Instructions for Side by Side Printing
- Print the notecards
- Fold each page in half along the solid vertical line
- Cut out the notecards by cutting along each horizontal dotted line
- Optional: Glue, tape or staple the ends of each notecard together
Section 2.2 Exercises
front 1 Select the correct answer. The review of systems section on a patient’s health record Multiple Choice
| back 1 describes the individual body systems in order to discover any symptoms not directly related to the main problem. |
front 2  Match the term with its definition below.
| back 2 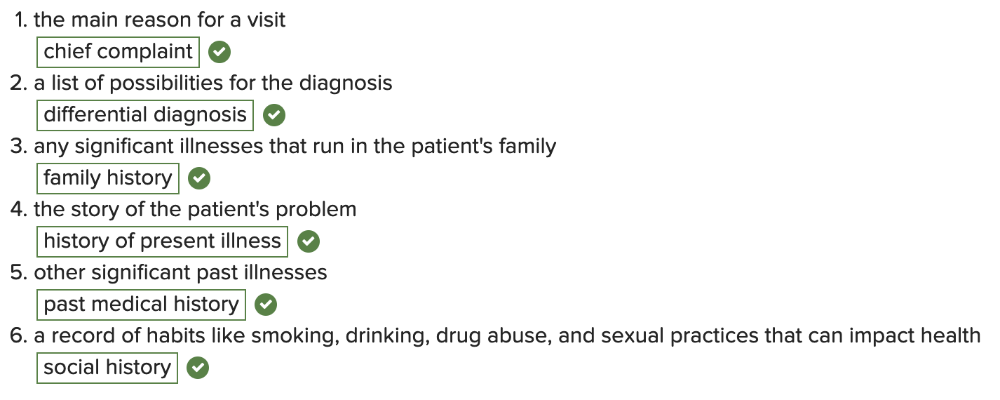 |
front 3 Select the correct answer. Which of the following is NOT true about the acronym SOAP? Multiple Choice
| back 3 It stands for Subjective, Objective, Assessment, and Procedure. |
front 4 Select the correct answer. Which health record note is written by a medical professional from an inpatient health care facility and documents daily hospital visits? Multiple Choice
| back 4 daily hospital note/progress note |
front 5 Which health record note ONLY includes the “Plan”? Multiple Choice
| back 5 prescription |