Infectious Diseases Manifesting in the Genitourinary System
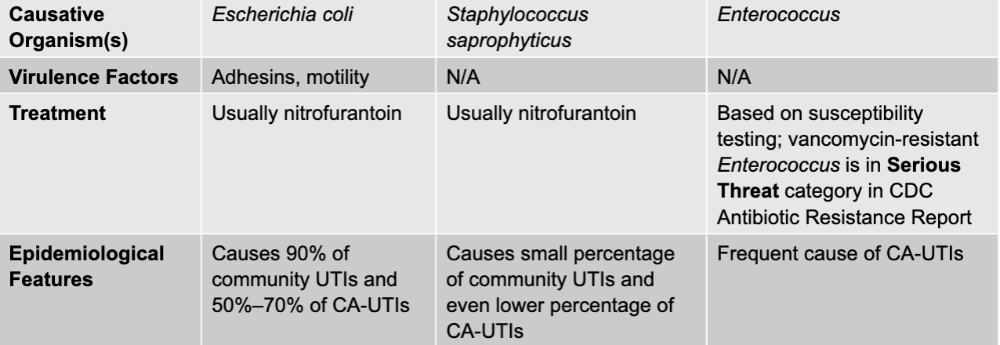
urinary tract infections causative agents
E.coli, staphylococcus saprophyticus, enterococcus
urinary tract infections mode of transmission
opportunism: transfer from GI tract (community-acquired) or environment or GI tract (via catheter)
urinary tract infection culture/diagnosis
usually culture-based; antimicrobial susceptibilities always checked
urinary tract infection prevention
hygiene practices; in case of CA-UTIs, limit catheter usage
E. coli (urinary tract infection) virulence factors
adhesions, motility
staphylococcus saprophyticus (urinary tract infection) treatment
usually nitrofurantoin
E. coli (urinary tract infection) treatment
usually nitrofurantoin
E. coli (urinary tract infection) epidemiological features
causes 90% of community UTIs and 50-70% of CA-UTIs
staphylococcus saprophyticus (urinary tract infection) epidemiological features
causes small percentage of community UTIs and even lower percentage of CA-UTIs
enterococcus (urinary tract infection) treatment
based on susceptibility testing; vancomycin-resistant enterococcus is in serious threat category in CDC antibiotic resistance report
enterococcus (urinary tract infection) epidemiological features
frequent cause of CA-UTIs
urinary tract infection disease table
leptospirosis disease table
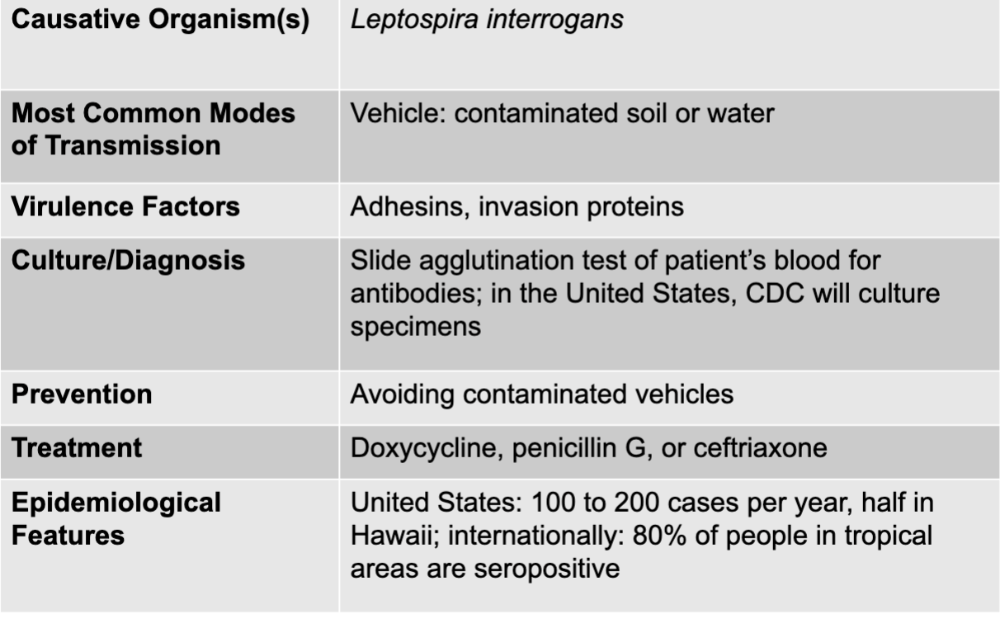
leptospirosis causative agent
leptospira interrogans
leptospirosis mode of transmission
vehicle: contaminated soil or water
leptospirosis virulence factors
adhesions, invasion proteins
leptospirosis culture/diagnosis
slide agglutination test of patient's blood for antibodies; in the US, CDC will culture specimens
leptospirosis prevention
avoiding contaminated vehicles
leptospirosis treatment
doxycycline, penicillin G, or ceftriaxone
leptospirosis epidemiological features
US: 100 to 200 cases per year, half in Hawaii; internationally: 80% of people in tropical areas are seropositive
urinary schistosomiasis disease table
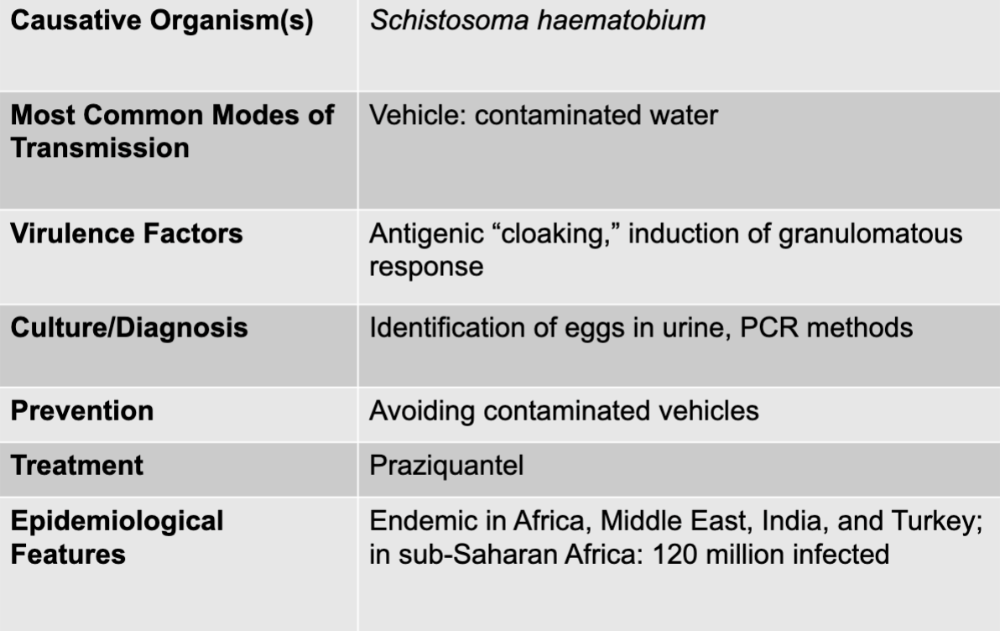
urinary schistosomiasis causative agent
schistosoma haematobium
urinary schistosomiasis mode of transmission
vehicle; contaminated water
urinary schistosomiasis virulence factors
antigenic "cloaking," induction of granulomatous response
urinary schistosomiasis culture/diagnosis
identification of eggs in urine, PCR methods
urinary schistosomiasis prevention
avoiding contaminated vehicles
urinary schistosomiasis treatment
praziquantel
urinary schistosomiasis epidemiological features
endemic in africa, middle east, india, and turkey, in sub-saharan african: 120 million infected
vaginitis disease table
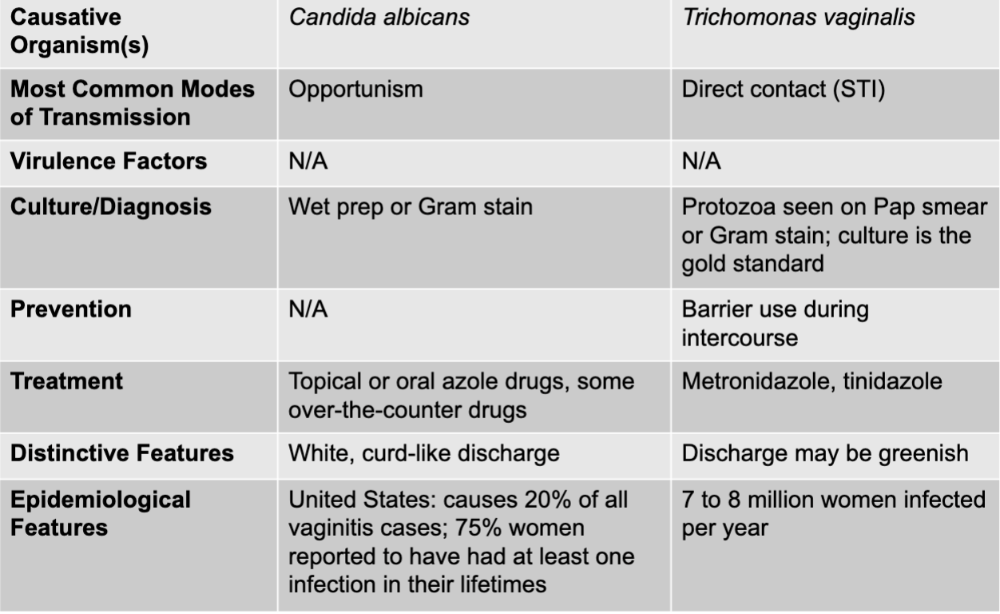
vaginitis causative agents
candida albicans and trichomonas vaginalis
vaginitis (candida albicans) mode of transmission
opportunism
vaginitis (candida albicans) culture/diagnosis
wet prep or gram stain
vaginitis (candida albicans) treatment
topical or oral azole drugs, some over-the-counter drugs
vaginitis (candida albicans) distinctive features
white, curd-like discharge
vaginitis (candida albicans) epidemiological features
US: causes 20% of all vaginitis cases; 75% women reported to have had at least one infection in their lifetimes
vaginitis (trichomonas vaginalis) mode of transmission
direct contact (STI)
vaginitis (trichomonas vaginalis) culture/diagnosis
protozoa seen on pap smear or gram stain; culture is the gold standard
vaginitis (trichomonas vaginalis) prevention
barrier use during intercourse
vaginitis (trichomonas vaginalis) distinctive features
discharge may be greenish
vaginitis (trichomonas vaginalis) epidemiological features
7 to 8 million women infected per year
vaginosis disease table
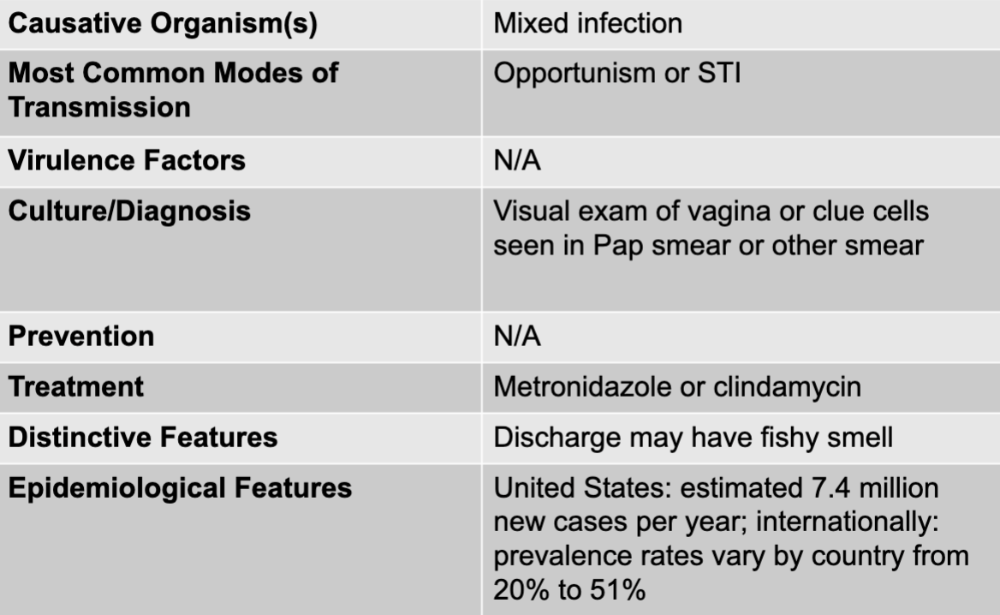
vaginosis causative organisms
mixed infection
vaginosis mode of transmission
opportunism or STI
vaginosis culture/diagnosis
visual exam of vagina or clue cells seen in pap smear or other smear
vaginosis treatment
metronidazole or clindamycin
vaginosis distinctive features
discharge may have fishy smell
vaginosis epidemiological features
US: estimated 7.4 million new cases per year; internationally: prevalence rates vary by country from 20% to 51%
prostatitis disease table
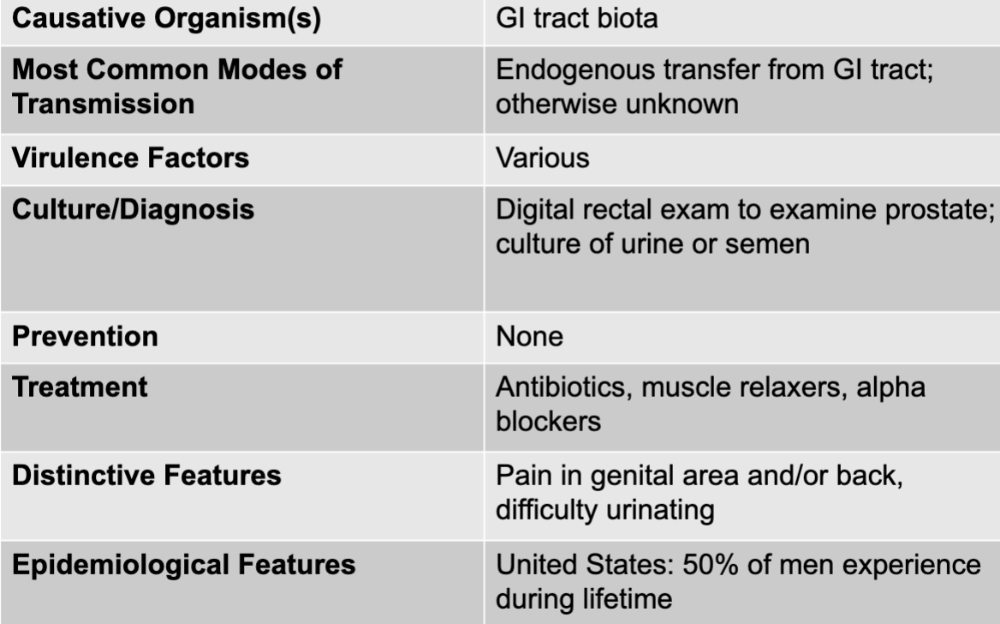
prostatitis causative agent
GI tract biota
prostatitis mode of transmission
endogenous transfer from GI tract; otherwise unknown
prostatitis virulence factors
various
prostatitis culture/diagnosis
digital rectal exam to examine prostate; culture or urine or semen
prostatitis treatment
antibiotics, muscle relaxers, alpha blockers
prostatitis distinctive features
pain in genital area and or/back, difficulty urinating
prostatitis epidemiological features
US: 50% of men experience during lifetime
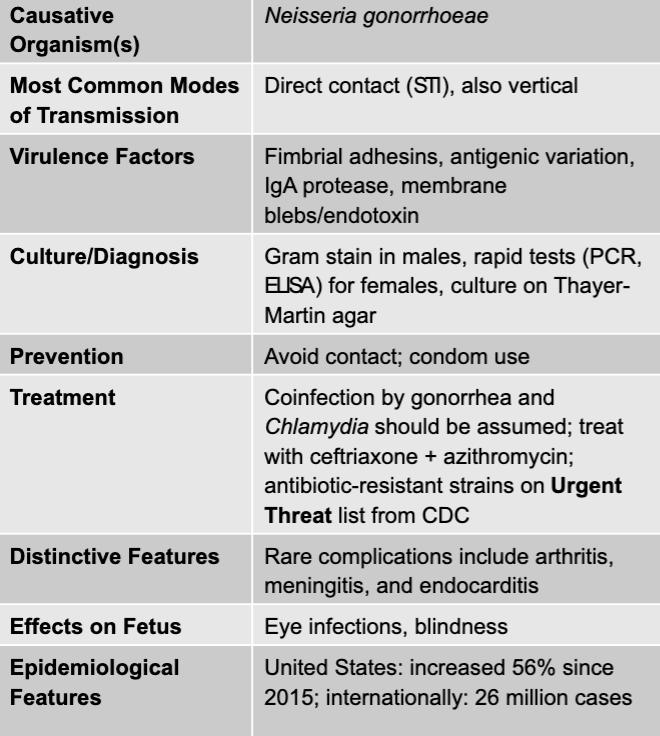
gonorrhea disease table
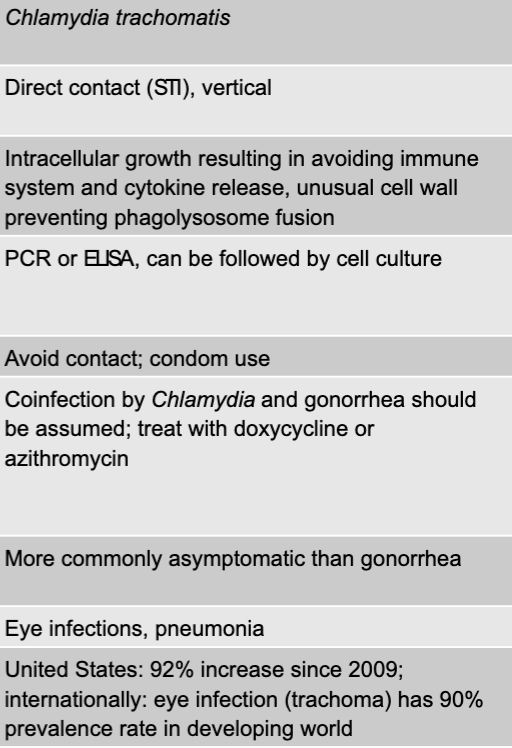
chlamydia disease table
gonorrhea causative agent
neisseria gonorrhoeae
gonorrhea mode of transmission
direct contact (STI), also vertical
gonorrhea virulence factors
fimbrial adhesins, antigenic vvariation, IgA protease, membrane blebs/endotoxin
gonorrhea culture/diagnosis
gram stain in males, rapid tests (PCR, ELISA) for females, culture on thayer-martin agar
gonorrhea prevention
avoid contact; condom use
gonorrhea treatment
coinfection by gonorrhea and chlamydia should be assumed; treat with ceftriaxone + azithromycin; antibiotic-resistant strains on urgent threat list from CDC
gonorrhea distinctive features
rare complications include arthritis, meningitis, and endocarditis
gonorrhea effects on fetus
eye infections, blindness
gonorrhea epidemiological features
US: increased 56% since 2015; internationally: 26 million cases
chlamydia causative agent
chlamydia tranchomatis
chlamydia mode of transmission
direct contract (STI), vertical
chlamydia virulence factors
intracellular growth resulting in avoiding immune system and cytokine release, unusual cell wall preventing phagolysosome fusion
chlamydia culture/diagnosis
PCR or ELISA, can be followed by cell culture
chlamydia prevention
avoid contact; condom use
chlamydia treatment
coinfecction by chlamydia and gonorrhea should be assumed; treat with doxycycline or azithromycin
chlamydia distinctive features
more commonly asymptomatic than gonorrhea
chlamydia effects on fetus
eye infections, pneumonia
chlamydia epidemiological features
US: 92% increase since 2009; internationally: eye infection (trachoma) has 90% prevalence rate in developing world
syphilis disease table
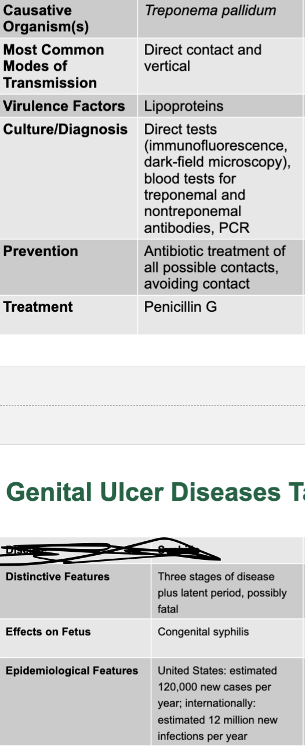
chancroid disease table
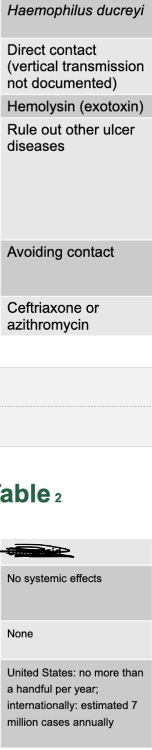
herpes disease table
syphilis causative agent
treponema pallidum
syphilis mode of transmission
direct contact and vertical
syphilis virulence factors
lipoproteins
syphilis culture/diagnosis
direct tests, blood tests for treponemal and nontreponemal antibodies, PCR
syphilis prevention
antibiotic treatment of all possible contacts, avoiding contact
syphilis treatment
penicillin G
syphilis distinctive features
three stages of disease plus latent period, possibly fatal
syphilis effects on fetus
congenital syphilis
syphilis epidemiological features
US: estimated 120,000 new cases per year; internationally; estimated 12 million new infections per year
chancroid causative agent
haemophilus ducreyi
chancroid mode transmission
direct contact (vertical transmission not documented)
chancroid virulence factors
hemolysin (exotoxin)
chancroid culture/diagnosis
rule out other ulcer diseases
chancroid prevention
avoiding contact
chancroid treatment
ceftriaxone or azithromycin
chancroid distinctive features
no systemic effects
chancroid effects of fetus
none
chancroid epidemiological features
US: no more than a handful per year; internationally: estimated 7 million cases annually
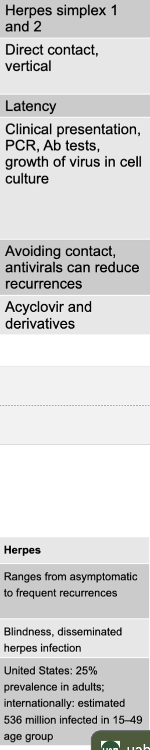
herpes causative agent
herpes simplex 1 and 2
herpes mode of transmission
direct contact, vertical
herpes virulence factors
latency
herpes culture/diagnosis
clinical presentation, PCR, Ab tests, growth of virus in cell culture
herpes prevention
avoiding contact, antivirals can reduce recurrences
herpes treatment
acyclovir and derivatives
herpes distinctive features
ranges from asymptomatic to frequent recurrences
herpes effects on fetus
blindness, disseminated herpes infection
herpes epidemiological features
US: 25% prevalence in adults; internationally: estimated 536 million infected in 15-49 age group
wart diseases causative agents
HPV and molluscum contagiosum
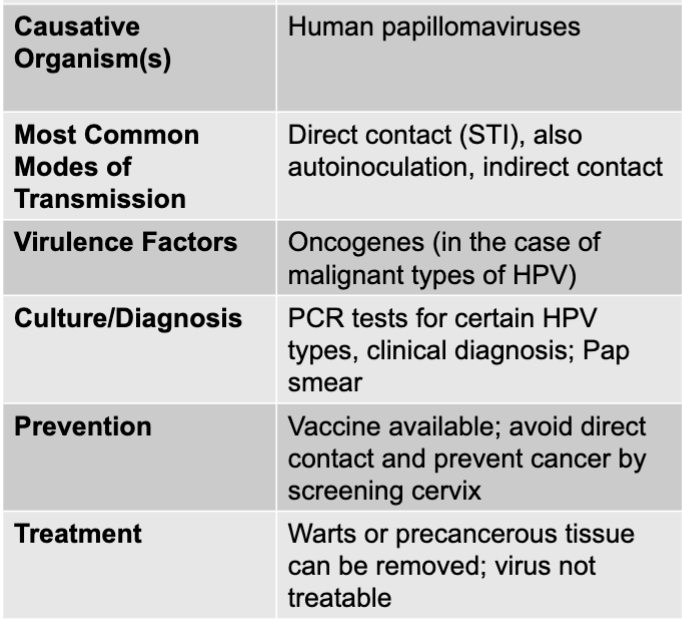
HPV disease table
molluscum contagiosum disease table
HPV causative agent
human papillomaviruses
HPV mode of transmission
direct contact (STI), also auto inoculation, indirect contact
HPV virulence factors
oncogenes (in the case of malignant types of HPV)
HPV culture and diagnosis
PCR tests for certain HPV types, clinical diagnosis; pap smear
HPV prevention
vaccine available; avoid direct contact and prevent cancer by screening cervix
HPV treatment
warts or precancerous tissue can be removed; virus not treatable
HPV distinguishing features
infection may or may not results in warts; infection may result in malignancy
HPV effects on fetus
may cause laryngeal warts
HPV epidemiological features
US: estimated 6 million new infections per year, 12,000 new cases of HPV-associated cervical cancer
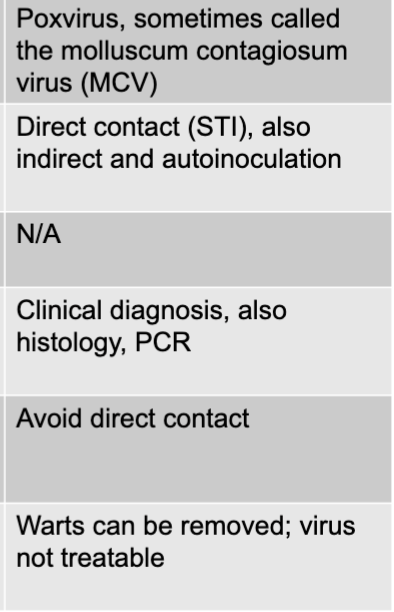
molluscum contagiosum causative agent
poxvirus, sometimes called the molluscum contagiosum virus (MCV)
molluscum contagiosum mode of transmission
direct contact (STI), also indirect and autoinoculation
molluscum contagiosum culutre/diagnosis
clinical diagnosis, also histology, PCR
molluscum contagiosum prevention
avoid detection contact
molluscum contagiosum treatment
warts can be removed; virus not treatable
molluscum contagiosum distinguishing features
wart-like growths are only known consequence of infection
molluscum contagiosum epidemiological features
US: affects 2-10% of children annually
group b streptococcus disease table
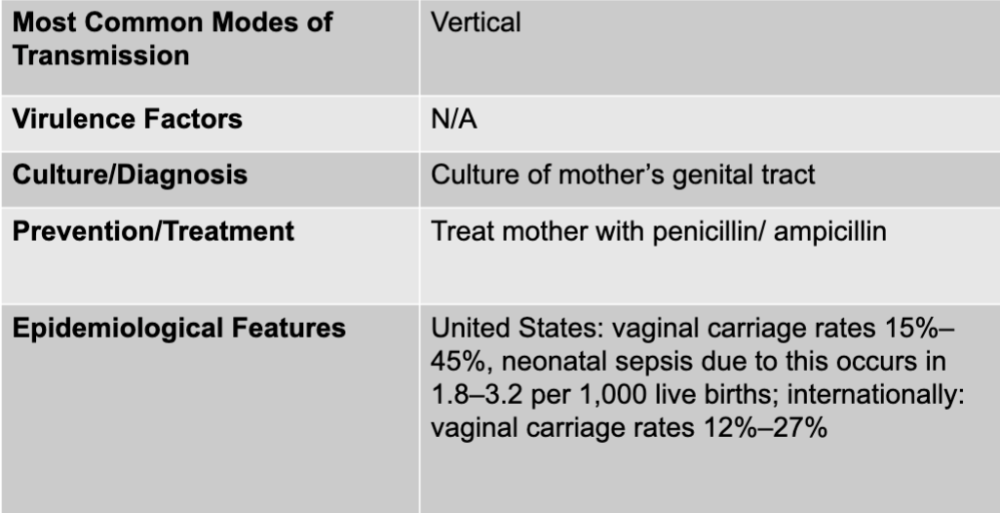
group b streptococcus mode of transmission
vertical
group bstreptococcus culture/diagnosis
culture of mother's genital tract
group b streptococcus prevention/treatment
treat mother with penicillin/ampicillin
group b streptococcus epidemiological features
US: vaginal carriage rates 15%-45%, neonatal sepsis due to this occurs in 1.8-3.2 per 1,000 live births; internationally: vaginal carriage rates 12%-27%
gram-positive bacteria
saphylococcus saprophyticus
group b stretococcus
gram-negative bacteria
E. coli
enterococcus
leptospira interrogans
neisseria gonorrhoeae
chlamydia trachomatis
treponema pallidum
haemophilus ducreyi
DNA viruses
herpes simplex viruses 1 and 2
human papillomaviruses
pox viruses
fungi
candida albicans
protozoa
trichomonas vaginalis
helminth-trematode
schistosoma haematobium