To print: Ctrl+PPrint as notecards
Section 2.2 Exercises
1.
Select the correct answer.
The review of systems section on a patient’s health record
Multiple Choice
- describes the individual body systems in order to discover any symptoms not directly related to the main problem.
- gives the story of the patient’s problem.
- includes any of the patient’s past surgeries.
- relates a record of habits that can impact health.
describes the individual body systems in order to discover any symptoms not directly related to the main problem.
2.
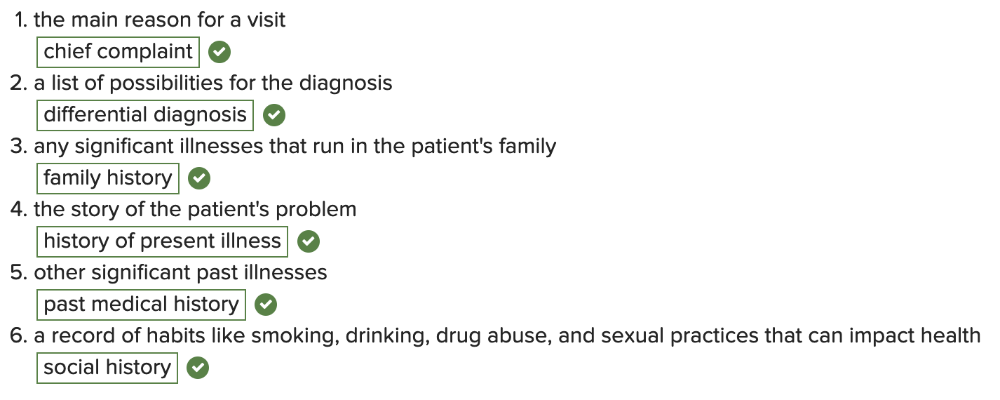
Match the term with its definition below.
- the main reason for a visit
- a list of possibilities for the diagnosis
- any significant illnesses that run in the patient's family
- the story of the patient's problem
- other significant past illnesses
- a record of habits like smoking, drinking, drug abuse, and sexual practices that can impact health
3.
Select the correct answer.
Which of the following is NOT true about the acronym SOAP?
Multiple Choice
- It reflects a basic thought pattern that health providers employ in solving patient problems.
- It stands for Subjective, Objective, Assessment, and Procedure.
- SOAP is a baseline of thought in all disciplines of medicine.
- SOAP is an acronym that stands for the four general parts of a medical note.
It stands for Subjective, Objective, Assessment, and Procedure.
4.
Select the correct answer.
Which health record note is written by a medical professional from an inpatient health care facility and documents daily hospital visits?
Multiple Choice
- admission summary
- clinic note
- daily hospital note/progress note
- discharge summary
daily hospital note/progress note
5.
Which health record note ONLY includes the “Plan”?
Multiple Choice
- consult note
- operative report
- pathology report
- prescription
prescription