Microbiology Exam 3 Review - Chapter 10 (Microbial Metabolism) + 23 (GI) Flashcards
Chapter 10
Microbial Metabolism
What is metabolism?
All the chemical reactions and physical workings of the cell.
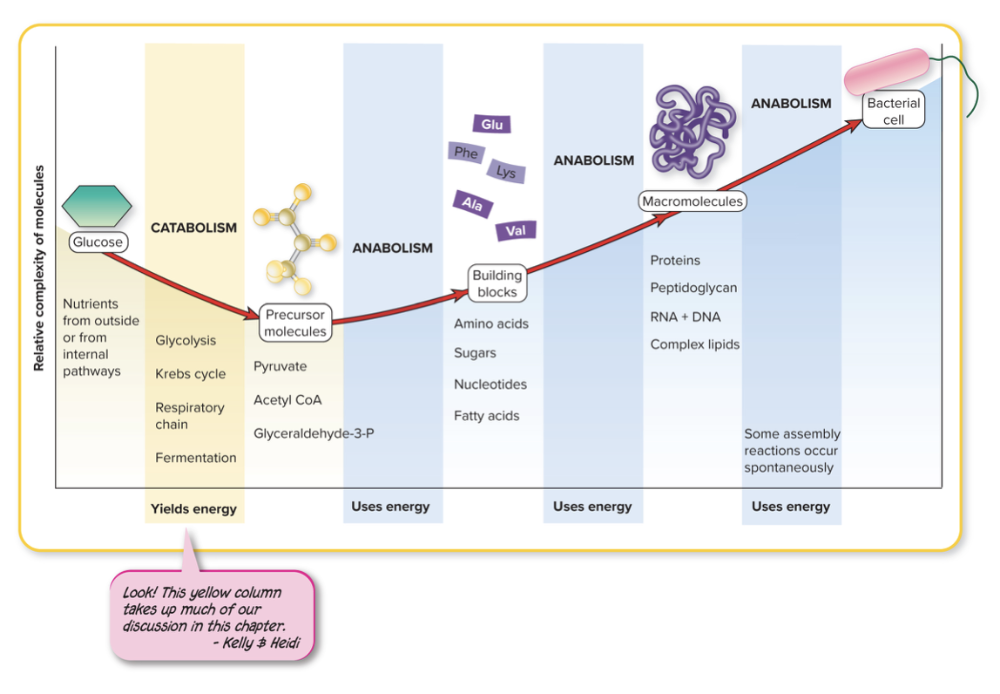
- Anabolic and Catabolic Reactions
- Collects and spends energy in the form of ATP or heat
What is anabolism?
The building of molecules
Biosynthesis: synthesis of cell molecules and structures
REQUIRES energy input
- Assembles smaller molecules into large macromolecules for the cell, utilizing ATP to form bonds (anabolism)
What is catabolism?
The breaking of the bonds of larger molecules
RELEASES energy
- Breaks down macromolecules into smaller molecules, a process that yields energy (catabolism)
What are catalysts?
Speed up the rate of a chemical reaction without becoming part of the products or being consumed in the reaction
How are enzymes catalysts?
Enzymes speed up a chemical reaction by LOWERING the activation energy allowing the reaction to proceed by
- Increasing thermal energy (heating) to increase the velocity of molecules
- Increasing the concentration of reactants to increase the rate of molecular collisions
- Adding a catalyst
What are the basic characteristics for an enzyme?
- Have an active site for target molecules (substrates) - specific
- Are much larger in size than their substrates
- Associate closely with substrates but do not become integrated into the reaction products (do NOT get used up)
- Are not used up or permanently changed by the reaction
- Can be recycled, thus function in extremely low concentrations
- Are greatly affected by temperature and pH (work at optimal temperatures and pH)
- Can be regulated by feedback and genetic mechanisms
How do enzymes work?
A substrate, which is the reactant molecule, binds to the active site of the enzyme and acts accordingly
Enzymes bind to substrate and participate directly in changes to the substrate BUT enzymes DO NOT become part of the product, get used up, or changed and can be RECYCLED
Most enzymes are ________ molecules. What's the difference between simple and conjugated enzymes?
protein
Simple enzymes - protein alone
Conjugated enzymes - contain protein and some other nonprotein molecule
When the protein is whole, meaning it has the nonprotein and protein portion (cofactors) is it called _____
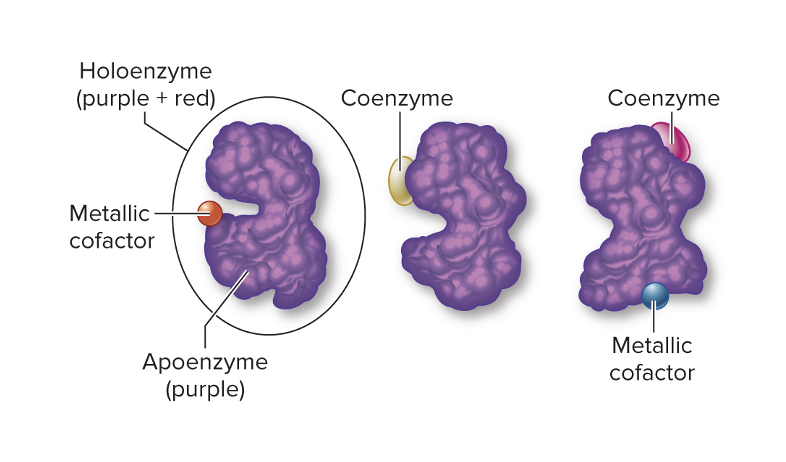
holoenzyme
Only the protein portion of the holoenzyme is called the ______
apoenzyme
The non-protein portion of the holoenzyme is called the ___
Cofactor
This can be an organic molecule (coenzyme) or an inorganic (metal ions)
Apoenzymes are _____
the protein portion of the holoenzyme
This is where the active site or catalytic site resides
- Actual site where substrate binds
- Three-dimensional crevice or groove formed by the way amino acid chains are folded
Each enzyme has a different:
- Primary structure
- Variation in folding
- Unique active site
Cofactors which are part of the non-protein part of the holoenzyme can include ________ and _______
1. Metal ions (metallic cofactors)
- Iron, copper, magnesium, manganese, zinc, cobalt, selenium, and so on.
Assist with precise functions between enzyme and substrate
- Activate enzymes
- Help bring the active site and substrate close together
- Participate directly in chemical reactions
2. Coenzymes (organic compounds)
- Organic compounds that work with the apoenzyme to alter the substrate
- Remove a chemical group from one substrate and add it to another substrate
- Carry and transfer hydrogen atoms, electrons, carbon dioxide, and amino groups
- Vitamins are an important component of coenzymes
- When an enzyme removes a chemical group (like a methyl, acetyl, or phosphate group) from one substrate, the coenzyme temporarily holds that group so it can be added to another substrate. This is crucial because many chemical groups aren’t stable or reactive enough to move on their own. Coenzymes make these transfers efficient, precise, and reversible, allowing metabolic pathways (like glycolysis, the citric acid cycle, or amino acid synthesis) to proceed smoothly. Essentially, they’re the enzyme’s helper molecules that shuttle functional groups safely between reactions.
____________ transfer electrons from one substrate to another, and ______________ transfer a hydrogen from one compound to another
Oxidoreductases (Oxidation is LOSS of elections, a compound that loses electrons is oxidized AND Reduction is gaining electrons and a compound that gains electrons is REDUCED)
**NAD and FAD are coeznyme carriers
dehydrogenases
What are some examples of oxidoreductase enzymes?
1. Lactate dehydrogenase
Substrate: pyruvic acid
Action: Catalyzes the conversion of pyruvic acid to lactic acid
2. Oxidase
Substrate: O2 (molecular oxygen)
Action: Catalyzes the reduction of O2 (addition of electrons and hydrogen)
_________ transfer functional groups from one substrate to another. What is an example?
Transferases
1. DNA Polymerase
Substrate: DNA nucleosides
Action: Synthesizes a strand of DNA using the complementary strand as a model
____________ cleave bonds on molecules with the addition of water
What's an example?
Hydrolases cleave bonds on molecules with the addition of water
1. Lactase
Substrate: Lactose
Action: Breaks lactose down into glucose and galactose
2. Penicillinase
Substrate: Penicillin
Action: Hydrolyzes beta-lactam ring
__________ add groups to or remove groups from double-bonded substrates
Lyases
____________ change a substrate to its isomeric form
Isomerases
___________ catalyze the formation of bonds with the input of ATP and the removal of water
Ligases
Where are enzymes found?
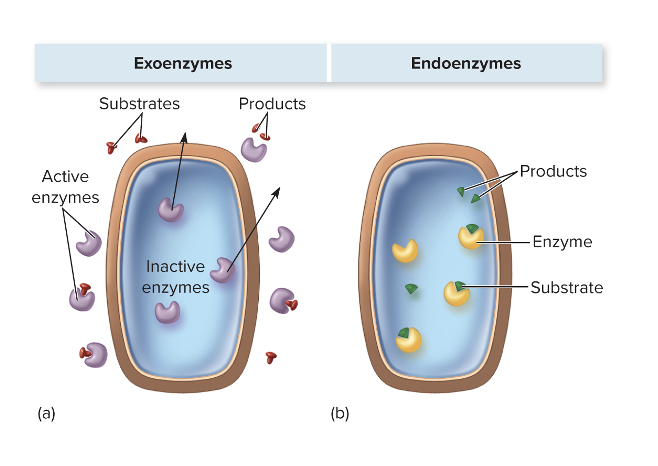
They can be exoenzymes or endoenzymes, and it depends on the microbe as well as the function of the enzyme.
Enzymes can be found inside or outside microbial cells, depending on their type and purpose. Endoenzymes are located inside the cell and carry out reactions necessary for the microbe’s metabolism, like breaking down nutrients for energy or synthesizing cellular components. Exoenzymes, on the other hand, are secreted outside the cell to break down large molecules in the environment into smaller pieces that the microbe can absorb. Whether a microbe produces endoenzymes, exoenzymes, or both depends on the species and the function of the enzyme—for example, pathogens often secrete exoenzymes like proteases or hyaluronidase to invade host tissues.
What are EXOenzymes?
These are enzymes that are meant to be sent (or active) when outside the cell
- Transported extracellularly
- Break down large food molecules or harmful chemicals (break down tissue or found and make it smaller for absorption inside bacterial cell)
Examples
These break down large molecules in the environment so the microbe can absorb them or help it invade host tissues. Examples include:
- Amylase – breaks down starch into sugars
- Proteases – break down proteins into amino acids
- Lipases – break down fats into fatty acids and glycerol
- Hyaluronidase – degrades connective tissue, helping pathogens spread
- Coagulase – causes clotting of blood plasma to protect some bacteria from immune cells
In short, endoenzymes help the microbe survive and grow inside itself, while exoenzymes interact with the environment or host.
What are ENDOenzymes?
- Retained intracellularly and function there
- Most enzymes of metabolic pathways
- Direct processes involved in the cell
Examples
- DNA polymerase – replicates the microbe’s DNA
- RNA polymerase – synthesizes RNA
- Dehydrogenases – involved in energy production (like in glycolysis or the citric acid cycle)
- ATP synthase – produces ATP inside the cell
What are constitutive enzymes?
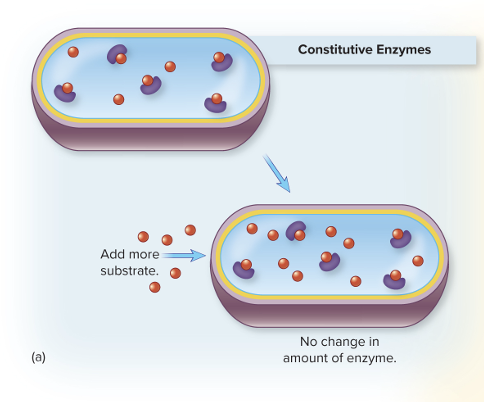
Always present in relatively constant amounts, regardless of the cellular environment
- Always present (not dependent on the amount of substrate; no matter how little or how much substrate is added to the cell, the protein amount never changes)
What are regulated enzymes?
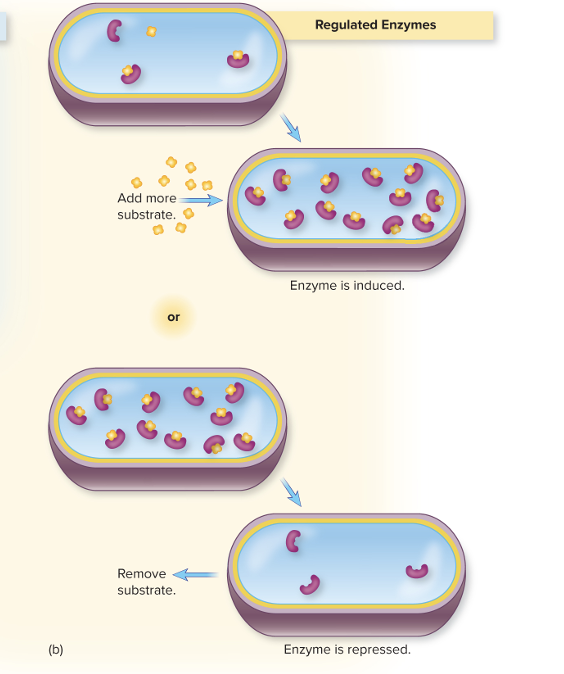
Production is turned on (induced) or turned off (repressed) in response to changes in concentration of substrate
- May NOT always be around (depends on what is expressed at all times) – depends on substrate. If there is a decrease in substrate, it will repress the enzyme, but if there is an increase in substrate, that increases expression of the enzyme
What is the role of microbial enzymes in disease?
- Pathogens secrete unique exoenzymes that help them avoid host defenses or promote multiplication in tissues
- Considered virulence factors because these enzymes contribute to pathogenicity
- Some of these enzymes function as toxins
- Examples: streptokinase, streptolysin, elastase, collagenase, lipase, and penicillinase
Enzyme Examples
- Streptokinase → breaks down blood clots outside the cell
- Streptolysin → lyses host cells like red blood cells
- Elastase → degrades elastin in connective tissue
- Collagenase → breaks down collagen in tissues
- Lipase → breaks down fats in the environment
- Penicillinase (β-lactamase) → breaks down penicillin outside the bacterial cell
- Elastase breaks down elastin, a protein that gives connective tissue its elasticity. By degrading elastin, bacteria can move more easily through tissues that would normally spring back and resist invasion.
- Collagenase digests collagen, the main structural protein in connective tissue. Breaking down collagen creates paths through dense tissue, letting bacteria penetrate deeper.
- Lipase breaks down fats, which can help bacteria access nutrients in host membranes or tissues. While its primary role is nutrient acquisition, this also indirectly facilitates bacterial spread by disrupting cell membranes and tissue barriers.
__________ is a term that explains how changes from normal conditions can make enzymes chemically unstable
Labile
- Enzymes are sensitive
What is denaturation?
- Weak bonds that maintain the shape of an apoenzyme are broken by heat, low or high pH, or certain chemicals
- Disruption distorts the enzyme’s shape
- Prevents the substrate from attaching to the active site
- Nonfunctional enzymes block metabolic reactions and can lead to cell death
- Primary structure = usually intact
- Secondary/tertiary/quaternay structure = disrupted
- Protein function = lost
Metabolic reactions most often occur in a _______ or pathway. Each step is ______ by an ________.
multi-step series
- Each step is catalyzed by an enzyme
- The product of one reaction is often the reactant (substrate) for the next
- Pathways are interconnected and merge at many sites
True or False: Many metabolic pathways have branches that have alternate methods for nutrient processing.
True
Protein catabolism (divergent) and anabolism (convergent) like amino acid synthesis are branched pathways
True or False: No metabolic pathways follow a cyclic form.
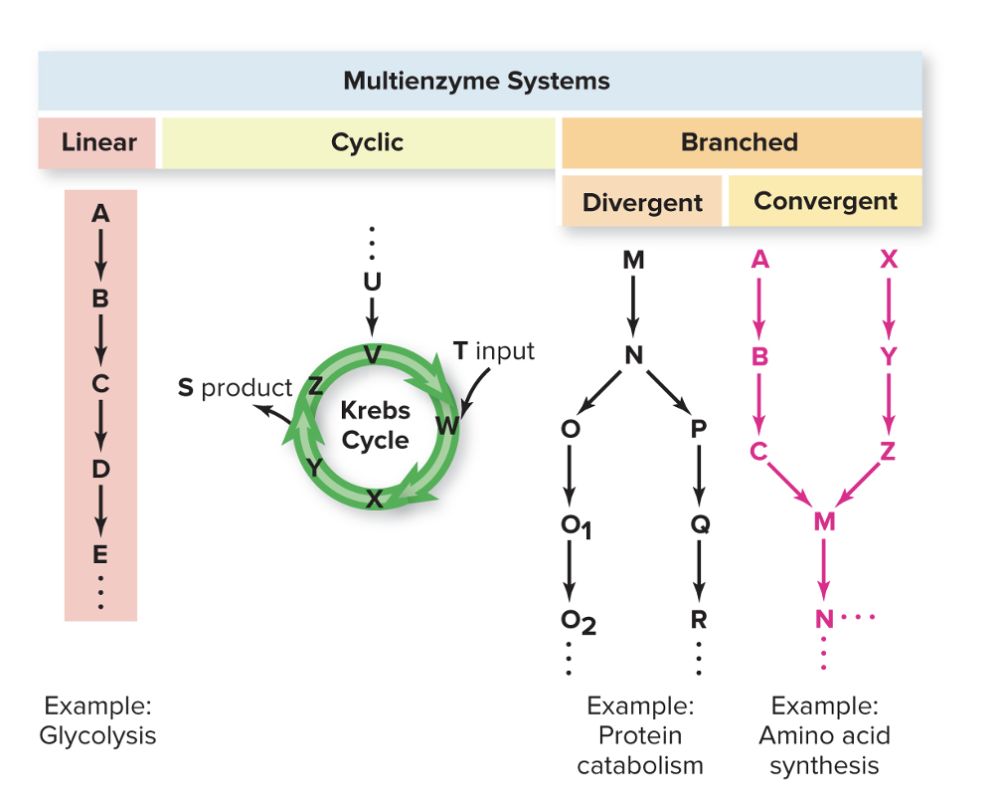
False
- Some pathways take a cyclic form
_____ is a cyclic cycle.
Krebs Cycle
Glycolysis is a ______ cycle.
Linear
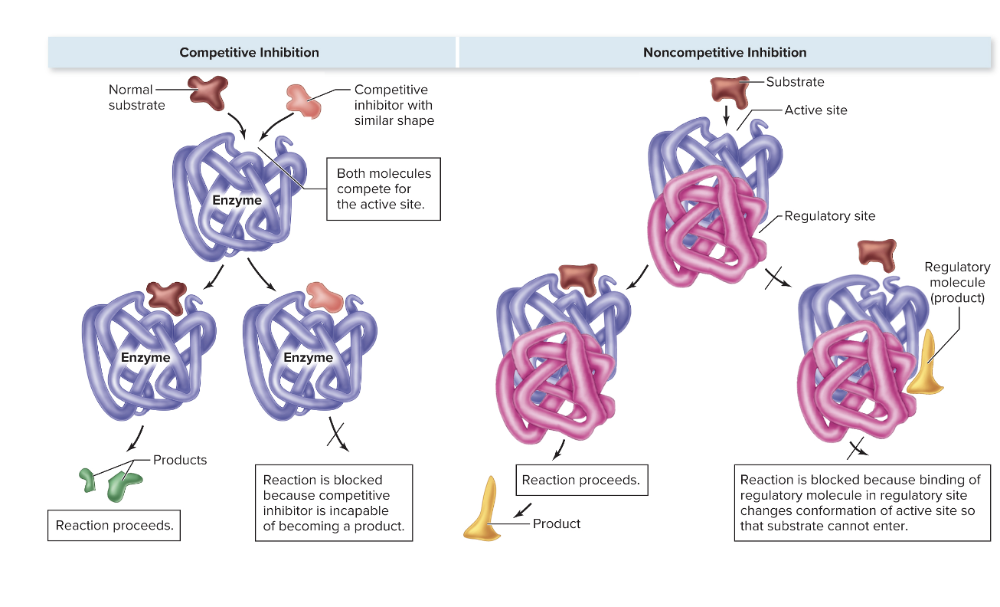
What is competitive inhibition?
- A molecule that resembles the substrate (called the mimic) occupies the active site, preventing the substrate from binding
- Enzyme cannot act on the inhibitor and is effectively shut down
What is noncompetitive inhibition?
- Some enzymes have two binding sites—the active site and the regulatory site
- Regulated by the binding of molecules other than the substrate to the regulatory site
- Regulated by the binding of molecules other than the substrate to the regulatory site
- In feedback inhibition, the end product of a metabolic pathway binds to an allosteric site on an enzyme that acts earlier in the pathway. This binding changes the shape of the enzyme, reducing its activity, but it does not compete with the substrate for the active site. Because the substrate can still bind, but the enzyme’s activity is blocked or slowed
Example – Allolactose (allosteric proteins) binds to that allosteric protein, causing conformational change and protein can no longer bind to operator
In noncompetitive inhibition, the inhibitor binds to an allosteric site (a site other than the active site), which changes the enzyme’s shape and reduces its activity. The substrate can still bind to the active site, but the enzyme’s ability to catalyze the reaction is diminished. Depending on the inhibitor concentration and the enzyme’s properties, activity can be partially reduced or nearly completely inhibited, but it usually doesn’t fully stop all enzyme molecules unless the inhibitor is very abundant or has very high affinity.
Compare and contrast competitive and noncompetitive inhibition?
What is enzyme repression? How is this different from feedback inhibition?
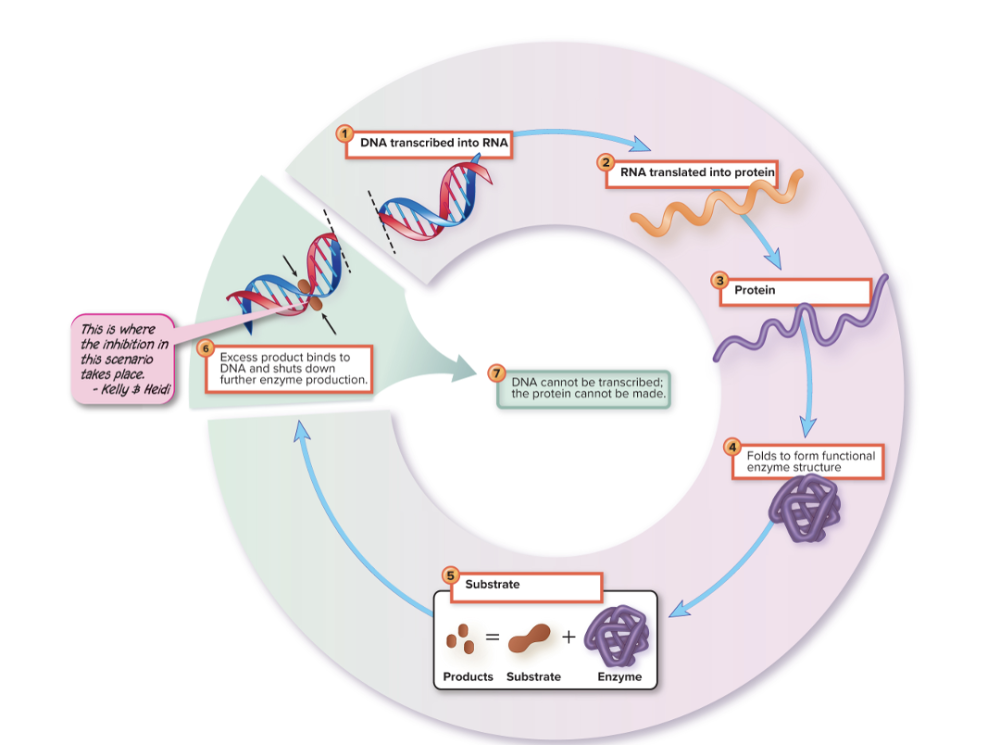
Stops further synthesis of an enzyme somewhere along its pathway
- If the end product of an enzymatic reaction reaches excess, the genetic apparatus for replacing enzymes is suppressed
- Response time is longer than for feedback inhibition, effects more enduring
What you’re describing is repression, which is different from feedback inhibition. Repression stops further synthesis of an enzyme at the genetic level: if the end product of a pathway accumulates, it signals the cell to suppress transcription or translation of the enzyme’s gene. This means no new enzyme molecules are made, so the effect is long-lasting. In contrast, feedback inhibition works at the enzyme activity level, not the gene level. It’s immediate: the end product binds to an existing enzyme to slow or stop its activity, but it doesn’t affect how much enzyme is being produced. Because repression controls enzyme production, its response time is slower than feedback inhibition, but the effect is more enduring since fewer enzymes are synthesized over time.
What is enzyme induction?
Enzyme induction: enzymes appear (are induced) only when suitable substrates are present
- Synthesis of an enzyme is induced by its substrate
- Inverse of enzyme repression
substrate → activates transcription factor → increases enzyme synthesis. The key is that induction is responsive to the environment and only produces the enzyme when it’s needed.
What are exergonic reactions?
- Release energy as they go forward
- Energy is available for doing cellular work
EXAMPLES
- Cellular respiration (glycolysis, citric acid cycle, oxidative phosphorylation) – glucose is broken down into CO₂ and H₂O, releasing energy stored in ATP.
- ATP hydrolysis (ATP → ADP + Pi) – energy released is used to drive other processes.
- Fatty acid oxidation – breaks down fats into acetyl-CoA units, releasing energy.
- Catabolic reactions in general – like protein degradation into amino acids.
What are endergonic reactions?
- Require the addition of energy to move forward
EXAMPLES
- Protein synthesis (translation) – linking amino acids into polypeptides requires energy from ATP/GTP.
- DNA and RNA synthesis – nucleotides are joined together using energy from nucleotide triphosphates.
- Gluconeogenesis – creating glucose from pyruvate or other precursors consumes ATP.
- Fatty acid synthesis – building long-chain fatty acids from acetyl-CoA consumes energy.
- Active transport – moving molecules against their concentration gradient requires energy.
True or False: Exergonic and endergonic reactions are often coupled
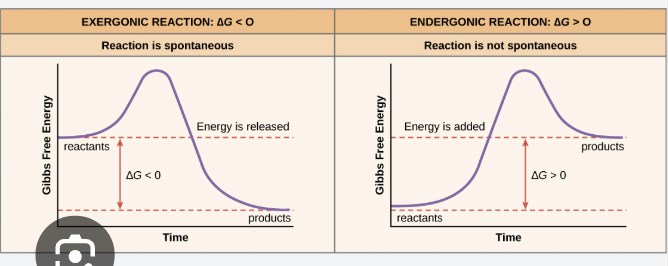
True
Redox reactions always occurs in __________
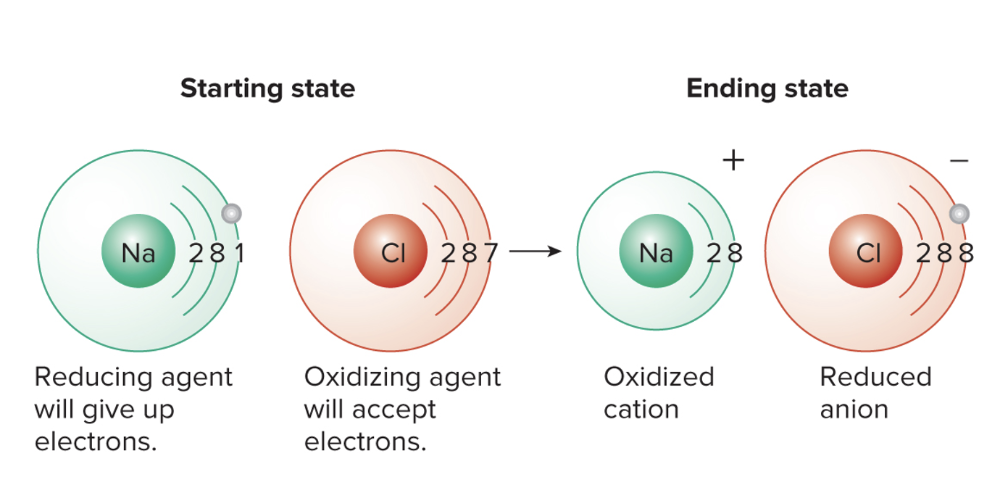
pairs called redox pairs. There is generally an electron donor and electron acceptor
- Oxidoreductases are important in cellular redox reactions
- Coenzyme carriers: NAD and FAD
- Newly reduced compounds (the ones that gain electrons) have more energy than they did in their oxidized state
- The energy now present in the electron acceptor can be captured to phosphorylate (add an inorganic phosphate) to ADP or some other compound
- This process stores the energy in a high-energy molecule
What are some common electron carriers?
NAD:
- Most common electron carrier
- Carries hydrogens and a pair of electrons from dehydrogenation reactions
- Reduced NAD is presented as NADH + H+ OR NADH
FAD:
- Reduced FAD is presented as FADH
NADP:
- NAD phosphate
What happens in catabolic pathways?
What are the two types of metabolisms?
Catabolic pathways:
- Electrons are extracted and carried through a series of redox reactions to a final electron acceptor
- Aerobic metabolism: oxygen is the final electron acceptor
- Anaerobic metabolism: come other inorganic or organic compound
What is ATP, what is it made out of, and how does it serve as an energy source?
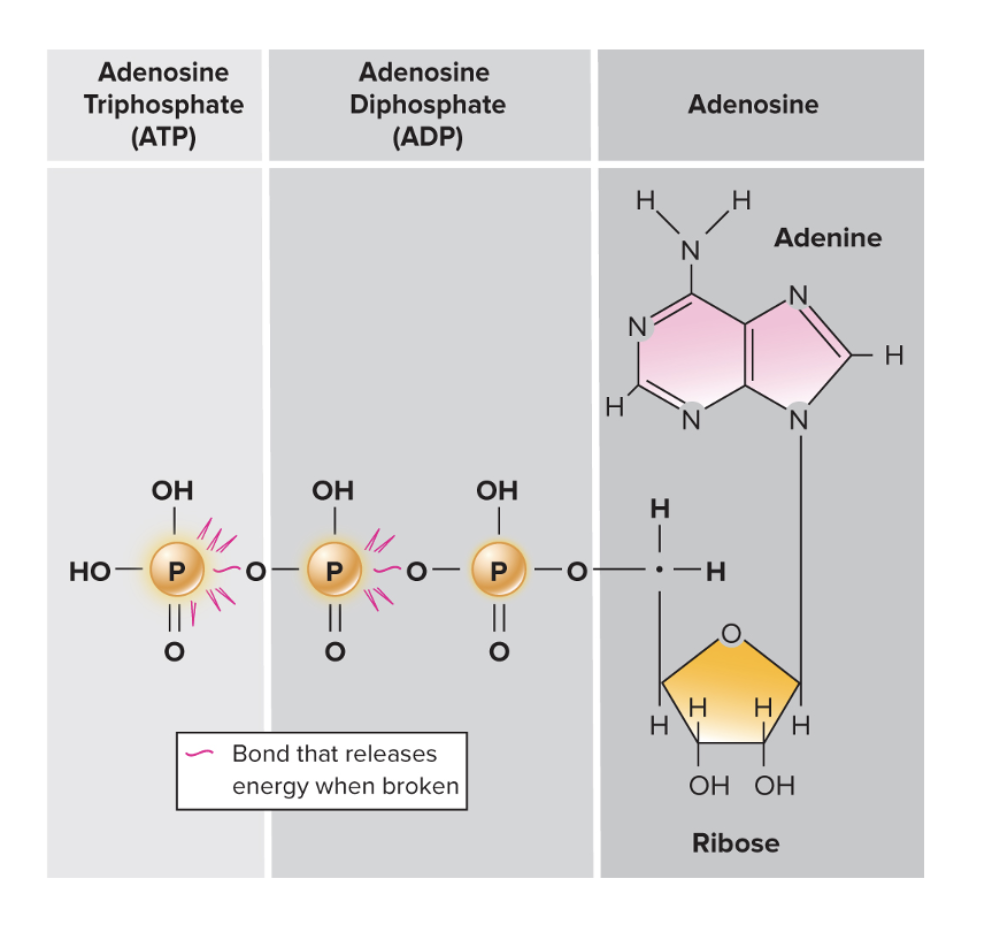
Three-part molecule: Adenosine Triphosphate
- Adenine: nitrogen base
- Ribose: 5-carbon sugar
Three phosphate groups bonded to the ribose
- Bulky and have a negative charge
- Repelling electrostatic charges imposes a strain between the last two phosphate groups
- Removal of phosphates releases free energy
Primary energy currency of the cell
- When it is used in a chemical reaction, it must be replaced
- ATP utilization and replenishment is an ongoing cycle
ATP (adenosine triphosphate) serves as the primary energy currency of the cell because it stores energy in the high-energy phosphate bonds between its three phosphate groups. When the terminal phosphate bond is broken through hydrolysis (ATP → ADP + Pi), a significant amount of free energy is released
What is substrate-level phosphorylation?
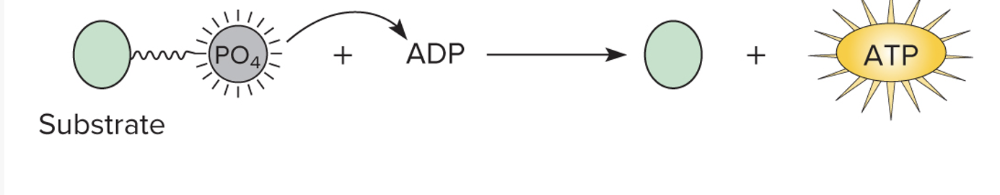
- Generation of ATP through a transfer of a phosphate group from a phosphorylated compound directly to ADP
What is oxidative phosphorylation?
A series of redox reactions occurring during the final phase of the respiratory pathway
Oxidative phosphorylation is the process your cells use to make most of their ATP. It happens in the mitochondria, where electrons from molecules like NADH and FADH₂ are passed along the electron transport chain. As the electrons move, they help pump protons across the mitochondrial membrane, creating a proton gradient. This gradient stores potential energy, and when protons flow back through ATP synthase, it drives the production of ATP from ADP and inorganic phosphate. Essentially, oxidative phosphorylation converts the energy from food molecules into usable ATP by using an electron flow to power a molecular “turbocharger.”
The electron transport chain (ETC) takes place in the inner mitochondrial membrane, where electrons from NADH and FADH₂ are passed along a series of protein complexes. As electrons move through the chain, these complexes pump protons from the mitochondrial matrix into the intermembrane space, creating a proton gradient. This gradient stores potential energy, which is then used to drive protons back through ATP synthase. The flow of protons through ATP synthase powers the conversion of ADP and inorganic phosphate into ATP, making it the main way cells produce energy in the form they can use.
What is photophosphorylation?
- ATP formed through a series of sunlight-driven reactions in phototrophs
What are the three main pathways of catabolism?
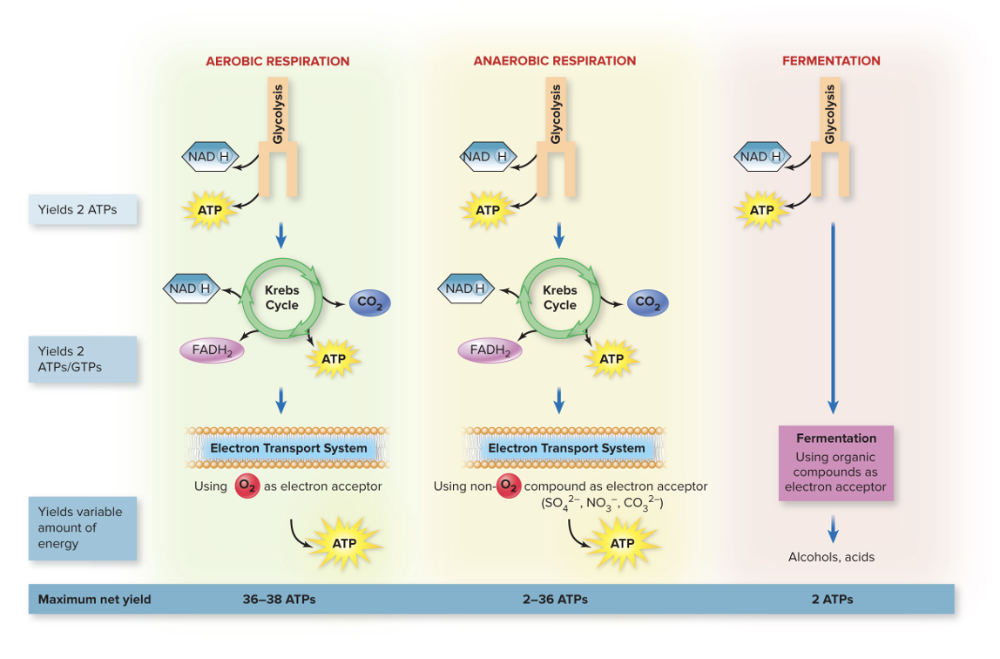
1. Aerobic Respiration
- Aerobic respiration is a process that uses oxygen as the final electron acceptor to completely break down glucose into carbon dioxide and water, producing a large amount of ATP. It includes glycolysis, the citric acid cycle, and oxidative phosphorylation, and is the most efficient way for cells to harvest energy.
2. Anaerobic Respiration
- Anaerobic respiration is similar, but it uses a molecule other than oxygen (like nitrate, sulfate, or carbon dioxide) as the final electron acceptor. It produces less ATP than aerobic respiration because the electron transport chain is less efficient without oxygen.
3. Fermentation
- Fermentation, on the other hand, does not use an electron transport chain at all. It regenerates NAD⁺ by transferring electrons from NADH to an organic molecule (like pyruvate), allowing glycolysis to continue and producing a small amount of ATP. Fermentation is much less efficient but allows cells to make energy in the absence of oxygen.
Compare and contrast Aerobic vs Anaerobic Respiration.
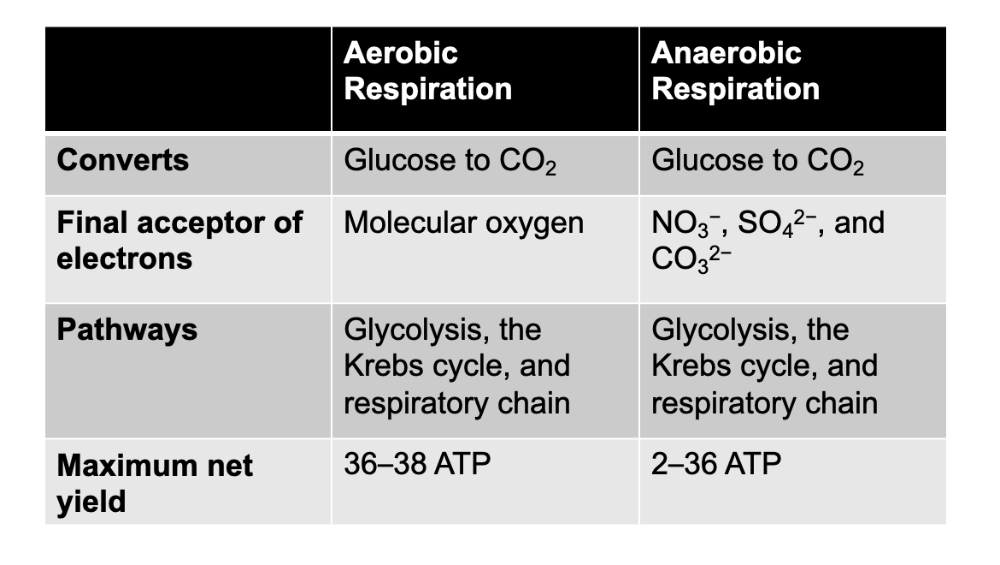
Main difference in the amount of energy they yield and the final electron acceptor
Fermentation is for _______ and ________ anaerobes.
1. Facultative
- Facultative refers to organisms that can survive in more than one condition, especially regarding oxygen. For example, facultative anaerobes can use oxygen to make energy when it’s available (aerobic respiration) but can also switch to fermentation or anaerobic respiration when oxygen is absent. Facultative anaerobes prefer oxygen because aerobic respiration produces much more ATP than fermentation or anaerobic respiration, but they can survive without it by switching to other energy-making pathways.
2. Aerotolerant
- Aerotolerant anaerobes, on the other hand, do not use oxygen at all for energy. They survive just fine whether oxygen is present or not, but they don’t gain any extra energy from it.
True or False: Fermentation only uses glycolysis and oxygen is NOT required as they use other organic compounds as electron acceptors.
True
What is the starting compound for respiration, and why?
Glucose!
- Carbohydrates such as glucose are good fuels because they are readily oxidized (losing electrons)
- They are excellent hydrogen and electron donors
- The enzymatic withdrawal of hydrogens from glucose removes electrons that can be used in energy transfers
What is the end product of this conversion from glucose to CO2, with aerobic and anerobic respiration?
The end products of the conversion of these carbon compounds are energy-rich ATP and energy-poor carbon dioxide and water
Review PPT slides for Respiration
237 to
Chapter 23
Infectious Diseases Manifesting in the GI tract
What are the eight main segments of the GI tract?
Mouth, pharynx, esophagus, stomach, small intestine, large intestine, rectum, and anus
What are the four accessory organs?
Salivary glands, liver, gallbladder, and pancreas
What are the defenses against a heavy load of microorganisms?
- Layer of mucus coating intestinal surfaces
- Secretory IgA
- Peristalsis keeps microbes moving
- Saliva: lysozyme, lactoferrin
- Stomach: extremely low pH
- Bile is antimicrobial
- GALT (gut-associated lymphoid tissue)
True of False: The GI tract has no normal biota.
False
- The GI tract is home to a very large variety of normal biota, and every portion of it has a distinct microbial population
- Oral cavity: saliva, sIgA, lysozyme, tonsils, and adenoids
- Rest of GI tract: GALT, lymphoid tissue, Peyer's patches, appendiz, sIgA, and rich normal microbiota
What are the different parts of the normal microbiota as part of the GI tract?
Oral microbiome:
- Dominated by bacterial species
- Methane-producing archaea
- Fungi
- Few protozoa species
- The virome is still being studied
Esophagus and stomach:
- 200 different species
- Most common types belong to the Firmicutes
Large intestine:
- 1011 microbes per gram of contents
- Includes bacteria, fungi, and several protozoa
What is the most common species of normal microbiota in the stomach/esophagus?
- Most common types belong to the Firmicutes
_______ organs are considered to be FREE of normal biota
Accessory organs
What are the functions of the normal gut biota?
Functions of normal gut biota:
- Protective function
- Teach immune system to react properly to microbial antigens
- Aid digestion and provide nutrients
A diverse gut microbiome is associated with health
Dental caries are caused by what, and what are the unique characteristics...
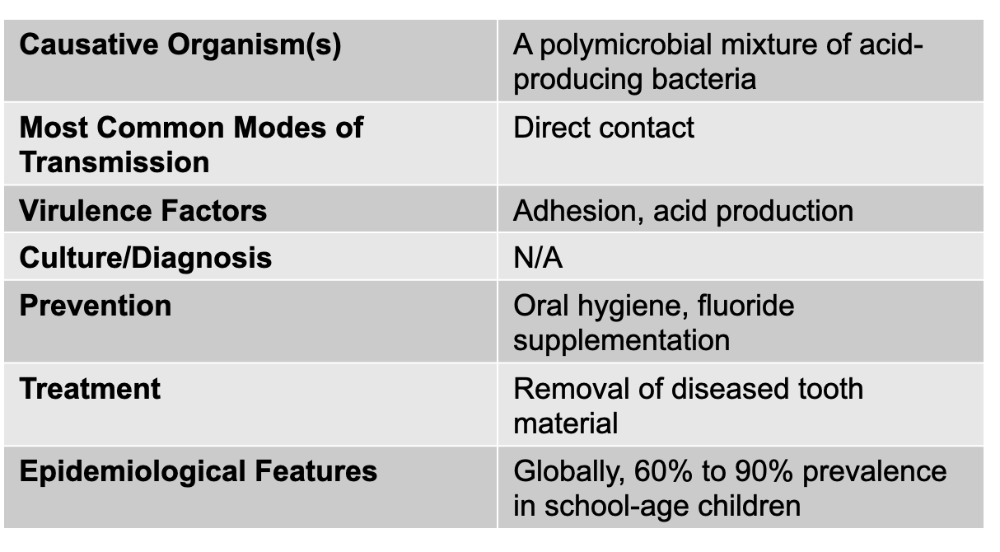
The most common infectious disease of human beings
- Dissolution of the tooth surface due to the metabolic action of bacteria
- Results in minor to complete disruption of enamel
- Destruction of deeper layers can result in infection of the pulp
- Streptococcus mutans and S. sobrinus are the main causes
- Incidence of dental carries varies according to carbohydrate consumption, oral hygiene, and genetic factors
Mumps is caused by what, and what are the unique characteristics about it?
- Associated with a distinctive and painful swelling at the angle of the jaw
- Caused by a single-stranded RNA virus from the paramyxovirus genus
- Incubation period is 2-3 weeks
- Signs and symptoms include fever, nasal discharge, muscle pain, malaise
- FOLLOWED by inflammation of the salivary glands causing gopherlike swelling of the cheeks
- There can be complications: meaning it can invade other organs, testes, ovaries, thyroid gland, pancrease, meninges, heart, and kidneys
- in 20-30% of young adult males, there is infection localized in the epididymis and testes, but it DOES NOT cause sterility
Causative agent: Mumps virus (genus paramyxovirus)
Mode of transmission: Droplet contact
Virulence Factors: spike-induced syncytium formation (Paramyxoviruses can infect multiple host cell types because they use a fusion (F) protein and an attachment protein (like HN, H, or G depending on the virus) that recognize receptors found on many different kinds of cells. Once the attachment protein binds its receptor, the F-protein is activated and causes the viral envelope to fuse directly with the host cell membrane. This fusion ability is not restricted to one cell type because the receptors they target—often sialic acid or broadly expressed surface proteins—are present on a wide range of respiratory and immune cells. Because of this broad receptor distribution, paramyxoviruses can spread from the respiratory epithelium into immune cells, syncytia-forming clusters, and even neural tissue in some cases. Their F-protein also allows cell-to-cell fusion, creating syncytia, which lets the virus move between cells without needing to exit the host cell, further expanding the number of cells they can infect and helping them evade the immune system.)
Culture/Diagnosis: ELISA for Ab; PCR
Prevention: MMR live attenuated vaccine
Treatment: Supportive
Epidemiological Features: United States: fluctuates between a few hundred cases a year and a few thousand; internationally: epidemic peaks every 2 to 5 years
For mumps, after the initial signs and symptoms, what follows?
- Followed by the inflammation of the salivary glands producing gopherlike swelling of cheeks
What can mumps lead to in 20-30% of young adult males....
Localized infection in the epididymis and testes, but does NOT cause sterility.
Gastritis and gastric/peptic ulcers are caused by what, and what are the unique characteristics?
- Gastritis: sharp or burning pain emanating from the abdomen
- Gastric or peptic ulcers: lesions in the mucosa of the stomach or uppermost portion of the small intestine
- Infects half of the world's population
Causative agent: helicobacter pylori
Mode of Transmission: oral to oral or oral-fecal route LIKELY
Virulence Factors: adhesions and urease (Adhesions are surface molecules that let the bacteria stick tightly to the stomach’s epithelial cells, anchoring it in place despite constant mucus flow and peristalsis. This close attachment allows the bacteria to deliver toxins and cause localized inflammation. Urease is an enzyme that breaks down urea into ammonia and carbon dioxide; the ammonia acts as a buffer that neutralizes stomach acid around the bacteria, creating a more alkaline “microenvironment” that keeps H. pylori alive. However, ammonia is also toxic to epithelial cells and contributes to tissue injury. Together, adhesions help H. pylori stay in the stomach long enough to cause disease, while urease enables survival in acid and directly contributes to mucosal damage, ultimately leading to chronic inflammation and ulcer formation.)
Culture/Diagnosis: direct antigen test on stool, urea breath test
Prevention: none
Treatment: Clarithromycin + acid suppression
Epidemiological Features: United States: infection (not disease) rates at 35% of adults; internationally: infection rates at 50%
What is the best treatment for gastritis/gastric ulcers?
Best treatment is clarithromycin
What is acute diarrhea (with or without vomiting)?
- Defined as three or more loose stools in a 24-hr period
- United States: average of 1.2 to 1.9 cases per person per year
- 1/3 of cases are transmitted by contaminated food
- In tropical countries, children experience more than 10 episodes per year
- More than 700,000 children die from diarrhea per year, mostly in developing countries
What is the most common cause of foodborne illness?
Norovirus
What is the most common cause of death due to foodborne illness?
Salmonella
What are the pathogens that cause acute diarrhea?
(SSSE CCV)
(CRN)
BACTERIAL CAUSES:
Salmonella
Shigella,
Shiga-toxin producing E-coli
Other E.coli (non-shiga toxin producing)
Campylobacter
Clostridiodies difficile
Vibrio cholerae
Non-cholera Vibrio species
NON-BACTERIAL CAUSES:
Cryptosporidium
Rotavirus
Norovirus
What is the most common cause of bacterial diarrhea in the U.S?
Campylobacter
Salmonella causes what, and what are the unique characteristics
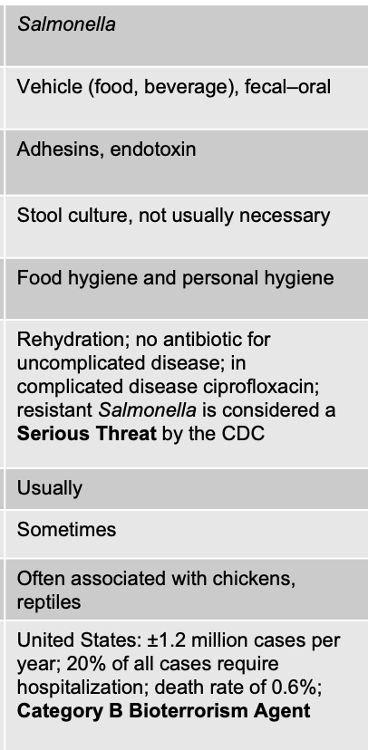
ACUTE DIARRHEA
Facts about Salmonella
- Gram -, motile bacteria divided into serotypes based on presence of MAJOR surface antigens
H, O, and K antigens are used to identify gram-negative enterics
- H: flagellar antigen
- K: capsular antigen
- O: cell wall antigen, the polysaccharide portion of the LPS
Ferment glucose with acid and gas production (we mean that the bacteria can use glucose as an energy source through fermentation, and in doing so they produce both acidic byproducts and gas. This pattern is important because it helps microbiologists distinguish Salmonella from other enteric bacteria during diagnostic testing.)
- Produce H2S (hydrogen sulfide) but not urease
- Grow readily on lab media and survive inhospitable environments
Signs/Symptoms
- causes variety of diseases, resulting in 1 million cases and 400 deaths a year
- Salmonellosis: enteric fever or gastroenteritis - can range form mild gastroenteritis (v,d, and musosal irritation) to fever and septicemia
- Typhoid fever: Salmonella enterica serotype Typhi
- Ability to cause disease is dependent on its ability to adhere to gut mucosa
- HAS A high ID50
____________________________
Causative: salmonella
Mode of transmission: vehicle (food and beverage), fecal-oral
Virulence Factors: adhesions and endotoxin
- Adhesins are specific surface proteins that bacteria use to attach to host cells. They function like molecular “hooks” that recognize and bind to receptors on intestinal epithelial cells. In contrast, the H, O, and K antigens are structural identification markers used for serotyping gram-negative bacteria, not for adhesion. Endotoxin, which is the lipid A portion of the gram-negative LPS in the outer membrane, contributes to disease by activating a strong inflammatory response. When endotoxin is released during bacterial growth or lysis, it stimulates immune cells to release cytokines that can cause fever, inflammation, and in severe cases contribute to septic shock.
Culture/Diagnosis: stool culture, usually not necessary
Prevention: food/ personal hygiene
Treatment: Rehydration; no antibiotic for uncomplicated disease; in complicated disease ciprofloxacin; resistant Salmonella is considered a Serious Threat by the CDC
FEVER PRESENT (usually)
BLOOD IN STOOL: sometimes
Distinctive Features: often associated with chickens, reptiles
Epidemiological: United States: ±1.2 million cases per year; 20% of all cases require hospitalization; death rate of 0.6%; Category B Bioterrorism Agent
What are the three antigens used to identify the gram-negative enterics or subtypes of salmonella?
- H: flagellar antigen
- K: capsular antigen
- O: cell wall antigen, the polysaccharide portion of the LPS
H, O, and K antigens are surface structures found on gram-negative enteric bacteria, and they’re used in serotyping to distinguish one species or strain from another. The O antigen refers to the outer portion of the lipopolysaccharide (LPS) on the bacterial outer membrane and varies widely among species, making it useful for identifying different serogroups. The H antigen is the flagellar protein, so only motile bacteria have it, and its variations help differentiate strains based on their flagellar structure. The K antigen is a capsular polysaccharide surrounding some bacteria; it can mask the O antigen and contributes to virulence by preventing phagocytosis.
Salmonella causing acute diarrhea has a ____ infectious dose.
Most Salmonella species that cause gastroenteritis require a high infectious dose, often around 10³–10⁵ organisms, because they are sensitive to stomach acid and many are killed before reaching the intestines. This is why Salmonella infections usually occur from eating a large bacterial load in contaminated foods like eggs, poultry, or undercooked meat.
Shigella causes what, and what are the unique characteristics?
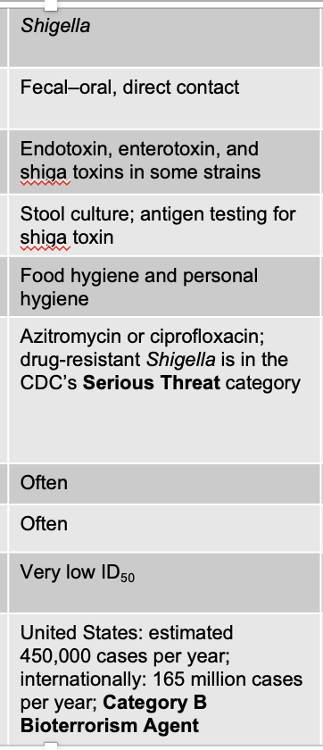
ACUTE DIARRHEA
- Gram -, straight rods, NON-motile
- Unable to form endospores, produce urease or H2S (hydrogen sulfide)
- Shigella dysenteriae: causes the most severe form, uncommon in the U.S., more common in the eastern hemisphere
Symptoms
- Frequent, watery stools, fever, and intense abdominal pain
- N,V are common
- Dysentery: diarrhea containing BLOOD
- Mucus from GI tract will also be present in stools
Pathogenesis and Virulence Factors
- Invades the villus cells of the large intestine but DOES NOT perforate the intestine or invade the blood
- Release of endotoxin causes fever
- Enterotoxin affects the GI, damages the mucosa and villi, gives rise to bleeding and secretion of mucus
- Shiga toxin: responsible for more serious damage to the intestine as well as systemic effects
_______________________________
Fecal–oral, direct contact
Virulence: Endotoxin, enterotoxin, and shiga toxins in some strains
- Shigella’s endotoxin, which is the lipid A portion of its LPS, contributes to inflammation by triggering cytokine release and causing fever, but it is not the main cause of its severe GI symptoms. Some Shigella strains also produce an enterotoxin that increases fluid secretion in the intestines, contributing to watery diarrhea in the early phase of infection.
Culture/Diagnosis: Stool culture; antigen testing for shiga toxin
Prevention: Food hygiene and personal hygiene
Treamtnet: Azitromycin or ciprofloxacin; drug-resistant Shigella is in the CDC’s Serious Threat category
Fever: Often
Blood in stool: Often
Distinctive Features: Very low ID50
United States: estimated 450,000 cases per year; internationally: 165 million cases per year; Category B Bioterrorism Agent
Shigella can also cause shigella _______, and dysentery is _______.
shigella dystenteriae
diarrhea containing blood
What are the virulence factors for Shigella
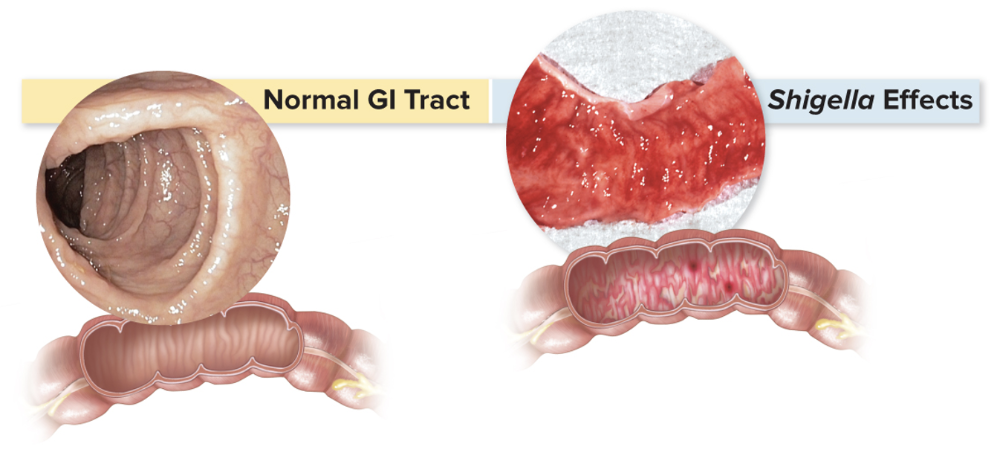
- Invades the villus cells of the large intestine but does not perforate the intestine or invade the blood
- Release of endotoxin causes fever
- Enterotoxin: affects the entire GI tract, damages the mucosa and villi, and gives rise to bleeding and secretion of mucus
- Shiga toxin: responsible for more serious damage to the intestine as well as systemic effects
Shiga-Toxin Producing Escherichia coli (STEC) causes what, and what are the unique characteristics?
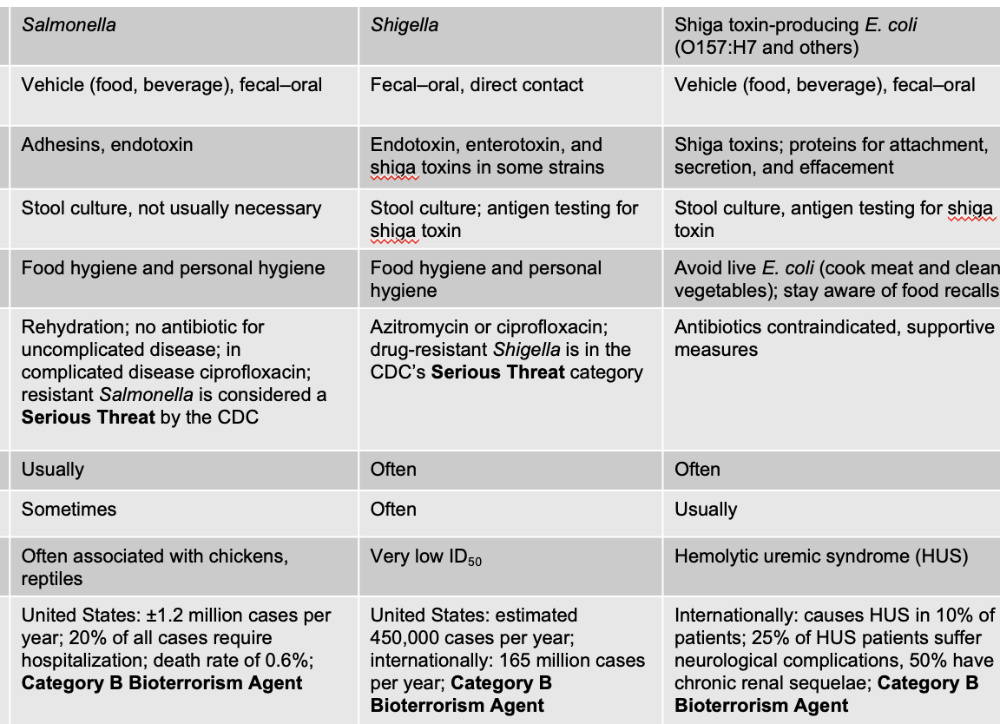
ACUTE DIARRHEA
E.coli O157:H7
Signs/Symptoms
- range from mild gastroenteritis with fever to BLOODY diarrhea
- Hemolytic uremic syndrome: severe hemolytic anemia that can cause kidney damage and failure
- Uremic: a build-up of toxins and waste products (like urea) in the blood because the kidneys have failed to filter them out
- Toxins identical to the shiga toxins produced by Shigella
- Transmission through ingestion of undercooked beef and other contaminated food/beverages
Mode: Vehicle (food, beverage), fecal–oral
Virulence: Shiga toxins; proteins for attachment, secretion, and effacement
- The most dangerous strains, like Shigella dysenteriae type 1, produce Shiga toxin, a potent AB toxin that enters host cells, destroys part of the 60S ribosomal subunit, and stops protein synthesis. This leads to cell death, ulceration of the intestinal mucosa, and bloody, mucus-filled stools. Shiga toxin can also enter the bloodstream and damage endothelial cells in the kidneys, contributing to hemolytic uremic syndrome (HUS).
- These proteins allow the bacteria to attach tightly to intestinal epithelial cells, inject bacterial proteins into the host cell using a type III secretion system, and then cause effacement, which is the destruction of the microvilli on the intestinal surface. This effacement disrupts absorption and contributes to diarrhea.
Culture/Diagnosis: Stool culture, antigen testing for shiga toxin
Prevention: Avoid live E. coli (cook meat and clean vegetables); stay aware of food recalls
Treatments: Antibiotics contraindicated, supportive measures
Fever: Often
Blood in stool: Usually
Distinctive: Hemolytic uremic syndrome (HUS)
Internationally: causes HUS in 10% of patients; 25% of HUS patients suffer neurological complications, 50% have chronic renal sequelae; Category B Bioterrorism Agent
What is the specific strain for Shiga-toxin producing E. coli?
The designation O157:H7 identifies the strain based on its O and H antigens, which are used for serotyping gram-negative enterics. The O157 refers to the specific type of O antigen on its lipopolysaccharide (LPS), while H7 refers to the H antigen on its flagella. This serotype is clinically important because it is the strain that produces Shiga toxin, causing bloody diarrhea, hemolytic uremic syndrome (HUS), and severe colitis.
Other E. coli (Non-Shiga Toxin Producing) causes what, and what are the unique characteristics?
ACUTE DIARRHEA
Causative agent: Other E. coli (Non-Shiga Toxin Producing)
Mode of transmission: Vehicle, fecal–oral
Virulence factors: Various: proteins for attachment, secretion, effacement; heat-labile, and/or heat-stable exotoxins; invasiveness
Culture/Diagnosis: Stool culture not usually necessary in absence of blood, fever
Prevention: Food and personal hygiene
Treatment: Rehydration, antimotility agent
Fever: Sometimes
Blood: Sometimes
Distinctive Features: ETEC, EIEC, EPEC, DAEC, EAEC
Epidemiological: N/A
Campylobacter causes what, and what are the unique characteristics?
ACUTE DIARRHEA
- Most common cause of bacterial diarrhea in the United States
Signs and symptoms:
- Frequent watery stools, fever, vomiting, headaches, and severe abdominal pain
- Symptoms may last longer than 2 weeks and recur
Bacteria
- Campylobacter jejuni is a slender, curved, or spiral gram-negative bacteria with polar flagella
- Microaerophilic inhabitants of the intestinal and genitourinary tracts and oral cavities of animals and humans
- Describing them as microaerophilic means they grow best in low oxygen and high CO₂ environments—not full oxygen like many bacteria—because their metabolism is adapted to those conditions. Finally, saying they inhabit the intestinal, genitourinary, and oral tracts of animals and humans tells you they are part of the natural flora of many species and that infections usually occur through contaminated food—especially poultry—where they can colonize the human intestines and cause diarrhea.
Transmission
- via ingestion of contaminated beverages, food, water, milk, meat, and chicken
- Late 2019 and 2020 outbreak affecting 30 states (due to contact of stool with healthy-looking puppies from a pet store)
- Small number of cases, infection can lead to serious neuromuscular paralysis caused Guillain–Barré syndrome
____________________________
Causative: Campylobacter
Mode of Transmission: Vehicle (food, water), fecal–oral
Virulence: Adhesins, exotoxin, and induction of autoimmunity
- Campylobacter jejuni uses adhesins to attach firmly to the intestinal epithelium, allowing it to resist being flushed out and giving it close contact with host cells so it can invade and trigger inflammation. It also produces an exotoxin, often called the cytolethal distending toxin (CDT), which damages host cell DNA, disrupts the cell cycle, and contributes to mucosal injury and diarrhea. The most unique part of its pathogenesis is its ability to trigger autoimmunity through molecular mimicry. Some of Campylobacter’s surface structures resemble human nerve gangliosides, so when the immune system makes antibodies against the bacteria, those antibodies can mistakenly attack peripheral nerves. This can lead to Guillain–Barré syndrome, a post-infectious autoimmune paralysis.
Culture/Diagnosis: Stool culture not usually necessary; dark-field microscopy
Prevention: Food and personal hygiene
Treatment: Rehydration; azithromycin in severe cases (antibiotic resistance rising; resistant Campylobacter is in CDC’s Serious Threat category)
Fever: Usually
Blood: No
Distinctive Features: Guillain-Barré syndrome
United States: 1.3 million cases per year; internationally: 400 million cases per year
Small number of cases of acute diarrhea caused by campylobacter jejuni can lead to a serious condition called ...
- In a small number of cases, infection can lead to a serious neuromuscular paralysis called Guillain–Barré syndrome
Clostridiodes difficile causes what, and what are unique characteristics of it?
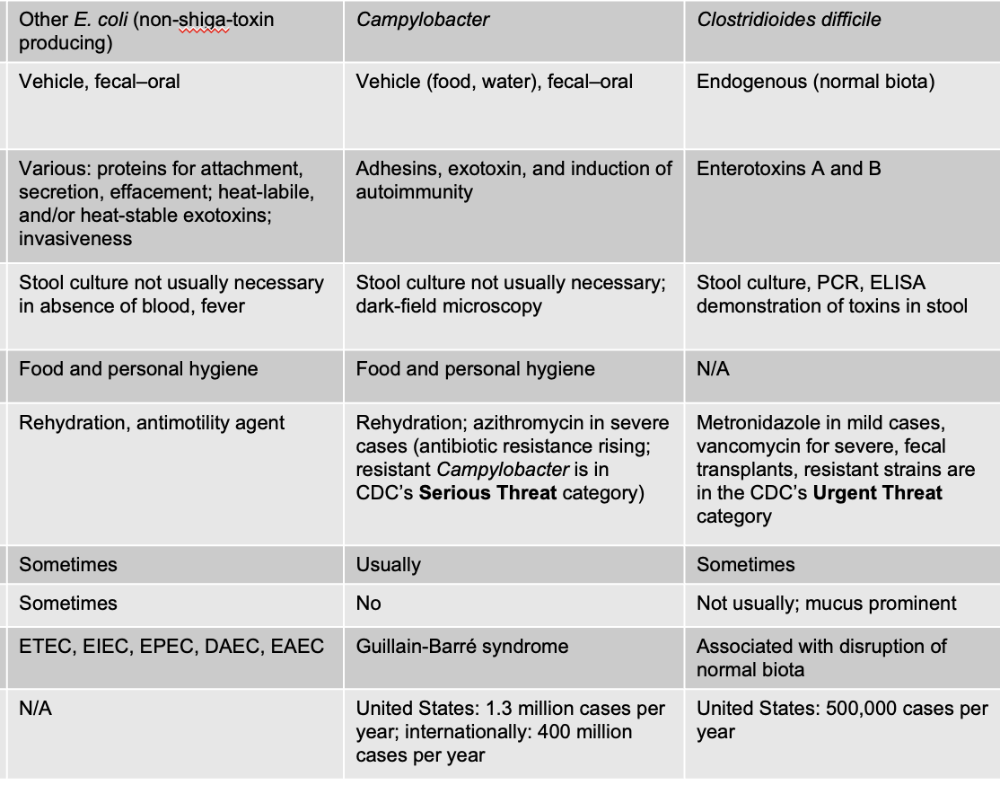
ACUTE DIARRHEA
Gram + endospore forming rod (found in normal biota of intestine)
- Pseudomembranous colitis, antibiotic-associated colitis
- Precipitated by therapy with broad-spectrum antibiotics
- Enterotoxins A and B cause necrosis in the wall of the intestine
Treatment
- Withdrawal of antibiotics, replacement of fluids
- Fidaxomicin or vancomycin
- Fecal transplant
- withdrawing the antibiotic that triggered the imbalance so healthy gut flora can begin to recover. Meanwhile, the toxins produced by C. diff cause severe diarrhea, which leads to dehydration, so fluid replacement is essential to prevent complications. Medications like fidaxomicin or oral vancomycin are used because they specifically kill C. diff while sparing much of the normal gut microbiota, helping restore balance without causing further disruption. For recurrent infections—when the gut microbiome cannot recover on its own—a fecal transplant is used to reintroduce a full, healthy community of bacteria, which outcompetes C. diff and dramatically reduces recurrence rates.
______________________________
Clostridioides difficile
Endogenous (normal biota)
Virulence Factors: Enterotoxins A and B
Culture/Diagnosis: Stool culture, PCR, ELISA demonstration of toxins in stool
Prevention: N/A
Treatment: Metronidazole in mild cases, vancomycin for severe, fecal transplants, resistant strains are in the CDC’s Urgent Threat category
Fever: Sometimes
Blood in Stool: Not usually; mucus prominent
Distinctive: Associated with disruption of normal biota
United States: 500,000 cases per year
Vibrio cholerae causes what, and what are the unique characteristics of it?
- Curved rod with a single polar flagellum
- Fermentative
- Grows on ordinary or selective media containing bile at 37 degrees Celsius
- Posses unique O and H antigens and other membrane receptor antigens
- Outbreaks of cholera are expected to happen after natural disasters, war, or large refugee movements
Signs/Symptoms:
- Vomiting
- Copious watery feces, "rice-water stool"
- Profuse water loss
- Loss of blood volume, acidosis, potassium depletion, muscle cramps, severe thirst, flaccid skin, and sunken eyes; convulsions and coma in young children
- Hypotension, tachycardia, cyanosis, shock
- 55% to 70% mortality rate
________________________________
Vibrio cholerae
Vehicle (water and some foods), fecal–oral
Cholera toxin (CT)
Culture/Diagnosis: Clinical diagnosis, microscopic techniques, serological detection of antitoxin
Prevention: Water and food hygiene
Treatment: Rehydration and possibly doxycycline
Fever: No
Blood in Stool: No
Distinctive Features: Rice-water stools
Global estimate: 21,000–143,000 deaths annually; Category B Bioterrorism Agent
What is the pathogenesis and virulence factors for vibrio cholerae like?
- Cholera toxin: disrupts the normal physiology of intestinal cells, causing them to shed large amounts of electrolytes into the intestine
- Uses quorum sensing to regulate the expression of virulence factors
Transmission and epidemiology:
- Warm, monsoon, alkaline, and saline conditions favor growth of Vibrio
Treatment: oral rehydration therapy
Non-Cholera Vibrio species causes what, and what are the unique characteristics?
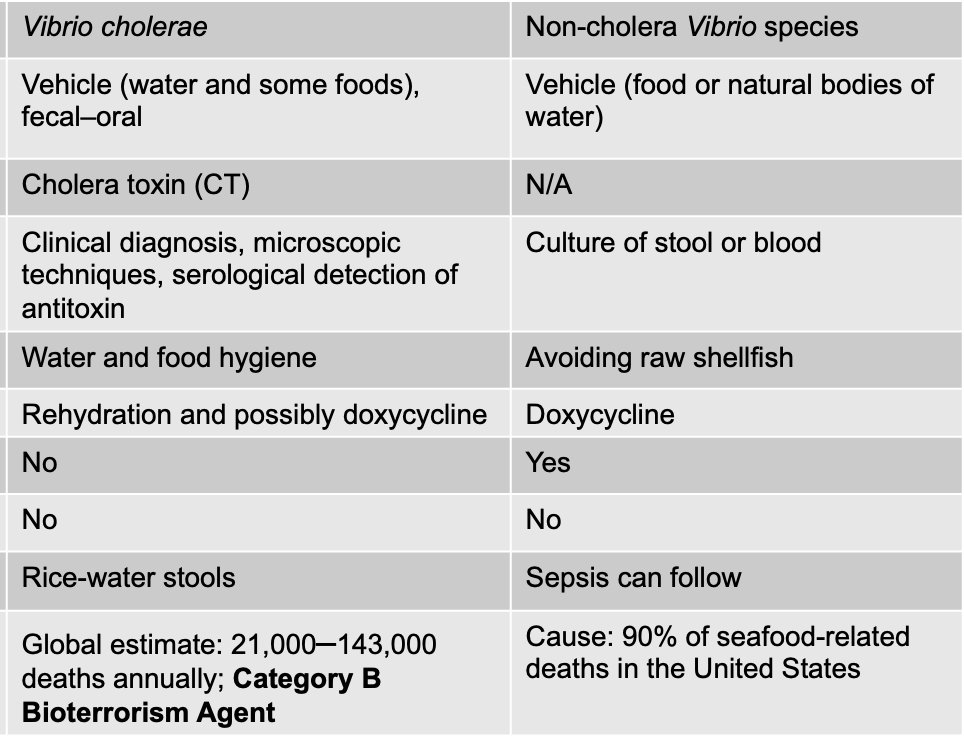
ACUTE DIARRHEA
- more common to experience an infection with a non-cholera species of Vibrio than a V. cholerae infection
- These infections are called vibrioses
- Prominent causative agents: V. vulnificus and V. parahaemolyticus
Factors that increase the chance of infection:
- Increased consumption of raw oysters
- Increased awareness; more people are diagnosed
- A warming climate increases the microbe’s habitats
_______________________________
Causative: Non-cholera Vibrio species
Mode: Vehicle (food or natural bodies of water)
Virulence: N/A
Culture/Diagnosis: Culture of stool or blood
Prevention: Avoiding raw shellfish
Treatment: Doxycycline
Fever: Yes
Blood in stool: No
Distinctive Features: Sepsis can follow
Cause: 90% of seafood-related deaths in the United States
Cryptosporidium causes what, and what are the unique characteristics? (non-bacterial)
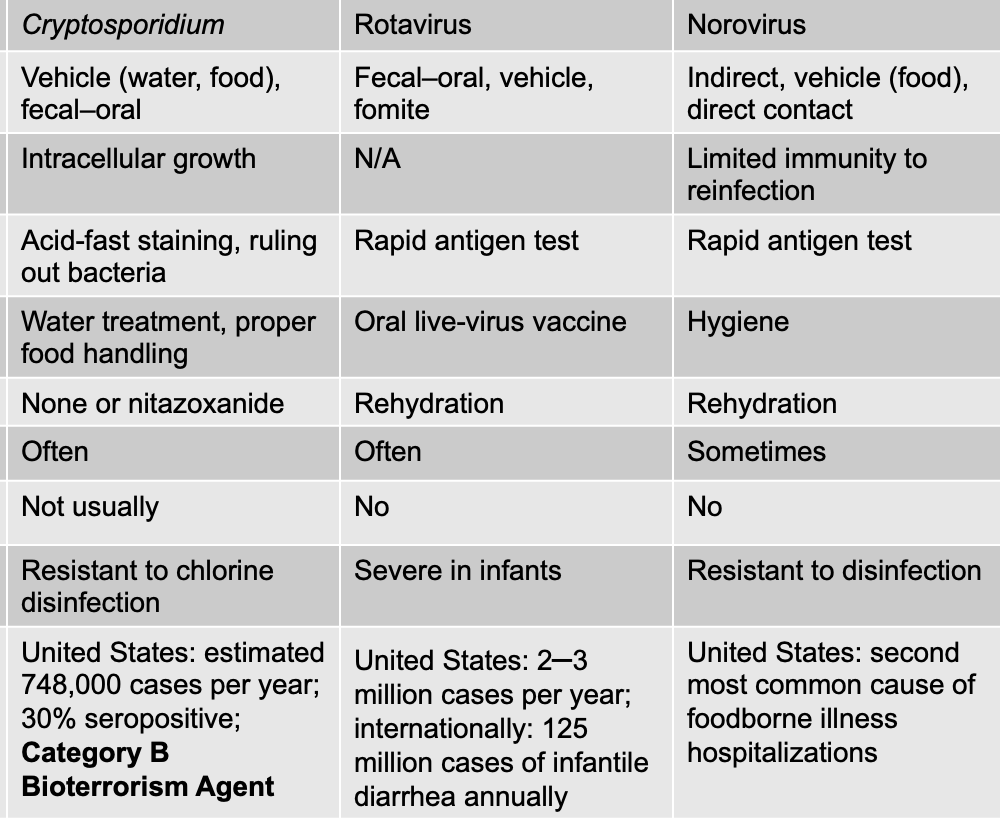
ACUTE DIARRHEA
Intestinal apicomplexan protozoan
- Hardy intestinal oocyst as well as a tissue phase
- Penetrates intestinal cell walls and lives intracellularly
- Oocysts are highly infectious and resistant to chlorine treatment
Symptoms
- headache, sweating, vomiting, severe abdominal cramps, and diarrhea
- Outbreaks associated with swimming pools
______________________________
Cryptosporidium
Vehicle (water, food), fecal–oral
Virulence: Intracellular growth
- Cryptosporidium uses intracellular growth as a virulence factor by invading the epithelial cells lining the small intestine and developing within a unique compartment just under the cell membrane. This location protects the parasite from much of the host’s immune response because it is technically inside the cell but still partly exposed to the intestinal lumen, allowing it to absorb nutrients.
Culture/Diagnosis: Acid-fast staining, ruling out bacteria
Prevention: Water treatment, proper food handling
Treatment: None or nitazoxanide
Fever: Often
Blood in stool: Not usually
Distinctive: Resistant to chlorine disinfection
United States: estimated 748,000 cases per year; 30% seropositive; Category B Bioterrorism Agent
Rotavirus causes what, and what are the unique characteristics?
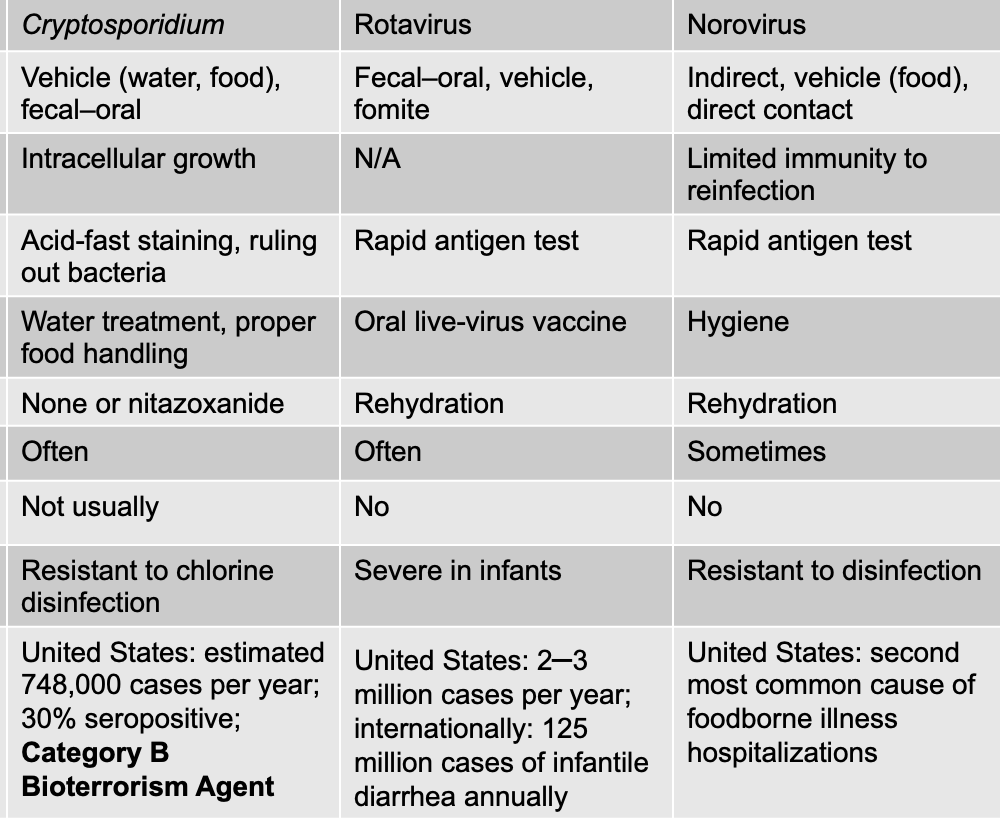
ACUTE DIARRHEA
- Double-stranded RNA genome with both an inner and outer capsid
- Primary cause of morbidity and mortality resulting from diarrhea
- 2 to 3 million cases per year, 70,000 hospitalizations
- Transmitted by fecal–oral route, including contaminated food, water, and fomites
- Children treated with ORT (Oral Rehydration Therapy)
- RotaTeq and Rotarix are live attenuated vaccines (preventative)
_____________________________
Rotavirus
Fecal–oral, vehicle, fomite
N/A
Culture/Diagnosis: Rapid antigen test
Prevention: Oral live-virus vaccine
Treatment: Rehydration
Fever: Often
Blood in stool: No
Distinctive Features: Severe in infants
United States: 2–3 million cases per year; internationally: 125 million cases of infantile diarrhea annually
Norovirus causes what, and what are the unique characteristics?
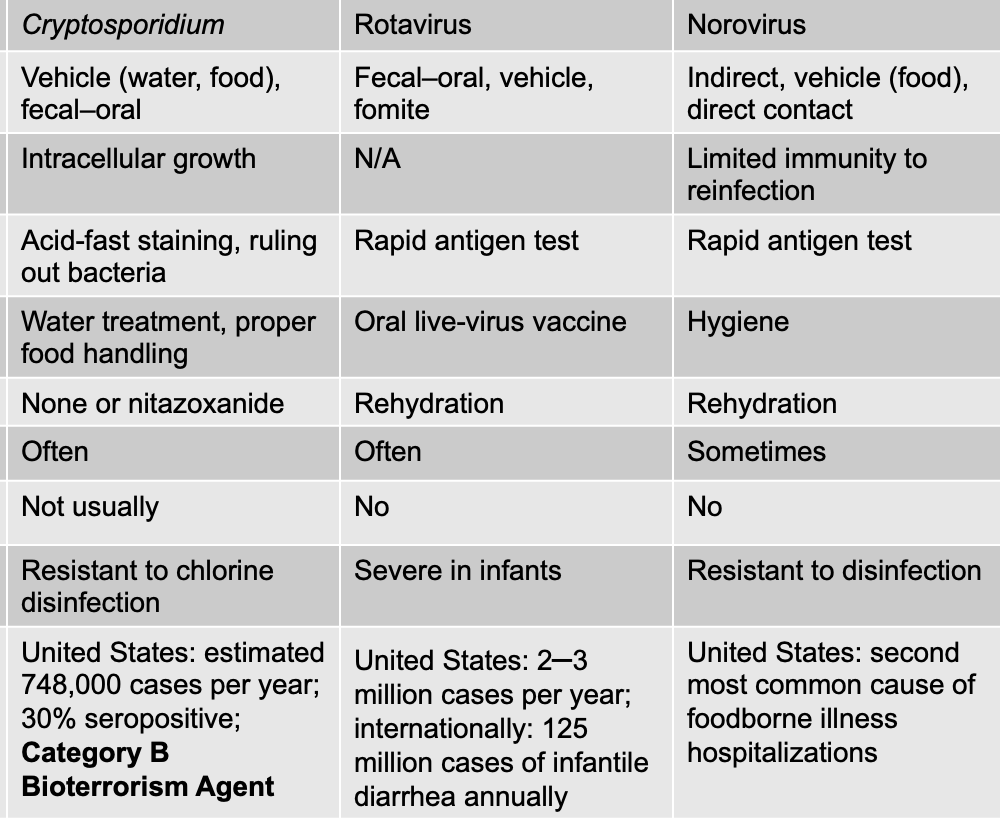
ACUTE DIARRHEA
Most common cause of foodborne disease in the United States
- Fecal–oral transmission or via contamination of food and water
- Profuse, watery diarrhea for 3 to 5 days, vomiting in the early stages, mild fever
- Low infectious dose: 1 to 20 viruses
- Many outbreaks associated with cruise ships
______________________________
Norovirus
Mode: Indirect, vehicle (food), direct contact
Virulence: Limited immunity to reinfection
- Norovirus causes only short-lived and incomplete immunity after infection, which means that even once someone recovers, they can easily get infected again. This happens because norovirus mutates rapidly, producing many different strains, and the immune response generated against one strain doesn’t protect well against others. Even immunity to the same strain fades quickly. As a result, norovirus can spread repeatedly through populations, causing frequent outbreaks in places like schools, cruise ships, nursing homes, and dorms. This ability to reinfect people over and over is a key virulence trait because it helps the virus maintain continuous transmission and makes long-term protection difficult to achieve
Culture: Rapid antigen test
Prevention: Hygiene
Treatment: Rehydration
Fever: Sometimes
Blood in stool: No
Distinctive Features: Resistant to disinfection
United States: second most common cause of foodborne illness hospitalizations
Acute diarrhea with vomiting caused by EXOTOXINS is known as __________
Food poisoning
- Nausea and vomiting accompanied by diarrhea, often companions that shared a meal suffer the same fate
- Symptoms in the gut caused by a preformed exotoxin
- Occasionally comes from non-microbial sources such as fish, shellfish, or mushrooms
- Intoxication rather than infection
What are the three agents that cause acute diarrhea with vomiting due to exotoxins (AKA food poisoning)
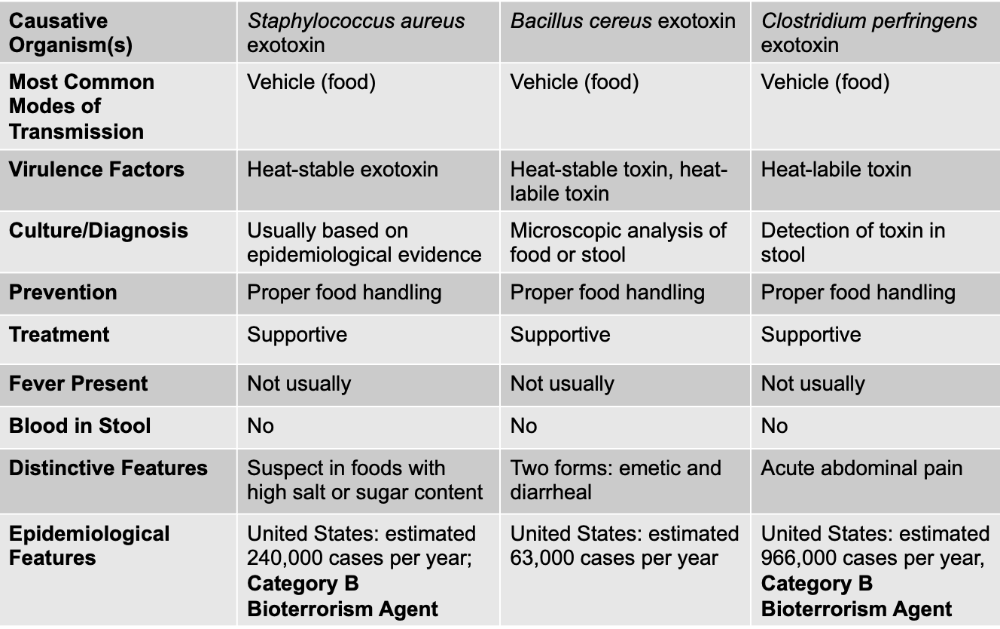
Staphylococcus aureus exotoxin
Bacillus cereus exotoxin
Clostridium perfringens exotoxin
For food poisoning illnesses caused specifically by preformed exotoxins (like Staphylococcus aureus, Bacillus cereus, and sometimes Clostridium perfringens), you do not use antibiotics because the bacteria are usually not alive or not actively infecting you when the symptoms start. The disease happens because you ate food that already contained the toxin, and once the toxin is in your gut, the symptoms occur rapidly—often within 1–6 hours. Since there is no live bacterial infection to kill, antibiotics offer no benefit and can even worsen the gut microbiome.
Staphylococcus aureus exotoxin causes what, and what are unique characteristics?
- Associated with custards, sauces, cream pastries, processed meats, chicken salad, or ham
- S. aureus thrives due to high salt tolerance
- Enterotoxin is heat stable and induces symptoms of cramping, nausea, vomiting, and diarrhea
- Onset within 1– to 6 hr, recovery within 24 hr
Self-limiting, antibiotics not warranted
- the disease resolves on its own without the need for antibiotics. The toxins cause rapid-onset vomiting, nausea, abdominal cramps, and sometimes diarrhea, but the bacteria themselves are typically not alive in the gut; only the toxins are present.
________________________________
Staphylococcus aureus exotoxin
MOT: Vehicle (food)
Virulence: Heat-stable exotoxin
Culture: Usually based on epidemiological evidence
Prevention: Proper food handling
Treatment: Supportive
Fever: Not usually
Blood in stool: No
Distinctive: Suspect in foods with high salt or sugar content
United States: estimated 240,000 cases per year; Category B Bioterrorism Agent
What are the two forms of food poisoning by bacillus cereus exotoxin?
Sporulating gram-positive bacterium that lives in the soil
- Emetic (vomiting) form most frequently tied to fried rice that has been cooked and kept warm for long periods of time
- Diarrheal form associated with cooked meats or vegetables held at a warm temperature for long periods of time
- Profuse, watery diarrhea that lasts about 24 hr
Bacillus cereus exotoxin causes what, and what are unique characteristics?
Sporulating gram-positive bacterium that lives in the soil
- Emetic (vomiting) form most frequently tied to fried rice that has been cooked and kept warm for long periods of time
- Diarrheal form associated with cooked meats or vegetables held at a warm temperature for long periods of time
- Profuse, watery diarrhea that lasts about 24 hr
____________________________
Bacillus cereus exotoxin
MOT: Vehicle (food)
Virulence: Heat-stable toxin, heat-labile toxin (easily destroyed)
Culture: Microscopic analysis of food or stool
Prevention: Proper food handling
Treatment: Supportive
Fever: Not usually
Blood in stool: No
Distinctive: Two forms: emetic and diarrheal
United States: estimated 63,000 cases per year
Clostridium perfringens exotoxin causes what, and what are unique characteristics?
- Also the causative agent of gas gangrene
- Contaminates meat, fish, and beans that have not been cooked thoroughly enough to destroy endospores
- Endospores germinate in foods, C. perfringens cells enter the small intestine and release exotoxin
- Abdominal pain, diarrhea, and nausea in 8 to 16 hr
- Also causes enterocolitis similar to that caused by C. difficile
_____________________________________
Clostridium perfringens exotoxin
Vehicle (food)
Virulence: Heat-labile toxin (destroying)
Culture: Detection of toxin in stool
Prevention: Proper food handling
Treatment: Supportive
Fever: Not usually
Blood in stool: No
Distinctive: Acute abdominal pain
United States: estimated 966,000 cases per year, Category B Bioterrorism Agent
Chronic diarrhea is diarrhea that lasts longer than ______
14 days
Can have an infectious or noninfectious cause
- Irritable bowel syndrome, ulcerative colitis (IBS or UC)
- Microbes in this section cause chronic diarrhea in otherwise healthy people
Giardia duodenalis causes what, and what are the unique characteristics?
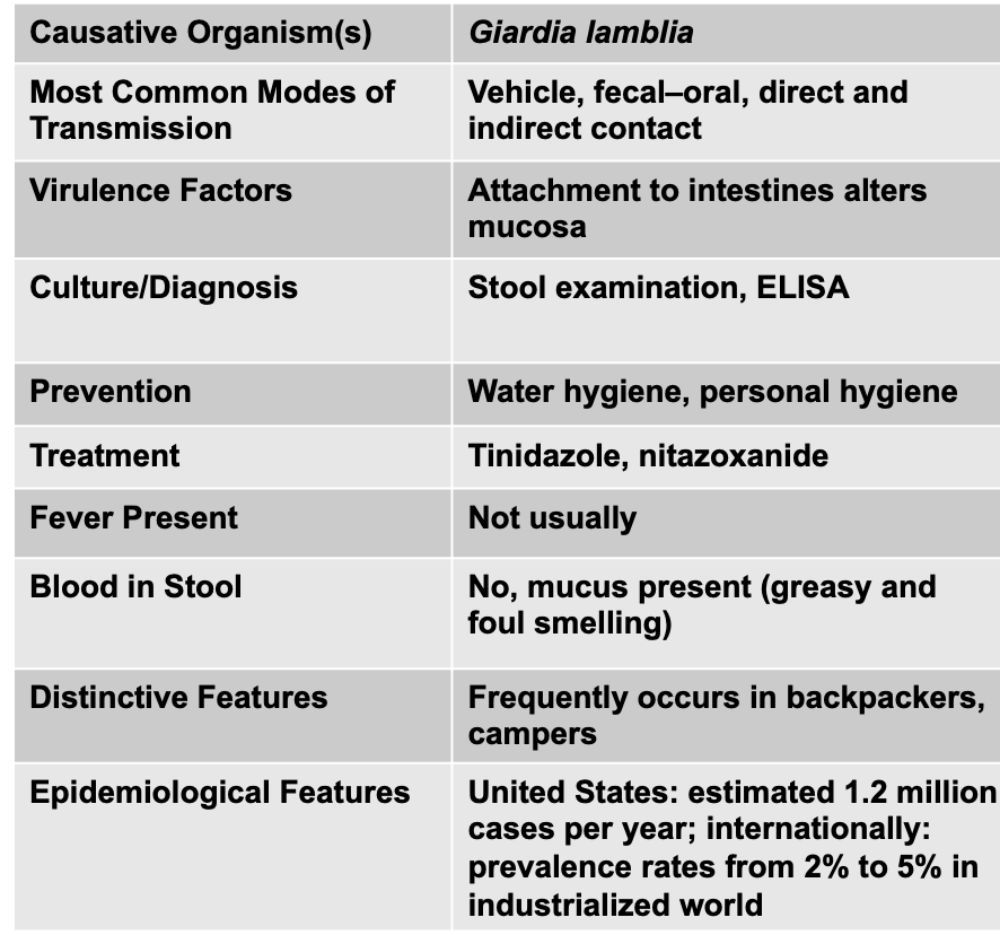
- Known as Giardia intestinalis and Giardia lamblia
- Pathogenic flagellated protozoan
- Identifiable by its unique symmetrical heart shape with organelles positioned in such a way that it resembles a face with four pairs of flagella emerging from the ventral surface
Signs and symptoms: diarrhea of long duration, abdominal pain, flatulence; greasy, and malodorous stools
Complex epidemiological pattern:
- Isolated from beavers, cattle, coyotes, cats, and human carriers
- Cysts survive for up to 2 months in the environment
- Epidemics traced to water from mountain streams as well as chlorinated municipal water
________________________________
Giardia lamblia
Mode of Transmission: Vehicle, fecal–oral, direct and indirect contact
Culture/Diagnosis: Attachment to intestines alters mucosa
Culture/Diagnosis: Stool examination, ELISA
Prevention: Water hygiene, personal hygiene
Treatment: Tinidazole, nitazoxanide
Fever: Not usually
Blood in stool: No, mucus present (greasy and foul smelling)
Distinctive: Frequently occurs in backpackers, campers
United States: estimated 1.2 million cases per year; internationally: prevalence rates from 2% to 5% in industrialized world
What is hepatitis? What does it lead to?
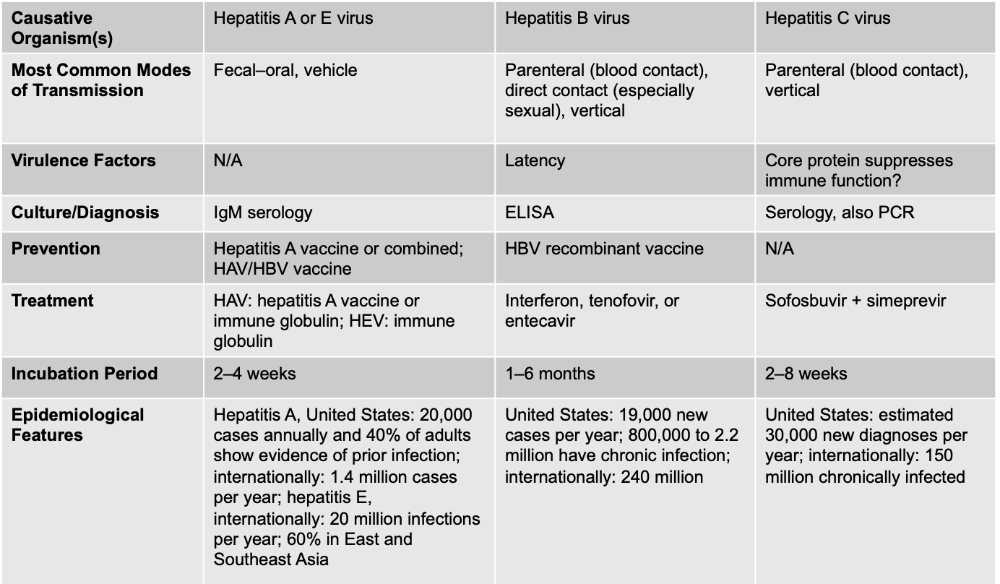
Inflammation of the liver
- Necrosis of hepatocytes
- Response by mononuclear WBCs that swells and disrupts the liver architecture
- Interferes with excretion of bile pigments and causes bilirubin to accumulate in blood and tissues, causing jaundice
Hepatitis A (or E) virus causes what, and what are the unique characteristics?
- Nonenveloped, single-stranded RNA enterovirus
Signs and symptoms:
- Subclinical or vague, flu-like symptoms
- Jaundice in only 10% of cases
Transmission and epidemiology:
- Fecal–oral route, associated with deficient personal hygiene and lack of public health measures
Immunizations are available
________________________________
Hepatitis A or E virus
MOT: Fecal–oral, vehicle
Virulence: N/A
Culture/Diagnosis: IgM serology
Prevention: Hepatitis A vaccine or combined; HAV/HBV vaccine
Treatment: HAV: hepatitis A vaccine or immune globulin; HEV: immune globulin
Incubation Period: 2–4 weeks
Epidemiological: Hepatitis A, United States: 20,000 cases annually and 40% of adults show evidence of prior infection; internationally: 1.4 million cases per year; hepatitis E, internationally: 20 million infections per year; 60% in East and Southeast Asia
Hepatitis B virus causes what, and what are the unique characteristics?
- Enveloped DNA virus
Signs and symptoms:
- Fever, chills, malaise, anorexia, abdominal discomfort, diarrhea, and nausea
- Rashes and arthritis may occur
- Cause of hepatocellular carcinoma
- Transmitted by minute amounts of blood
An effective vaccine is available
- Important for health care workers and students, patients receiving multiple transfusions, immunodeficient persons, and cancer patients
_______________________________
Hepatitis B virus
MOD: Parenteral (blood contact), direct contact (especially sexual), vertical
Virulence: Latency
Culture: ELISA
Prevention: HBV recombinant vaccine
Treatment: Interferon, tenofovir, or entecavir
Incubation Period: 1–6 months
Epidemiological: United States: 19,000 new cases per year; 800,000 to 2.2 million have chronic infection; internationally: 240 million
Hepatitis C virus causes what, and what are the unique characteristics?
Silent epidemic: 3.5 million Americans infected
Signs and symptoms:
- Similar to hepatitis B virus
- 75% to 85% remain infected indefinitely
Transmission and epidemiology:
- Blood transfusions, needle sharing
Treatment:
- No vaccine available
- Two-drug regimen: Sofosbuvir (a nucleotide analog that “fools” the RNA polymerase of the virus) and simeprevir (a protease inhibitor)
________________________________
Hepatitis C virus
MOT: Parenteral (blood contact), vertical
Virulence: Core protein suppresses immune function?
Culture: Serology, also PCR
Prevention: N/A
Treatment: Sofosbuvir + simeprevir
Incubation: 2–8 weeks
United States: estimated 30,000 new diagnoses per year; internationally: 150 million chronically infected
Which hepatitis has a vaccine available?
A
B (important for healthcare workers)
Which virus is an enveloped virus?
B - enveloped, DNA
C - enveloped RNA
Which virus is non-eveloped
A - non-enveloped, ssRNA
Which hepatitis is a silent epidemic?
Which hepatitis can cause hepatocellular carcinoma
Silent - C
Carcinoma - B
Hepatitis C is called the “silent killer” not because of its incubation period, but because of its long-term, symptomless progression. While Hepatitis B does have a longer incubation period before acute symptoms appear, most people with Hepatitis B either clear the infection or develop symptoms early enough to be diagnosed. In contrast, Hepatitis C infection often causes no noticeable acute symptoms at all, and people can stay infected for 10–30 years without knowing it while the virus quietly causes chronic inflammation, fibrosis, and eventually cirrhosis or liver cancer. By the time symptoms appear, significant and sometimes irreversible liver damage has already occurred. The “silent killer” nickname refers to this decades-long asymptomatic period that leads to severe chronic disease—not the length of the incubation period.
PRIOR TO THIS, all the GI disease were non-helminthic diseases, moving forward they are helminthic diseases
KEEP GOING!!
What is a hallmark of helminthic infections? Helminths parasitize humans
- Eosinophilia is a hallmark of helminthic infection
- Eosinophilia means you have more eosinophils than normal in your blood. Eosinophils are a type of white blood cell your body uses to fight parasites, allergies, and some infections.
Neglected tropical infections:
- Cause a large burden of disease in the poorest countries in the world
- Receive the least recognition and research funding
What are the general pathogenesis and virulence factors for helminths?
Virulence
- Specialized mouthparts for attachment and feeding, enzymes to liquefy and penetrate tissues, and cuticle for protection from host defenses
- Definitive host: host in which the adult worm reproduces sexually
Diagnosis
- Eosinophilia
- Discovery of eggs, larvae, or adult worms in stool or tissues
What is the general prevention and treatment for helminth infections?
- NO vaccines available
- Regular treatment with antihelminthic drugs
Prevention
- Proper sewage disposal
- Avoiding using human feces as fertilizer
- Disinfection of the water supply
- Thoroughly washing and cooking vegetables and meats
- Freezing food
What are the four basic helminth life cycles?
- Cycle A involves fecal–oral transmission, where the helminth’s eggs are released in feces, mature in the environment, and infect a new host when swallowed. This is the cycle for Ascaris, Trichuris, and Enterobius.
- Cycle B requires the parasite to enter through the skin; the infective larvae develop in the environment and actively penetrate human skin, then migrate through the bloodstream to the intestines. This applies to hookworms (Necator, Ancylostoma) and Strongyloides.
- Cycle C involves a vertebrate intermediate host—usually cattle, pigs, or fish—where larvae develop in the tissues. Humans become infected by eating undercooked meat from the intermediate host. Tapeworms like Taenia and Diphyllobothrium follow this cycle.
- Cycle D uses an insect vector that carries and transmits the infective stage to humans through a bite. Filarial worms like Wuchereria and Onchocerca are the classic examples.
- But in cycle D, the parasite cannot reach the human host on its own; it relies on an arthropod, like a mosquito, blackfly, or sandfly, to carry the infective stage and deposit it into the human’s bloodstream or tissues during a bite. This distinction is important because it changes prevention strategies—vector control is key for cycle D, whereas hygiene or protective footwear is more relevant for cycles A and B.
In cycle A, the worm develops in the _________.
Eggs are released with _____ into the environment.
Eggs are _______ by new host and hatch in intesine.
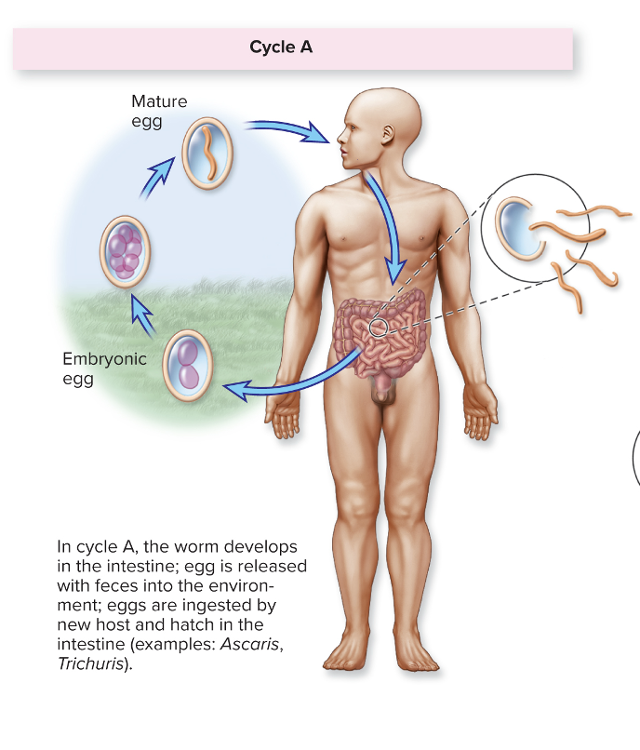
intestines
feces
ingested
In cycle B, the worms mature in the ______, eggs are released with ______
Larvae hatch and develop in the ______, and infection occurs through _______ by ________-
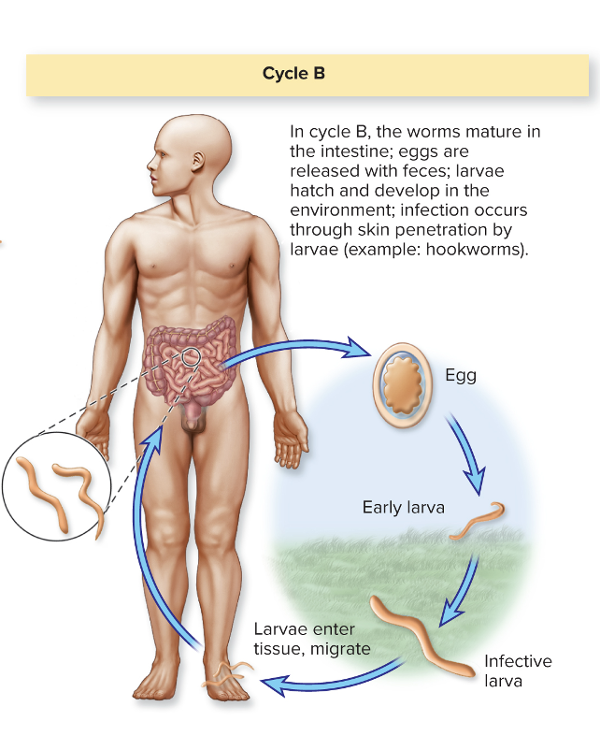
intestines; feces
environment; skin penetration by larvae
In cycle C, the adult matures in human ______; eggs are released with _____ into the environment
Eggs are eaten by ________; larval forms encyst in tissue
Humans eating ____ are infected.
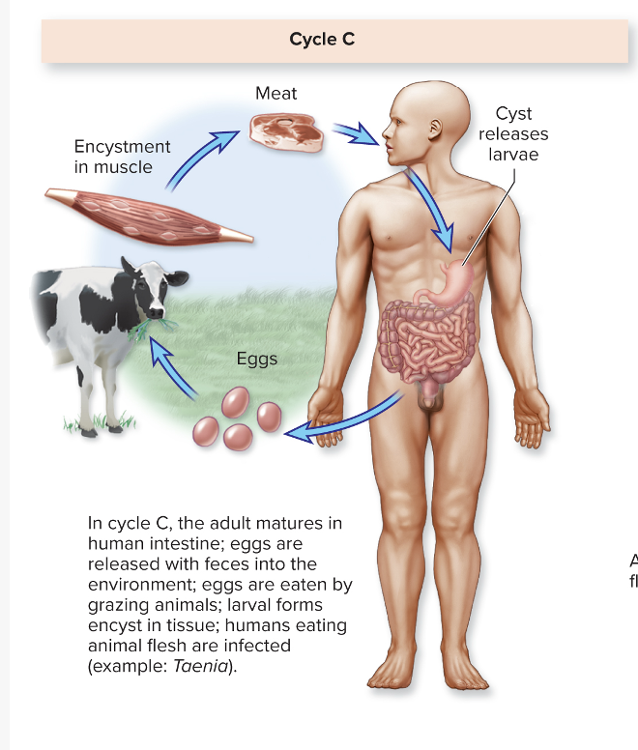
intestine; feces
grazing animals
animal flesh
In cycle D, eggs are released with ____.
Humans are infected through ______ or ________ by larval phase.
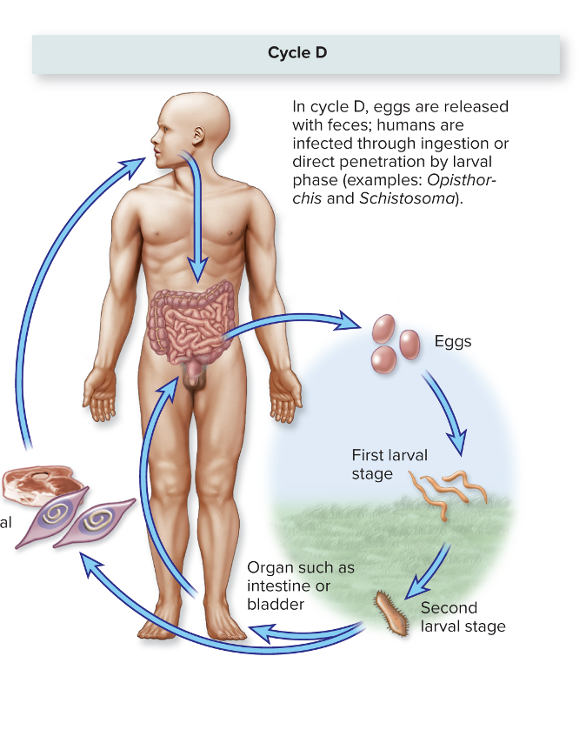
feces
ingestion or direct penetration
Schistosoma
Enterobius vermicularis causes what, and what are the unique characteristics...
Disease: INTESTINAL DISTRESS
Pinworms
- Most common cause of worm disease of children in TEMPERATE zones
- Life cycle A
- Hallmark symptom: pronounced anal itching
- Infection is not fatal and most cases are asymptomatic
- When one member of the family is diagnosed, the entire family should be tested and/or treated because it is likely that multiple members are infected
_______________________________
Enterobius vermicularis (pinworm)
MOT: Cycle A: vehicle (food, water), fomites, self-inoculation
Virulence: N/A
Culture/Diagnosis: Adhesive tape + microscopy
Prevention: Hygiene
Treatment: Mebendazole, piperazine
Distinctive: Common in the United States
United States: up to 40 million cases per year
Hallmark anal itching is the hallmark symptom for which causative agent...
Enterobius vermicularis
Taenia solium causes what, and what are the unique characteristics?
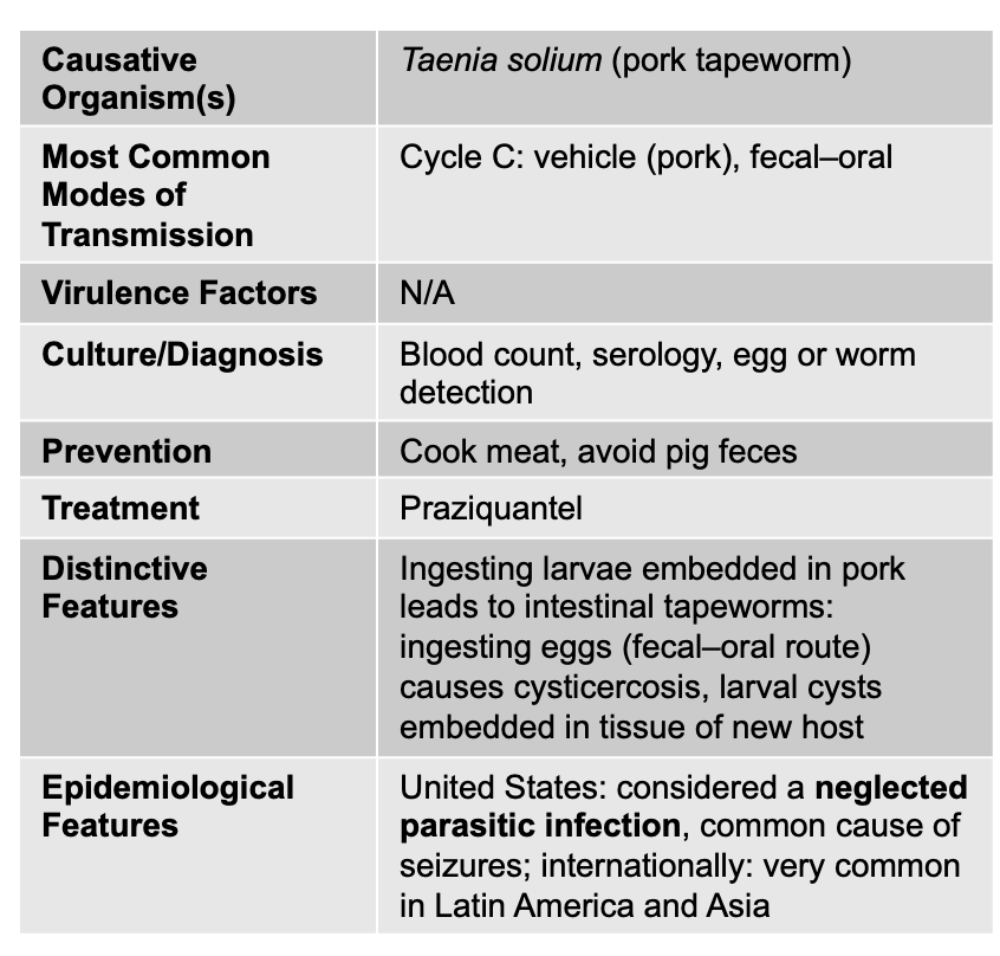
Cysticercosis
Tapeworm:
- Adult worms are up to 5 m long
- Distributed worldwide, but concentrated in areas where humans live in close proximity with pigs or eat undercooked pork
- Life cycle C
- Cysticercosis occurs when humans ingest tapeworm eggs rather than infected meat
______________________________
Taenia solium (pork tapeworm)
Cycle C: vehicle (pork), fecal–oral
N/A
Blood count, serology, egg or worm detection
Cook meat, avoid pig feces
Praziquantel
Ingesting larvae embedded in pork leads to intestinal tapeworms: ingesting eggs (fecal–oral route) causes cysticercosis, larval cysts embedded in tissue of new host
United States: considered a neglected parasitic infection, common cause of seizures; internationally: very common in Latin America and Asia
Fasciola hepatica causes what, and what are the unique characteristics?
Liver and Intestinal Disease
- Liver fluke common in sheep, cattle, goats, and other mammals
- Outbreaks associated with eating wild watercress (plant)
- Complex life cycle, mammal is the definitive host
Symptoms
- Vomiting, diarrhea, hepatomegaly, and bile obstruction if infected with a large number of flukes
________________________________
Fasciola hepatica
Cycle D: vehicle (water and water plants)
Virulence: N/A
Blood count, serology, egg or worm detection
Prevention: Sanitation of water
Treatment: Triclabendazole
Distinctive Features: Live in liver and gallbladder
Epidemiological: United States: most cases imported; internationally: 56 million infected
Schistosoma masoni and S. japonicum causes what, and what are the unique characteristics?
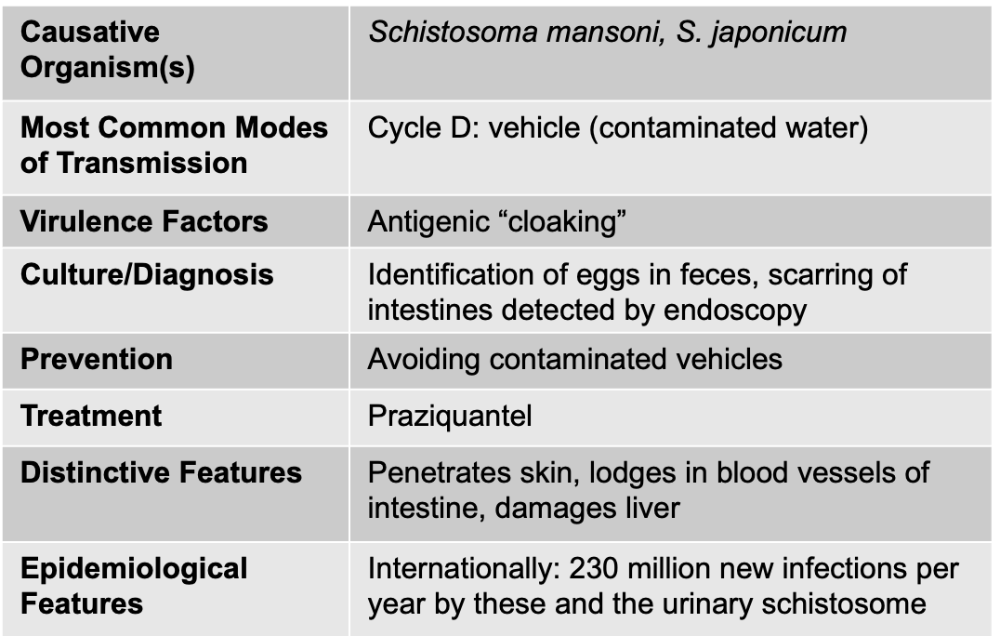
Liver Disease: Schistosomiasis
- Morphologically and geographically distinct
- Similar life cycles, transmission methods, and disease manifestations
- Can invade intact skin
Signs/Symptoms
- Itchiness in the area where the worm enters the body, fever, chills, diarrhea, and cough
- Chronic infection: hepatomegaly, liver disease, splenomegaly
- Bladder obstruction, and blood in the urine
- Can cause a granulomatous response in the nervous system and heart
Pathogenesis/Virulence Factors
- Parasite coats its outer surface with proteins from the bloodstream, cloaking itself from the host defense system
- Diagnosed through identifying eggs in urine or feces
- Cycle of infection cannot be broken as long as people are exposed to untreated sewage
Clostridioides difficile
Gram-Positive, Endospore-Forming Bacteria
Antibiotic-associated diarrhea
Bacillus cereus
Gram-Positive, Endospore-Forming Bacteria
Food poisoning
Clostridium perfringens
Gram-Positive, Endospore-Forming Bacteria
Food poisoning
Streptococcus mutans
Gram Positive
Dental caries
Staphylococcus aureus
Gram Positive
Food poisoning
Helicobacter pylori
Gram Negative
Gastritis/Gastric Ulcers
Salmonella
Gram Negative
Acute Diarrhea
Shigella
Gram Negative
Acute diarrhea and dysentery
Escherichia coli STEC
Gram Negative
Acute diarrhea plus hemolytic syndrome
Other E. coli
Gram Negative
Acute or chronic diarrhea
Campylobacter jejuni
Gram Negative
Acute diarrhea
Vibrio cholera
Gram Negative
Acute Diarrhea
Cholera
Non-cholera Vibrio species
Gram Negative
Vibrioses
Acute Diarrhea
Hepatitis B virus
DNA viruses
“Serum” hepatitis
Mumps Virus
RNA virus
Rotavirus
RNA virus
Acute diarrhea
Norovirus
RNA virus
Acute diarrhea
Hepatitis A
RNA
Infectious hepatitis
Hepatitis E
RNA
Infectious hepatitis
Hepatitis C
RNA "serum hepatitis"
Cryptosporidium
Protozoa
Acute diarrhea
Giardia duodenalis
Chronic Diarrhea
Protozoa
Enterobius vermicularis
Helminths - nematodes (roundworms, pinworms)
Intestinal Distress
Taenia solium
Helminths - Cestodes (flatworms), segmented
Cysticercosis
Fasciola hepatica
Helminths -Trematodes
unsegmented flat worms)
Liver and intestinal disease
Schistosoma mansoni,
S. japonicum
Helminths -Trematodes (unsegmented flat worms)
Schistosomiasis