Instructions for Side by Side Printing
- Print the notecards
- Fold each page in half along the solid vertical line
- Cut out the notecards by cutting along each horizontal dotted line
- Optional: Glue, tape or staple the ends of each notecard together
Microbiology Exam 3 Review - Chapter 10 (Microbial Metabolism) + 23 (GI) Flashcards
front 1 Chapter 10 | back 1 Microbial Metabolism |
front 2 What is metabolism? | back 2 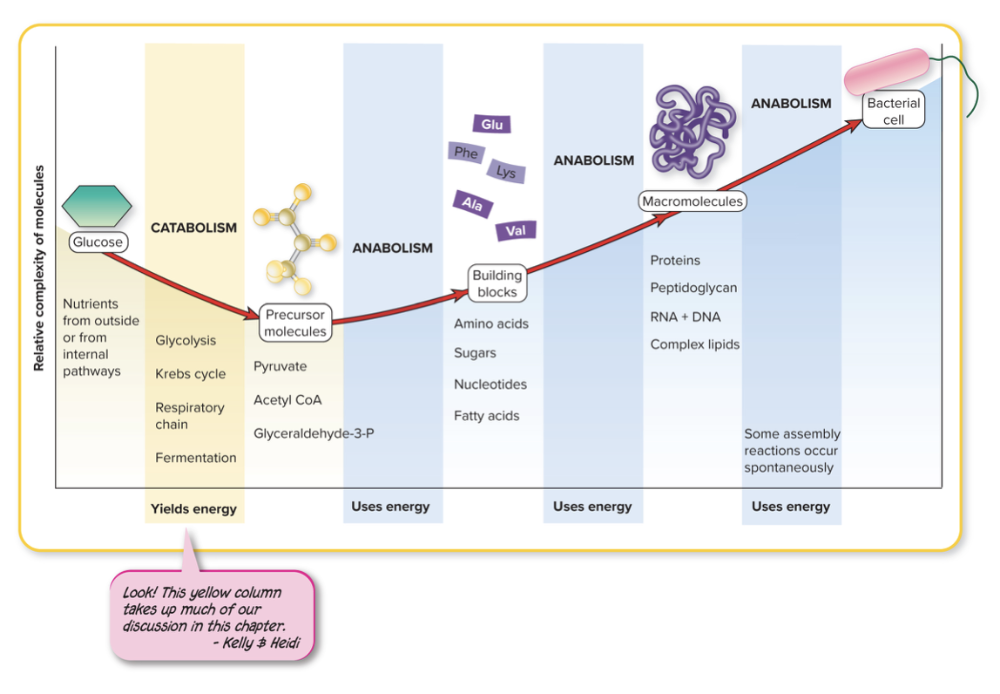 All the chemical reactions and physical workings of the cell. - Anabolic and Catabolic Reactions - Collects and spends energy in the form of ATP or heat |
front 3 What is anabolism? | back 3 The building of molecules Biosynthesis: synthesis of cell molecules and structures REQUIRES energy input
|
front 4 What is catabolism? | back 4 The breaking of the bonds of larger molecules RELEASES energy
|
front 5 What are catalysts? | back 5 Speed up the rate of a chemical reaction without becoming part of the products or being consumed in the reaction |
front 6 How are enzymes catalysts? | back 6 Enzymes speed up a chemical reaction by LOWERING the activation energy allowing the reaction to proceed by
|
front 7 What are the basic characteristics for an enzyme? | back 7
|
front 8 How do enzymes work? | back 8 A substrate, which is the reactant molecule, binds to the active site of the enzyme and acts accordingly Enzymes bind to substrate and participate directly in changes to the substrate BUT enzymes DO NOT become part of the product, get used up, or changed and can be RECYCLED |
front 9 Most enzymes are ________ molecules. What's the difference between simple and conjugated enzymes? | back 9 protein Simple enzymes - protein alone Conjugated enzymes - contain protein and some other nonprotein molecule |
front 10 When the protein is whole, meaning it has the nonprotein and protein portion (cofactors) is it called _____ | back 10 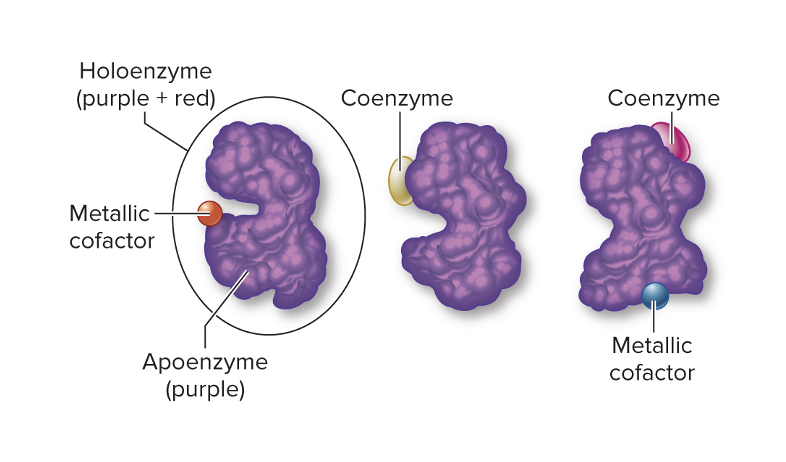 holoenzyme |
front 11 Only the protein portion of the holoenzyme is called the ______ | back 11 apoenzyme |
front 12 The non-protein portion of the holoenzyme is called the ___ | back 12 Cofactor This can be an organic molecule (coenzyme) or an inorganic (metal ions) |
front 13 Apoenzymes are _____ | back 13 the protein portion of the holoenzyme This is where the active site or catalytic site resides
Each enzyme has a different:
|
front 14 Cofactors which are part of the non-protein part of the holoenzyme can include ________ and _______ | back 14 1. Metal ions (metallic cofactors)
Assist with precise functions between enzyme and substrate
2. Coenzymes (organic compounds)
|
front 15 ____________ transfer electrons from one substrate to another, and ______________ transfer a hydrogen from one compound to another | back 15 Oxidoreductases (Oxidation is LOSS of elections, a compound that loses electrons is oxidized AND Reduction is gaining electrons and a compound that gains electrons is REDUCED) **NAD and FAD are coeznyme carriers dehydrogenases |
front 16 What are some examples of oxidoreductase enzymes? | back 16 1. Lactate dehydrogenase Substrate: pyruvic acid Action: Catalyzes the conversion of pyruvic acid to lactic acid 2. Oxidase Substrate: O2 (molecular oxygen) Action: Catalyzes the reduction of O2 (addition of electrons and hydrogen) |
front 17 _________ transfer functional groups from one substrate to another. What is an example? | back 17 Transferases 1. DNA Polymerase Substrate: DNA nucleosides Action: Synthesizes a strand of DNA using the complementary strand as a model |
front 18 ____________ cleave bonds on molecules with the addition of water What's an example? | back 18 Hydrolases cleave bonds on molecules with the addition of water 1. Lactase Substrate: Lactose Action: Breaks lactose down into glucose and galactose 2. Penicillinase Substrate: Penicillin Action: Hydrolyzes beta-lactam ring |
front 19 __________ add groups to or remove groups from double-bonded substrates | back 19 Lyases |
front 20 ____________ change a substrate to its isomeric form | back 20 Isomerases |
front 21 ___________ catalyze the formation of bonds with the input of ATP and the removal of water | back 21 Ligases |
front 22 Where are enzymes found? | back 22 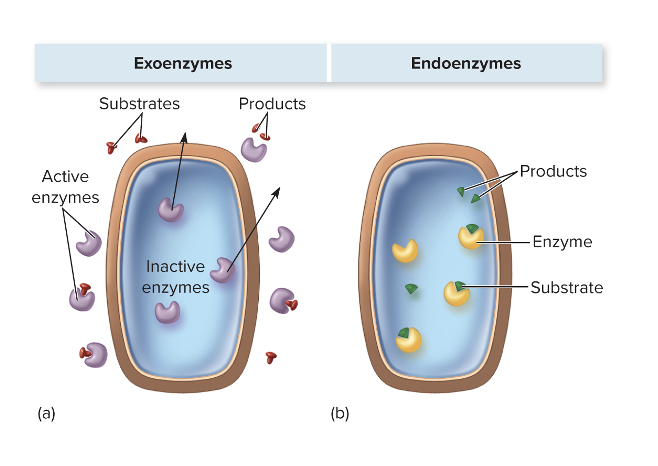 They can be exoenzymes or endoenzymes, and it depends on the microbe as well as the function of the enzyme. Enzymes can be found inside or outside microbial cells, depending on their type and purpose. Endoenzymes are located inside the cell and carry out reactions necessary for the microbe’s metabolism, like breaking down nutrients for energy or synthesizing cellular components. Exoenzymes, on the other hand, are secreted outside the cell to break down large molecules in the environment into smaller pieces that the microbe can absorb. Whether a microbe produces endoenzymes, exoenzymes, or both depends on the species and the function of the enzyme—for example, pathogens often secrete exoenzymes like proteases or hyaluronidase to invade host tissues. |
front 23 What are EXOenzymes? | back 23 These are enzymes that are meant to be sent (or active) when outside the cell
Examples These break down large molecules in the environment so the microbe can absorb them or help it invade host tissues. Examples include:
In short, endoenzymes help the microbe survive and grow inside itself, while exoenzymes interact with the environment or host. |
front 24 What are ENDOenzymes? | back 24
Examples
|
front 25 What are constitutive enzymes? | back 25 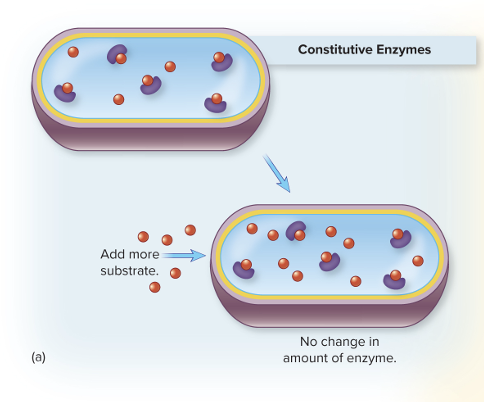 Always present in relatively constant amounts, regardless of the cellular environment
|
front 26 What are regulated enzymes? | back 26 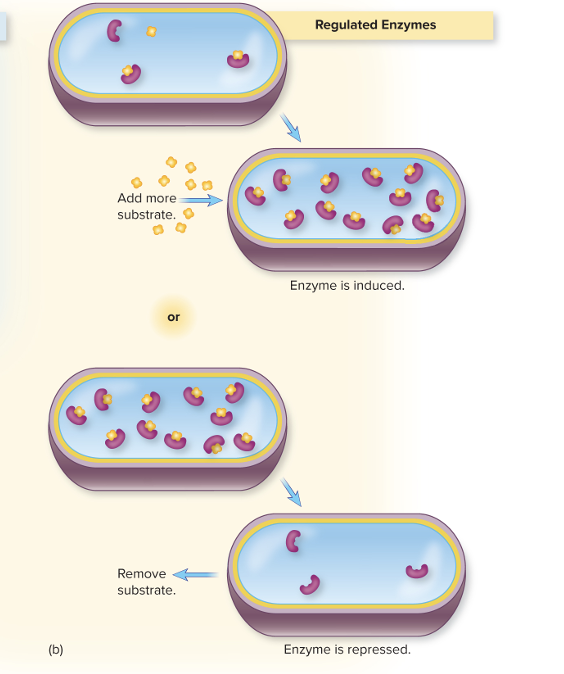 Production is turned on (induced) or turned off (repressed) in response to changes in concentration of substrate
|
front 27 What is the role of microbial enzymes in disease? | back 27
Enzyme Examples
|
front 28 __________ is a term that explains how changes from normal conditions can make enzymes chemically unstable | back 28 Labile
|
front 29 What is denaturation? | back 29
|
front 30 Metabolic reactions most often occur in a _______ or pathway. Each step is ______ by an ________. | back 30 multi-step series
|
front 31 True or False: Many metabolic pathways have branches that have alternate methods for nutrient processing. | back 31 True Protein catabolism (divergent) and anabolism (convergent) like amino acid synthesis are branched pathways |
front 32 True or False: No metabolic pathways follow a cyclic form. | back 32 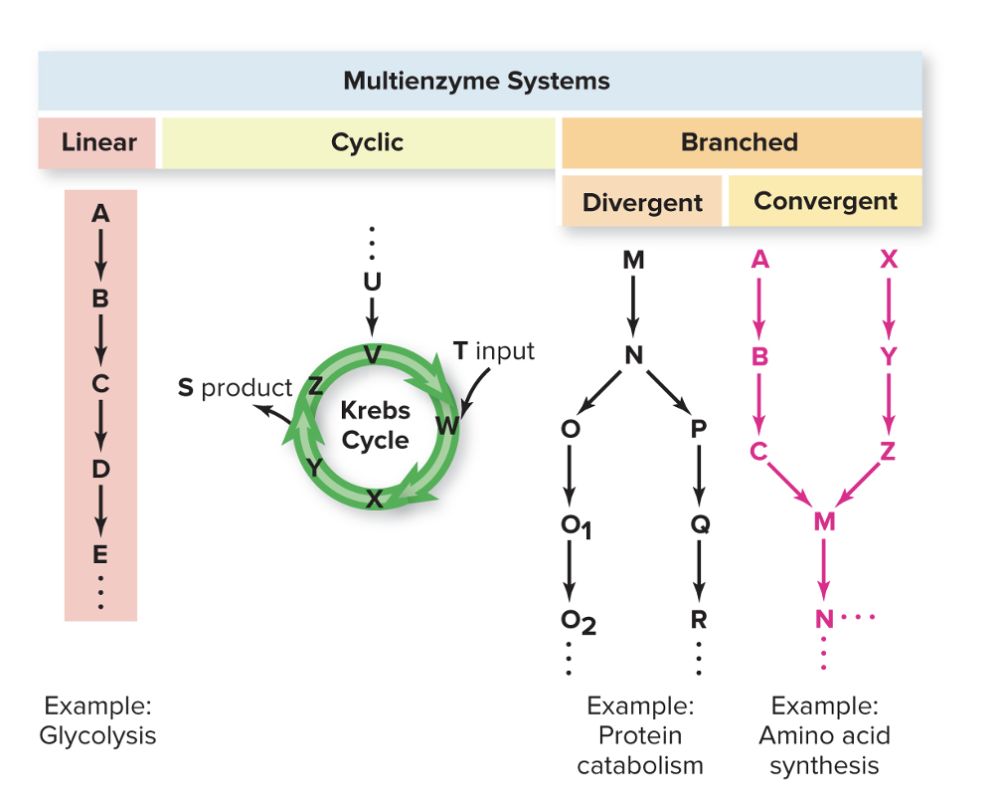 False
|
front 33 _____ is a cyclic cycle. | back 33 Krebs Cycle |
front 34 Glycolysis is a ______ cycle. | back 34 Linear |
front 35 What is competitive inhibition? | back 35
|
front 36 What is noncompetitive inhibition? | back 36
Example – Allolactose (allosteric proteins) binds to that allosteric protein, causing conformational change and protein can no longer bind to operator In noncompetitive inhibition, the inhibitor binds to an allosteric site (a site other than the active site), which changes the enzyme’s shape and reduces its activity. The substrate can still bind to the active site, but the enzyme’s ability to catalyze the reaction is diminished. Depending on the inhibitor concentration and the enzyme’s properties, activity can be partially reduced or nearly completely inhibited, but it usually doesn’t fully stop all enzyme molecules unless the inhibitor is very abundant or has very high affinity. |
front 37 Compare and contrast competitive and noncompetitive inhibition? | back 37 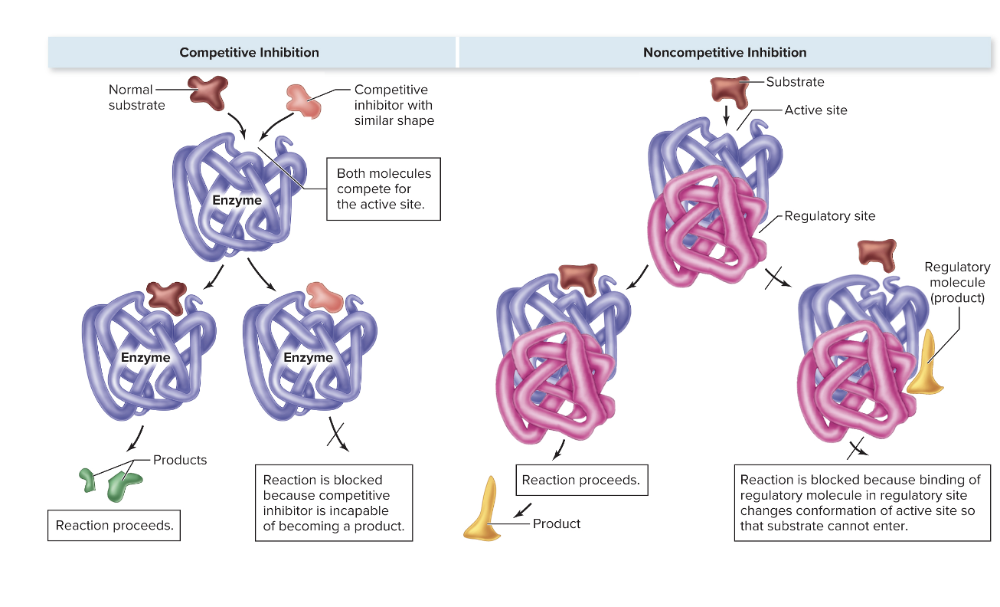 |
front 38 What is enzyme repression? How is this different from feedback inhibition? | back 38 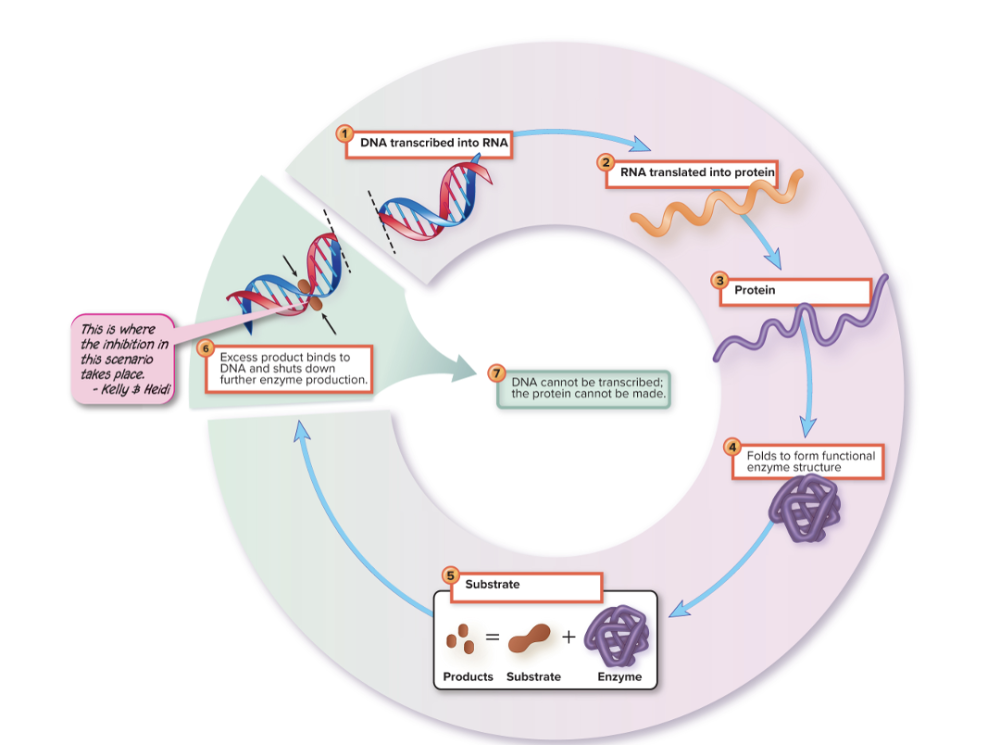 Stops further synthesis of an enzyme somewhere along its pathway
What you’re describing is repression, which is different from feedback inhibition. Repression stops further synthesis of an enzyme at the genetic level: if the end product of a pathway accumulates, it signals the cell to suppress transcription or translation of the enzyme’s gene. This means no new enzyme molecules are made, so the effect is long-lasting. In contrast, feedback inhibition works at the enzyme activity level, not the gene level. It’s immediate: the end product binds to an existing enzyme to slow or stop its activity, but it doesn’t affect how much enzyme is being produced. Because repression controls enzyme production, its response time is slower than feedback inhibition, but the effect is more enduring since fewer enzymes are synthesized over time. |
front 39 What is enzyme induction? | back 39 Enzyme induction: enzymes appear (are induced) only when suitable substrates are present
substrate → activates transcription factor → increases enzyme synthesis. The key is that induction is responsive to the environment and only produces the enzyme when it’s needed. |
front 40 What are exergonic reactions? | back 40
EXAMPLES
|
front 41 What are endergonic reactions? | back 41
EXAMPLES
|
front 42 True or False: Exergonic and endergonic reactions are often coupled | back 42 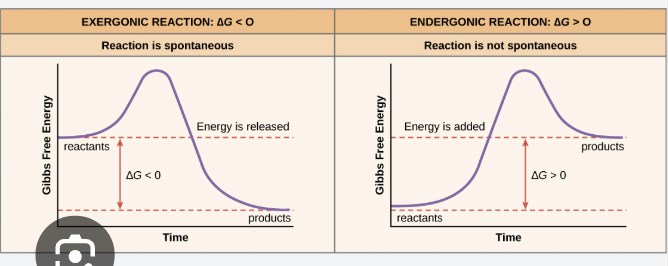 True |
front 43 Redox reactions always occurs in __________ | back 43 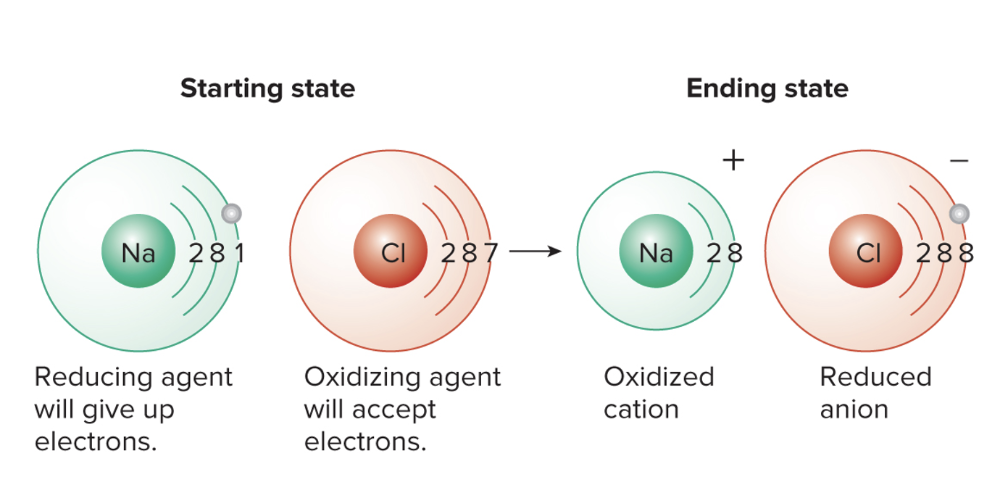 pairs called redox pairs. There is generally an electron donor and electron acceptor
|
front 44 What are some common electron carriers? | back 44 NAD:
FAD:
NADP:
|
front 45 What happens in catabolic pathways? What are the two types of metabolisms? | back 45 Catabolic pathways:
|
front 46 What is ATP, what is it made out of, and how does it serve as an energy source? | back 46 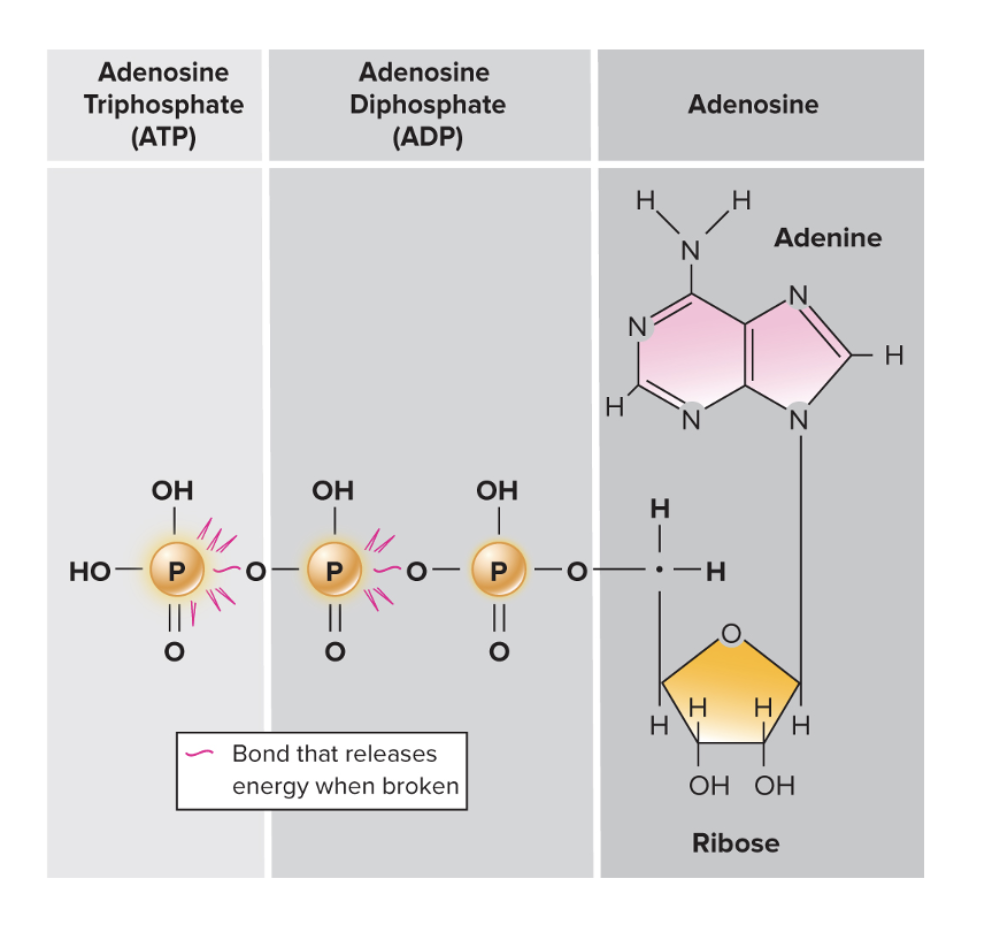 Three-part molecule: Adenosine Triphosphate
Three phosphate groups bonded to the ribose
Primary energy currency of the cell
ATP (adenosine triphosphate) serves as the primary energy currency of the cell because it stores energy in the high-energy phosphate bonds between its three phosphate groups. When the terminal phosphate bond is broken through hydrolysis (ATP → ADP + Pi), a significant amount of free energy is released |
front 47 What is substrate-level phosphorylation? | back 47 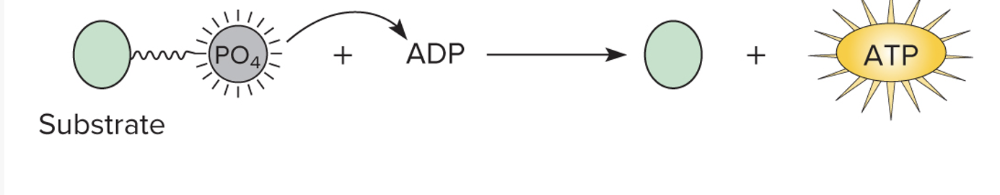
|
front 48 What is oxidative phosphorylation? | back 48 A series of redox reactions occurring during the final phase of the respiratory pathway Oxidative phosphorylation is the process your cells use to make most of their ATP. It happens in the mitochondria, where electrons from molecules like NADH and FADH₂ are passed along the electron transport chain. As the electrons move, they help pump protons across the mitochondrial membrane, creating a proton gradient. This gradient stores potential energy, and when protons flow back through ATP synthase, it drives the production of ATP from ADP and inorganic phosphate. Essentially, oxidative phosphorylation converts the energy from food molecules into usable ATP by using an electron flow to power a molecular “turbocharger.” The electron transport chain (ETC) takes place in the inner mitochondrial membrane, where electrons from NADH and FADH₂ are passed along a series of protein complexes. As electrons move through the chain, these complexes pump protons from the mitochondrial matrix into the intermembrane space, creating a proton gradient. This gradient stores potential energy, which is then used to drive protons back through ATP synthase. The flow of protons through ATP synthase powers the conversion of ADP and inorganic phosphate into ATP, making it the main way cells produce energy in the form they can use. |
front 49 What is photophosphorylation? | back 49
|
front 50 What are the three main pathways of catabolism? | back 50 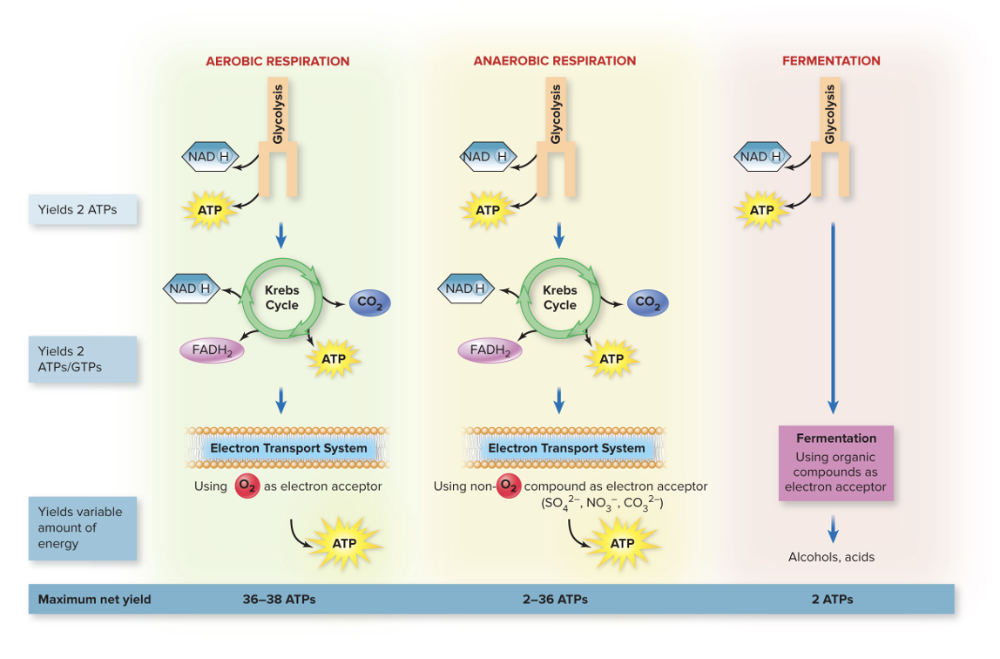 1. Aerobic Respiration
2. Anaerobic Respiration
3. Fermentation
|
front 51 Compare and contrast Aerobic vs Anaerobic Respiration. | back 51 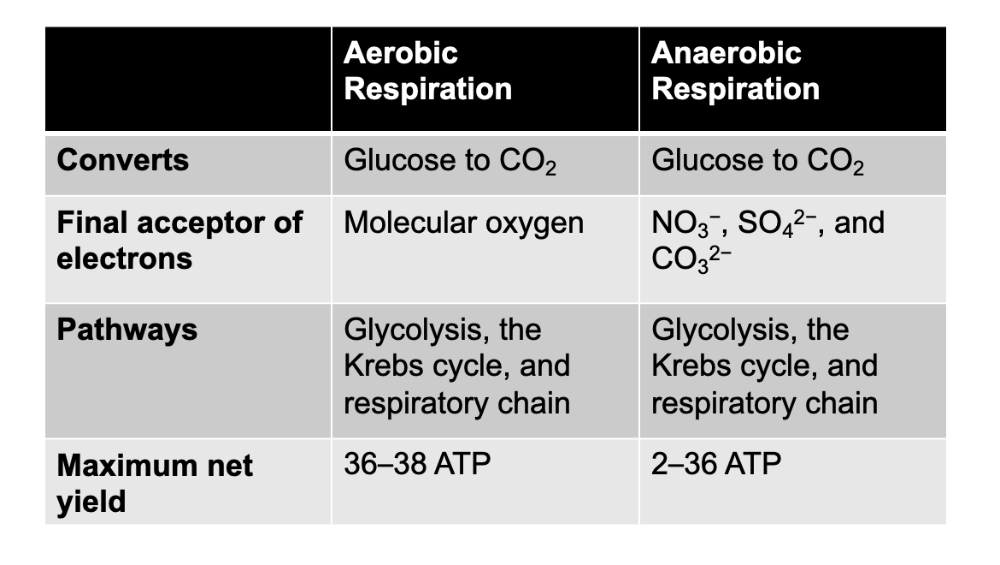 Main difference in the amount of energy they yield and the final electron acceptor |
front 52 Fermentation is for _______ and ________ anaerobes. | back 52 1. Facultative
2. Aerotolerant
|
front 53 True or False: Fermentation only uses glycolysis and oxygen is NOT required as they use other organic compounds as electron acceptors. | back 53 True |
front 54 What is the starting compound for respiration, and why? | back 54 Glucose!
|
front 55 What is the end product of this conversion from glucose to CO2, with aerobic and anerobic respiration? | back 55 The end products of the conversion of these carbon compounds are energy-rich ATP and energy-poor carbon dioxide and water |
front 56 Review PPT slides for Respiration | back 56 237 to |
front 57 Chapter 23 | back 57 Infectious Diseases Manifesting in the GI tract |
front 58 What are the eight main segments of the GI tract? | back 58 Mouth, pharynx, esophagus, stomach, small intestine, large intestine, rectum, and anus |
front 59 What are the four accessory organs? | back 59 Salivary glands, liver, gallbladder, and pancreas |
front 60 What are the defenses against a heavy load of microorganisms? | back 60
|
front 61 True of False: The GI tract has no normal biota. | back 61 False
|
front 62 What are the different parts of the normal microbiota as part of the GI tract? | back 62 Oral microbiome:
Esophagus and stomach:
Large intestine:
|
front 63 What is the most common species of normal microbiota in the stomach/esophagus? | back 63
|
front 64 _______ organs are considered to be FREE of normal biota | back 64 Accessory organs |
front 65 What are the functions of the normal gut biota? | back 65 Functions of normal gut biota:
A diverse gut microbiome is associated with health |
front 66 Dental caries are caused by what, and what are the unique characteristics... | back 66 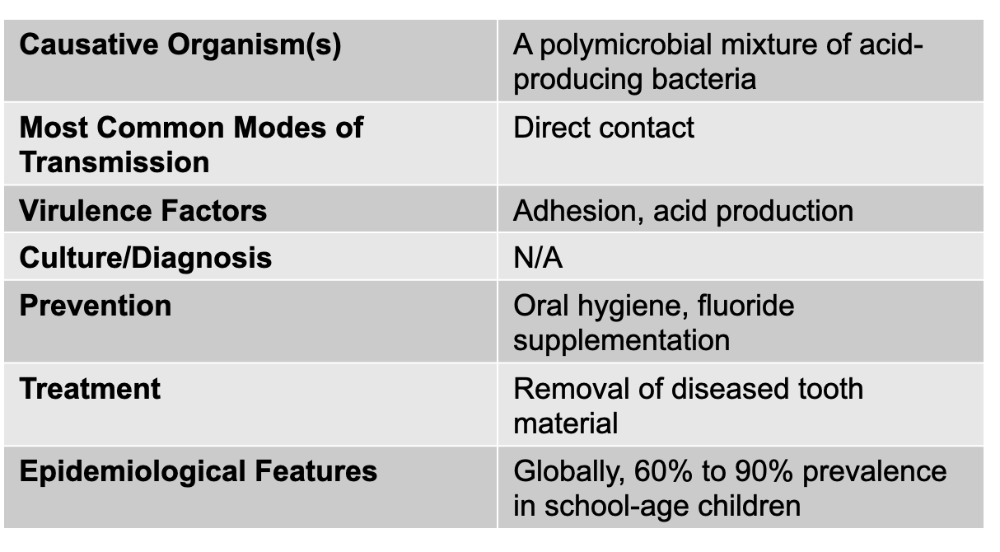 The most common infectious disease of human beings
|
front 67 Mumps is caused by what, and what are the unique characteristics about it? | back 67
Causative agent: Mumps virus (genus paramyxovirus) Mode of transmission: Droplet contact Virulence Factors: spike-induced syncytium formation (Paramyxoviruses can infect multiple host cell types because they use a fusion (F) protein and an attachment protein (like HN, H, or G depending on the virus) that recognize receptors found on many different kinds of cells. Once the attachment protein binds its receptor, the F-protein is activated and causes the viral envelope to fuse directly with the host cell membrane. This fusion ability is not restricted to one cell type because the receptors they target—often sialic acid or broadly expressed surface proteins—are present on a wide range of respiratory and immune cells. Because of this broad receptor distribution, paramyxoviruses can spread from the respiratory epithelium into immune cells, syncytia-forming clusters, and even neural tissue in some cases. Their F-protein also allows cell-to-cell fusion, creating syncytia, which lets the virus move between cells without needing to exit the host cell, further expanding the number of cells they can infect and helping them evade the immune system.) Culture/Diagnosis: ELISA for Ab; PCR Prevention: MMR live attenuated vaccine Treatment: Supportive Epidemiological Features: United States: fluctuates between a few hundred cases a year and a few thousand; internationally: epidemic peaks every 2 to 5 years |
front 68 For mumps, after the initial signs and symptoms, what follows? | back 68
|
front 69 What can mumps lead to in 20-30% of young adult males.... | back 69 Localized infection in the epididymis and testes, but does NOT cause sterility. |
front 70 Gastritis and gastric/peptic ulcers are caused by what, and what are the unique characteristics? | back 70
Causative agent: helicobacter pylori Mode of Transmission: oral to oral or oral-fecal route LIKELY Virulence Factors: adhesions and urease (Adhesions are surface molecules that let the bacteria stick tightly to the stomach’s epithelial cells, anchoring it in place despite constant mucus flow and peristalsis. This close attachment allows the bacteria to deliver toxins and cause localized inflammation. Urease is an enzyme that breaks down urea into ammonia and carbon dioxide; the ammonia acts as a buffer that neutralizes stomach acid around the bacteria, creating a more alkaline “microenvironment” that keeps H. pylori alive. However, ammonia is also toxic to epithelial cells and contributes to tissue injury. Together, adhesions help H. pylori stay in the stomach long enough to cause disease, while urease enables survival in acid and directly contributes to mucosal damage, ultimately leading to chronic inflammation and ulcer formation.) Culture/Diagnosis: direct antigen test on stool, urea breath test Prevention: none Treatment: Clarithromycin + acid suppression Epidemiological Features: United States: infection (not disease) rates at 35% of adults; internationally: infection rates at 50% |
front 71 What is the best treatment for gastritis/gastric ulcers? | back 71 Best treatment is clarithromycin |
front 72 What is acute diarrhea (with or without vomiting)? | back 72
|
front 73 What is the most common cause of foodborne illness? | back 73 Norovirus |
front 74 What is the most common cause of death due to foodborne illness? | back 74 Salmonella |
front 75 What are the pathogens that cause acute diarrhea? (SSSE CCV) (CRN) | back 75 BACTERIAL CAUSES: Salmonella Shigella, Shiga-toxin producing E-coli Other E.coli (non-shiga toxin producing) Campylobacter Clostridiodies difficile Vibrio cholerae Non-cholera Vibrio species NON-BACTERIAL CAUSES: Cryptosporidium Rotavirus Norovirus |
front 76 What is the most common cause of bacterial diarrhea in the U.S? | back 76 Campylobacter |
front 77 Salmonella causes what, and what are the unique characteristics | back 77 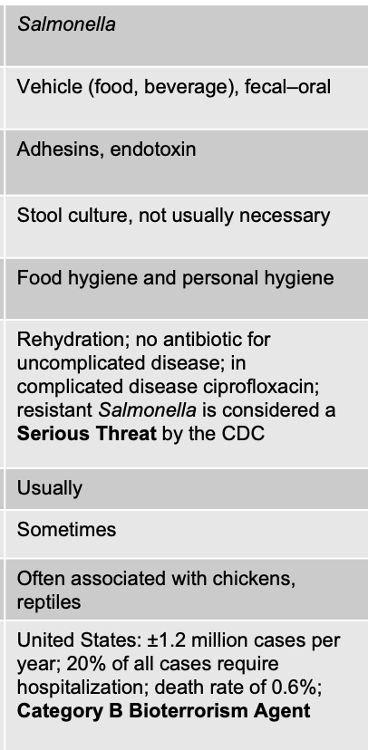 ACUTE DIARRHEA Facts about Salmonella
H, O, and K antigens are used to identify gram-negative enterics
Ferment glucose with acid and gas production (we mean that the bacteria can use glucose as an energy source through fermentation, and in doing so they produce both acidic byproducts and gas. This pattern is important because it helps microbiologists distinguish Salmonella from other enteric bacteria during diagnostic testing.)
Signs/Symptoms
____________________________ Causative: salmonella Mode of transmission: vehicle (food and beverage), fecal-oral Virulence Factors: adhesions and endotoxin
Culture/Diagnosis: stool culture, usually not necessary Prevention: food/ personal hygiene Treatment: Rehydration; no antibiotic for uncomplicated disease; in complicated disease ciprofloxacin; resistant Salmonella is considered a Serious Threat by the CDC FEVER PRESENT (usually) BLOOD IN STOOL: sometimes Distinctive Features: often associated with chickens, reptiles Epidemiological: United States: ±1.2 million cases per year; 20% of all cases require hospitalization; death rate of 0.6%; Category B Bioterrorism Agent |
front 78 What are the three antigens used to identify the gram-negative enterics or subtypes of salmonella? | back 78
H, O, and K antigens are surface structures found on gram-negative enteric bacteria, and they’re used in serotyping to distinguish one species or strain from another. The O antigen refers to the outer portion of the lipopolysaccharide (LPS) on the bacterial outer membrane and varies widely among species, making it useful for identifying different serogroups. The H antigen is the flagellar protein, so only motile bacteria have it, and its variations help differentiate strains based on their flagellar structure. The K antigen is a capsular polysaccharide surrounding some bacteria; it can mask the O antigen and contributes to virulence by preventing phagocytosis. |
front 79 Salmonella causing acute diarrhea has a ____ infectious dose. | back 79 Most Salmonella species that cause gastroenteritis require a high infectious dose, often around 10³–10⁵ organisms, because they are sensitive to stomach acid and many are killed before reaching the intestines. This is why Salmonella infections usually occur from eating a large bacterial load in contaminated foods like eggs, poultry, or undercooked meat. |
front 80 Shigella causes what, and what are the unique characteristics? | back 80 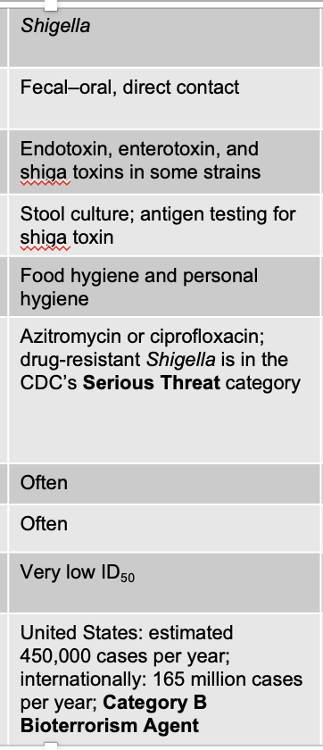 ACUTE DIARRHEA
Symptoms
Pathogenesis and Virulence Factors
_______________________________ Fecal–oral, direct contact Virulence: Endotoxin, enterotoxin, and shiga toxins in some strains
Culture/Diagnosis: Stool culture; antigen testing for shiga toxin Prevention: Food hygiene and personal hygiene Treamtnet: Azitromycin or ciprofloxacin; drug-resistant Shigella is in the CDC’s Serious Threat category Fever: Often Blood in stool: Often Distinctive Features: Very low ID50 United States: estimated 450,000 cases per year; internationally: 165 million cases per year; Category B Bioterrorism Agent |
front 81 Shigella can also cause shigella _______, and dysentery is _______. | back 81 shigella dystenteriae diarrhea containing blood |
front 82 What are the virulence factors for Shigella | back 82 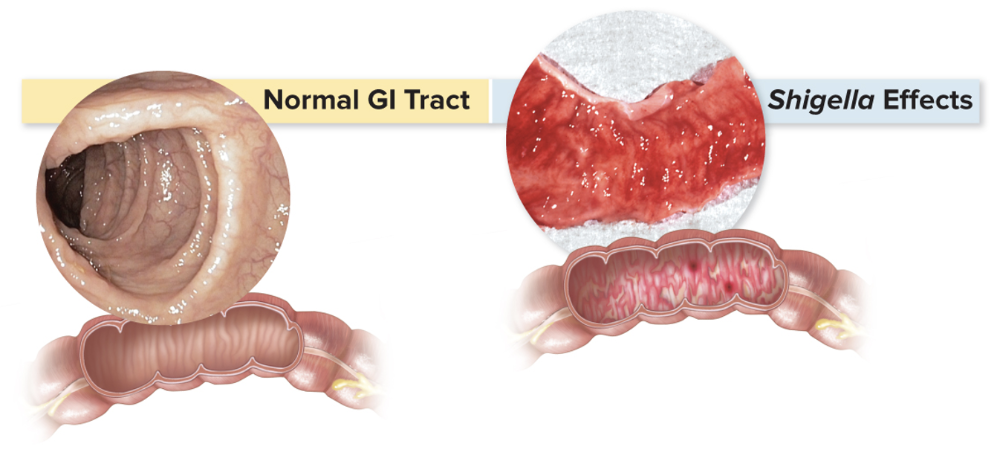
|
front 83 Shiga-Toxin Producing Escherichia coli (STEC) causes what, and what are the unique characteristics? | back 83 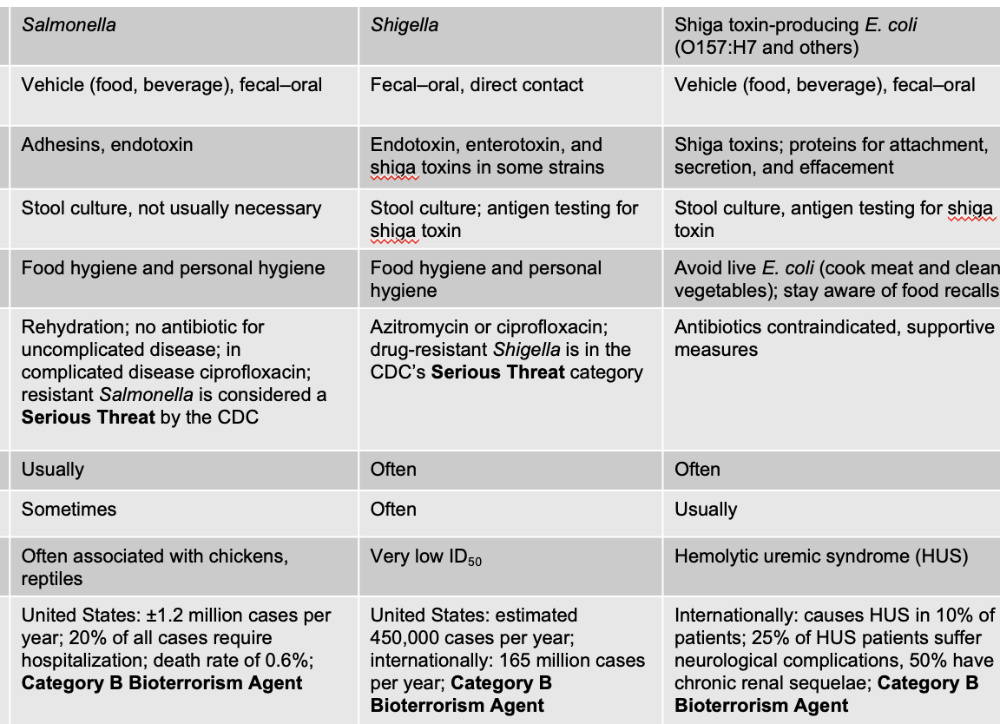 ACUTE DIARRHEA E.coli O157:H7 Signs/Symptoms
Mode: Vehicle (food, beverage), fecal–oral Virulence: Shiga toxins; proteins for attachment, secretion, and effacement
Culture/Diagnosis: Stool culture, antigen testing for shiga toxin Prevention: Avoid live E. coli (cook meat and clean vegetables); stay aware of food recalls Treatments: Antibiotics contraindicated, supportive measures Fever: Often Blood in stool: Usually Distinctive: Hemolytic uremic syndrome (HUS) Internationally: causes HUS in 10% of patients; 25% of HUS patients suffer neurological complications, 50% have chronic renal sequelae; Category B Bioterrorism Agent |
front 84 What is the specific strain for Shiga-toxin producing E. coli? | back 84 The designation O157:H7 identifies the strain based on its O and H antigens, which are used for serotyping gram-negative enterics. The O157 refers to the specific type of O antigen on its lipopolysaccharide (LPS), while H7 refers to the H antigen on its flagella. This serotype is clinically important because it is the strain that produces Shiga toxin, causing bloody diarrhea, hemolytic uremic syndrome (HUS), and severe colitis. |
front 85 Other E. coli (Non-Shiga Toxin Producing) causes what, and what are the unique characteristics? | back 85 ACUTE DIARRHEA Causative agent: Other E. coli (Non-Shiga Toxin Producing) Mode of transmission: Vehicle, fecal–oral Virulence factors: Various: proteins for attachment, secretion, effacement; heat-labile, and/or heat-stable exotoxins; invasiveness Culture/Diagnosis: Stool culture not usually necessary in absence of blood, fever Prevention: Food and personal hygiene Treatment: Rehydration, antimotility agent Fever: Sometimes Blood: Sometimes Distinctive Features: ETEC, EIEC, EPEC, DAEC, EAEC Epidemiological: N/A |
front 86 Campylobacter causes what, and what are the unique characteristics? | back 86 ACUTE DIARRHEA
Signs and symptoms:
Bacteria
Transmission
____________________________ Causative: Campylobacter Mode of Transmission: Vehicle (food, water), fecal–oral Virulence: Adhesins, exotoxin, and induction of autoimmunity
Culture/Diagnosis: Stool culture not usually necessary; dark-field microscopy Prevention: Food and personal hygiene Treatment: Rehydration; azithromycin in severe cases (antibiotic resistance rising; resistant Campylobacter is in CDC’s Serious Threat category) Fever: Usually Blood: No Distinctive Features: Guillain-Barré syndrome United States: 1.3 million cases per year; internationally: 400 million cases per year |
front 87 Small number of cases of acute diarrhea caused by campylobacter jejuni can lead to a serious condition called ... | back 87
|
front 88 Clostridiodes difficile causes what, and what are unique characteristics of it? | back 88 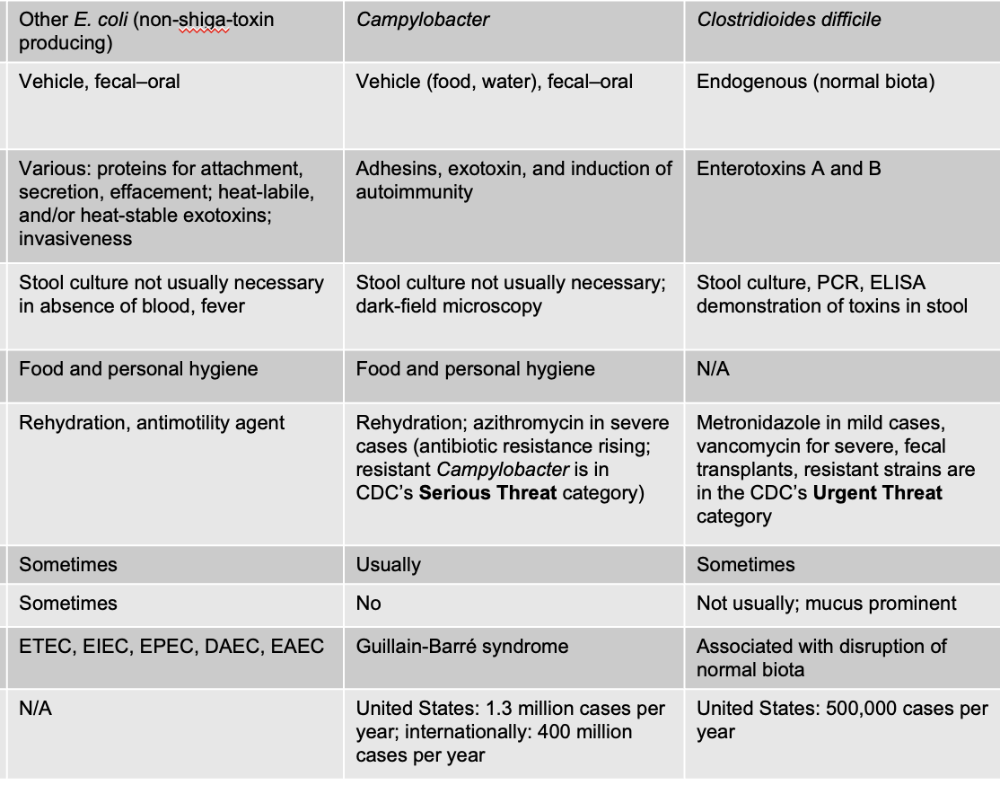 ACUTE DIARRHEA Gram + endospore forming rod (found in normal biota of intestine)
Treatment
______________________________ Clostridioides difficile Endogenous (normal biota) Virulence Factors: Enterotoxins A and B Culture/Diagnosis: Stool culture, PCR, ELISA demonstration of toxins in stool Prevention: N/A Treatment: Metronidazole in mild cases, vancomycin for severe, fecal transplants, resistant strains are in the CDC’s Urgent Threat category Fever: Sometimes Blood in Stool: Not usually; mucus prominent Distinctive: Associated with disruption of normal biota United States: 500,000 cases per year |
front 89 Vibrio cholerae causes what, and what are the unique characteristics of it? | back 89
Signs/Symptoms:
________________________________ Vibrio cholerae Vehicle (water and some foods), fecal–oral Cholera toxin (CT) Culture/Diagnosis: Clinical diagnosis, microscopic techniques, serological detection of antitoxin Prevention: Water and food hygiene Treatment: Rehydration and possibly doxycycline Fever: No Blood in Stool: No Distinctive Features: Rice-water stools Global estimate: 21,000–143,000 deaths annually; Category B Bioterrorism Agent |
front 90 What is the pathogenesis and virulence factors for vibrio cholerae like? | back 90
Transmission and epidemiology:
Treatment: oral rehydration therapy |
front 91 Non-Cholera Vibrio species causes what, and what are the unique characteristics? | back 91 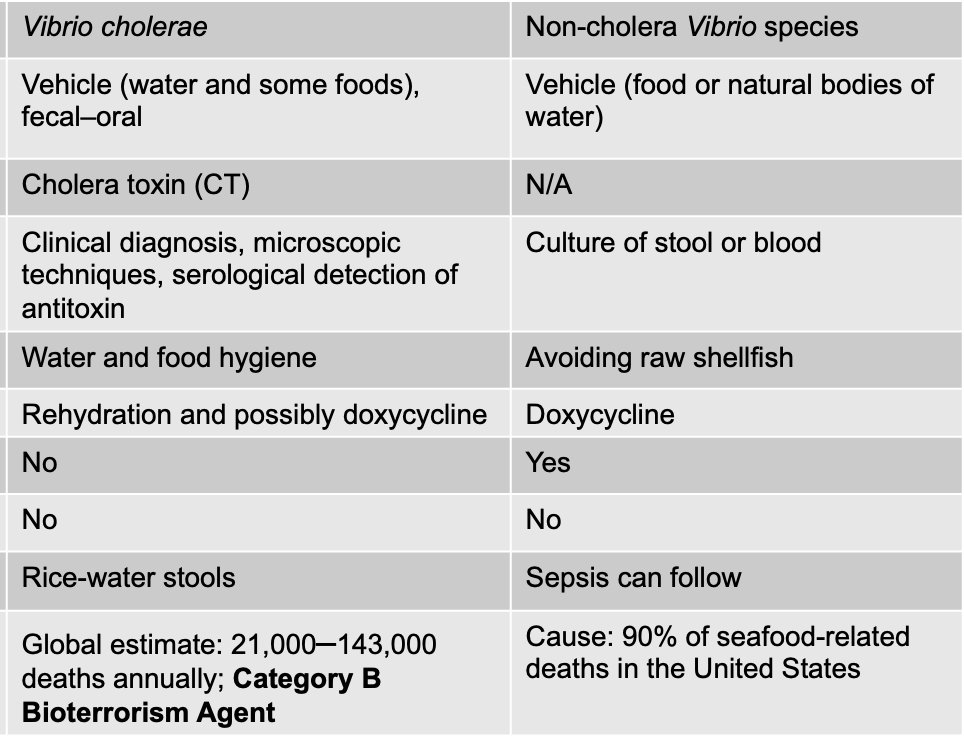 ACUTE DIARRHEA
Factors that increase the chance of infection:
_______________________________ Causative: Non-cholera Vibrio species Mode: Vehicle (food or natural bodies of water) Virulence: N/A Culture/Diagnosis: Culture of stool or blood Prevention: Avoiding raw shellfish Treatment: Doxycycline Fever: Yes Blood in stool: No Distinctive Features: Sepsis can follow Cause: 90% of seafood-related deaths in the United States |
front 92 Cryptosporidium causes what, and what are the unique characteristics? (non-bacterial) | back 92 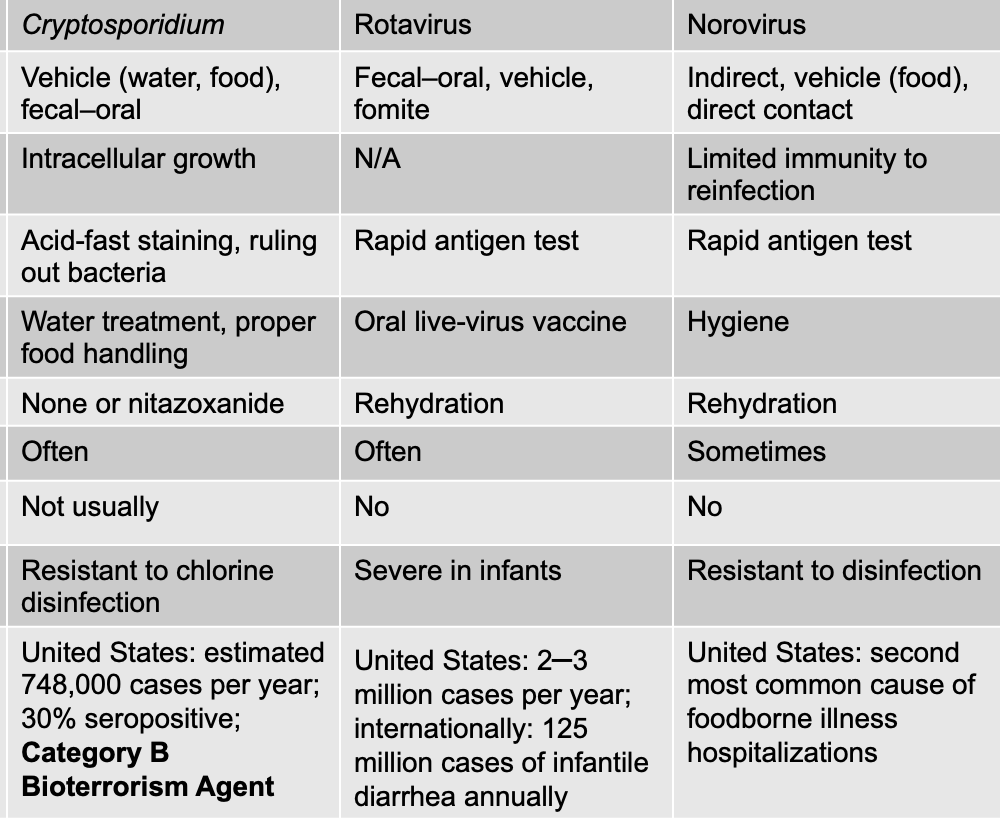 ACUTE DIARRHEA Intestinal apicomplexan protozoan
Symptoms
______________________________ Cryptosporidium Vehicle (water, food), fecal–oral Virulence: Intracellular growth
Culture/Diagnosis: Acid-fast staining, ruling out bacteria Prevention: Water treatment, proper food handling Treatment: None or nitazoxanide Fever: Often Blood in stool: Not usually Distinctive: Resistant to chlorine disinfection United States: estimated 748,000 cases per year; 30% seropositive; Category B Bioterrorism Agent |
front 93 Rotavirus causes what, and what are the unique characteristics? | back 93  ACUTE DIARRHEA
_____________________________ Rotavirus Fecal–oral, vehicle, fomite N/A Culture/Diagnosis: Rapid antigen test Prevention: Oral live-virus vaccine Treatment: Rehydration Fever: Often Blood in stool: No Distinctive Features: Severe in infants United States: 2–3 million cases per year; internationally: 125 million cases of infantile diarrhea annually |
front 94 Norovirus causes what, and what are the unique characteristics? | back 94  ACUTE DIARRHEA Most common cause of foodborne disease in the United States
______________________________ Norovirus Mode: Indirect, vehicle (food), direct contact Virulence: Limited immunity to reinfection
Culture: Rapid antigen test Prevention: Hygiene Treatment: Rehydration Fever: Sometimes Blood in stool: No Distinctive Features: Resistant to disinfection United States: second most common cause of foodborne illness hospitalizations |
front 95 Acute diarrhea with vomiting caused by EXOTOXINS is known as __________ | back 95 Food poisoning
|
front 96 What are the three agents that cause acute diarrhea with vomiting due to exotoxins (AKA food poisoning) | back 96 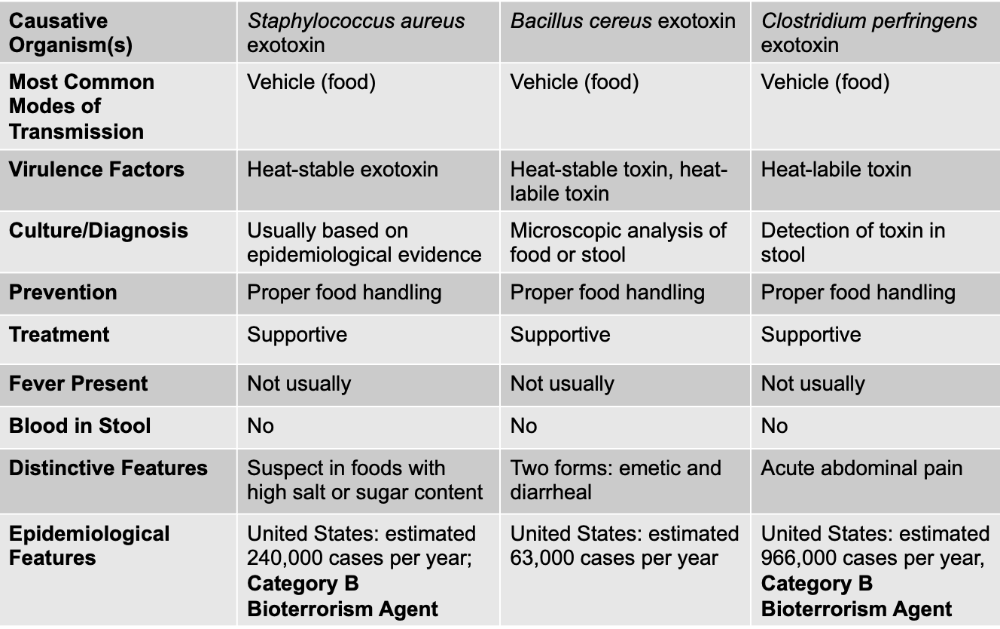 Staphylococcus aureus exotoxin Bacillus cereus exotoxin Clostridium perfringens exotoxin For food poisoning illnesses caused specifically by preformed exotoxins (like Staphylococcus aureus, Bacillus cereus, and sometimes Clostridium perfringens), you do not use antibiotics because the bacteria are usually not alive or not actively infecting you when the symptoms start. The disease happens because you ate food that already contained the toxin, and once the toxin is in your gut, the symptoms occur rapidly—often within 1–6 hours. Since there is no live bacterial infection to kill, antibiotics offer no benefit and can even worsen the gut microbiome. |
front 97 Staphylococcus aureus exotoxin causes what, and what are unique characteristics? | back 97
Self-limiting, antibiotics not warranted
________________________________ Staphylococcus aureus exotoxin MOT: Vehicle (food) Virulence: Heat-stable exotoxin Culture: Usually based on epidemiological evidence Prevention: Proper food handling Treatment: Supportive Fever: Not usually Blood in stool: No Distinctive: Suspect in foods with high salt or sugar content United States: estimated 240,000 cases per year; Category B Bioterrorism Agent |
front 98 What are the two forms of food poisoning by bacillus cereus exotoxin? | back 98 Sporulating gram-positive bacterium that lives in the soil
|
front 99 Bacillus cereus exotoxin causes what, and what are unique characteristics? | back 99 Sporulating gram-positive bacterium that lives in the soil
____________________________ Bacillus cereus exotoxin MOT: Vehicle (food) Virulence: Heat-stable toxin, heat-labile toxin (easily destroyed) Culture: Microscopic analysis of food or stool Prevention: Proper food handling Treatment: Supportive Fever: Not usually Blood in stool: No Distinctive: Two forms: emetic and diarrheal United States: estimated 63,000 cases per year |
front 100 Clostridium perfringens exotoxin causes what, and what are unique characteristics? | back 100
_____________________________________ Clostridium perfringens exotoxin Vehicle (food) Virulence: Heat-labile toxin (destroying) Culture: Detection of toxin in stool Prevention: Proper food handling Treatment: Supportive Fever: Not usually Blood in stool: No Distinctive: Acute abdominal pain United States: estimated 966,000 cases per year, Category B Bioterrorism Agent |
front 101 Chronic diarrhea is diarrhea that lasts longer than ______ | back 101 14 days Can have an infectious or noninfectious cause
|
front 102 Giardia duodenalis causes what, and what are the unique characteristics? | back 102 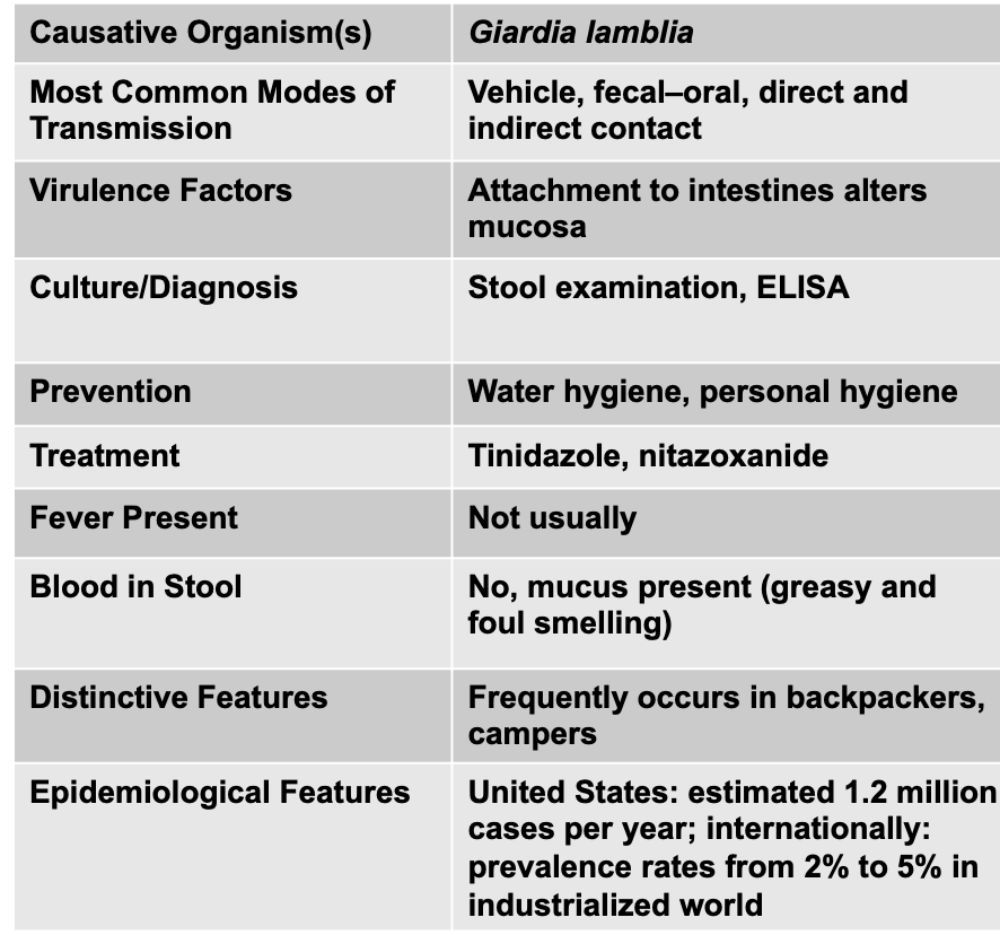
Signs and symptoms: diarrhea of long duration, abdominal pain, flatulence; greasy, and malodorous stools Complex epidemiological pattern:
________________________________ Giardia lamblia Mode of Transmission: Vehicle, fecal–oral, direct and indirect contact Culture/Diagnosis: Attachment to intestines alters mucosa Culture/Diagnosis: Stool examination, ELISA Prevention: Water hygiene, personal hygiene Treatment: Tinidazole, nitazoxanide Fever: Not usually Blood in stool: No, mucus present (greasy and foul smelling) Distinctive: Frequently occurs in backpackers, campers United States: estimated 1.2 million cases per year; internationally: prevalence rates from 2% to 5% in industrialized world |
front 103 What is hepatitis? What does it lead to? | back 103 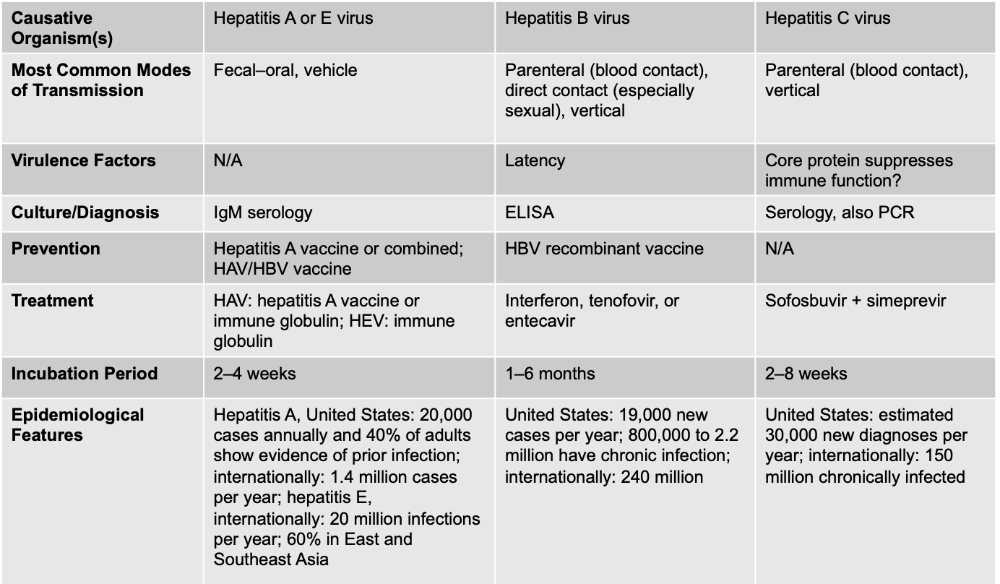 Inflammation of the liver
|
front 104 Hepatitis A (or E) virus causes what, and what are the unique characteristics? | back 104
Signs and symptoms:
Transmission and epidemiology:
Immunizations are available ________________________________ Hepatitis A or E virus MOT: Fecal–oral, vehicle Virulence: N/A Culture/Diagnosis: IgM serology Prevention: Hepatitis A vaccine or combined; HAV/HBV vaccine Treatment: HAV: hepatitis A vaccine or immune globulin; HEV: immune globulin Incubation Period: 2–4 weeks Epidemiological: Hepatitis A, United States: 20,000 cases annually and 40% of adults show evidence of prior infection; internationally: 1.4 million cases per year; hepatitis E, internationally: 20 million infections per year; 60% in East and Southeast Asia |
front 105 Hepatitis B virus causes what, and what are the unique characteristics? | back 105
Signs and symptoms:
An effective vaccine is available
_______________________________ Hepatitis B virus MOD: Parenteral (blood contact), direct contact (especially sexual), vertical Virulence: Latency Culture: ELISA Prevention: HBV recombinant vaccine Treatment: Interferon, tenofovir, or entecavir Incubation Period: 1–6 months Epidemiological: United States: 19,000 new cases per year; 800,000 to 2.2 million have chronic infection; internationally: 240 million |
front 106 Hepatitis C virus causes what, and what are the unique characteristics? | back 106 Silent epidemic: 3.5 million Americans infected Signs and symptoms:
Transmission and epidemiology:
Treatment:
________________________________ Hepatitis C virus MOT: Parenteral (blood contact), vertical Virulence: Core protein suppresses immune function? Culture: Serology, also PCR Prevention: N/A Treatment: Sofosbuvir + simeprevir Incubation: 2–8 weeks United States: estimated 30,000 new diagnoses per year; internationally: 150 million chronically infected |
front 107 Which hepatitis has a vaccine available? | back 107 A B (important for healthcare workers) |
front 108 Which virus is an enveloped virus? | back 108 B - enveloped, DNA C - enveloped RNA |
front 109 Which virus is non-eveloped | back 109 A - non-enveloped, ssRNA |
front 110 Which hepatitis is a silent epidemic? Which hepatitis can cause hepatocellular carcinoma | back 110 Silent - C Carcinoma - B Hepatitis C is called the “silent killer” not because of its incubation period, but because of its long-term, symptomless progression. While Hepatitis B does have a longer incubation period before acute symptoms appear, most people with Hepatitis B either clear the infection or develop symptoms early enough to be diagnosed. In contrast, Hepatitis C infection often causes no noticeable acute symptoms at all, and people can stay infected for 10–30 years without knowing it while the virus quietly causes chronic inflammation, fibrosis, and eventually cirrhosis or liver cancer. By the time symptoms appear, significant and sometimes irreversible liver damage has already occurred. The “silent killer” nickname refers to this decades-long asymptomatic period that leads to severe chronic disease—not the length of the incubation period. |
front 111 PRIOR TO THIS, all the GI disease were non-helminthic diseases, moving forward they are helminthic diseases | back 111 KEEP GOING!! |
front 112 What is a hallmark of helminthic infections? Helminths parasitize humans | back 112
Neglected tropical infections:
|
front 113 What are the general pathogenesis and virulence factors for helminths? | back 113 Virulence
Diagnosis
|
front 114 What is the general prevention and treatment for helminth infections? | back 114
Prevention
|
front 115 What are the four basic helminth life cycles? | back 115
|
front 116 In cycle A, the worm develops in the _________. Eggs are released with _____ into the environment. Eggs are _______ by new host and hatch in intesine. | back 116 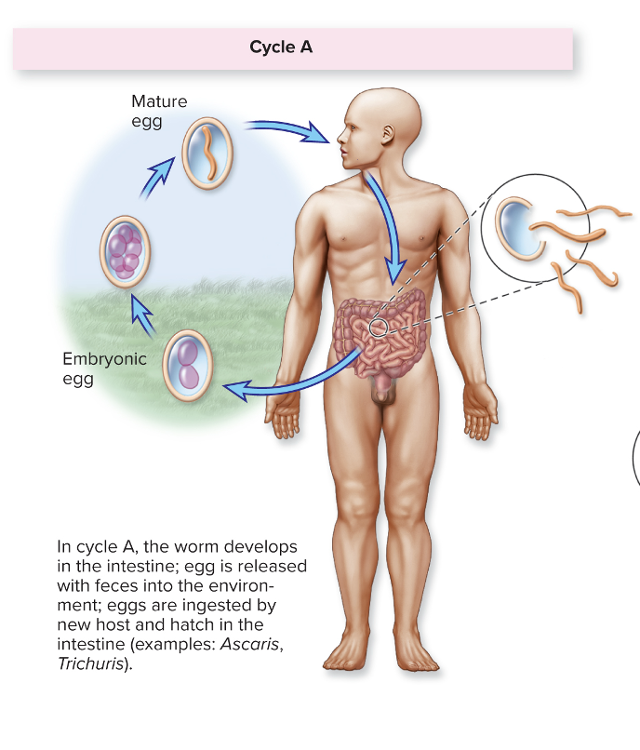 intestines feces ingested |
front 117 In cycle B, the worms mature in the ______, eggs are released with ______ Larvae hatch and develop in the ______, and infection occurs through _______ by ________- | back 117 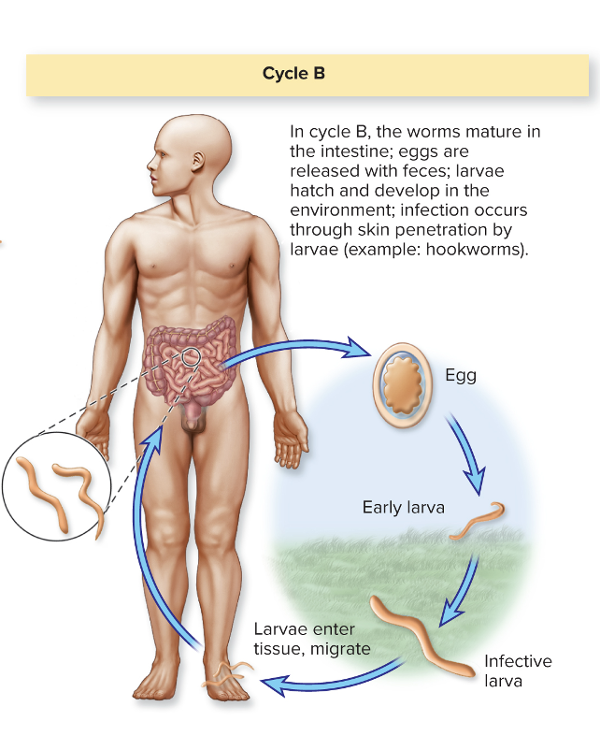 intestines; feces environment; skin penetration by larvae |
front 118 In cycle C, the adult matures in human ______; eggs are released with _____ into the environment Eggs are eaten by ________; larval forms encyst in tissue Humans eating ____ are infected. | back 118 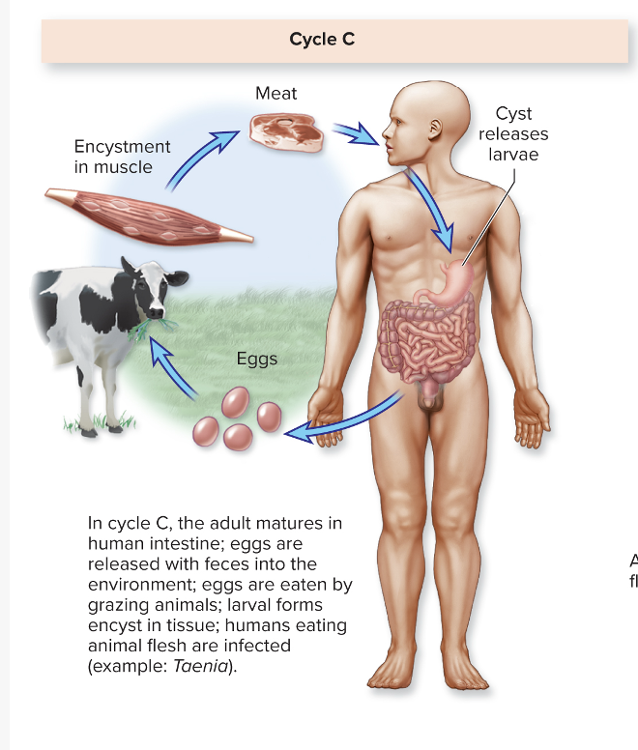 intestine; feces grazing animals animal flesh |
front 119 In cycle D, eggs are released with ____. Humans are infected through ______ or ________ by larval phase. | back 119 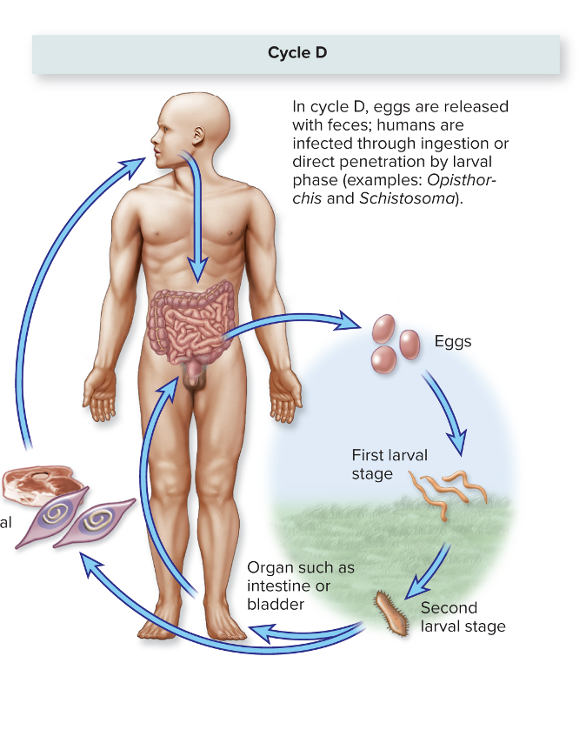 feces ingestion or direct penetration Schistosoma |
front 120 Enterobius vermicularis causes what, and what are the unique characteristics... | back 120 Disease: INTESTINAL DISTRESS Pinworms
_______________________________ Enterobius vermicularis (pinworm) MOT: Cycle A: vehicle (food, water), fomites, self-inoculation Virulence: N/A Culture/Diagnosis: Adhesive tape + microscopy Prevention: Hygiene Treatment: Mebendazole, piperazine Distinctive: Common in the United States United States: up to 40 million cases per year |
front 121 Hallmark anal itching is the hallmark symptom for which causative agent... | back 121 Enterobius vermicularis |
front 122 Taenia solium causes what, and what are the unique characteristics? | back 122 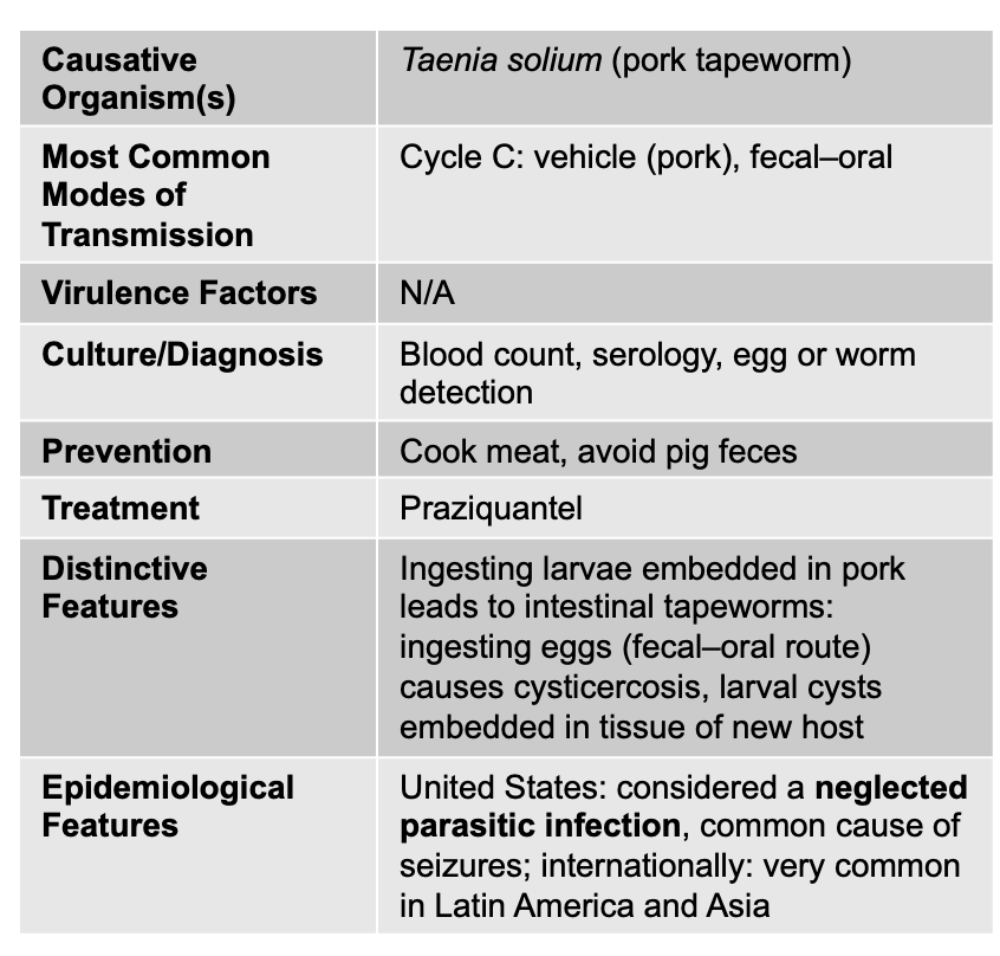 Cysticercosis Tapeworm:
______________________________ Taenia solium (pork tapeworm) Cycle C: vehicle (pork), fecal–oral N/A Blood count, serology, egg or worm detection Cook meat, avoid pig feces Praziquantel Ingesting larvae embedded in pork leads to intestinal tapeworms: ingesting eggs (fecal–oral route) causes cysticercosis, larval cysts embedded in tissue of new host United States: considered a neglected parasitic infection, common cause of seizures; internationally: very common in Latin America and Asia |
front 123 Fasciola hepatica causes what, and what are the unique characteristics? | back 123 Liver and Intestinal Disease
Symptoms
________________________________ Fasciola hepatica Cycle D: vehicle (water and water plants) Virulence: N/A Blood count, serology, egg or worm detection Prevention: Sanitation of water Treatment: Triclabendazole Distinctive Features: Live in liver and gallbladder Epidemiological: United States: most cases imported; internationally: 56 million infected |
front 124 Schistosoma masoni and S. japonicum causes what, and what are the unique characteristics? | back 124 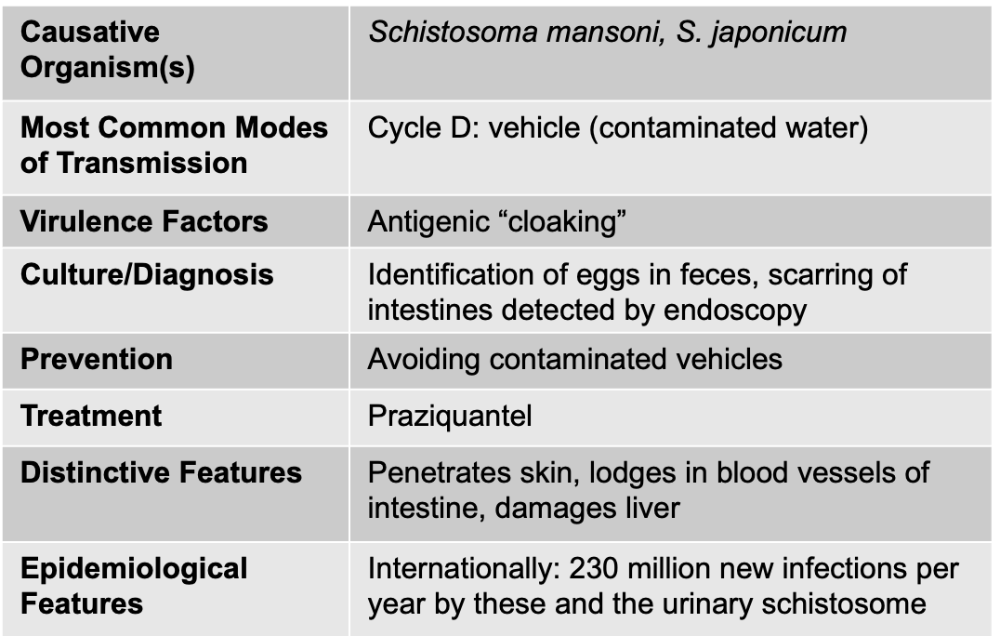 Liver Disease: Schistosomiasis
Signs/Symptoms
Pathogenesis/Virulence Factors
|
front 125 Clostridioides difficile | back 125 Gram-Positive, Endospore-Forming Bacteria Antibiotic-associated diarrhea |
front 126 Bacillus cereus | back 126 Gram-Positive, Endospore-Forming Bacteria Food poisoning |
front 127 Clostridium perfringens | back 127 Gram-Positive, Endospore-Forming Bacteria Food poisoning |
front 128 Streptococcus mutans | back 128 Gram Positive Dental caries |
front 129 Staphylococcus aureus | back 129 Gram Positive Food poisoning |
front 130 Helicobacter pylori | back 130 Gram Negative Gastritis/Gastric Ulcers |
front 131 Salmonella | back 131 Gram Negative Acute Diarrhea |
front 132 Shigella | back 132 Gram Negative Acute diarrhea and dysentery |
front 133 Escherichia coli STEC | back 133 Gram Negative Acute diarrhea plus hemolytic syndrome |
front 134 Other E. coli | back 134 Gram Negative Acute or chronic diarrhea |
front 135 Campylobacter jejuni | back 135 Gram Negative Acute diarrhea |
front 136 Vibrio cholera | back 136 Gram Negative Acute Diarrhea Cholera |
front 137 Non-cholera Vibrio species | back 137 Gram Negative Vibrioses Acute Diarrhea |
front 138 Hepatitis B virus | back 138 DNA viruses “Serum” hepatitis |
front 139 Mumps Virus | back 139 RNA virus |
front 140 Rotavirus | back 140 RNA virus Acute diarrhea |
front 141 Norovirus | back 141 RNA virus Acute diarrhea |
front 142 Hepatitis A | back 142 RNA Infectious hepatitis |
front 143 Hepatitis E | back 143 RNA Infectious hepatitis |
front 144 Hepatitis C | back 144 RNA "serum hepatitis" |
front 145 Cryptosporidium | back 145 Protozoa Acute diarrhea |
front 146 Giardia duodenalis | back 146 Chronic Diarrhea Protozoa |
front 147 Enterobius vermicularis | back 147 Helminths - nematodes (roundworms, pinworms) Intestinal Distress |
front 148 Taenia solium | back 148 Helminths - Cestodes (flatworms), segmented Cysticercosis |
front 149 Fasciola hepatica | back 149 Helminths -Trematodes unsegmented flat worms) Liver and intestinal disease |
front 150
Schistosoma mansoni, | back 150 Helminths -Trematodes (unsegmented flat worms) Schistosomiasis |