Chapter 6
Chapter 6:
Bones and skeletal tissue
Skeletal System:
1. Composed of bones, cartilages, ligaments and tendons
2. A BONE is considered an organ
A. composed of different tissues: bone (or osseus tissue), cartilage, dense connective tissue, adipose tissue, epithelium and nervous tissue
B. It is initially made of cartilage which is then mostly replaced by bone
C. Continuously being remodelled by construction and breaking down of bone tissue
1ST Function of Bone and Skeletal System:
1. Supports the body
A. Supports soft tissues
B. Provides attachment points for tendons of skeletal
muscle
2ND Function of Bone and Skeletal System:
1. Protects important internal organs
A. Cranium protects brain
B. Vertebrae protect spinal cord
C. Ribs protect lungs and heart
3RD Function of Bone and Skeletal System:
1. Assistance in Movement
A. Skeletal muscle attaches to bones
a. Skeletal muscle contraction pulls on bones producing movement (voluntary movement)
Mineral Homeostasis:
1. Bone tissue store several minerals
A. Acts to serve as a reservoir of critical minerals
***Calcium (99% of body’s content)
***Phosphorus
Blood Cell Production (Hemopoesis):
Red bone marrow produces Red blood cells, White blood
Triglyceride Storage:
1. Yellow bone marrow
2. Triglycerides stored in adipose cells: serves as a potential chemical energy reserve
Bones in Human skeleton:
206 named bones
Bones of the skeleton are grouped into two principal divisions:
1. Axial skeleton
2. Appendicular skeleton
Axial skeleton:
Bones along the longitudinal axis of the human body
A.Skull bones, auditory ossicles (ear bones), hyoid bone, thorax (sternum, ribs), and bones of the vertebral column
Appendicular skeleton :
Bones of the upper and lower limbs (extremities)
A. Bones forming the pectoral and pelvic girdles that connect the limbs to the axial skeleton
Long Bones:
Greater length than width, slightly curved for strength
******Femur, tibia, fibula, humerus, ulna, radius, phalanges
Short bones:
Cube-shaped
***Carpal, tarsal
Flat bones:
Thin, two parallel plates of compact bone tissue enclosing spongy bone tissue
*****Cranial, sternum, ribs, scapulae
Irregular bones:
Complex shapes that cannot be grouped into any of the previous categories
****Vertebrae, hip bones, some facial bones, calcaneus
Sesamoid bones:
Protect tendons from excessive wear and tear
***Patellae, foot, hand
Sutural bones:
Small bones located in sutures of cranial bones
Surface markings:
Structural features adapted for specific functions
Two major types of surface markings:
1. Depressions and openings
2. Projections/Processes
Depressions and openings:
1. Allow the passage of blood vessels and nerves
2. Form joints
Projections/Processes:
1. Projections or outgrowths that form joints
2. Serve as attachment points for ligaments and tendons
Diaphysis:
Shaft
Epiphysis :
distal and proximal ends
Metaphysis:
Epiphyseal growth plate (hyaline cartila)
Articular cartilage:
Hyaline cartilage
Periosteum:
1.Membrane surrounding bone
A. Protection, innervated, vascularized
B. Bone growth in thickness (osteogenic cells, osteoblasts, osteclasts)
C.Attachment for ligaments
Medullary cavity:
yellow marrow
Epiphyseal line:
membrane lining canals and trabeculae (osteoblasts, osteoclasts)
Type of cells:
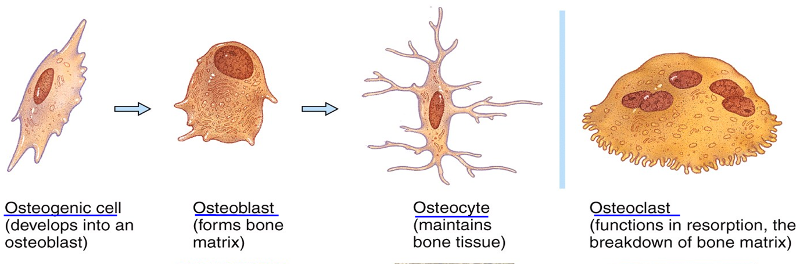
Osteogenic cells
osteoblasts
osteocytes
osteoclasts
Extracellular surrounding widely separated cells:
Matrix
- 25% water
- 25% collagen fibers
- 50% crystallized mineral salts
- Calcium phosphate (“hydroxyapatite”)– most abundant chemical compound
How Many Types Of Cells In Bone Tissue:
Four
Osteogenic cells:
1. Undergo cell division
2. Resulting cells develop into osteoblasts
Osteoblasts:
"Bone-building cells"
- Synthesize extracellular matrix of bone tissue: collagen fibers and initiate calcification
Osteocytes:
1. Mature bone cells, “trapped” in mineralized extracellular matrix
2. Maintain the bone matrix: exchange nutrients and wastes with the blood (spider shaped)
Osteoclasts:
1. Release enzymes and acids that digest the protein and mineral components of bone matrix (resorption)
2. Huge cells: derive from fusion of up to 50 monocytes; located on the Endosteum
3. Regulate blood calcium level
Two Bone Categories:
1. Compact
2. Spongy
Compact Bone:
(80% of skeleton)
1. Strongest form of bone tissue
2. External
3. Provides protection and support
-----------------------------------------
Compact Bone PART 2:
1. Resists the stresses produced by weight and movement
2. Components arranged in repeating structural units called osteons or Haversian systems
3. Osteons consist of a central (Haversian) canal with concentrically arranged lamellae, lacunae, osteocytes, and canaliculi
Spongy Bone:
1. Internal to Compact bone
2. Consists of lamellae arranged in an irregular lattice of thin columns
3. Columns called trabeculae
(yellow or red bone marrow)
Spongy Bone PART 2:
1. Lacks osteons
2. Lamellae are arranged columns called trabeculae
3. Spaces between the trabeculae make bones lighter
4. Trabeculae of spongy bone support and protect the red bone marrow
5. Hemopoiesis (blood cell production) occurs in spongy bone
6. Trabecula contain lacunae that contain osteocytes
7. Interior bone tissue is made up primarily of spongy bone
Osteon:
1. Canals tha run through bones
2. surrounded by concentric lamellae
3. between lamellae are lucanae which have osteocytes
4. canaliculi come fom lucanae
& is filled with extracellular fluid
5. Canaliculi connect lacunae provides path for nutrients and oxygen
Ossification / osteogenesis:
Bone Formatic
- Initiated by bone-building cells called osteoblasts
- Connective tissue or cartilage are replaced by bone tissue
Bone formation occurs in four situations:
- Formation of bone in an embryo
- Growth of bones until adulthood
- Remodeling of bone
- Repair of fractures
Calciification:
hardening of tissue, occurs during ossification
Bone’s flexibility depends on:
collagen fibers
Two Types Of Ossification:
1. Intramembranous
2. Endochondrial / intracartilaginous
Intramembranous ossification:
direct laying down of bone into the primitive connective tissue (mesenchyme REPLACED by BONE)
*********Connective tissue (=mesenchime) > Bone
(within membranes) LESS COMMON
Endochondrial / intracartilaginous ossification:
(involves chartilage) MORE COMMON
bone develops from hyaline cartilage bone
******Cartilage tissue > Bone
Endochondral ossification/intracartilaginous(prenatal):
1. First osteoblasts appear at Bone collar.
2. Cartilage calcifies and die
> cavities
3. Blood vessels invade cavities and Osteoblasts from periosteum migrate in:
> Primary Ossification Ctr
(SPONGY BONE)
4. Osteoclasts break down spongy bone and leave a Medullary cavity
5. Epiphysis: Secondary Ossification Center (SPONGY BONE)
6. Hyaline cartilage remains only at the articular cartilage and epiphysial plate
Growth in Length (postnatal):
1. Interstitial growth at the epiphyseal plate: chondrocytes keep dividing and secreting ECM at the epiph side
2. Cartilage becomes calcified
3. Osteoclasts dissolve the calcified cartilage and osteoblasts invade the area laying down bone matrix
***At adulthood (age 18-21), the epiphyseal plates close and
bone replaces all the cartilage leaving the epiphyseal line
Growth in Thickness (postnatal):
1. Occurs by appositional growth:
- Bones grow in thickness at the outer surface
- Chondrocytes divide and secrete ECM to the periphery
- Osteoblasts differentiate from the periosteum and secrete bone matrix to the outside
Bone REMODELLING:
1. Adult bone tissue continually renews itself
- Old bone is continually destroyed and new
bone is formed in its place throughout aN individual’s life
- A balance must exist between the actions of osteoclasts (bone resorption) and osteoblasts (bone deposition)
*** 5-7% of our bone mass is recycled
Normal bone metabolism depends on several factors
2 main control loops:
1. Negative feedback that maintains Ca2+
homeostasis in the blood
2. Responses to mechanical and
gravitational forces acting on the
skeleton (life style: exercise vs sedentary) life
Bone’s Role in Calcium Homeostasis:
1. Bone is the body’s major calcium reservoir (99% of total body Ca)
2. Levels of calcium in the blood are maintained by controlling the rates of calcium resorption from bone into blood (osteoclasts) and of calcium deposition from blood into bone (osteoblasts): stable level of 9-11mg Ca/100ml
Parathyroid hormone (PTH):
produced in parathyroid glands
- elevate blood Calcium levels
- Stimulate osteoclasts to resorb bone (increases number and activity)
Calcitonin :
1. secreted by the thyroid gland
- opposes PTH actions, (but NOT very effective)
- lowers only slightly blood calcium levels
- Inhibits osteoclasts and promotes Ca uptake by bone
- Salmon Calcitonin (Miacalcin) used
for osteoporosis
The main mechanical stresses on bone are those that result from the :
pull of skeletal muscles and the pull of gravity.
Minerals:
Large amounts of calcium and phosphorus and smaller amounts of magnesium, fluoride, and manganese are required for bone growth and remodeling
Vitamins:
- Vitamin A: stimulates activity of osteoblasts
- Vitamin C: needed for synthesis of collagen
- Vitamin D: helps build bone by increasing the absorption of calcium from foods in the gastrointestinal tract into the blood
- Vitamins K and B12: needed for synthesis of bone proteins
GH:
Growth Hormone
Giantism:
^^^ GH
Dwarfism:
vvv GH
Acromegaly:
^^^ GH in adulthood
Types Of Fractures:
1. Bone penetrates skin or not
2. Completeness of the break
3. Position of the bone ends after fracture
Bone penetrates skin or not:
- Simple (closed) fracture
- Compound (open) fracture
Completeness of the break:
Complete, incomplete (greenstick)
Position of the bone ends after fracture:
Non displaced, displaced (2 ends not lined up), comminuted (many pieces)
Treatment:
1. Closed reduction: alignment by manipulation
2. Open reduction: surgery: screws, plates, rods, pins
The repair of a bone fracture involves:
1. Formation of fracture hematoma
Blood leaks from the torn ends of blood vessels
2. Fibrocartilaginous callus formation (takes ~3 weeks)
Fibroblasts invade the fracture site and produce collagen fibers which bridge the broken ends of the bone
3. Bony callus formation
Osteoblasts begin to produce spongy bone
4. Bone remodeling
Compact bone replaces spongy bone
Formation of fracture hematoma:
Blood leaks from the torn ends of blood vessels
Fibrocartilaginous callus formation:
Fibroblasts invade the fracture site and produce collagen fibers which bridge the broken ends of the bone (takes ~3 weeks
Bony callus formation:
Osteoblasts begin to produce spongy bone
Bone remodeling
Compact bone replaces spongy bone
Homeostatic imbalances:
Imbalances between bone formation and resorption
can lead to skeletal disorders
Osteomalacia/Rickets:
- adults/children
- occur when bones are inadequately mineralized
- Due to insufficient Vitamin D, or insufficient Ca in the diet (malnutrition)
*****Bowed legs, bone deformities
Paget’s disease:
- Excessive remodelling (bone deposition and resorbtion)
- Abnormally high ratio of spongy to compact bone
Osteoporosis:
- Bones become fragile, bone mass is reduced
- More common in post-menopausal women with decreased estrogen