Instructions for Side by Side Printing
- Print the notecards
- Fold each page in half along the solid vertical line
- Cut out the notecards by cutting along each horizontal dotted line
- Optional: Glue, tape or staple the ends of each notecard together
Bilateral lower extremity
front 1 What are the primary reasons for Venous vascular leg exam? | back 1
|
front 2 How do the deep veins course? | back 2 adjacent to major arteries and have the same names as the arteries (exception- IVC) |
front 3 How much blood do the deep veins in the legs carry? | back 3 85% of blood volume |
front 4 Name the deep veins in the pelvis? | back 4 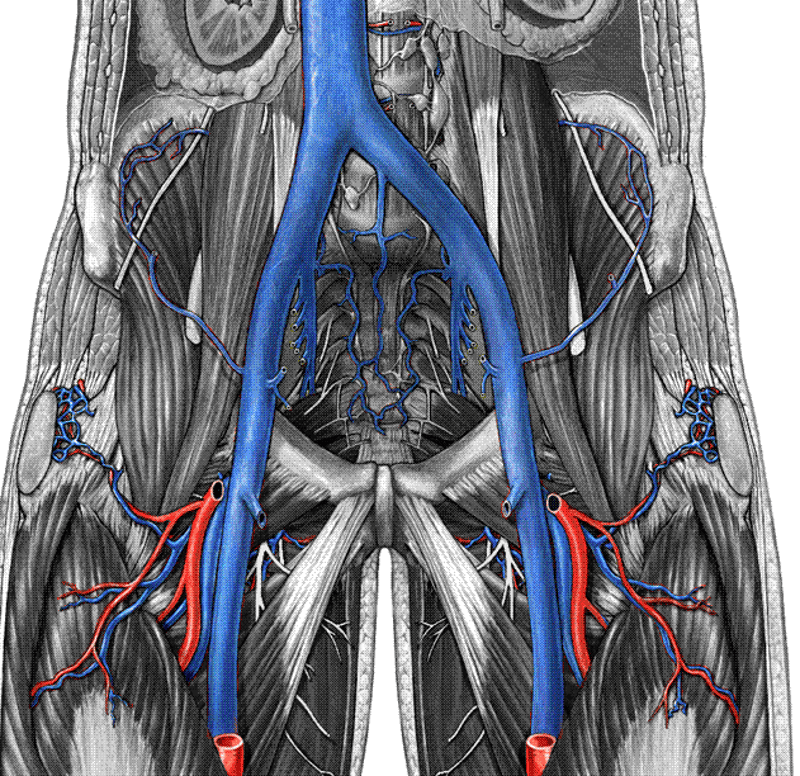 Inferior Vena Cava (IVC) Common Iliac Vein (CIV) Internal Iliac Vein (IIV) External Iliac Vein (EIV) |
front 5 What is another name for the internal iliac vein? | back 5 Hypogastric vein |
front 6 Name the deep veins in the thigh. | back 6 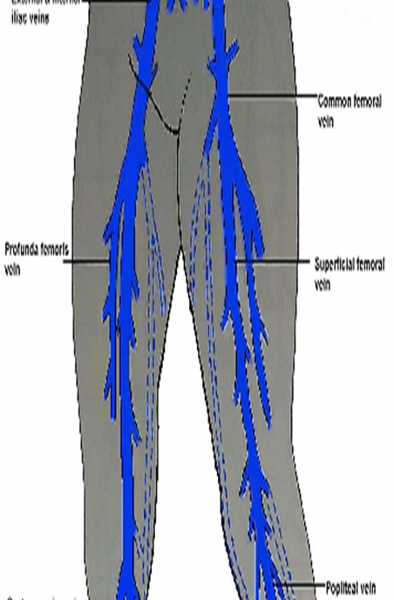 Common Femoral Vein (CFV) Profunda Femoris Vein (PFV) Femoral Vein (FV) |
front 7 When does the external illiac become the common femoral | back 7 after it crosses the inguinal ligament |
front 8 What is another name for the Profunda Femoris Vein? | back 8 Deep Femoral vein (DFV) |
front 9 Where does the greater saphenous start and end? | back 9 starts at ankle joins the common femoral at the groin |
front 10 What was the Femoral vein previously known as? | back 10 Superficial Femoral Vein |
front 11 Where is the Femoral vein? | back 11 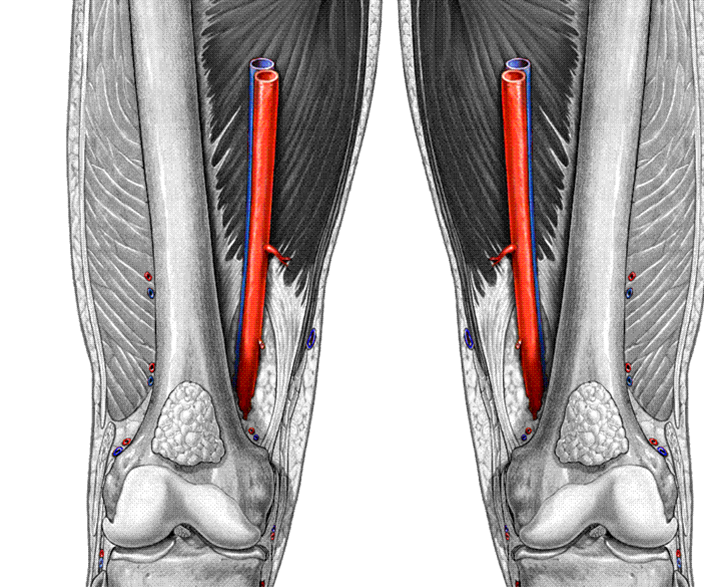 |
front 12 What is the name of the vein that runs behind the knee? | back 12 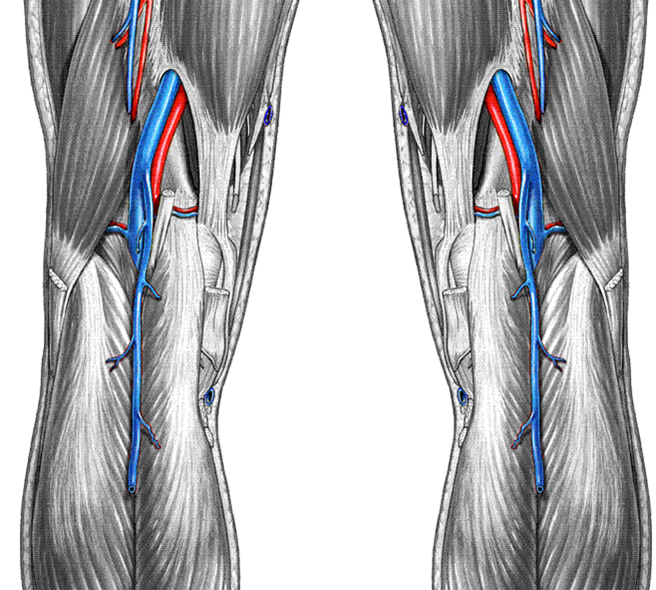 Popliteal vein (Pop V) |
front 13 When does the femoral vein become the popliteal vein? | back 13 when the femoral crosses the adductor canal |
front 14 Where is the Small Saphenous vein (SSV) ? | back 14 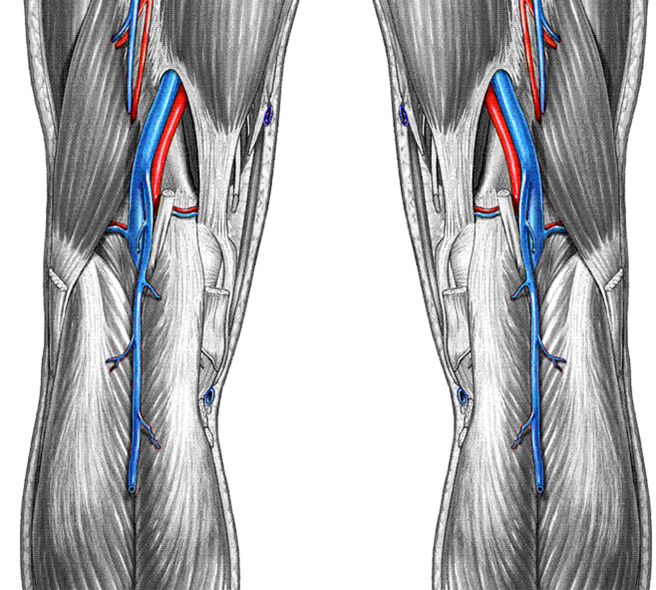 Small Saphenous vein (SSV) |
front 15 What was the Small Saphenous vein (SSV) previously known as? | back 15 Lesser Saphenous Vein (LSV) |
front 16 Name the veins in the calf. | back 16 Popliteal vein (Pop V) Gastrocnemius Veins Anterior Tibial Veins (ATVs) Posterior Tibial Veins (PTVs) Peroneal Veins (Per. V) |
front 17 All veins below the knee there are _____ veins to every one artery. | back 17 two 2 veins to every 1 artery |
front 18 The Anterior Tibial Veins (ATVs) courses ________. | back 18 lateral |
front 19 The Posterior Tibial Veins (PTVs) courses ________. | back 19 medial |
front 20 The Peroneal Veins (Per. V) courses ________. | back 20 deep medial |
front 21 Explain the course of the large saphenous vein. | back 21 GSV courses along the medial aspect of the leg from the ankle to the groin where it enters the deep system at the CFV (Saphenofemoral junction) |
front 22 What is the difference between the deep and superficial veins? | back 22 superficial lie above the muscle deep veins lie within muscle |
front 23 Explain the course of the small saphenous vein. | back 23 SSV courses up the posterior aspect of the lower leg from the Achilles tendon region to the Popliteal vein confluence in the Popliteal Fossa |
front 24 How many cases of DVT a year? | back 24 1 - 10 million |
front 25 How many cases of Pulmonary Embolus a year? | back 25 600,000 cases |
front 26 How many death a year from Pulmonary Embolus? | back 26 200,000 deaths |
front 27 What are the reasons for a BLE? | back 27 Stasis - bedrest - lack of movement hypercoagulability vein wall injury - stab, gunshot, IV drugs thrombofilia hormone replacement |
front 28 What are the Risk factors for DVT? | back 28 post - operative state previous DVT cancer thrombophilia
trauma pregnancy high dose estrogen RX Immobility (long car or plane ride) Bed-rest > 4 days Lower limb paralysis |
front 29 What are the symptoms of a DVT? | back 29
|
front 30 Leg swelling will be ________ if a DVT is present. | back 30 Leg swelling will be unilateral if a DVT is present. |
front 31 Why are DVTs have low sensitivity? | back 31 Many DVTs are clinically asymptomatic |
front 32 Why are DVTs have low specificity? | back 32 Non-thrombotic disorders can cause the same clinical symptoms as DVT |
front 33 What symptom has high positive predictive value for DVT? | back 33  Phlegmasia cerulea dolens |
front 34 What is Phlegmasia cerulea dolens? | back 34  massive thigh and calf swelling limb cyanosis iIlio - femoral outflow obstruction painful blue anemia |
front 35 superficial thrombophlebitis | back 35 erythema / inflammation (swelling) local tenderness palpable cord or mass usually more painful that DVT |
front 36 What is the main problem with superficial thromboplebitis? | back 36 hurts like hell but probably will not throw an embolism unless proximal to the deep wein system. |
front 37 What is the treatment with superficial thromboplebitis? | back 37 warm compress and aspirin |
front 38 What should be looked for on a physical exam? | back 38 swelling limb discoloration - venous insufficiency stasis dermatitis, ulceration varicose veins palpable “cords” (STP-superficial thrombophlebitis) |
front 39 What are the four parts o?f a Venous Duplex Techniques? | back 39 1.compressibility / coaptation of vein 2.visualization of thrombus 3.spectral Doppler - pos augmentation 4.color Doppler - wall to wall filling |
front 40 What are the techniques used for a Venous Duplex Techniques? | back 40 Torso elevated 10-20 degrees - tilted bed Leg rotated externally Start at groin crease in transverse plane |
front 41 What is coaptation? | back 41 close |
front 42 phasic & spontaneous flow | back 42 no data |
front 43 site 1 | back 43 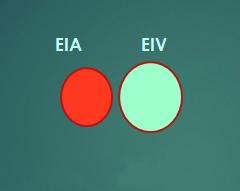 |
front 44 site 2 | back 44  |
front 45 site 3 | back 45 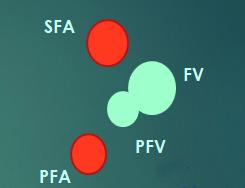 |
front 46 site 4 | back 46  |
front 47 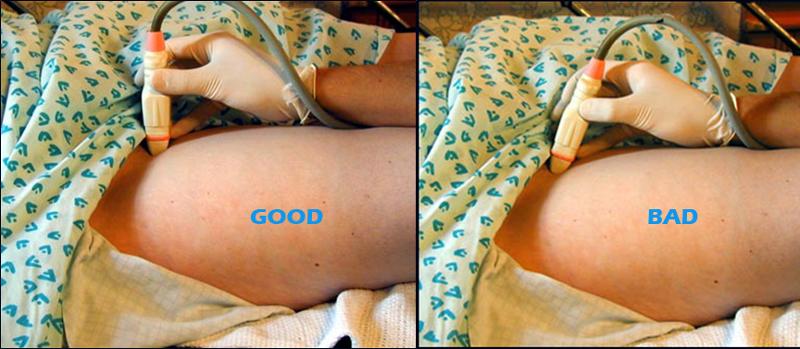 site 5+ | back 47 no data |
front 48 Why would you scan through the adductor canal? | back 48 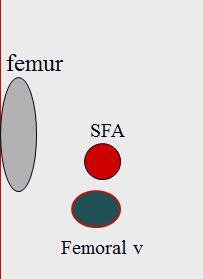 On many patients, this approach provides an excellent acoustic window to the FV and SFA in the adductor canal. However, you must compress from the posterior thigh |
front 49 What is the Valsalva Maneuver? | back 49 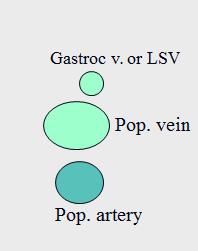 During inspiration, diaphragm moves downward and increases intra-abdominal pressure. IVC is compressed and venous outflow is temporarily reduced or stopped. Flow resumes during exhalation *bearing down like you are pooping stops slows blood flow |
front 50 If there is no close and back filling during valsalva maneuver what does this mean? | back 50 reflux |
front 51 Flow direction display | back 51 Traditionally, the Doppler waveform has been displayed below baseline This is not necessary with duplex ultrasound systems. |
front 52 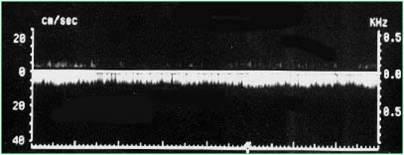 Continuous venous flow in CFV? | back 52 proximal obstruction |
front 53 Respiratory phasicity may not be present due to: | back 53 Shallow breathers, (patients with pulmonary embolus-PE). Patients who are lying supine. Patients who have their arms raised and hands behind their head. Spinal cord injured patients due to reduced abdominal muscle tone. Proximal DVT or extrinsic venous compression. |
front 54 Where is cardiac activity most influential? | back 54 thoracic vessels. |
front 55 Explain cardiac influence in the lower extremities | back 55 Cardiac influence is usually not apparent or is reduced in the lower extremities |
front 56  | back 56 Pulsatile flow due to congestive heart failure |
front 57 Where should you begin with Calf imaging? | back 57 at the ankle |
front 58 Which vessel should be identified first in the calf? | back 58 PTV |
front 59 What plain are the calf vessels imaged? | back 59 You may use color Doppler in transverse plane, but it’s not as good as in long view |
front 60 What are some methods to improve calf vein visualization? | back 60 Leg dependent position Maximum vein dilation ****Don’t expect spontaneous flow |
front 61 What is the leg dependent position? | back 61 reverse trndenburg |
front 62 When do we examine the anterior tibial veins? | back 62 Don’t bother ! Too tedious Too small They’re rarely involved unless there is extensive DVT in other vessels |
front 63 Explain the importance of Gastroc vein thrombosis. | back 63 May be clinically important if thrombus extends to popliteal vein. So, determine the extent of thrombus |
front 64 What should you do if the patient has tenderness in her calf? | back 64 If the patient is symptomatic (tenderness), look for muscular vein thrombosis |
front 65 Why must you augment most of the time in the calf? | back 65 Flow in calf veins is usually not spontaneous, you often must augment flow by squeezing the calf or ankle. |
front 66 Explain the most important perspective of bilateral lower extremity exam | back 66 thrombus anywhere from the popliteal to the iliac veins is life
threatening. |
front 67 What is the Criteria for Venous Thrombosis? | back 67 Absence of vein compressibility Visualization of thrombus Vein distention Abnormal Doppler signals Reduced / absent augmentation Reduced / absent color filling |
front 68 What is the sonographic appearance of acute DVT? | back 68 vein distended somewhat hypo-echoic no collaterals maybe free floating Tail!!!!!!!!!! |
front 69 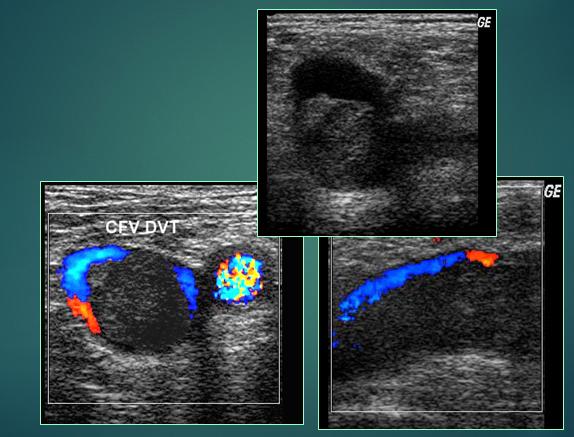 | back 69 Acute DVT CFV |
front 70 What must you do if PTV or peroneal vein thrombus is detected? | back 70 You must look carefully in the distal pop vein for propagation. It’s a difficult region to image. |
front 71 What will eventually happen with chronic? | back 71 vein will eventually open back up & flow again |
front 72 What are the symptoms of chronic DVT? | back 72 echogenic thrombus - more echogenic then acute vein smaller than artery presence of collaterals recannalization constricted vein |
front 73 What us a Baker's cyst? | back 73 Synovial lining and fluid bulge into the popliteal space. May dissect into calf muscles or along intermuscular septums |
front 74 What is another name for a baker's cyst? | back 74 Synovial cyst |
front 75 What should you do to confirm a baker's cyst? | back 75 Rule out calf hematoma by demonstrating communication with joint space |
front 76 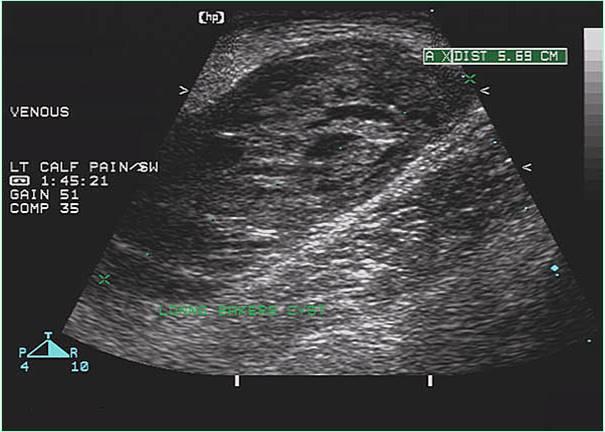 | back 76 no data |
front 77 How do you tell the difference between a Calf hematoma and a baker's cyst? | back 77 absence of joint space communication helps differentiate from Baker’s cyst |
front 78 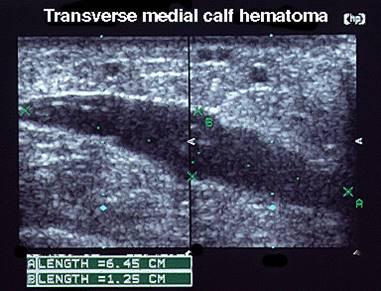 | back 78 Calf hematoma |
front 79 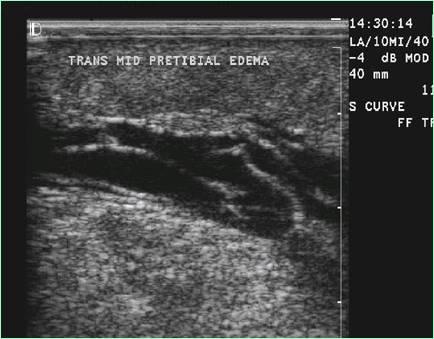 | back 79 Lymphedema |
front 80 What is the sonographic appearance of a Lymphedema? | back 80 “Ant farm” appearance |
front 81 What is Lymphedema? | back 81 Lymphedema refers to swelling that generally occurs in one of your arms or legs. Sometimes both arms or both legs swell. Lymphedema is most commonly caused by the removal of or damage to your lymph nodes as a part of cancer treatment. It results from a blockage in your lymphatic system |
front 82 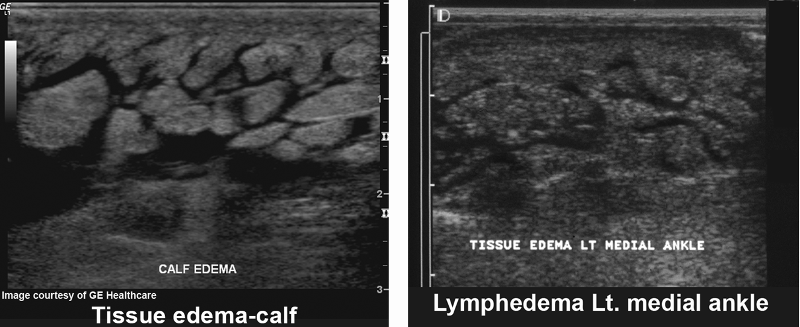 | back 82 Lymphedema |
front 83 Where are Lymph nodes commonly seen? | back 83 Commonly seen in the groin region. |
front 84 When are lymph nodes commonly seen? | back 84 Kidney-shaped and can be swollen in the presence of systemic infection, malignancy, |
front 85 What should be done when lymph nodes are seen? | back 85 Should be measured in three dimensions and reported. |
front 86 What is May Thurner Syndrome? | back 86 May-Thurner syndrome (MTS) is caused when the left iliac vein is compressed by the right iliac artery. |
front 87 Why is May Thurner syndrome dangerous? | back 87 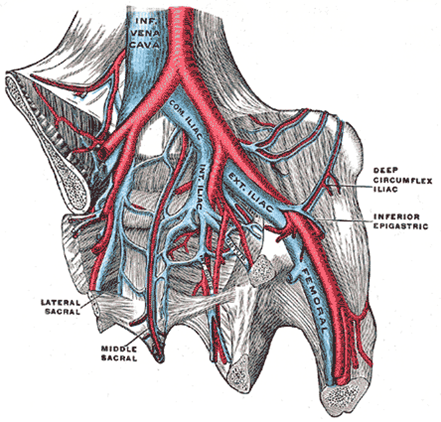 increases the risk of deep vein thrombosis (DVT) in the left extremity |
front 88 VENOUS acute onset SX limb swelling persistent pain calf/thigh local tenderness palpable “cord” chest pain/SOB | back 88 ARTERIAL progressive SX intermittent pain when walking foot/limb coolness limb pallor gangrene, tissue necrosis |
front 89 Venous Insufficiency/ | back 89 Primary Congenital absence or defect of valves Secondary Post- phlebitic: valves damaged by venous thrombosis, and/or chronic outflow obstruction |
front 90 How many valves are there in the IVC? | back 90 0 |
front 91 How many valves are there in the CIV? | back 91 0 |
front 92 How many valves are there in the EIV? | back 92 0 |
front 93 How many valves are there in the FV? | back 93 4 |
front 94 How many valves are there in the Pop? | back 94 2 |
front 95 How many valves are there in the PTV? | back 95 10 |
front 96 How many valves are there in the ATV? | back 96 10 |
front 97 How many valves are there in the ATV? | back 97 10 |
front 98 What are the 3 pump systems in the lower extremities? | back 98 Foot pump Thigh pump Calf veno-motor pump |
front 99 What is the foot pump responsible for? | back 99 primes the calf pump Thigh pump Calf veno-motor pump |
front 100 What is the thigh pump responsible for? | back 100 ejects thigh blood volume |
front 101 What is the Calf veno-motor pump responsible for? | back 101 major ejection Facilitates venous return to heart Reduces the effect of hydrostatic pressure Reduces venous pooling Is dependent on competent valves and muscle contraction |
front 102 What are the veins in the calves? | back 102 PTV’s Peroneals ATV’s Gastrocs Soleal sinuses Greater & Small Saphenous Perferators |
front 103 How does the Veno-motor Pump work? | back 103 Muscle contraction squeezes blood upward, valves prevent return |
front 104 What is the efficiency of the calf veno-motor pump is dependent upon? | back 104 1)The ability of the calf skeletal muscles to contract. 2)The competency of the venous valves. 3)The patency of outflow veins. |
front 105 What can cause perforators? | back 105 Increased deep vein intraluminal pressure may cause perforators |
front 106 What is a perforator? | back 106 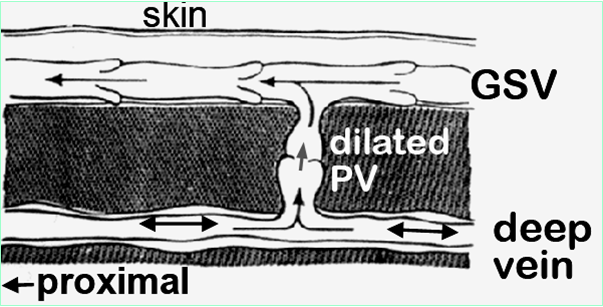 shunt venous blood from Superficial to deep system) to dilate and become incompetent. |
front 107 What are the Venous insufficiency symptoms? | back 107 Recurrent swelling (walking all day) Varicose veins-Spider veins Venous claudication - tired achy legs at end of day Stasis dermatitis - pigment stain from leak Ulceration |
front 108 What is Stasis dermatitis ? | back 108 pigment stain from leak |
front 109 What is Venous claudication? | back 109 tired achy legs at end of day |
front 110 Explain the Flow patterns in upper extremities- central veins | back 110 Cardiac pulsatility is usually apparent and pronounced. Respiratory variation occurs, but flow during inspiration INCREASES, due to changes in thoracic pressure. |
front 111 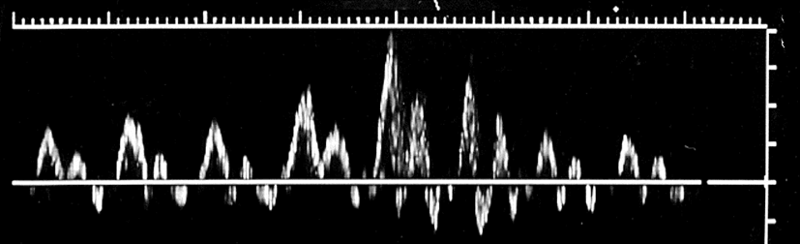 | back 111 subclavian |
front 112 What is the difference between a midline and a Picc catheter? | back 112 midline ends in the subclavian before the cephalic picc ends just outside the heart in the SVC |
front 113 What are the Indications for UE venous duplex? | back 113 Pain and swelling in arm or neck PE Dilated SF veins of the arm or shoulder Palpable cord in arm (SVT) Infusion difficulty with indwelling catheters Pre-op assessment for hemodialysis access placement |
front 114 What are the Deep Veins of the upper extremity? | back 114 SVC Innominate Subclavian Axillary Brachial Radial Ulnar |
front 115 What are the superficial Veins of the upper extremity? | back 115 Basilic Cephalic Median cubital |
front 116 What is the Patient position for evaluation of proximal veins? | back 116 Supine for maximum venous filling |
front 117 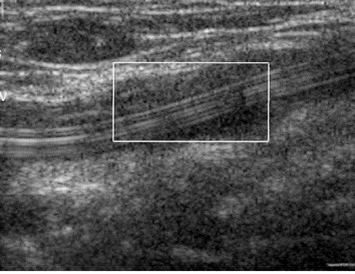 | back 117 no data |
front 118 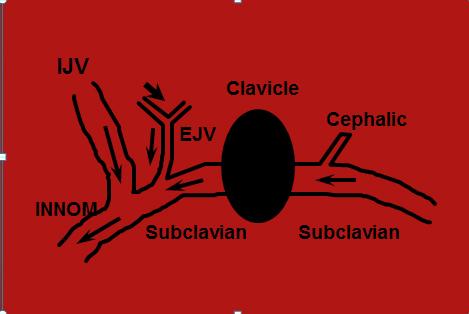 | back 118 no data |
front 119 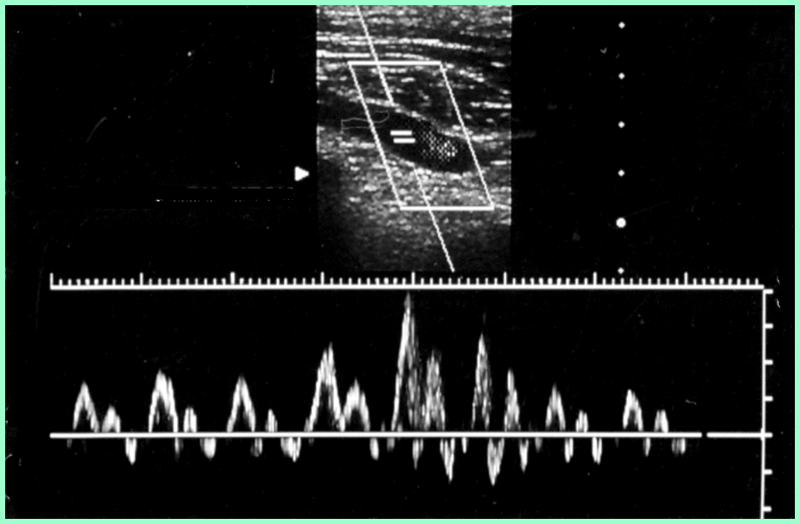 | back 119 Normal upper venous flow |
front 120 What are the normal characteristics of upper venous flow? | back 120 respiratory phasicity cardiac influence |
front 121 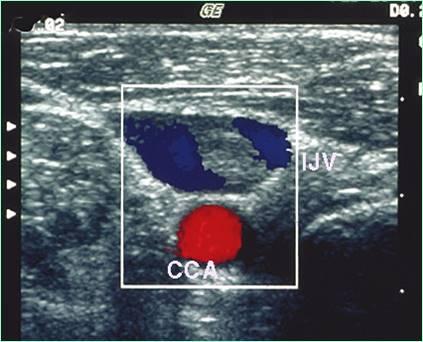 | back 121 no data |
front 122  | back 122 Infraclavicular Subclavian Vein |
front 123 What will alleviate transient axillary vein compression? | back 123 Abduct arm to alleviate transient axillary vein compression |
front 124 Arm veins | back 124 Use compression- release method Pulsatile- phasic flow may be absent Very superficial veins need standoff |
front 125 Assess flow direction in all proximal veins Bilateral comparison of proximal veins for waveform symmetry Waveform assessment priority for prox veins | back 125 no data |
front 126 What is the rule about when an artery bifurcates? | back 126 before venous anastomosis |
front 127 What is important when looking for reflux? | back 127 augmentation |
front 128 If the vein is above the artery, where are you? | back 128 popliteal |
front 129 What does continuous flow in the common femoral vein indicate? | back 129 proximal thrombosis |
front 130 WHat is the easiest vein the identify below the knee? | back 130 posterior tibial |
front 131 How do you find the peroneal veins? | back 131 posterior and deep to the PTV |
front 132 If calf is swollen due to venous instruction what is involved? | back 132 popliteal |
front 133 Where does DVT usually originate in the calf? | back 133 Soleal vein |
front 134 Where is the soleus located? | back 134 small sinus that drains into PTV & Perotoneal |
front 135 What does the gastrocnemius vein drain? | back 135 head of calf drains into popliteal |
front 136 What does poor augmentation indicate? | back 136 obstruction between transducer & augmentation |
front 137 recanalization GSV with residual fibrous band is also called? | back 137 scaring |
front 138 What is sub acute? | back 138 between acute and chronic |
front 139 What is the treatment for a free floating thrombus? | back 139 NO AUGMENTATION!!!!!!!!!!!! heprin/lebenen shot immediately |
front 140 What will lymphedema cause with augmentation? | back 140 difficult augmenatation |
front 141 What is progressive sx? | back 141 cholesterol problems smoking BP issues |
front 142 What causes foot/limb coolness limb pallor gangrene tissue necrosis | back 142 lack of arterial flow |
front 143 The venous system is a ____ pressure system? | back 143 low |
front 144 The rule for valves is | back 144 more distal more valves |
front 145 What will venous obstruction in illiac, femoral or popliteal vein cause | back 145 sweeling & venous swelling |
front 146 Why is dilated perforators a problem? | back 146 when veins stretch valves cannot "touch" and fully shut anymore |
front 147 What is Paget–von Schrötter disease? | back 147 is a form of upper extremity deep vein thrombosis(DVT), in the axillary or subclavian veins. |
front 148 What else is Paget–von Schrötter disease called? | back 148 "effort-induced thrombosis" |
front 149 How many veins and arteries for the brachial, radial & ulnar? | back 149 2 veins 1 artery |
front 150 Where does the basilic dump into? | back 150 axillary or brachial |
front 151 What should be done when there is a thrombus in the basilic vein? | back 151 document how far it is from deep system |
front 152 What is upper extremity exam not as accurate as the lower extremity exam? | back 152 confidence & volume |