake of water is not restricted by my treatment plan or medication regimen.”
C
The client should not completely eliminate carbohydrates from the diet, and should reduce protein if microalbuminuria is present. The client should increase dietary intake of complex carbohydrates, including vegetables, and decrease intake of fat. Water does not need to be restricted unless kidney failure is present.
A nurse assesses a client with diabetes mellitus who self-administers subcutaneous insulin. The nurse notes a spongy, swelling area at the site the client uses most frequently for insulin injection. What action would the nurse take?
A. Apply ice to the site to reduce inflammation.
B. Consult the provider for a new administration route.
C. Assess the client for other signs of cellulitis.
D. Instruct the client to rotate sites for insulin injection.
D
The client’s tissue has been damaged from continuous use of the same site. The client would be educated to rotate sites. The damaged tissue is not caused by cellulitis or any type of infection, and applying ice may cause more damage to the tissue. Insulin can only be administered subcutaneously and intravenously. It would not be appropriate or practical to change the administration route.
When teaching a client recently diagnosed with type 1 diabetes mellitus, the client states, “I will never be able to stick myself with a needle.” How would the nurse respond?
A. “I can give your injections to you while you are here in the hospital.”
B. “Everyone gets used to giving themselves injections. It really does not hurt.”
C. “Your disease will not be managed properly if you refuse to administer the shots.”
D. “Tell me what it is about the injections that are concerning you.”
D
Devote as much teaching time as possible to insulin injection and blood glucose monitoring. Clients with newly diagnosed diabetes are often fearful of giving themselves injections. If the client is worried about giving the injections, it is best to try to find out what specifically is causing the concern, so it can be addressed. Giving the injections for the client does not promote self-care ability. Telling the client that others give themselves injections may cause the client to feel bad. Stating that you don’t know another way to manage the disease is dismissive of the client’s concerns.
The nurse is caring for a client who has diabetes mellitus. The nurse administers 6 units of regular insulin and 10 units of NPH insulin at 7:00 a.m. (0700). At which time would the nurse assess the client for potential hypoglycemia related to the NPH insulin?
A. 8:00 a.m. (0800)
B. 4:00 p.m. (1600)
C. 8:00 p.m. (2000)
D. 11:00 p.m. (2300)
B
Neutral protamine Hagedorn (NPH) is an intermediate-acting insulin with an onset of 1.5 hours, peak of 4 to 12 hours, and duration of action of 22 hours. Checking the client at 0800 would be too soon. Checking the patient at 2000 and 2300 would be too late. The nurse would check the patient at 1600 (4:00 p.m.).
A nurse reviews the laboratory results of a client who is receiving intravenous insulin. Which would alert the nurse to intervene immediately?
A. Serum chloride level of 98 mEq/L (98 mmol/L)
B. Serum calcium level of 8.8 mg/dL (2.2 mmol/L)
C. Serum sodium level of 132 mEq (132 mmol/L)
D. Serum potassium level of 2.5 mEq/L (2.5 mmol/L)
D
Insulin activates the sodium–potassium ATPase pump, increasing the movement of potassium
from the extracellular fluid into the intracellular fluid, resulting in hypokalemia. In hyperglycemia, hypokalemia can also result from excessive urine loss of potassium. The chloride level is normal. The calcium and sodium levels are slightly low, but this would not be related to hyperglycemia and insulin administration.
A nurse teaches a client with diabetes mellitus about sick-day management. Which statement would the nurse include in this client’s teaching?
A. “When ill, avoid eating or drinking to reduce vomiting and diarrhea.”
B. “Monitor your blood glucose levels at least every 4 hours while sick.”
C. “If vomiting, do not use insulin or take your oral antidiabetic agent.”
D. “Try to continue your prescribed exercise regimen even if you are sick.”
B
When ill, the client should monitor his or her blood glucose at least every 4 hours. The client should continue taking the medication regimen while ill. The client should continue to eat and drink as tolerated but should not exercise while sick.
A nurse assesses a client who has diabetes mellitus and notes that the client is awake and alert, but shaky, diaphoretic, and weak. Five minutes after administering a half-cup (120 mL) of orange juice, the client’s signs and symptoms have not changed. What action would the nurse take next?
A. Administer another half-cup (120 mL) of orange juice.
B. Administer a half-ampule of dextrose 50% intravenously.
C. Administer 10 units of regular insulin subcutaneously.
D. Administer 1 mg of glucagon intramuscularly.
A
This patient is experiencing mild hypoglycemia. For mild hypoglycemic manifestations, the nurse would administer oral glucose in the form of orange juice. If the symptoms do not resolve immediately, the treatment would be repeated. The patient does not need intravenous dextrose, insulin, or glucagon.
A nurse develops a dietary plan for a client with diabetes mellitus and new-onset microalbuminuria. Which component of the client’s diet would the nurse decrease?
A. Carbohydrates
B. Proteins
C. Fats
D. Total calories
B
Restriction of dietary protein is recommended for clients with microalbuminuria to delay progression to renal failure. The client’s diet does not need to be decreased in carbohydrates, fats, or total calories.
A nurse assesses a client with diabetes mellitus. Which assessment finding would alert the nurse to decreased kidney function in this client?
A. Urine specific gravity of 1.033
B. Presence of protein in the urine
C. Elevated capillary blood glucose level
D. Presence of ketone bodies in the urine
B
Renal dysfunction often occurs in the client with diabetes. Proteinuria is a result of renal dysfunction. Specific gravity is elevated with dehydration. Elevated capillary blood glucose levels and ketones in the urine are consistent with diabetes mellitus but are not specific to renal function.
A nurse assesses a client who has diabetes mellitus. Which arterial blood gas values would the nurse identify as potential ketoacidosis in this client?
A. pH 7.38, HCO3 22 mEq/L (22 mmol/L), PCO2 38 mm Hg, PO2 98 mm Hg
B. pH 7.28, HCO3 18 mEq/L (18 mmol/L), PCO2 28 mm Hg, PO2 98 mm Hg
C. pH 7.48, HCO3 28 mEq/L (28 mmol/L), PCO2 38 mm Hg, PO2 98 mm Hg
D. pH 7.32, HCO3 22 mEq/L (22 mmol/L), PCO2 58 mm Hg, PO2 88 mm Hg
B
When the lungs can no longer offset acidosis, the pH decreases to below normal. A client who has diabetic ketoacidosis would present with arterial blood gas values that show primary metabolic acidosis with decreased bicarbonate levels and a compensatory respiratory alkalosis with decreased carbon dioxide levels.
A nurse cares for a client experiencing diabetic ketoacidosis who presents with Kussmaul respirations. What action would the nurse take?
A. Administration of oxygen via facemask
B. Intravenous administration of 10% glucose
C. Implementation of seizure precautions
D. Administration of intravenous insulin
D
The rapid, deep respiratory efforts of Kussmaul respirations are the body’s attempt to reduce the acids produced by using fat rather than glucose for fuel. Only the administration of insulin will reduce this type of respiration by assisting glucose to move into cells and to be used for fuel instead of fat. The patient who is in ketoacidosis may not experience any respiratory impairment and therefore does not need additional oxygen. Giving the patient glucose would be contraindicated. The patient does not require seizure precautions.
The nurse assesses a client with diabetic ketoacidosis. Which assessment finding would the nurse correlate with this condition?
A. Increased rate and depth of respiration
B. Extremity tremors followed by seizure activity
C. Oral temperature of 102° F (38.9° C)
D. Severe orthostatic hypotension
A
Ketoacidosis decreases the pH of the blood, stimulating the respiratory control areas of the brain to buffer the effects of increasing acidosis. The rate and depth of respiration are increased (Kussmaul respirations) in an attempt to excrete more acids by exhalation. Tremors, elevated temperature, and orthostatic hypotension are not associated with ketoacidosis.
A nurse cares for a patient who is prescribed pioglitazone. After 6 months of therapy, the client reports that he has a new onset of ankle edema. What assessment question would the nurse take?
A. “Have you gained unexpected weight this week?”
B. “Has your urinary output declined recently?”
C. “Have you had fever and achiness this week?”
D. “Have you had abdominal pain recently?”
A
Thiazolidinediones (including pioglitazone) can cause cardiovascular adverse effects including health failure which is manifested by peripheral edema and unintentional weight gain. The client should have been taught to weigh every week and report sudden increases in weight.
A nurse asks the staff development nurse what “apoptosis” means. What response best?
A. Growth by cells enlarging
B. Having the normal number of chromosomes
C. Inhibition of cell growth
D. Programmed cell death
D
Apoptosis is programmed cell death. With this characteristic, organs and tissues function with cells that are at their peak of performance. Growth by cells enlarging is hyperplasia. Having the normal number of chromosomes is euploidy. Inhibition of cell growth is contact inhibition.
A nurse is learning the difference between normal cells and benign tumor cells. What information does this include?
A. Benign tumors grow through invasion of other tissue.
B. Benign tumors have lost their cellular regulation from contact inhibition.
C. Growing in the wrong place or time is typical of benign tumors.
D. The loss of characteristics of the parent cells is called anaplasia.
C
Benign tumors are basically normal cells growing in the wrong place or at the wrong time. Benign cells grow through hyperplasia, not invasion. Benign tumor cells retain contact inhibition. Anaplasia is a characteristic of cancer cells.
A nurse learns that which of the following is the single biggest risk factor for developing cancer?
A. Exposure to tobacco
B. Advancing age
C. Occupational chemicals
D. Oncovirus infection
B
The single biggest risk factor for developing cancer is advancing age. As one ages, immunity decreases, and exposures increase. Tobacco use is the single most preventable cause of cancer. Exposure to chemicals and oncoviruses cause fewer cancers.
Which statement about carcinogenesis is accurate?
A. An initiated cell will always become clinical cancer.
B. Cancer becomes a health problem once it is 1 cm in size.
C. Normal hormones and proteins do not promote cancer growth.
D. Tumor cells need to develop their own blood supply.
D
Tumors need to develop their own blood supply through a process called angiogenesis. An initiated cell needs a promoter to continue its malignant path. Normal hormones and proteins in the body can act as promoters. A 1-cm tumor is a detectable size, but other events have to occur for it to become a health problem.
The nurse caring for oncology clients knows that which form of metastasis is the most common?
A. Bloodborne
B. Direct invasion
C. Lymphatic spread
D. Via bone marrow
A
Bloodborne metastasis is the most common way for cancer to metastasize. Direct invasion and lymphatic spread are other methods. Bone marrow is not a medium in which cancer spreads, although cancer can occur in the bone marrow.
A nurse is assessing a client with glioblastoma. What assessment is most important?
A. Abdominal palpation
B. Abdominal percussion
C.Lung auscultation
D. Neurologic examination
D
A glioblastoma arises in the brain. The most important assessment for this client is the neurologic examination.
A nurse has taught a client about dietary changes that can reduce the chances of developing cancer. What statement by the client indicates the nurse needs to provide additional teaching?
A. “Foods high in vitamin A and vitamin C are important.
B. “I’ll have to cut down on the amount of bacon I eat.”
C. “I’m so glad I don’t have to give up my juicy steaks.”
D. “Vegetables, fruit, and high-fiber grains are important.”
C
To decrease the risk of developing cancer, one should cut down on the consumption of red meats and animal fat. The other statements are correct.
A client is in the oncology clinic for a first visit since being diagnosed with cancer. The nurse reads in the client’s chart that the cancer classification is TISN0M0. What does the nurse conclude about this client’s cancer?
A. The primary site of the cancer cannot be determined.
B. Regional lymph nodes could not be assessed.
C. There are multiple lymph nodes involved already.
D. There are no distant metastases noted in the report.
D
TIS stands for carcinoma in situ; N0 stands for no regional lymph node metastasis; and M0 stands for no distant metastasis.
A client asks the nurse if eating only preservative- and dye-free foods will decrease cancer risk. What response by the nurse is best?
A. “Maybe; preservatives, dyes, and preparation methods may be risk factors.”
B. “No; research studies have never shown those things to cause cancer.”
C. “There are other things you can do that will more effectively lower your risk.”
D. “Yes; preservatives and dyes are well known to be carcinogens.”
A
Dietary factors related to cancer development are poorly understood, although dietary practices are suspected to alter cancer risk. Suspected dietary risk factors include low-fiber intake and a high intake of red meat or animal fat. Preservatives, preparation methods, and additives (dyes, flavorings, sweeteners) may have cancer-promoting effects. It is correct to say that other things can lower risk more effectively, but this does not give the client concrete information about how to do so, and also does not answer the client’s question.
The nurse working with oncology clients understands that interacting factors affect cancer development. Which factors does this include? (Select all that apply.
A. Exposure to carcinogens
B. Genetic predisposition
C. Immune function
D. Normal doubling time
E. State of euploidy
A, B, C
The three interacting factors needed for cancer development are exposure to carcinogens, genetic predisposition, and immune function.
A nurse is providing community education on the seven warning signs of cancer. Which signs are included? (Select all that apply.)
A. A sore that does not heal
B. Changes in menstrual patterns
C. Indigestion or trouble swallowing
D. Near-daily abdominal pain
E. Obvious change in a mole
F. Frequent indigestion
A, B, C, E, F
The seven warning signs for cancer can be remembered with the acronym CAUTION:
changes in bowel or bladder habits, a sore that does not heal, unusual bleeding or discharge, thickening or lump in the breast or elsewhere, indigestion or difficulty swallowing, obvious change in a wart or mole, and nagging cough or hoarseness. Abdominal pain is not a warning sign.
A nurse in the oncology clinic is providing preoperative education to a client just diagnosed with cancer. The client has been scheduled for surgery in 3 days. What action by the nurse is best?
A. Call the client at home the next day to review teaching.
B. Give the client information about a cancer support group.
C. Provide all the preoperative instructions in writing.
D. Reassure the client that surgery will be over soon.
A
Clients are often overwhelmed at a sudden diagnosis of cancer and may be more overwhelmed at the idea of a major operation so soon. This stress significantly impacts the client’s ability to understand, retain, and recall information. The nurse would call the client at home the next day to review the teaching and to answer questions. The client may or may not be ready to investigate a support group, but this does not help with teaching. Giving information in writing is important (if the client can read it), but in itself will not be enough. Telling the client that surgery will be over soon is giving false reassurance and does nothing for teaching.
A nurse is caring for a client admitted for Non-Hodgkin’s lymphoma and chemotherapy. The client reports nausea, flank pain, and muscle cramps. What action by the nurse is most important?
A. Request an order for serum electrolytes and uric acid.
B. Increase the client’s IV infusion rate.
C. Instruct assistive personnel to strain all urine.
D. Administer an IV antiemetic.
A
This client’s reports are consistent with tumor lysis syndrome, for which he or she is at risk due to the diagnosis. Early symptoms of TLS stem from electrolyte imbalances and can include lethargy, nausea, vomiting, anorexia, flank pain, muscle weakness, cramps, seizures, and altered mental status. The nurse would notify the primary health care provider and request an order for serum electrolytes. Hydration is important in both preventing and managing this syndrome, but the nurse would not just increase the IV rate. Assistive personnel may need to strain the client’s urine and the client may need an antiemetic, but first the nurse would assess the situation further by obtaining pertinent lab tests.
A new nurse has been assigned a client who is in the hospital to receive iodine-131 treatment. Which action by the nurse is best?
A. Ensure the client is placed in protective isolation.
B. Have pregnant visitors stay 6 feet from the client
C. No special action is necessary to care for this client.
D. Read the policy on handling radioactive excreta.
D
This type of radioisotope is excreted in body fluids and excreta (urine and feces) and would not be handled directly. The nurse would read the facility’s policy for handling and disposing of this type of waste. The other actions are not warranted.
A client in the oncology clinic reports her family is frustrated at her ongoing fatigue 4 months after radiation therapy for breast cancer. What response by the nurse is most appropriate?
A. “Are you getting adequate rest and sleep each day?”
B. “It is normal to be fatigued even for months afterward.”
C. “This is not normal and I’ll let the primary health care provider know.”
D. “Try adding more vitamins B and C to your diet.”
B
Radiation-induced fatigue can be debilitating and may last for months after treatment has ended. Rest and adequate nutrition can affect fatigue, but it is most important that the client (and family) understands this is normal.
A client tells the oncology nurse about an upcoming vacation to the beach to celebrate completing radiation treatments for cancer. What response by the nurse is most appropriate?
A. “Avoid getting salt water on the radiation site.”
B. “Do not expose the radiation area to direct sunlight.”
C. “Have a wonderful time and enjoy your vacation!”
D. “Remember you should not drink alcohol for a year.”
B
The skin overlying the radiation site is extremely sensitive to sunlight after radiation therapy has been completed. The nurse would inform the client to avoid sun exposure to this area. This advice continues for 1 year after treatment has been completed. The other statements are not appropriate.
A client is receiving chemotherapy through a peripheral IV line. What action by the nurse is most important?
A. Assessing the IV site and blood return every hour
B. Educating the client on side effects
C. Monitoring the client for nausea
D. Providing warm packs for comfort
A
Intravenous chemotherapy can cause local tissue destruction if it extravasates into the surrounding tissues. Peripheral IV lines are more prone to this than centrally placed lines. The most important intervention is prevention, so the nurse would check hourly to ensure the IV site is patent, or frequently depending on facility policy. Education and monitoring for side effects such as nausea are important for all clients receiving chemotherapy. Warm packs may be helpful for some drugs, whereas for others ice is more comfortable. would monitor the site and check for blood return to prevent injury from infiltration or extravasation.
A client with cancer is admitted to a short-term rehabilitation facility. The nurse prepares to administer the client’s oral chemotherapy medications. What action by the nurse is most appropriate?
A. Crush the medications if the client cannot swallow them.
B. Give one medication at a time with a full glass of water.
C. No special precautions are needed for these medications.
D. Wear personal protective equipment when handling the medications.
D
During the administration of oral chemotherapy agents, nurses must take the same precautions that are used when administering IV chemotherapy. This includes using personal protective equipment. These medications cannot be crushed, split, or chewed. Giving one at a time is not needed.
The nurse working with oncology clients understands that which age-related change increases the older client’s susceptibility to infection during chemotherapy?
A. Decreased immune function
B. Diminished nutritional stores
C. Existing cognitive deficits
D. Poor physical reserves
A
As people age, there is an age-related decrease in immune function, causing the older adult to be more susceptible to infection than other clients. Not all older adults have diminished nutritional stores, cognitive dysfunction, or poor physical reserves.
The nurse has educated a client on precautions to take with thrombocytopenia. What statement by the client indicates a need to review the information?
A. “I will be careful if I need enemas for constipation.”
B. “I will use an electric shaver instead of a razor.”
C. “I should only eat soft food that is either cool or warm.”
D. “I won’t be able to play sports with my grandkids.”
A
The thrombocytopenic client is at high risk for bleeding even from minor trauma. Due to the risk of injuring rectal and anal tissue, the client should not use enemas or rectal thermometers. This statement would indicate the client needs more information. The other statements are appropriate for the thrombocytopenic client.
A nurse works with clients who have alopecia from chemotherapy. What action by the nurse takes priority?
A. Helping clients adjust to their appearance
B. Reassuring clients that this change is temporary
C. Referring clients to a reputable wig shop
D. Teaching measures to prevent scalp injury
D
All of the actions are appropriate for clients with alopecia. However, the priority is client safety, so the nurse would first teach ways to prevent scalp injury.
A client is receiving rituximab. What assessment by the nurse takes priority?
A. Blood pressure
B. Temperature
C. Oral mucous membranes
D. Pain
A
Rituximab can cause infusion-related reactions, including hypotension, so monitoring blood pressure is the priority. Other complications of this drug include fever with chills/rigors, headache and abdominal pain, shortness of breath, bronchospasm, nausea and vomiting, and rash. Assessing the client’s temperature and for pain are both pertinent assessments, but do not take priority over the blood pressure. Oral mucus membrane assessment is important for clients with cancer.
A nurse is assessing a female client who is taking hormone therapy for breast cancer. What assessment finding requires the nurse to notify the primary health care provider immediately?
A. Irregular menses
B. Edema in the lower extremities
C. Ongoing breast tenderness
D. Red, warm, swollen calf
D
Clients receiving hormone therapy are at risk for thromboembolism. A red, warm, swollen calf is indicative of deep vein thrombosis and would be reported to the provider. Irregular menses, edema in the lower extremities, and breast tenderness are not as urgent as the possible thromboembolism.
A client with a history of prostate cancer is in the clinic and reports new onset of severe low back pain. What action by the nurse is most important?
A. Assess the client’s gait and balance.
B. Ask the client about the ease of urine flow.
C. Document the report completely.
D. Inquire about the client’s job risks.
A
This client has symptoms of spinal cord compression, which can be seen with prostate cancer. This may affect both gait and balance and urinary function. For client safety, assessing gait and balance is most important. Documentation would be complete. The client may or may not have occupational risks for low back pain, but with his history of prostate cancer, this would not be where the nurse starts investigating.
The nurse has taught a client with cancer ways to prevent infection. What statement by the client indicates that more teaching is needed?
A. “I should take my temperature daily and when I don’t feel well.”
B. “I will discard perishable liquids after sitting out for over an hour.”
C. “I won’t let anyone share any of my personal toiletries.”
D. “It’s alright for me to keep my pets and change the litter box.”
D
Clients should wash their hands after touching their pets and would not empty or scoop the cat litter box. The other statements are appropriate for self-management.
A client is admitted with superior vena cava syndrome. What action by the nurse is most appropriate?
A. Administer a dose of allopurinol.
B. Assess the client’s serum potassium level.
C. Gently inquire about advance directives.
D. Prepare the client for emergency surgery.
C
Superior vena cava syndrome is often a late-stage manifestation. After the client is stabilized and comfortable, the nurse would initiate a conversation about advance directives. Allopurinol is used for tumor lysis syndrome. Potassium levels are important in tumor lysis syndrome, in which cell destruction leads to large quantities of potassium being released into the bloodstream. Surgery is rarely done for superior vena cava syndrome.
A client’s family members are concerned that telling the client about a new finding of cancer will cause extreme emotional distress. They approach the nurse and ask if this can be kept from the client. What actions by the nurse are most appropriate? (Select all that apply.)
A. Ask the family to describe their concerns more fuLly.
B. Consult with a social worker, chaplain, or ethics committee.
C. Explain the client’s right to know and ask for their assistance.
D. Have the unit manager take over the care of this client and family.
E. Tell the family that this secret will not be kept from the client.
A, B, C
The client’s right of autonomy means that the client must be fully informed as to his or her diagnosis and treatment options. The nurse cannot ethically keep this information from the client. The nurse can ask the family to explain their concerns more fully so everyone understands them. A social worker, chaplain, or ethics committee can become involved to assist the nurse, client, and family. The nurse would explain the client’s right to know and ask the family how best to proceed. Enlisting their help might reduce their reluctance for the client to be informed. The nurse would not abdicate responsibility for this difficult situation by transferring care to another nurse. Simply telling the family that he or she will not keep this secret sets up an adversarial relationship. Explaining this fact along with the concept of autonomy would be acceptable, but this by itself is not.
A client has thrombocytopenia. What actions does the nurse delegate to assistive personnel
(AP)? (Select all that apply.)
A. Apply the client’s shoes before getting the client out of bed.
B. Assist the client with ambulation.
C. Shave the client with a safety razor only.
D. Use a lift sheet to move the client up in bed.
E. Use a water pressure device be set on low for oral care.
A, B, C , D , E
Clients with thrombocytopenia are at risk of significant bleeding even with minor injuries. The nurse instructs the AP to put the client’s shoes on before getting the client out of bed, assist with ambulation, shave the client with an electric razor, use a lift sheet when needed to reposition the client, and use a soft-bristled toothbrush for oral care. All of these measures help prevent client injury.
A client receiving radiation therapy reports severe skin itching and irritation. What actions does the nurse delegate to assistive personnel (AP)? (Select all that apply.)
A. Apply approved moisturizers to dry skin.
B. Apply steroid creams to the skin.
C. Bathe the client using mild soap.
D. Help the client pat skin dry after a bath.
E. Teach the client to avoid sunlight.
F. Make sure no clothing is rubbing the site.
A, C, D,
The nurse can delegate applying moisturizer approved by the radiation oncologist using mild soap for bathing, and helping the client pat wet skin dry after bathing. Any clothing worn over the site should be soft and not create friction. Steroid creams are not used for this condition. Hot water will worsen the irritation. Client teaching is a nursing function.
The nurse caring for clients who have cancer understands that the general consequences of cancer include which client problems? (Select all that apply.)
A. Clotting abnormalities from thrombocythemia
B. Increased risk of infection from white blood cell deficits
C. Nutritional deficits such as early satiety and cachexia
D. Potential for reduced gas exchange
E. Various motor and sensory deficits
F. Increased risk of bone fractures
A, B, C, D, E, F
The general consequences of cancer include reduced immunity and blood-producing functions, altered GI structure and function, decreased respiratory function, and motor and sensory deficits. Clotting problems often occur due to thrombocytopenia (not enough platelets), not thrombocythemia (too many platelets).

A client in the emergency department reports difficulty breathing. The nurse assesses the client’s appearance as depicted below:
What action by the nurse is most important?
A. Assess blood pressure and pulses
B. Attach the client to a pulse oximeter.
C. Have the client rate his or her pain.
D. Facilitate urgent radiation therapy.
A
This client has superior vena cava syndrome, in which venous return from the head, neck, and trunk is blocked. Decreased cardiac output can occur. The nurse would assess indicators of cardiac output, including blood pressure and pulse, as the priority. The other actions are also appropriate but are not as important. The ED nurse may or may not be able to facilitate radiation therapy.
A client with cancer has anorexia and mucositis and is losing weight. The client’s family members continually bring favorite foods to the client and are distressed when the client won’t eat them. What action by the nurse is best?
A. Explain the pathophysiologic reasons behind the client not eating.
B. Help the family show other ways to demonstrate love and caring.
C. Suggest foods and liquids the client might be willing to try to eat.
D. Tell the family the client isn’t able to eat now no matter what they bring.
B
Families often become distressed when their loved ones won’t eat. Providing food is a universal sign of caring, and to some people the refusal to eat signifies worsening of the condition. The best option for the nurse is to help the family find other ways to demonstrate caring and love, because with treatment-related anorexia and mucositis, the client is not likely to eat anything right now. Explaining the rationale for the problem is a good idea but does not suggest to the family anything that they can do for the client. Simply telling the family the client is not able to eat does not give them useful information and is dismissive of their concerns.
A nurse works on an oncology unit and delegates personal hygiene to assistive personnel (AP). What action by the AP requires intervention from the nurse?
A. Allowing a very tired client to skip oral hygiene and sleep
B. Assisting clients with washing the perianal area every 12 hours
C. Helping the client use a soft-bristled toothbrush for oral care
D. Reminding the client to rinse the mouth with water or saline
A
Even though clients may be tired, they still need to participate in hygiene to help prevent infection. The nurse would intervene and explain this to AP. The other options are all appropriate.