Instructions for Side by Side Printing
- Print the notecards
- Fold each page in half along the solid vertical line
- Cut out the notecards by cutting along each horizontal dotted line
- Optional: Glue, tape or staple the ends of each notecard together
NURS 401_Oxygenation & Asthma
front 1 Trachea is shorter; angle of right bronchus at bifurcation is more acute (steeper slope) | back 1 Children |
front 2 What are some A&P differences in the respiratory system or that affect the respiratory system of children? | back 2 Fewer alveoli Less flow between alveoli Lower Hgb Lower SV Higher metabolic rate |
front 3 Average respiratory rate for a newborn | back 3 30-60 |
front 4 Average respiratory rate for infants | back 4 30 |
front 5 Average respiratory rate for preschoolers | back 5 25 |
front 6 Average respiratory rate for school age | back 6 20 |
front 7 Average respiratory rate for adolescents & adults | back 7 12-18 |
front 8 Airway edema, although serious with any age, is especially dangerous with this population r/t level of diameter decrease it causes | back 8 Newborns (small airway of 4mm can decrease to 2mm) |
front 9 Mechanisms that facilitate or impair the body's ability to supply oxygen to cells | back 9 Oxygenation |
front 10 Which of the following individuals would be at greatest risk for pneumonia
| back 10 D. A 72 year old who has the flu |
front 11 A patient is scheduled to have a ventilation/perfusion (V/Q) scan. The nurse knows this is to diagnose:
| back 11 3. Pulmonary embolus |
front 12 When teaching the patient with asthma about the use of the peak flow meter, the nurse instructs the patient to:
| back 12 1. Increase the use of rescue inhalers (albuterol) if the meter indicates the yellow zone |
front 13 You monitor your patient oxygen saturation during exercise and finds that it drops from 94% to 87%. The nurse interprets this data
| back 13 1. The patient requires higher concentration of oxygen during ambulation |
front 14 Your patient has chronic COPD with hypercapnia. Which of the following would be the safest order for oxygen for this patient?
| back 14 3. 28% venturi mask |
front 15 Your patient is diagnosed with tuberculosis. Which of the following is most important in treatment
| back 15 3. Ensure that the patient complete the full course of antibiotic treatment |
front 16 Jennie Dasher is recovering from and aortic valve replacement. Her intial blood gas values come back as: pH 7.5, PCO2 30, HCO3 22, PO2 92. These date support which acid base disturbance?
| back 16 2. Uncompensated respiratory alkalosis |
front 17 Act of inhaling & exhaling air to transport O2 to alveoli | back 17 Respiration |
front 18 ACTUAL exchange of O2 & CO2 (breathing) | back 18 Ventilation |
front 19 A continuous supply of oxygenated blood to every cell in the body (pumped to all parts) | back 19 Perfusion |
front 20 What are the 3 main components that make up the umbrella of oxygenation? | back 20 Ventilation (breathing) Diffusion (gas exchange) Perfusion (pumping to all parts of body) |
front 21 This age group is known for being obligated nose breathers | back 21 Newborns |
front 22 Inadequate supply of O2 in the blood | back 22 Hypoxemia |
front 23 What are some late S/S of hypoxemia? | back 23 Combative/coma Dyspnea @ rest Cyanosis Cool, clammy skin Low BP/HR |
front 24 What are some early S/S of hypoxemia? | back 24 Irritability/restlessness Tachypnea/dyspnea High BP/HR |
front 25 What are some red flags r/t hypoxemia? | back 25 Change in mentation: LOC Orientation Irritability Confusion Lethargy |
front 26 What other problems may result in S/S similar to SNS response to hypoxemia? *Would require us to distinguish between whether or not it's hypoxemia | back 26 SNS response to: Pain Fear Sepsis |
front 27 Alphabet soup r/t oxygenation: C = ? | back 27 Concentration |
front 28 Alphabet soup r/t oxygenation: F = ? | back 28 Fractional concentration |
front 29 Alphabet soup r/t oxygenation: E = ? | back 29 Expired |
front 30 Alphabet soup r/t oxygenation: I = ? | back 30 Inspired |
front 31 Alphabet soup r/t oxygenation: P = ? | back 31 Partial pressure |
front 32 Alphabet soup r/t oxygenation: Q = ? | back 32 Volume of blood |
front 33 Alphabet soup r/t oxygenation: S = ? | back 33 Saturation |
front 34 Alphabet soup r/t oxygenation: V = ? | back 34 Volume of gas |
front 35 Alphabet soup r/t oxygenation: a = ? | back 35 arterial |
front 36 Alphabet soup r/t oxygenation: c = ? | back 36 capillary |
front 37 Alphabet soup r/t oxygenation: v = ? | back 37 venous |
front 38 Alphabet soup r/t oxygenation: p = ? | back 38 pulse oximetry |
front 39 Alphabet soup r/t oxygenation: A = ? | back 39 Alveolar |
front 40 This is a measure of the hydrogen ion concentration | back 40 pH |
front 41 Alphabet soup r/t oxygenation: pCO2 = ? | back 41 Partial pressure of CO2 |
front 42 Alphabet soup r/t oxygenation: pO2 = ? | back 42 Partial pressure of O2 |
front 43 Alphabet soup r/t oxygenation: SO2 = ? | back 43 Saturation of O2 |
front 44 Alphabet soup r/t oxygenation: HCO3 = ? | back 44 Bicarbonate |
front 45 "Gold standard" for measuring oxygenation | back 45 ABG |
front 46 If performing a radial ABG, which side should you stick? | back 46 Non-dominant hand |
front 47 What type of patient would we not want to perform a brachial stick to obtain an ABG? | back 47 Obese (difficult to assess for hemostasis) |
front 48 Where would you obtain an ABG on a newborn? | back 48 Umbilical artery line |
front 49 ABG: Normal PaO2 | back 49 80-100 |
front 50 ABG: Normal SaO2 | back 50 95-100% |
front 51 ABG: Normal CO2 | back 51 35-45 |
front 52 ABG: Normal HCO3 | back 52 22-26 |
front 53 ABG: Normal Base Excess (BE) | back 53 -2.0 to 2.0 mEq/L |
front 54 Hgb is almost fully saturated at this pO2 | back 54 80-100 mm Hg |
front 55 Hg saturation with O2 is high in the __1__ and is greatest in the __2__ | back 55 1. Tissues 2. Lungs |
front 56 If Hg experiences an increased affinity for O2, these manifestations will ensue | back 56 Lower temp Lower pCO2 Lower 2, 3-DPG Increased pH |
front 57 The ease with which hemoglobin releases oxygen to the tissues is controlled by this | back 57 2, 3-DPG |
front 58 If Hg experiences a decreased affinity for O2, these manifestations will ensue | back 58 Increased temp Increased pCO2 Increased 2, 3-DPG Lower pH |
front 59 In what different situations can PaO2 & SaO2 not be consistent? | back 59 SpO2 <70% Hg abnormality Movement/exercise Vasoconstriction (low perfusion) Skin color Intravascular/intradermal dyes Bright fluorescent lights Anemia |
front 60 Hg & O2: __1__ is the maximum amt. of O2 that can be combined with Hg, whereas __2__ is the actual amount of O2 being carried by Hg | back 60 1. Capacity 2. Saturation |
front 61 How does O2 blood saturation affect Hg saturation? | back 61 If Hg isn't fully saturated, a high O2 blood content will result in high Hg If Hg is highly saturated, a low O2 blood content will result in low Hg |
front 62 Classical cyanosis is present when 5 g/dL of __1__ or greater is present, and is usually apparent when SaO2 is less than or equal to __2__ | back 62 1. Deoxyhemoglobin 2. 85% |
front 63 This sign is not a good indicator of oxygenation | back 63 Cyanosis |
front 64 These 3 systems regulate acid-base balance | back 64 Buffer system (metabolic) Kidneys (metabolic) Lungs (respiratory) |
front 65 This counteracts changes to pH due to ability to either absorb or release H+ ions First line of defense vs. pH changes | back 65 Buffer system |
front 66 3 main buffers of the buffer system of pH maintenance include: | back 66 HCO3 Phosphate Protein |
front 67 Can directly affect acid-base balance status more quickly & efficiently than all the buffer systems combined | back 67 Respiratory system |
front 68 Can activate pH changes within 1-3 minutes | back 68 Respiratory system |
front 69 Slower process; requires 1-5 days for complete activation to correct acid-base imbalances | back 69 Kidneys |
front 70 How do kidneys react to changes in pH? | back 70 Regulate excretion or conservation of H+ & HCO3 |
front 71 How soon are pH buffer systems operational? | back 71 In utero *Renal system limited in newborns |
front 72 Do newborns have the ability to control pH using their respiratory system? | back 72 Yes, so long as pulmonary function is adequate |
front 73 The renal buffer system is limited in its capacity to respond to pH changes in this age group | back 73 Newborns |
front 74 pH <7.35 pCO2 >45mm Hg | back 74 Respiratory acidosis |
front 75 pH <7.35 HCO3 <22mm Hg | back 75 Metabolic acidosis |
front 76 The body has accumulated too much acid & doesn't have enough HCO3 to neutralize its effects | back 76 Metabolic acidosis |
front 77 This acid-base imbalance is often r/t hyperventilation | back 77 Respiratory alkalosis |
front 78 pH >7.45 pCO2 <35mm Hg | back 78 Respiratory alkalosis |
front 79 pH >7.45 HCO3 >26mm Hg | back 79 Metabolic alkalosis |
front 80 pH is abnormal pCO2 & HCO3 abnormal | back 80 Partial compensation |
front 81 pH is normal pCO2 & HCO3 abnormal | back 81 Full compensation |
front 82 At what age will most children first have respiratory symptoms indicative of asthma? | back 82 <4 years |
front 83 What is one of the first signs that a person is having airway restriction indicative of asthma? | back 83 Cough *Wheezing is a medium-late sign of asthma |
front 84 What's the most common trigger for children's asthma attacks? | back 84 Viruses |
front 85 These factors often predispose children to having asthma later in life | back 85 Parental asthma Eczema/atopy |
front 86 Asthma is an INFLAMMATORY disease with these 3 characteristics | back 86 Edema Excess mucus production Bronchospasm |
front 87 Can mild asthma have a severe exacerbation? | back 87 Yes |
front 88 This doesn't disappear along with the symptoms of asthma following treatment | back 88 Airway inflammation (chronically present regardless of symptoms) |
front 89 In a large number of children, asthma remits at this point in life | back 89 Early adolescence/adulthood |
front 90 This medication is both a bronchodilator & anticholinergic used to treat asthma; thus, you're treating inflammation via both sympathetic & parasympathetic routes | back 90 Atrovent (ipratropium bromide) |
front 91 Incidence of asthma is greater in boys up until this point in life; after this point, it's more prevalent in girls | back 91 Until puberty |
front 92 What are the 2 major groups of medications used to TX asthma? | back 92 Rescue & controller medications |
front 93 Types of rescue medications for asthma | back 93 Beta 2's (albuterol, atrovent) Oral steroids Anticholinergics (atrovent) |
front 94 Types of controller medications for asthma | back 94 Inhaled corticosteroids Anti-leukotrienes (Montelukast) Long-active beta 2's Combo inhaled & long-acting (Advair, Symbicort) |
front 95 What objective information is needed for asthma treatment? | back 95 Peak flow meters Spirometry for child >5 yrs (or infant spirometry) Exhaled nitric oxide measurement (normal eNO = 5-15 ppb) Allergy testing |
front 96 This helps w/diagnosis & ongoing TX decisions r/t asthma Provides objective data for management Measures obstruction to airflow in airways | back 96 Spirometry |
front 97 Early phase of acute asthma exacerbation: 1. What causes symptoms? 2. What is the treatment? | back 97 1. Bronchoconstriction & inflammation 2. Beta 2 agonist (i.e. bronchodilator) |
front 98 Late phase of acute asthma exacerbation: 1. What is happening to respiratory A&P? 2. What is the treatment? | back 98 1. Bronchial hyperresponsiveness 2. Bronchodilator & antiinflammatory medications |
front 99 Early warning signs of asthma | back 99 Cough, throat clearing Chest tightness SOB EXPIRATORY wheezing |
front 100 Late warning signs of asthma | back 100 Cough, vomit Stop to breathe when walking Trouble walking normal distances Accessory muscle use INSPIRATORY & EXPIRATORY wheezing |
front 101 What does giving a daily inhaled mcg dose of corticosteroid controller medication prevent? | back 101 Having to take an oral milligram dose of corticosteroid medication |
front 102 What are some worrisome signs during an acute asthma exacerbation? | back 102 Climbing pCO2 (35-45) No wheezing is ominous Unable to say more than a few words Confusion Don't care what's happening around them (just care about oxygen) |
front 103 Asthma guidelines address these 3 different age ranges | back 103 0-4 5-11 >12 |
front 104 How many puffs are in a normal dose of your rescue inhaler? | back 104 4 |
front 105 Analyze asthma severity chart on reverse side | back 105 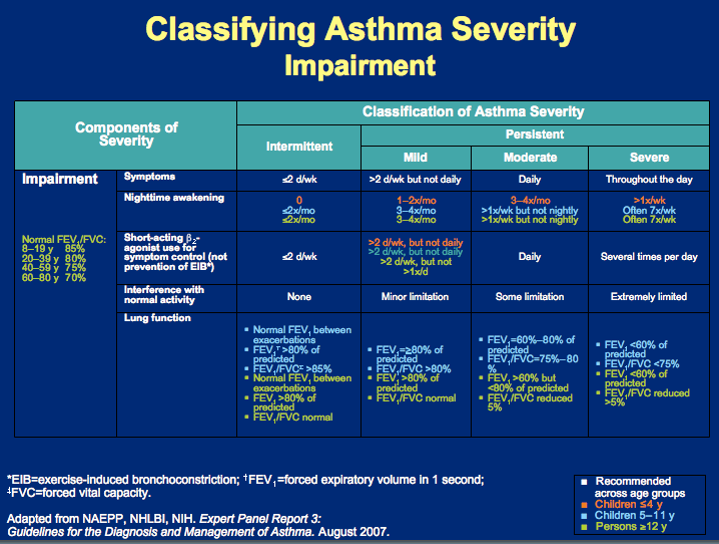 |
front 106 Along with rescue meds, this will most likely be added to the TX plan of a mild asthmatic | back 106 Low-dose ICS |
front 107 Along with rescue meds, this will most likely be added to the TX plan of a moderate asthmatic | back 107 Medium-dose ICS |
front 108 Along with rescue meds, this will most likely be added to the TX plan of a severe asthmatic | back 108 High-dose ICS + LABA or montelukast; potentially oral systemic corticosteroids depending on severity |
front 109 What's the "Rule of 2's", as proposed by Baylor University? | back 109 Does your child use albuterol > 2x/week? Does your child have symptoms @ night > 2x/month? Do you refill your rescue med > 2x/year? Peak flow < 20% from personal best blow? |
front 110 What happens if there's a "yes" answer to any of the questions in the "Rule of 2's" from Baylor University? | back 110 Indicates asthma isn't under control Chronic inflammation requiring a controller med Indicates child has reached level of PERSISTENT asthma |
front 111 The always-present inflammatory cells in the asthmatic's airway result in hyper-__1__ & hyper-__2__ airways that, when hit with a __3__, become further inflamed & edematous, increasing __4__ production & constricting of smooth muscle | back 111 1. Reactive 2. Sensitized 3. Trigger 4. Mucus |
front 112 What's the ultimate goal of asthma treatment? | back 112 Prevention of exacerbations (which will prevent airway remodeling) |
front 113 With a child of this age, they may help with minimal task, such as holding equipment | back 113 <2 yrs |
front 114 With a child of this age, they may be able to get some equipment, ID some body parts involved in asthma, & help with TX | back 114 2-4 yrs |
front 115 With a child of this age, parents are still responsible for care, but the child can learn early warning signs, triggers, and correct words to label body parts & symptoms | back 115 4-6 yrs |
front 116 With a child of this age, parents are still needed, but child is starting to take more active care role; can set up equipment, recite meds & info, and link cause & effect | back 116 6-9 yrs |
front 117 During normal, asymptomatic days, the asthmatic will take a/an __1__ (green zone); when entering the caution zone (yellow), where symptoms develop, the asthmatic will add a/an __2__; when symptoms are severe (red zone - danger), a/an __3__ will be added | back 117 1. Low-dose ICS 2. Rescue inhaler (albuterol) 3. Oral steroid |
front 118 The nurse reviews an arterial blood gas report for a client with chronic obstructive pulmonary disease (COPD). The results are: pH 7.25; PCO2 62; PO2 70; HCO3 34. The nurse should first:
| back 118 B: Clients with chronic COPD have CO2 retention and the respiratory drive is stimulated when the PO2 decreases. The heart rate, respiratory rate, and the blood pressure should be evaluated to determine if the client is hemodynamically stable. Symptoms, such as dyspnea, should also be assessed. Oxygen supplementation, if indicated, should be titrated upward in small increments. There is no indication that the client is experiencing respiratory distress requiring intubation. |
front 119 A client’s arterial blood gas values are as follows: pH 7.31; PaO2 80 mmHg; PaCO2 65 mmHg; HCO3 36 mEq/L. The nurse should assess the client for:
| back 119 B: The high PaCO2 level causes flushing due to vasodilation. The client also becomes drowsy and lethargic because carbon dioxide has a depressant effect on the central nervous system. Cyanosis is a sign of hypoxia. Irritability and anxiety are not common with a PaCO2 level of 65 mmHg but are associated with hypoxemia. |