A&P I - Joints
Joints (aka Articulartions)
Sites where 2 or more bones meet.
Functions of Joints
Functions of joints: give skeleton mobility and hold skeleton together
Classifications of Joints
2 classifications of Joints:
1. Structural: 3 types based on what material binds the joints and whether a cavity is present.
Fibrous (Connective Tissue)
Cartilaginous (Cartilage)
Synovial (Joint Cavity)
2. Functional classifications: 3 types based on
movement joint allows
Synarthroses: immovable joints
Amphiarthroses: slightly movable joints
Diarthroses:
freely movable joints (synovial joints)
Fibrous Joints
- Bones joined by dense fibrous connective tissue
- No joint cavity
- Most are immovable (Depends on length of connective tissue fibers)
-
Three types of fibrous joints
- Sutures
- Syndesmoses
- Gomphoses
Fibrous Joints: Sutures
Fibrous joint
- Rigid, interlocking joints of skull
- Allow for growth during youth (Contain short connective tissue fibers that allow for expansion)
- In middle age, sutures ossify and fuse (Immovable joints join skull into one unit that protects brain)
Fibrous Joints: Syndesmoses
- Bones connected by ligaments, bands of fibrous tissue
- Fiber length varies, so movement varies
- Short fibers offer little to no movement - ex: inferior tibiofibular joint, which is the tibia/fibula
- Longer fibers
offer a larger amount of movement
- ex: interosseous membrane connecting radius and ulna
Fibrous Joints: Gomphoses
- Peg-in-socket joints
- Only examples are the teeth in alveolar sockets
- Fibrous connection is the periodontal
ligament
- Holds tooth in socket
Cartilaginous Joints
- Bones united by cartilage
- Like fibrous joints, have no joint cavity
- Not highly movable (slightly movable)
-
Two types:
- Synchondroses
- Symphyses
Cartilaginous Joints: Synchondroses
- Bar or plate of hyaline cartilage unites bones
- Almost
all are synarthrotic (immovable)
- Examples–Temporary epiphyseal plate joints§Become synostoses after plate closure
- Cartilage of 1st rib with manubrium of sternum
Cartilaginous Joints: Symphyses
- Fibrocartilage unites bone in symphysis joint
- Hyaline cartilage also present as articular cartilage on bony surfaces
- Symphyses are strong, amphiarthrotic (slightly movable) joints
-
Examples:
- Intervertebral joints
- Pubic symphysis
Synovial Joints
- Bones separated by fluid-filled joint cavity
- All are diarthrotic (freely movable)
- Include almost all limb joints
Characteristics of synovial joints
- Characteristics of synovial joints:
- Have six general features
- Have bursae and tendon sheaths associated with them
- Stability is influenced by three factors
- Allow several types of movements
- Classified into six different types
General Structure of Synovial Joints:
Synovial joints have 6 general features:
1. Articular cartilage
2. Joint (synovial) cavity
3. Articular (joint) capsule
4. Synovial fluid
5. Different types of reinforcing ligaments
6. Nerves &
blood vessels
General Structure of Synovial Joints: Articular Cartilage
1. Articular cartilage: consists of hyaline cartilage covering ends of bones (Prevents crushing of bone ends)
General Structure of Synovial Joints: Joint (Synovial) Cavity
2. Joint (synovial) cavity: small, fluid-filled potential space that is unique to synovial joints
General Structure of Synovial Joints: Articular (joint) capsule
3. Articular (joint) capsule: 2 layers thick
-External fibrous layer: dense regular CT
-Inner synovial membrane: loose CT that makes
synovial fluid
General Structure of Synovial Joints: Synovial fluid
4. Synovial fluid: viscous, slippery filtrate of plasma & hyaluronic acid. Lubricates & nourishes articular cartilage. Contains phagocytic cells to remove microbes & debris.
General Structure of Synovial Joints:
Different Types of reinforcing ligaments
5. Different types of reinforcing ligaments
-Capsular: thickened part of fibrous layer
-Extracapsular: outside the capsule
-Intracapsular: deep to capsule; covered by synovial membrane
General Structure of Synovial Joints: Nerves & blood vessels
6. Nerves & blood vessels: Nerves detect pain; monitor joint position & stretch. Capillary beds supply filtrate for synovial fluid.
General Structure of Synovial Joints - other features
- Other features of some synovial joints:
- Fatty pads (For cushioning between fibrous layer of capsule and synovial membrane or bone)
-
Articular discs (menisci) (Meniscus for
singular - seen in knee joint)
- Fibrocartilage separates articular surfaces to improve “fit” of bone ends, stabilize joint, and reduce wear and tear
Bursae and Tendon Sheaths
- Bags of synovial fluid that act as lubricating “ball bearing”
- Not strictly part of synovial joints, but closely associated
- Bursae: reduce friction where ligaments, muscles, skin, tendons, or bones rub together
- Tendon sheaths: elongated bursae wrapped completely around tendons subjected to friction
Factors Influencing Stability of Synovial Joints
Three factors determine stability of joints to prevent dislocations:
- Shape of articular surface (minor role)
- Shallow surfaces less stable than ball-and-socket
-
Ligament number and location (limited role)
- The more ligaments, the stronger the joint
-
Muscle tone keeps tendons taut as they cross joints
(most important)
- Extremely important in reinforcing shoulder and knee joints and arches of the foot
Movements Allowed by Synovial Joints
- All muscles attach to bone or connective tissue at no fewer
than two points
- Origin: attachment to immovable bone (fixed point)
- Insertion: attachment to movable bone (movable point)
- Muscle contraction causes insertion to move toward origin
- Movements occur along transverse, frontal, or sagittal planes
3 General Types of Movements Allowed by Synovial Joints
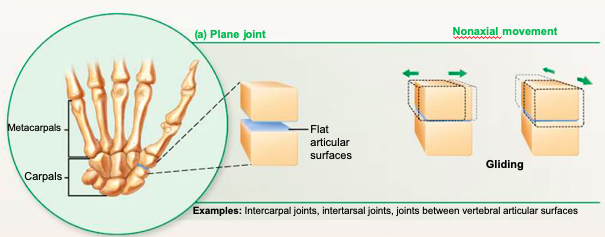
Three general types of movements
- Gliding
- Angular movements
- Rotation
Synovial Joints: Gliding Movements
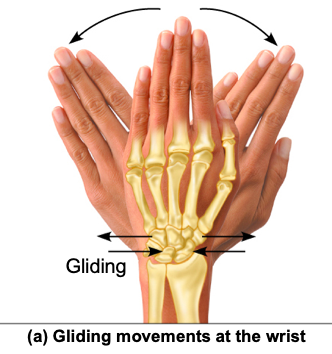
Gliding movements: One flat bone surface glides or slips over another
similar surface.
Examples:
Intercarpal
joints
Intertarsal joints
Between articular processes of vertebrae
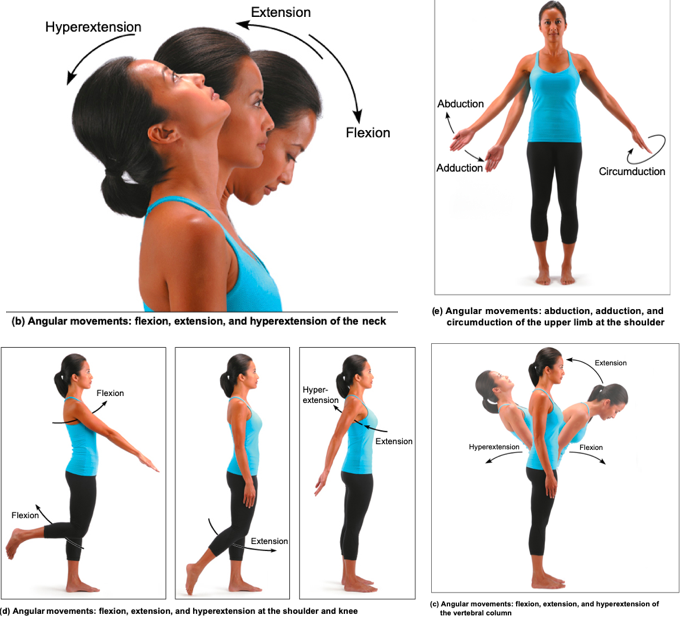
Synovial Joints: Angular Movements
Angular movements: Increase or decrease angle between 2 bones. Movement along sagittal plane. Angular movements include:
- Flexion: decreases the angle of the joint
-
Extension: increases the angle of the joint
- Hyperextension: movement beyond the anatomical position
- Abduction: movement along frontal plane, away from midline
- Adduction: movement along frontal plane, toward midline
-
Circumduction
- Involves flexion, abduction, extension, & adduction of limb
- Limb describes cone in space
Synovial Joint - Angular Movements in Pictures
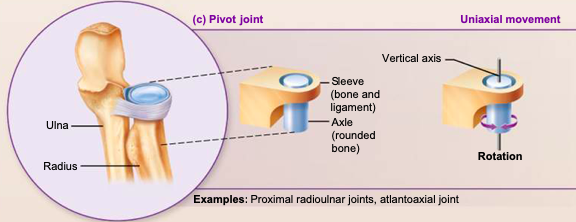
Synovial Joints: Rotations
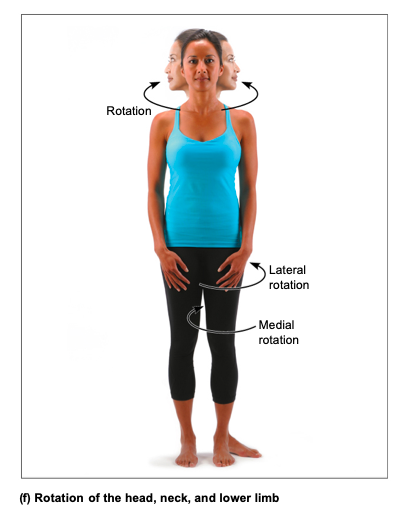
Rotation: turning of bone around its own long axis, toward midline or away from it
- Medial: rotation toward midline
- Lateral: rotation away from midline
- Examples
- Rotation between C1 and C2 vertebrae
- Rotation of humerus and femur
Synovial Joints, Special movements: Supination and pronation
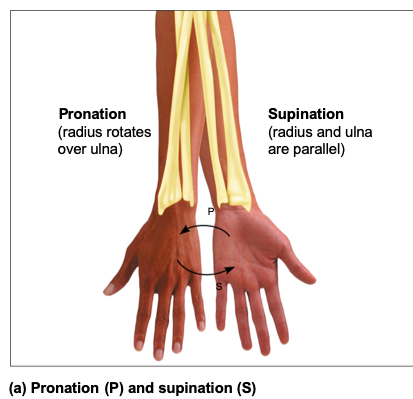
Supination and pronation: rotation of radius and ulna
-
Supination: palms face anteriorly
- Radius and ulna are parallel
-
Pronation: palms face posteriorly
- Radius rotates over ulna
Synovial Joints, Special movements: Inversion and Eversion
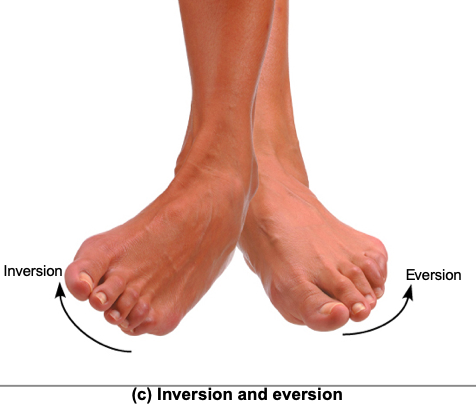
-
Inversion and eversion of foot
- Inversion: sole of foot faces medially
- Eversion: sole of foot faces laterally
Synovial Joints, Special movements: Protraction and retraction
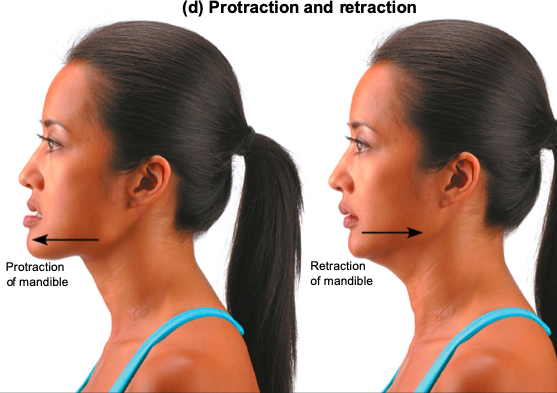
-
Protraction and retraction:
movement in lateral plane
- Protraction: mandible juts out
- Retraction: mandible is pulled toward neck
Synovial Joints, Special movements: Dorsiflexion and plantar flexion
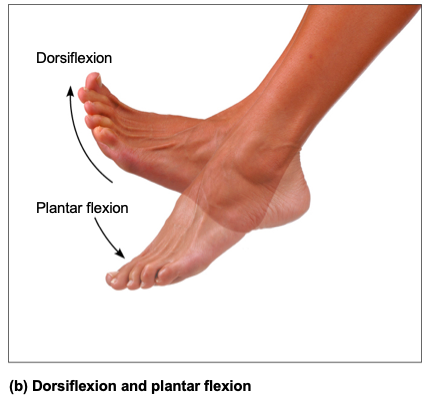
Dorsiflexion and plantar flexion of foot
- Dorsiflexion: bending foot toward shin
- Plantar flexion: pointing toes
Synovial Joints, Special movements: Elevation and Depression of mandible

Elevation and depression of mandible:
Elevation: lifting body part superiorly
Example: shrugging shoulders
Depression: lowering body part
Example:
opening jaw
Synovial Joints, Special movements: Opposition
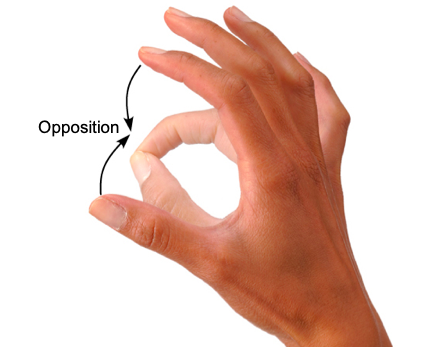
Opposition: movement of thumb
Example: touching thumb to tips of other fingers on same hand
or any grasping movement
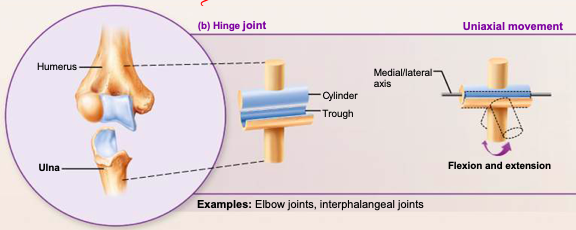
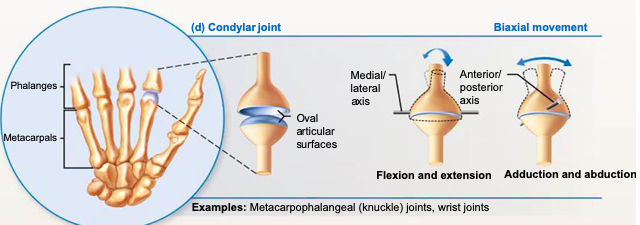
Six different types of synovial joints
Categories are based on shape of articular surface, as well as movement joint is capable of
- Plane
- Hinge
- Pivot
- Condylar
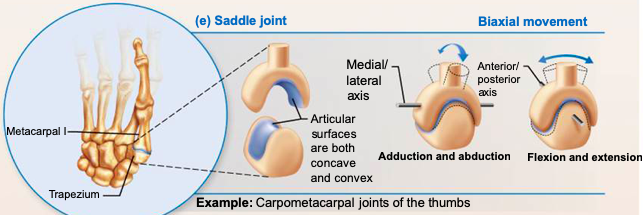
- Saddle
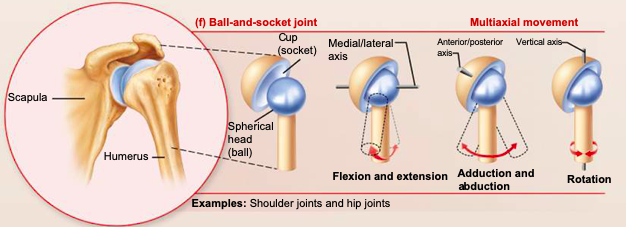
- Ball-and-socket
Synovial Plane Joint - diagram
Synovial Hinge Joint - diagram
Synovial Pivot Joint - diagram
Synovial Condylar Joint - diagram
Synovial Saddle Joint - diagram
Synovial Ball-and-socket Joint: diagram
Knee Joint
- Largest, most complex joint of body. Consists of joints surrounded by single cavity.
- Joint capsule is thin and absent anteriorly
- Anteriorly, quadriceps tendon gives rise to 3 broad ligaments that run from patella to tibia
-
Medial and lateral
patellar retinacula that flank
the patellar ligament
- Doctors tap patellar ligament to test knee-jerk reflex
- At least 12 bursae associated with knee joint
Knee Joint: Femoropatellar joint
Femoropatellar joint (femur & patella)
- Plane joint
- Allows gliding motion during knee flexion
Knee Joint: Lateral & Medial Joints
- Lateral joint and
-
Medial joint
- Lateral and medial joints together are called tibiofemoral joint (femur & tibia)
- Joint between femoral condyles and lateral and medial menisci of tibia
- Hinge joint that allows flexion, extension, and some rotation when knee partly flexed
Three ligaments that act to stabilize knee joint
Capsular, extracapsular, or intracapsular ligaments
Intracapsular ligaments
1 of 3 ligaments that act to stabilize knee joint
Intracapsular ligaments reside within capsule, but
outside synovial cavity:
-Help to prevent anterior-posterior
displacement
-Anterior cruciate ligament
(ACL)
*Attaches to anterior tibia & prevents
forward sliding of tibia and stops hyperextension of knee
-Posterior cruciate ligament (PCL)
*Attaches
to posterior tibia & prevents backward sliding of tibia and
forward sliding of femur
Capsular, extracapsular ligaments
2 of 3 ligaments that act to stabilize knee joint:
-
Capsular & extracapsular
ligaments help prevent hyperextension of knee
- Fibular & tibial collateral ligaments: prevent rotation when knee is extended
- Oblique popliteal ligament: stabilizes posterior knee joint
- Arcuate popliteal ligament: reinforces joint capsule posteriorly
Common Knee Injuries
Knee absorbs great amount of vertical force; however, it is
vulnerable to horizontal blows
Common knee
injuries involved the 3 C’s:
1. Collateral ligaments
(tibia & fibula)
2. Cruciate ligaments (ant /
posterior)
3. Cartilages (menisci) (medial & lateral)
–Lateral blows to extended knee can result in tears in tibial collateral ligament, medial meniscus, & anterior cruciate ligament
–Injuries affecting just ACL are common in runners who change direction, twisting ACL
–Surgery usually needed for repairs
Common Joint Injuries: Cartilage Tears
Cartilage tears:
- Due to compression and shear stress
- Fragments may cause joint to lock or bind
- Cartilage rarely repairs itself
- Repaired with arthroscopic surgery
- Partial menisci removal renders joint less stable but mobile; complete removal leads to osteoarthritis
- Meniscal transplant possible in younger patients
- Perhaps meniscus grown from own stem cells in future
Common Joint Injuries: Sprains
Sprains
- Reinforcing ligaments are stretched or torn
- Common sites are ankle, knee, & lumbar region of back
- Partial tears repair very slowly because of poor vascularization
- 3 options if torn completely:
- Ends of ligaments can be sewn together
- Replaced with grafts
- Just allow time and immobilization for healing