KAAP310: The Urinary System
what is the main function of the kidneys (general)
major excretory organ, maintain the body's internal environment
how do the kidneys maintain the body's internal environment
regulating total water volume and total solute concentration in water, regulating ion concentrations in ECF, ensuring long-term acid base balance, excreting metabolic wastes, toxins, drugs, producing erythropoietin and renin (regulate RBC production and BP respectively), activating vitamin D, and carrying out gluconeogenesis if needed
what does the urinary system include
kidneys, ureters, urinary bladder, urethra
transport urine from kidneys to urinary bladder
ureters
temporary storage reservoir for urine
urinary bladder
transports urine out of the body
urethra
location of the kidneys
retroperitoneal, in the superior lumbar region
why is the right kidney lower than the left kidney
the right kidney is crowded by the liver
where are the adrenal (suprarenal) glands
sitting atop each kidney
which part of the kidney is convex and which is concave
convex lateral surface; concave medial surface with vertical renal hilum
leads to internal space of the kidneys, renal sinus - ureters, renal blood vessels, lymphatics, and nerves enter and exit here
renal hilum
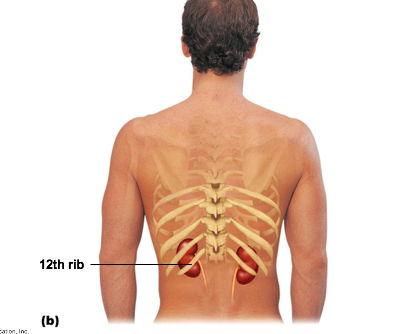
posterior view of the kidneys in relation to ribs
what are the 3 supportive tissue layers surrounding the kidneys
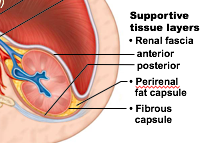
renal fascia (anterior and posterior), perirenal fat capsule, fibrous capsule
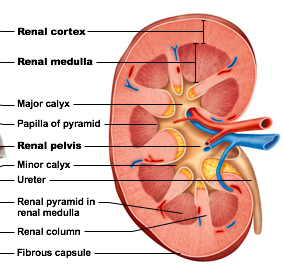
what are the three distinct regions of the internal kidney
renal cortex, renal medulla, renal pelvis
granular appearing superficial region
renal cortex
deep to cortex, composed of cone shaped medullary (renal) pyramids
renal medulla
what are the medullary (renal) pyramids structured like
broad base of pyramid faces cortex, papilla (tip of pyramid) points internally, renal pyramids are separated by renal columns, inward extensions of cortical tissue, lobe - medullary pyramid and its surrounding cortical tissue; about 8 lobes per kidney
funnel-shaped tube continuous with ureter
renal pelvis
what does the renal pelvis have
minor calyces, major calyces
cup shaped areas that collect urine draining from pyramid papillae
minor calyces of renal pelvis
areas that collect urine from minor calyces, empty urine into renal pelvis
major calyces of renal pelvis
urine flow goes from what to what
renal pyramid -> minor calyx -> major calyx -> renal pelvis -> ureter
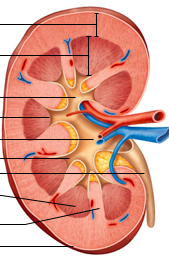
label the renal cortex, renal medulla, major calyx, papilla of pyramid, renal pelvis, minor calyx, ureter, renal pyramid in renal medulla
homeostatic imbalance: infection of renal pelvis and calyces
pyelitis
homeostatic imbalance: infection or inflammation of entire kidney, severe cases can cause swelling of kidney and abscess formation, and pus may fill renal pelvis
pyelonephritis
pyelonephritis infections in females are usually caused by what
fecal bacteria entering urinary tract
how are kidneys and blood related
kidneys cleanse blood and adjust its composition, so it has a rich blood supply
what delivers about 1/4 of cardiac output to kidneys each minute
renal arteries
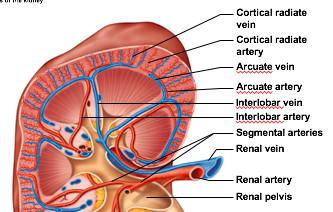
arterial flow:
rena -> segmental -> interlobar -> arcuate -> cortical radiate (interlobular)
venous flow:
cortical radiate -> arcuate -> interlobar -> renal veins (no segmental veins)
nerve supply
via sympathetic fibers from renal plexus
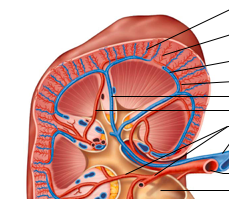
label the following: cortical radiate vein, cortical radiate artery, arcuate vein, arcuate artery, interlobar vein, interlobar artery, segmental arteries, renal vein, renal artery
structural and functional units that form urine
nephrons, more than 1 million nephrons per kidney
two main parts of the nephron
renal corpuscle, renal tubule
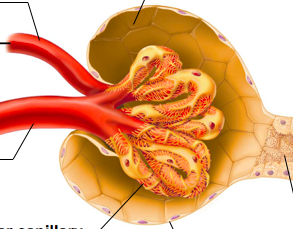
what are the two main parts of the renal corpuscle
glomerulus, glomerular capsule
tuft of capillaries composed of fenestrated endothelium - highly porous capillaries, allows for efficient filtrate formation
glomerulus
plasma-derived fluid that renal tubules process to form urine
filtrate
what is also called the bowmans capsule
glomerular capsule
cup shaped, hollow structure surrounding glomerulus
glomerular capsule
two layers of the glomerular capsule
parietal layer and visceral layer
which layer is simple squamous epithelium
parietal layer
which layer clings to glomerular capillaries; branding epithelial podocytes
visceral layer
extensions terminate in foot processes that cling to basement membrane, filtrate slits between foot processes allow filtrate to pass into capsular space
podocytes
3 cm long, consists of single layer of epithelial cells, but each region has its own unique histology and function
renal tubule
what are the three major parts of the renal tubule
proximal convoluted tubule, nephron loop, distal convoluted tubule
where does that distal convoluted tubule drain into
collecting duct
cuboidal cells with dense microvilli that form brush border (increases surface area, have large mitochondria), functions in reabsorption and secretion, confined to cortex
proximal convoluted tubule (PCT)
formerly called loop of henle, U shaped structure consisting of two limbs - descending and ascending
nephron loop
proximal part is continuous with proximal tubule, distal portion also called descending thin limb, simple squamous epithelium
descending limb
thick (but can be thin in some nephrons), cuboidal or columnar cells
ascending limb
cuboidal cells with very few microvilli, function more in secretion than reabsorption, confined to cortex
distal convoluted tubule (DCT)
receive filtrate from many nephrons, run through medullary pyramids, fuse together to deliver urine through papillae into minor calyces
collecting ducts
what are the two major groups of nephrons
cortical and juxtamedullary
make up 85% of nephrons, almost entirely in cortex
cortical nephrons
long nephron loops deeply invade medulla, ascending limbs have thick and thin segments, important in production of concentrated urine
juxtamedullary nephrons
renal tubules are associated with what two capillary beds
glomerulus, peritubular capillaries ... juxtamedullary nephrons are associated with vasa recta
capillaries are specialized for filtration, different from other capillary beds because they are fed and drained by arteriole
glomerulus
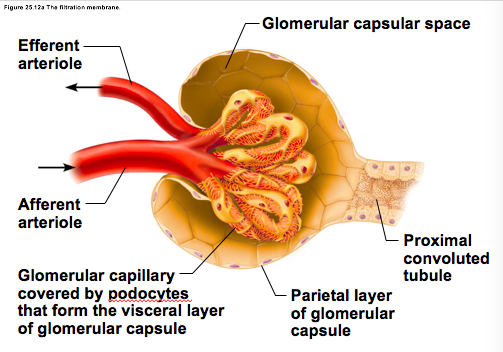
enters glomerulus, arises from cortical radiate arteries
afferent arteriole
leaves glomerlus, feed into either peritubular capillaries or vasa recta
efferent arteriole
why is BP high in glomerulus
afferent arterioles are larger in diameter than efferent arterioles, arterioles are high resistance vessels
around the proximal and distal convoluted tubules, water and many solutes moves from tubules into peritubular capillaries; some solutes (not water) move from peritubular caps into tubules
peritubular capillaries
long, thin walled vessels parallel to long nephron loops of juxtamedullary nephrons, function in formation of concentrated urine
vasa recta
each nephron has 1, involves modified portions of distal portion of ascending limb of nephron loop and afferent (sometimes efferent) arteriole; important in regulating rate of filtrate formation and BP
juxtalomerular complex (JGC)
what are the three things that JGC includes
macula densa, granular cells (JG cells), extraglomerular mesangial cells
cells contain chemoreceptors that sense NaCl content of filtrate
macula densa
enlarged, smooth muscle cells of arteriole, act as mechanoreceptors to sense BP in afferent arteriole
granular cells (Juxtaglomerular or JG cells)
may pass signals between macula densa and granular cells
extraglomerular mesangial cells
how many L of fluid is processed daily in the kidney
180 L
how many L of urine is formed daily
1.5 L
how many times per day do the kidneys filter the bodys entire plasma volume
60 times
at rest, what % of oxygen used by the body is consumed by the kidneys
20-25%
what is filtrate (produced by glomerular filtration) composed of
blood plasma minus proteins
what is urine
<1% of original filtrate, contains metabolic wastes and unneeded substances
what are the 3 processes involved in urine formation and adjustment of blood composition
1. glomerular filtration. 2. tubular reabsorption. 3. tubular secretion
produces cell- and protein- free filtrate
glomerular filtration
selectively returns 99% of substances from filtrate to blood in renal tubules and collecting ducts
tubular reabsorption
selectively moves substances from blood to filtrate in renal tubules and collecting ducts
tubular secretion
a passive process (no metabolic energy required), hydrostatic pressure forces fluids and solutes through filtration membrane into glomerular capsule, no reabsorption into capillaries of glomerulus occurs
glomerular filtration
porous membrane between blood and interior of glomerular capsule, allows water and solutes smaller than plasma proteins to pass (normally no cells can pass)
the filtration membrane
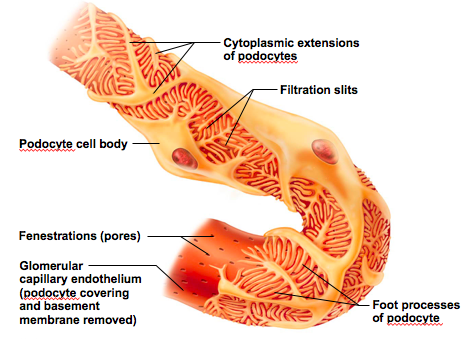
what are the three layers of the filtration membrane
fenestrated endothelium of glomerular capillaries, basement membrane, foot processes of podocytes
fused basal laminae of two other layers
basement membrane
which layer of the filtration membrane has filtration slits? Slit diaphragms repel macromolecules
foot processes of podocytes
label the following: efferent arteriole, afferent arteriole, glomerular capsular space, proximal convoluted tubule, parietal layer of glomerular capsule, glomerular capillary covered by podocytes that form the visceral layer of glomerular capsule
label the following: cytoplasmic extensions of podocytes, filtration slits, podocyle cell body, fenestratons (pores), glomerular capillary endothelium, foot processes of podocyte
forces that promote filtrate formation, hydrostatic pressure in glom capillaries is essentially glom BP
outward pressures
forces inhibiting filtrate formation, hydrostatic pressure in capsular space, colloid osmotic pressure in capillaries
inward pressures
sum of forces, pressure responsible for filtrate formation, main controllable factor determining GFR
net filtration pressure NFP
NFP equation
(HPgc)-(HPcs+OPgc)
outward-inward pressures
volume of filtrate formed per minute by both kidneys (normal is 120-125ml/min)
GFR
GFR is directly proportional to:
NFP, total surface area available for filtration, filtration membrane permeability
how does GFR affect systemic BP
increased GFR causes inc urine output, which lowers BP