Instructions for Side by Side Printing
- Print the notecards
- Fold each page in half along the solid vertical line
- Cut out the notecards by cutting along each horizontal dotted line
- Optional: Glue, tape or staple the ends of each notecard together
Activity 1: Identifying Urinary System Organs
front 1 Metabolism of nutrients by the body produces what 3 wastes that must be eliminated from the body? | back 1 1. Carbon dioxide 2. Nitrogenous wastes 3. Ammonia |
front 2 The urinary system is primarily responsible for the removal of what type of wastes? | back 2 Nitrogenous wastes |
front 3 In addition to the removal of nitrogenous wastes, the kidney of the urinary system also has what 3 important functions? (Hint: Think ions, acid-base, and fluid..) | back 3 1. Electrolyte balance 2. Acid-base balance 3. Fluid balances of the blood |
front 4 The kidneys also produce what fluid? | back 4 Urine |
front 5 Is the kidney a major homeostatic organ of the body? | back 5 Yes |
front 6 To perform all its functions, the kidney first acts as what type of filter and then as what type of processor? | back 6 It first acts as a blood filter and then as a filtrate processor. |
front 7 The kidney allows what 3 substances to leave the body in the urine while simultaneously doing what? | back 7 1. Toxins 2. Metabolic wastes 3. Excess ions ...while simultaneously retaining needed substances and returning them to the blood |
front 8 Malfunction of the urinary system, especially of the kidneys, leads to a failure in homeostasis, which uncorrected, is fatal. T/F? | back 8 True |
front 9 The urinary system consists of what 4 structures? | back 9 1. Kidneys (paired) 2. Ureters (paired) 3. Urinary bladder 4. Urethra |
front 10 Of the urinary system, the ureters, urinary bladder, and urethra provide what 2 functions? | back 10 1. Provide temporary storage reservoirs 2. Act as transportation channels |
front 11 Why is the right kidney slightly lower than the left kidney? | back 11 It is crowded by the liver |
front 12 How many layers of support tissue surround each kidney (from the innermost layer to the outermost layer)? What are they? | back 12 1. Fibrous capsule 2. Perirenal fat capslue 3. Renal fascia |
front 13 Describe the texture of the renal fascia? | back 13 Fibrous |
front 14 What is the function of the fibrous renal fascia? | back 14 Holds the kidneys in place in a retroperitoneal position |
front 15 In cases of rapid weight loss or in very thin individuals, what may happen to the fat capsule? | back 15 It may be reduced in amount |
front 16 1. When the fat capsule of the kidneys is reduced with rapid weight loss or in very thin individuals, what is the consequence? 2. What is the condition above called? | back 16 1. The kidneys are less anchored and may drop to a more inferior position in the abdominal cavity 2. Ptosis |
front 17 The renal arteries diverge from what major artery and plunge into what area of the kidney? | back 17 Diverge from the descending aorta and plunge into the renal hilum |
front 18 What blood vessels drain the kidneys? | back 18 Renal veins |
front 19 What is the function of the two ureters? | back 19 Carry urine from the kidneys to the bladder |
front 20 How do the two ureters move the urine from the kidneys? | back 20 By peristalsis |
front 21 Is the bladder involved in temporary storage? | back 21 Yes |
front 22 Which part of the urinary system drains the urinary bladder? | back 22 The urethra |
front 23 The triangular region of the bladder that lies above the opening of the urethra and is delineated by the openings of the ureters is referred to as what? | back 23 The trigone |
front 24 The urethra travels the length of what organ in males? | back 24 The penis |
front 25 The urethra in males is made up of what 3 regions? | back 25 1. Prostatic urethra 2. Intermediate part of the urethra aka membranous urethra 3. Spongy urethra |
front 26 1. The male urethra has how many functions? 2. About how long is the male urethra? | back 26 1. Two 2. About 20 cm or 8inches long |
front 27 What are the 2 functions of the male urethra? | back 27 1. Carries urine to the body exterior 2. Provides a passageway for semen ejaculation |
front 28 In males, the urethra is part of what 2 systems? | back 28 1. Urinary system 2. Reproductive system |
front 29 1. Compared to the male urethra, are there any reproductive pathways in the female urethra? 2. About how long is the female urethra? | back 29 1. No 2. About 4 cm or 1.5 inches long |
front 30 What is the sole function of the female urethra? | back 30 Serves to transport urine to the body exterior |
front 31 What is the external opening of the male and female urethra? | back 31 The external urethral orifice |
front 32 How does the fibrous capsule adhere to the kidney and to which aspect? (Hint: think external or internal.) | back 32 Adheres tightly to the external aspect of the kidney |
front 33 What 3 structures enter the renal hilum? | back 33 1. Ureter 2. Renal vein 3. Renal artery |
front 34 Of the ureter, renal vein, and renal artery, which one has the thinnest wall and will be collapsed? | back 34 Renal vein |
front 35 Of the ureter, renal vein, and renal artery, which one has the thickest wall? | back 35 Ureter |
front 36 Where is the renal cortex located? | back 36 Superficial kidney region or outermost region |
front 37 The renal cortex is rich in what type of supply? | back 37 Vascular supply |
front 38 In the medullary region, the medulla is separated into what regions? | back 38 Renal pyramids |
front 39 How do the renal pyramids appear? (Hint: striped or non-striped?) | back 39 They are striped |
front 40 The base of each pyramid faces toward what region of the kidney? | back 40 Toward the cortex of the kidney |
front 41 The part of the renal pyramids that points to the innermost kidney region is called what? | back 41 Papilla or apex |
front 42 The renal columns are similar in appearance to what region of the kidney? | back 42 The renal cortex |
front 43 What is the function of the renal columns? | back 43 Separate the renal pyramids |
front 44 Extending inward from the hilum is what basin-like cavity that is continuous with the ureter? | back 44 The renal pelvis |
front 45 The ureter exits from what region of the kidney? | back 45 The hilum region |
front 46 What is the larger or primary extension of the renal pelvis called? | back 46 Major calyx |
front 47 A smaller subdivision of the major calyx is called what? | back 47 Minor calyx |
front 48 A minor calyx terminates in cup-like areas that enclose what? | back 48 The apexes or papilla of the renal pyramids |
front 49 What is the function of a minor calyx? | back 49 To collect urine draining from the apexes or papilla of the renal pyramids and transfer it to the renal pelvis |
front 50 What fraction of the total blood flow of the body is delivered to the kidneys each minute? | back 50 1/4 |
front 51 What vessels deliver blood to the kidneys? | back 51 Renal arteries |
front 52 As a renal artery approaches the kidney, it breaks up into what arteries? | back 52 Segmental arteries |
front 53 1. The segmental arteries enter what region of the kidneys? 2.The segmental arteries further break up into what arteries? | back 53 1. Renal hilum 2. Interlobar arteries |
front 54 The interlobar arteries extend outward toward what region of the kidneys? | back 54 Renal cortex |
front 55 Approaching the base of the renal pyramids, the interlobar arteries further branch into what arteries? | back 55 Arcuate arteries |
front 56 The arcuate arteries curve over which part of the renal pyramids? | back 56 Base of the renal pyramids |
front 57 The arcuate arteries further branch into what arteries and extend into what region of the kidneys? | back 57 Further branch into cortical radiate arteries that ascend into the cortex |
front 58 In the cortical region of the kidneys, the cortical radiate arteries further branch off into what blood vessels? | back 58 Afferent arterioles |
front 59 Afferent arterioles enter which specific structure of the kidney? (Hint: part of the nephron) | back 59 The glomerulus |
front 60 The glomerulus is a ball of what blood vessel? | back 60 A ball of capillaries |
front 61 What blood vessels drain the glomerulus? | back 61 Efferent arterioles |
front 62 The efferent arterioles that drain the glomerulus feed into one of what 2 capillary beds? | back 62 1. Peritubular capillaries 2. Vasa recta |
front 63 Blood draining from the peritubular capillaries or vasa recta then enter what blood vessels? | back 63 The cortical radiate veins |
front 64 The cortical radiate veins then drain into what blood vessels? | back 64 Arcuate veins |
front 65 The arcuate veins then drain into what blood vessels? | back 65 Interlobar veins |
front 66 The interlobar veins then drain into what blood vessel? | back 66 The renal vein |
front 67 The renal veins then drain into what major blood vessel? | back 67 The inferior vena cava |
front 68 Trace a drop of blood from the renal artery to the renal vein. (Hint: 13 steps) | back 68 1. Renal artery 2. Segmental arteries 3. Interlobar arteries 4. Arcuate arteries 5. Cortical radiate arteries 6. Afferent arterioles 7. Glomerulus 8. Efferent arterioles 9. Vasa recta or peritubular capillaries 10. Cortical radiate veins 11. Arcuate veins 12. Interlobar veins 13. Renal vein |
front 69 Each kidney contains over a million what? | back 69 Nephrons |
front 70 What are the structural and functional units of the kidneys? | back 70 Nephrons |
front 71 What are the 2 functions of the nephrons? | back 71 1. Filtering the blood 2. Forming urine |
front 72 Each nephron consists of what 2 major structures? | back 72 1. Renal corpuscle 2. Renal tubule |
front 73 What are the 3 structures within the renal corpuscle? (Hint: Think capillaries and 2 other layers) | back 73 1. Glomerulus 2. Visceral layer of the glomerular capsule 3. Parietal layer of the glomerular capsule |
front 74 The glomerulus is made up of what epithelium? | back 74 Fenestrated endothelium or simple squamous epithelium |
front 75 What is the function of the glomerulus? | back 75 Forms part of the filtration membrane |
front 76 The visceral layer of the glomerular capsule is composed of what type of cells? | back 76 Podocytes |
front 77 The visceral layer of the glomerular capsule is composed of what type of epithelium? | back 77 Simple squamous epithelium |
front 78 What is the function of the podocytes of the visceral layer of the glomerular capsule? | back 78 Forms part of the filtration membrane |
front 79 The spaces between the podocytes form what type of slits? | back 79 Filtration slits |
front 80 The parietal layer of the glomerular capsule is composed of what type of epithelium? | back 80 Simple squamous epithelium |
front 81 What is the function of the parietal layer of the glomerular capsule? | back 81 Forms the outside of the glomerular capsule |
front 82 Does the parietal layer of the glomerular capsule play any role in filtration? | back 82 No |
front 83 What are the 6 structures within the renal tubule (following the glomerular capsule)? | back 83 1. Proximal convoluted tubule (PCT) 2. Descending limb of the nephron loop 3. Descending thin limb of the nephron loop 4. Thick ascending limb of the nephron loop 5. Distal convoluted tubule (DCT) 6. Collecting duct |
front 84 What is the epithelium of the proximal convoluted tubule? | back 84 Simple cuboidal |
front 85 1. Does the proximal convoluted tubule contain many mitochondria? 2. Does the proximal convoluted tubule contain many microvilli? | back 85 1. Yes 2. Yes |
front 86 1. What is the main function of the proximal convoluted tubule? 2. Does some secretion also occur? | back 86 1. Primary site of tubular reabsorption of water and solutes 2. Yes |
front 87 What is the epithelium of the descending limb of the nephron loop? | back 87 Simple cuboidal epithelium |
front 88 What is the microvilli concentration like in the descending limb of the nephron loop? | back 88 Some microvilli, decreased in number compared to the concentration seen in the PCT |
front 89 What are the 2 functions of the descending limb of the nephron loop? | back 89 1. Tubular reabsorption 2. Tubular secretion |
front 90 What is the epithelium of the descending thin limb of the nephron loop? | back 90 Simple squamous epithelium |
front 91 What is the concentration of aquaporins like in the descending thin limb of the nephron loop? | back 91 Many aquaporins |
front 92 1. What is the main function of the descending thin limb of the nephron loop? (Hint: think water) 2. Is the descending thin limb of the nephron permeable to water? | back 92 1. Water is reabsorbed, but no solutes are reabsorbed. 2. Yes |
front 93 What are the 2 epitheliums of the thick ascending limb of the nephron loop? | back 93 1. Cuboidal epithelium 2. Low columnar epithelium |
front 94 What is the concentration of aquaporins like in the thick ascending limb of the nephron loop? | back 94 Very few aquaporins |
front 95 1. What is the main function of the thick ascending limb of the nephron loop? 2. Is the thick ascending limb of the nephron loop permeable to water? | back 95 1. Passive and active reabsorption of solutes 2. Not permeable to water |
front 96 What is the epithelum of the distal convoluted tubule? | back 96 Simple cuboidal |
front 97 1. What is the microvilli concentration in the distal convoluted tubule? 2. What is the mitochondria concentration in the distal convoluted tubule? | back 97 1. Few microvilli 2. Many mitochondria |
front 98 What are the 2 main functions of the distal convoluted tubule? | back 98 1. Some reabsorption of water and solutes 2. Some secretion |
front 99 The collecting duct receives filtrate from what structure within the renal tubule? | back 99 Receives filtrate form the distal collecting tubule of many nephrons |
front 100 What is the epithelium of the collecting duct? | back 100 Simple cuboidal |
front 101 What 2 specialized cells are also found in the collecting duct? | back 101 1. Principal cells 2. Intercalated cells |
front 102 1. What is the function of principal cells? 2. What is the function of intercalated cells? | back 102 1. Electrolyte homeostasis 2. Maintain acid-base homeostasis |
front 103 What are the 4 functions of the collecting duct? | back 103 1. Some reabsorption of body fluids 2. Some secretion of body fluids 3. Maintain blood pH 4. Regulate solute concentrations |
front 104 What are the 2 kinds of nephrons? | back 104 1. Cortical nephrons 2. Juxtamedullary nephrons |
front 105 What are the most numerous type of nephrons, and they comprise what percentage of all the body's nephrons? | back 105 Cortical nephrons are the most numerous ones, and they make up about 85% of all nephrons |
front 106 Cortical nephrons are located almost entirely within what region of the kidney? | back 106 The renal cortex |
front 107 Although cortical nephrons are almost entirely located within the renal cortex, small parts of their loops do dip into what area of the kidney? | back 107 The renal medulla |
front 108 How are the renal corpuscles of juxtamedullary nephrons different from the renal corpuscles of cortical nephrons (in regards to location in the renal cortex)? | back 108 The renal corpuscles of juxtamedullary nephrons are located deep in the renal cortex at the border with the renal medulla |
front 109 How are the long nephron loops of juxtamedullary nephrons different from the nephron loops of cortical nephrons (in regards to location in the renal medulla)? | back 109 Their long nephron loops penetrate deeply into the medulla |
front 110 Which group of nephrons play an important role in concentrating urine? | back 110 Juxtamedullary nephrons |
front 111 The function of the nephron depends on what 3 features of renal circulation? | back 111 1. Glomerular filtration 2. Tubular resorption 3. Tubular secretion |
front 112 What are the 3 capillary vascular supply of nephrons? | back 112 1. Glomerulus 2. Pertitubular capillary bed 3. Vasa recta |
front 113 Of the 3 capillary beds, glomerulus, peritubular capillary bed, and vasa recta, which one is first encountered in the nephron? | back 113 Glomerulus |
front 114 Vessels leading to and from the glomerulus are what type of arterioles? | back 114 Glomerular arterioles |
front 115 Which arteriole feeds the glomerulus and which arteriole drains it? | back 115 The afferent arteriole feeds the glomerulus, and the efferent arterole drains it. |
front 116 Why is the glomerular capillary bed unique in the body? (Hint: think pressure) | back 116 It is a high-pressure bed |
front 117 The glomerular capillary bed is a high-pressure bed because of what reason? | back 117 The afferent feeder arteriole is larger in diameter than the efferent arteriole draining it |
front 118 How are fluid and blood components smaller than proteins forced out of the glomerulus into the glomerular capsule? | back 118 The afferent and efferent arterioles create high hydrostatic pressure to force fluid and blood components out of the glomerulus into the glomerular capsule |
front 119 Fluid and blood components forced out of the glomerulus into the glomerular capsule (through the high hydrostatic pressure created by afferent and efferent arterioles) form what, and what is it processed by? | back 119 The filtrate is formed, which is processed by the nephron tubule |
front 120 Efferent arterioles that supply cortical nephrons and drain the glomerulus tend to form what specific type of capillary bed? | back 120 The peritubular capillary bed |
front 121 How does this set of capillaries cling to the renal tubule? | back 121 They cling very closely to the renal tubule |
front 122 Describe the peritubular capillary bed in regards to pressure and porosity? | back 122 Low-pressure, high porosity |
front 123 The peritubular capillary bed is mainly adapted for what function? (Hint: absorption or filtration?) | back 123 Absorption |
front 124 Since the peritubular capillary bed is mainly adapted for absorption rather than filtration, what 2 substances does it take up from the filtrate? | back 124 1. Solutes 2. Water |
front 125 Which cells process and resorb the solutes and water of the filtrate, two substances that are eventually absorbed again by the peritubular capillary bed? | back 125 Tubule cells |
front 126 Efferent arterioles that supply juxtaglomerular nephrons tend not to form peritubular capillaries, and instead, form what specific capillary bed? | back 126 The vasa recta |
front 127 Differentiate the structure of the peritubular capillary bed and the vasa recta in regards to structure and how the run to their nephron loops. | back 127 The peritubular capillary bed clings intimately to its renal tubule and is very coiled. The vasa recta runs parallel to its renal tubule and also clings close, but it is not coiled. |
front 128 The vasa recta is essential for what to happen? | back 128 The concentration of urine |
front 129 Each nephron also has what complex? | back 129 A juxtaglomerular complex |
front 130 Where is the juxtaglomerular complex located? (Hint: think of the nephron loop and the afferent arteriole) | back 130 Located where the most distal portion of the ascending limb of the nephron loop touches the afferent arteriole |
front 131 What 2 cell types form the juxtaglomerular complex? | back 131 1. Granular cells or juxtaglomerular cells 2. Macula densa cells |
front 132 1. The granular cells or juxtaglomerular cells are located where? 2. What is their function? | back 132 1. Located in the arteriole walls of the afferent arteriole 2. Sense blood pressure in the afferent arteriole |
front 133 1. The macula densa cells are located where? 2. What is their function? | back 133 1. Located in the most distal portion of the ascending limb of the nephron loop 2. Monitors sodium chloride concentration in the filtrate |
front 134 What are the 2 functions of the juxtaglomerular complex? | back 134 1. Regulate the rate of filtration based on the salt concentration 2. Regulate systemic blood pressure |
front 135 Urine forms as a result of what 3 processes? | back 135 1. Glomerular filtration 2. Tubular resorption 3. Tubular secretion |
front 136 Glomerular filtration is accomplished by feature of the nephron? | back 136 The glomerulus |
front 137 Is glomerular filtration passive or active? | back 137 Passive |
front 138 Describe glomerular filtration. | back 138 A portion of the blood passes from the glomerular capillary into the glomerular capsule |
front 139 What happens during tubular resorption? (Hint: Filtrate components move through what cells and return to what?) | back 139 Filtrate components move through the tubule cells and return to the blood in the peritubular capillaries |
front 140 1. Is tubular resorption passive or active, or both? 2. If both, describe what is passively resorbed (by what process) and what is actively resorbed? | back 140 1. Both 2. Water is passively resorbed by osmosis, but most substances are actively resorbed. |
front 141 What are 3 substances that are almost entirely resorbed from the filtrate? | back 141 1. Water 2. Glucose 3. Amino acids |
front 142 Of water, glucose, and amino acids, what is passively resorbed, and what 2 are actively resorbed? | back 142 Water is passively resorbed, while glucose and amino acids are actively resorbed. |
front 143 Is active resorption highly selective? | back 143 Yes |
front 144 Various ions are selectively resorbed or allowed to go out into the urine based on what 2 conditions? | back 144 1. What is required to maintain appropriate blood pH 2. What is required to maintain appropriate electrolyte composition |
front 145 What 4 substances are resorbed to a lesser degree or not resorbed at all? | back 145 1. Urea 2. Creatinine 3. Uric acid 4. Drug metabolites |
front 146 Most of tubular resorption occurs in what part of the nephron tubule? (Hint: Give the percentage of tubular resorption for the associated part of the tubule) | back 146 Most (about 75-85%) of tubular resorption occurs in the proximal convoluted tubule |
front 147 Tubular secretion is the reverse process of what of the 3 process that form urine: glomerular filtration, tubular resorption, and tubular secretion? | back 147 Tubular resorption |
front 148 1. What 3 substances move from the blood of the peritubular capillaries through the tubular cells into the filtrate to be disposed of in urine? 2. Describe the process of tubular secretion from the blood in the peritubular capillaries to urine. (Hint: 4 steps) | back 148 1. Hydrogen 2. Potassium ions 3. Creatinine ____________________ 1. Peritubular capillaries 2. Tubular cells 3. Filtrate 4. Urine |
front 149  Identify the blanks. | back 149 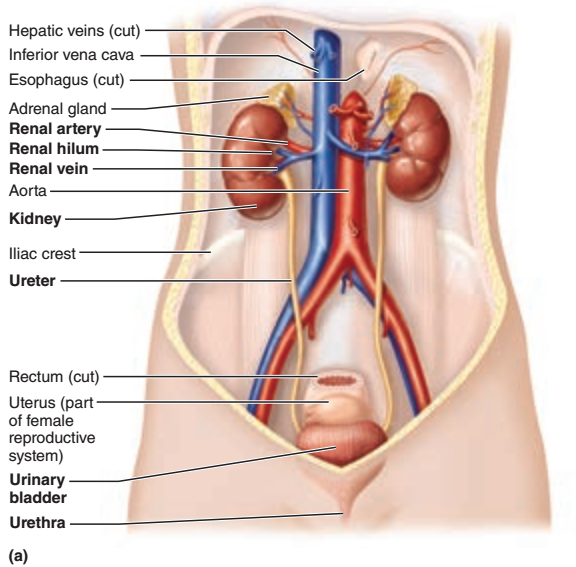 |
front 150  Identify the blanks. | back 150 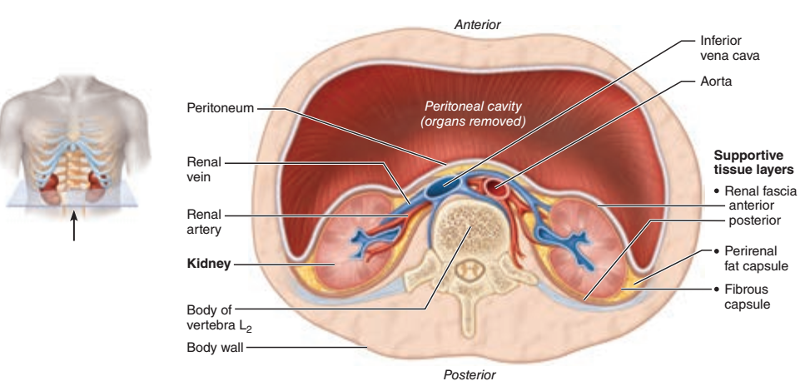 |
front 151  Identify the blanks. | back 151 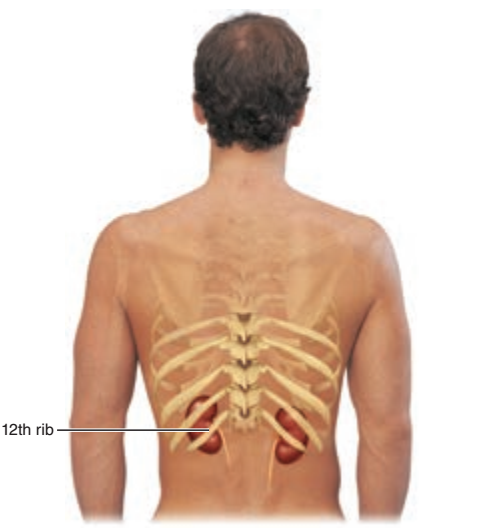 |
front 152 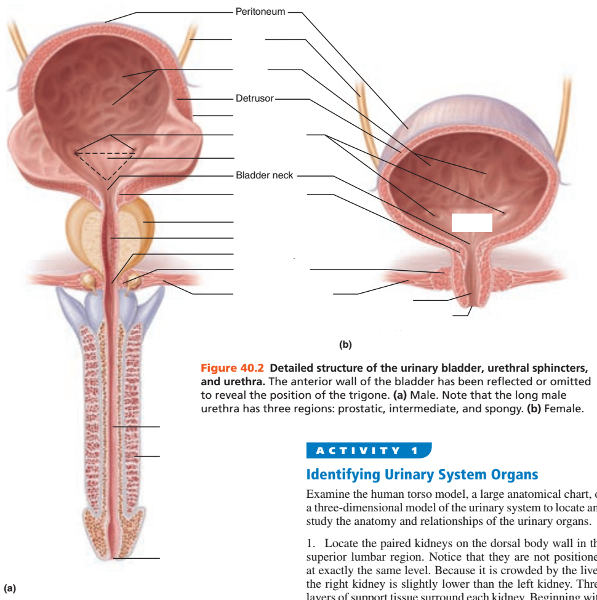 Identify the blanks. | back 152 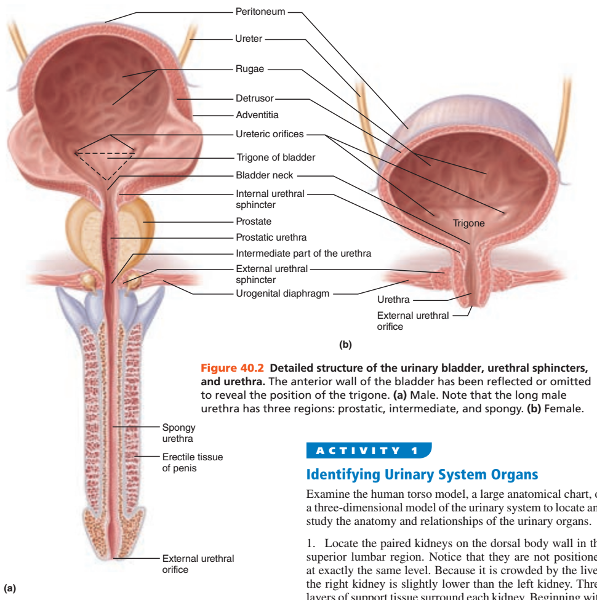 |
front 153 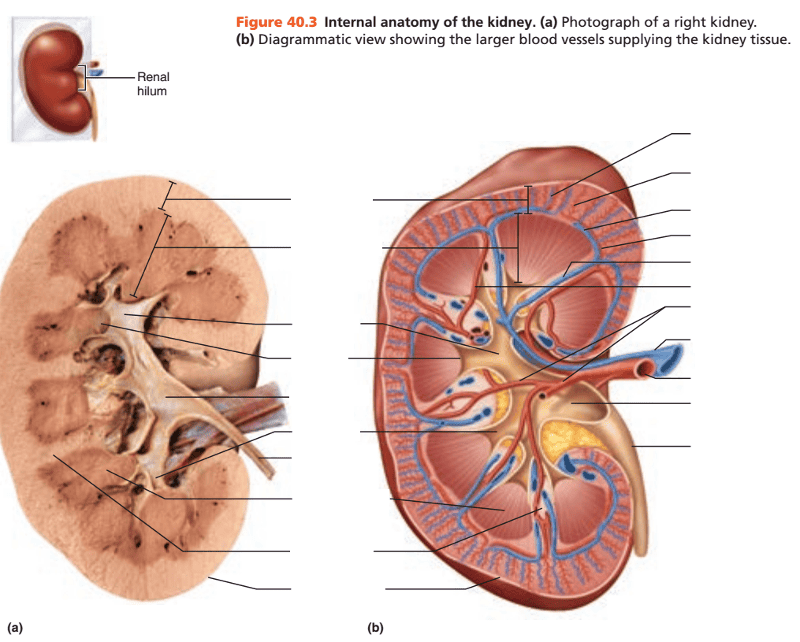 Identify the blanks. | back 153 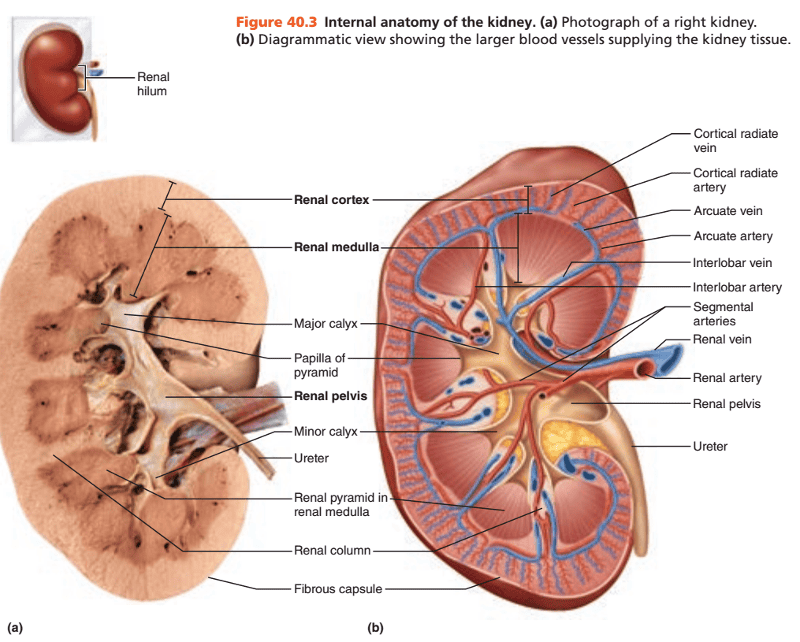 |
front 154 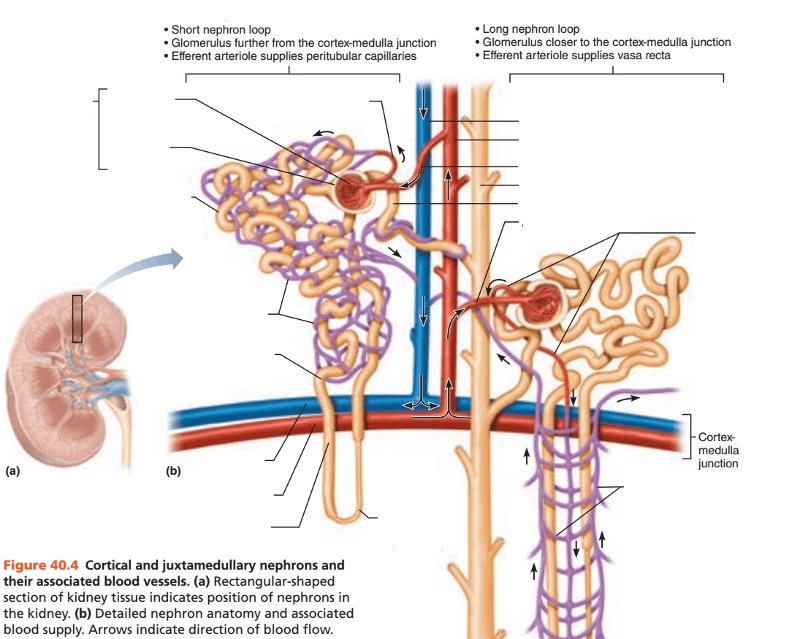 Identify the blanks. | back 154 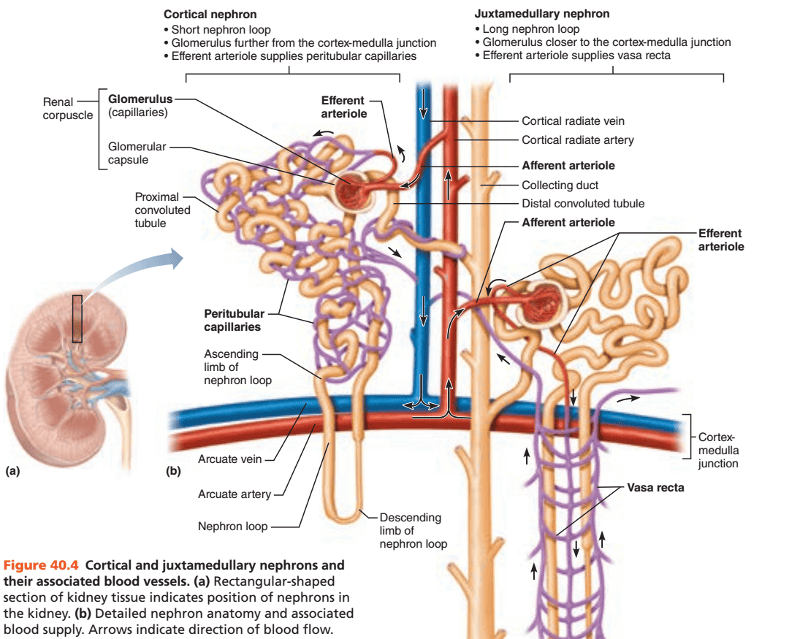 |
front 155 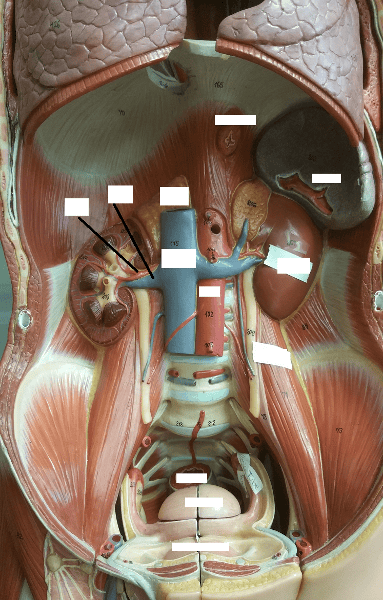 Identify the blanks. | back 155 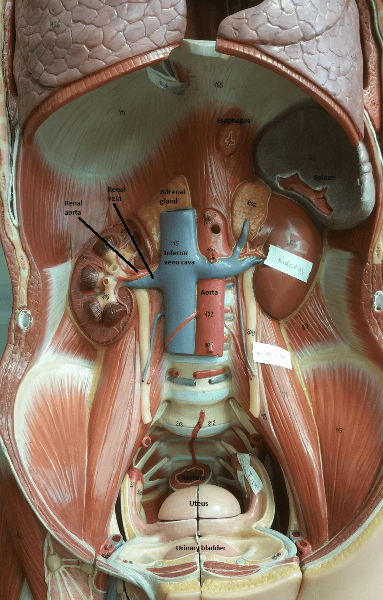 |
front 156  Identify the blanks. | back 156 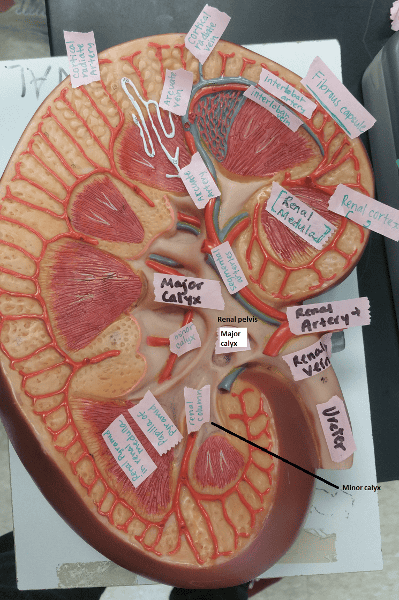 |
front 157 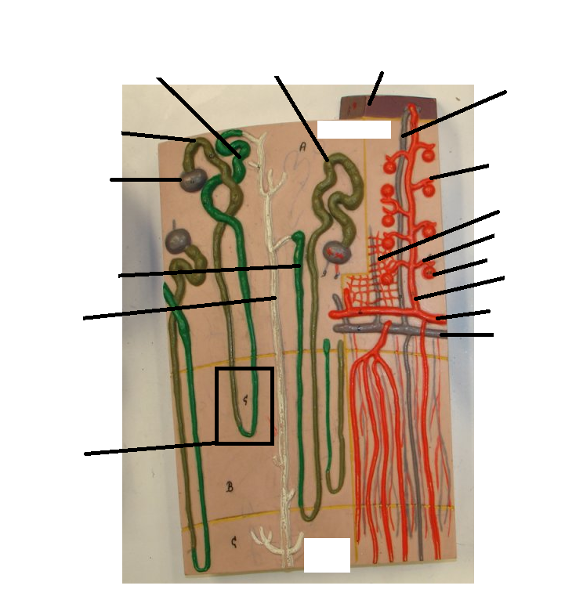 Identify the blanks. | back 157 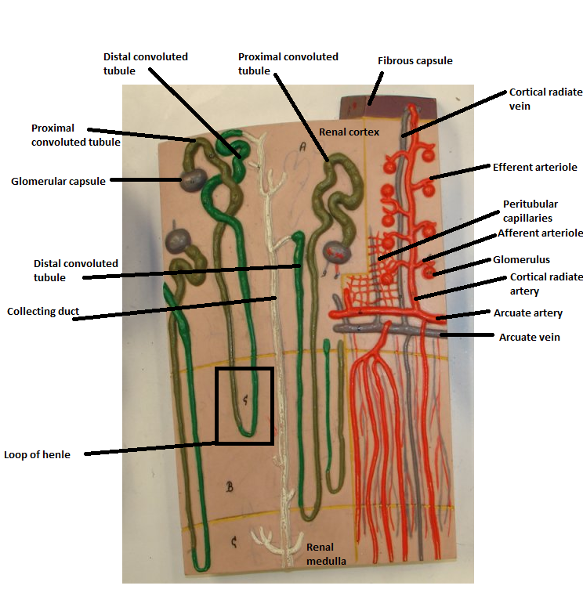 |
front 158  Identify the blanks. | back 158 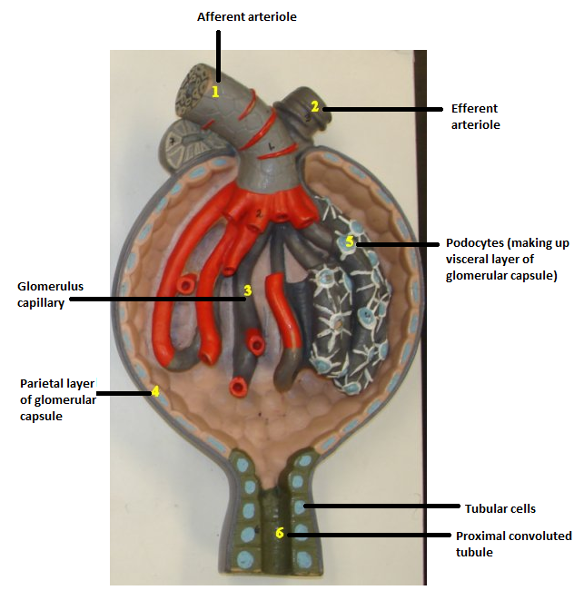 |
front 159 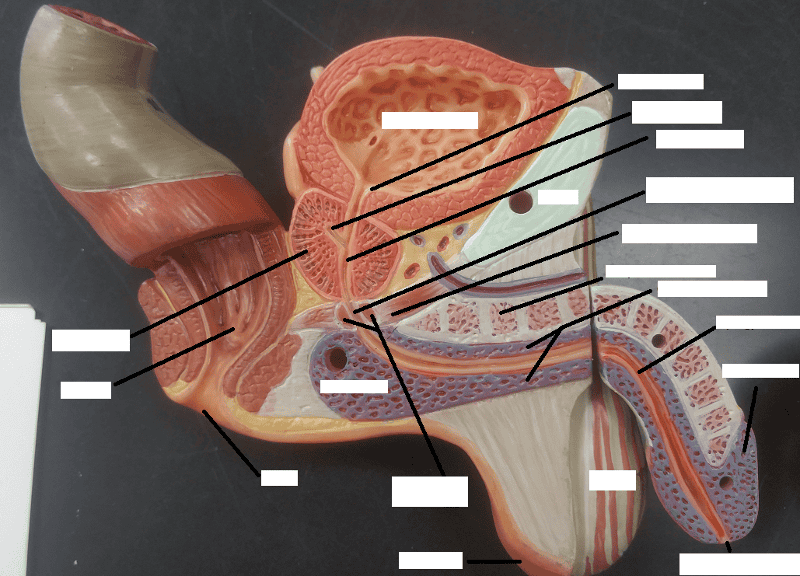 | back 159 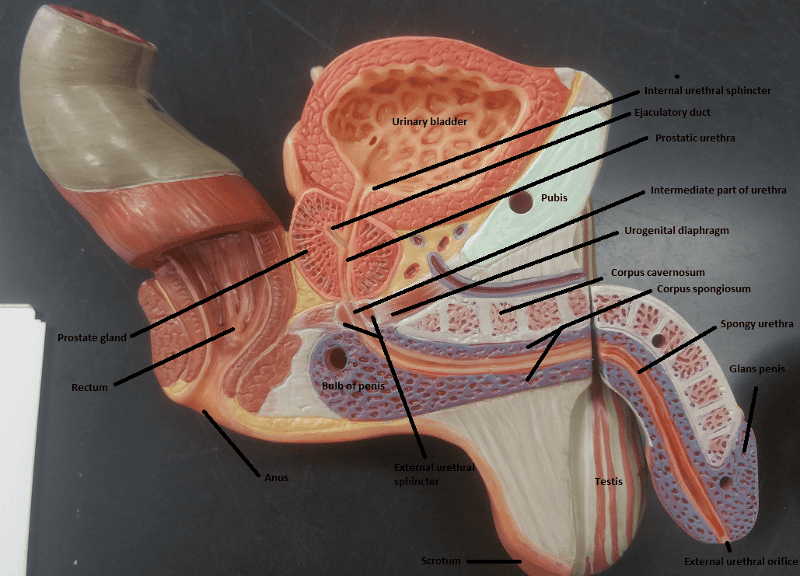 |
front 160 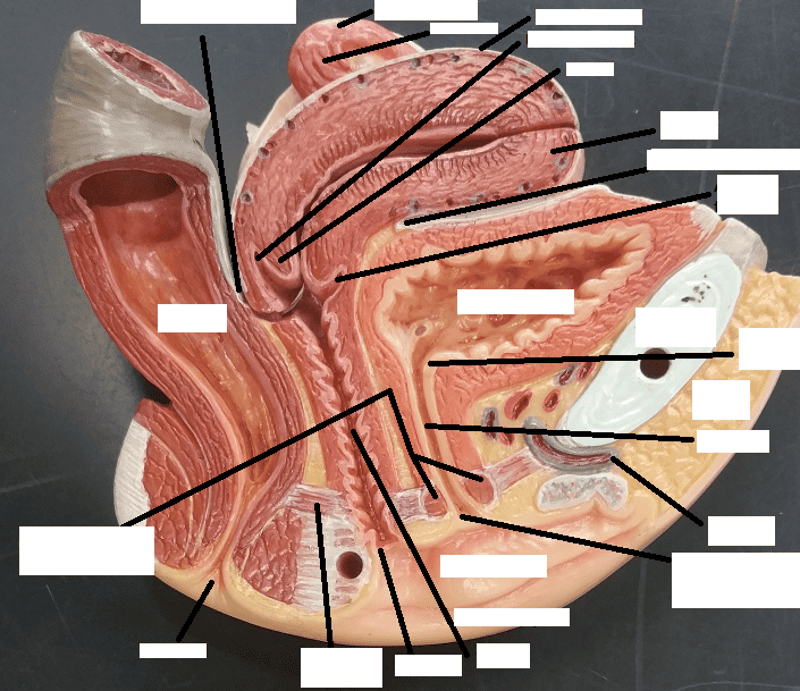 | back 160  |