front 5 Inflammation
suffix: -itis | back 5 - a sequence of events intended to limit the effects of injury or
a dangerous agent in the body
- is intended to localize and
remove an injurious agent
- the general signs and symptoms
serve as a warning of a problem which may be hidden within the
body
- non specific response
- results in redness,
swelling, warmth, and pain
|
| back 6 - nonspecific agents
- protect uninfected cells against
viruses
|
| back 7 - specific defense
- provides protection by stimulating
the production of specific antibodies and sensitized
lymphocytes
|
front 8 Normal Capillary Exchange | back 8 - usually not all capillaries in a particular capillary bed are
open
- unless the cells' metabolic needs are not being
met by the blood supply to the area
- or an
accumulation of wastes occurs
|
front 9 Arterial End of Capillary | back 9 - movement of fluid, electrolytes, oxygen, and nutrients
- based on net hydrostatic pressure (pushes things
out)
|
| back 10 - hydrostatic pressure is decreased
- osmotic pressure
(pulls things in)- relatively high
- b/c plasma proteins
remain within the vessels
|
| back 11 - acts as an anti-inflammatory by decreasing capillary
permeability
|
| back 12 - direct physical damage
- caustic chemicals
- such as: acids or drain
cleaner
- ischemia or infarction
- local
deficiency of blood
- allergic reactions
- extremes of heat and cold
- foreign bodies
- infection
|
| back 13 - An injury to capillaries and tissue cells will result in the
following reactions:
- Bradykinin is released from injured
cells
- Bradykinin activates pain receptors
- Sensation of pain stimulates mast cells and basophils to
release histamine
- Bradykinin and Histamine cause
capillary dilation
- results in an increase in blood flow
and increased capillary permeability
- Break in skin allows bacteria to enter the tissue
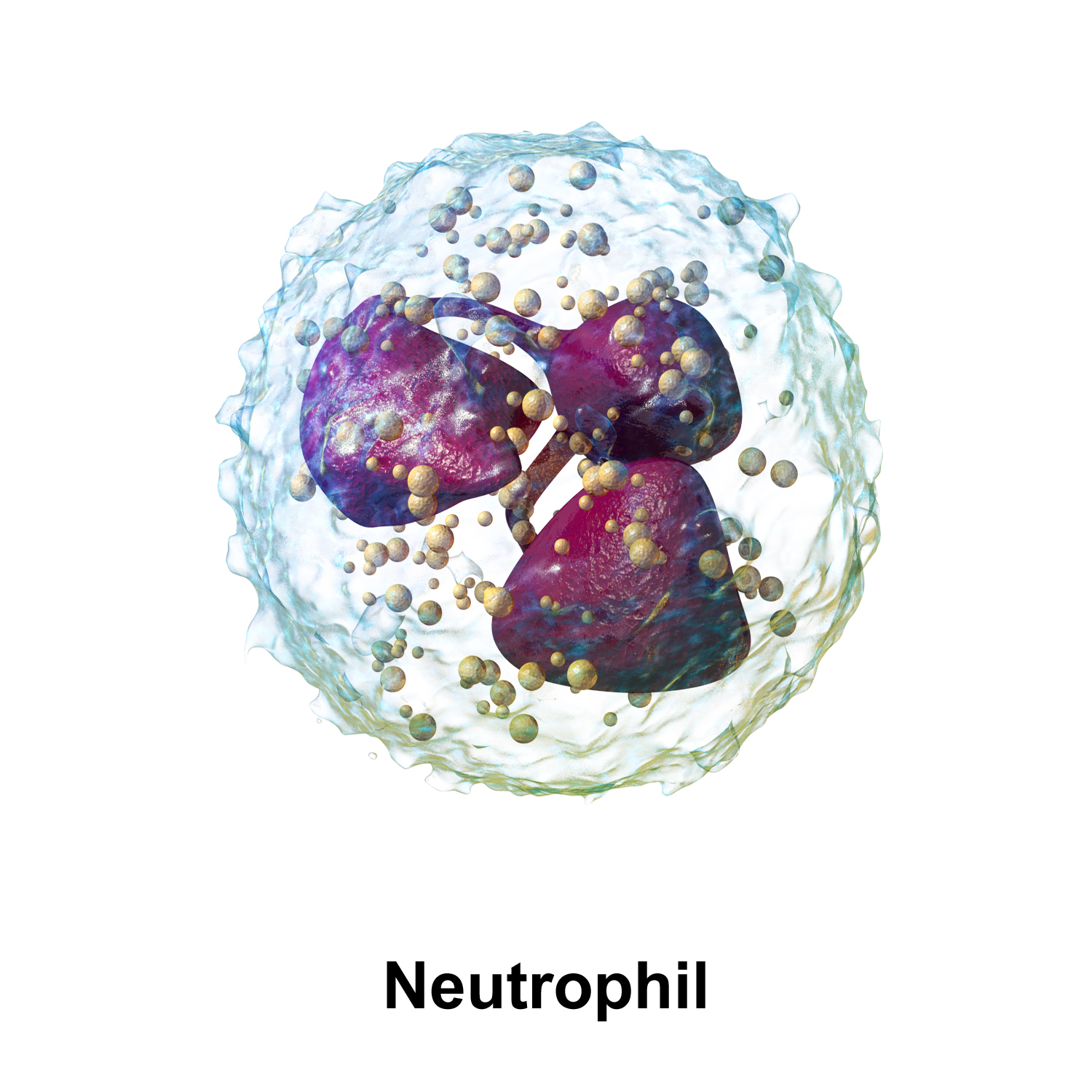
- results in migration of neutrophils and monocytes to the
site of injury
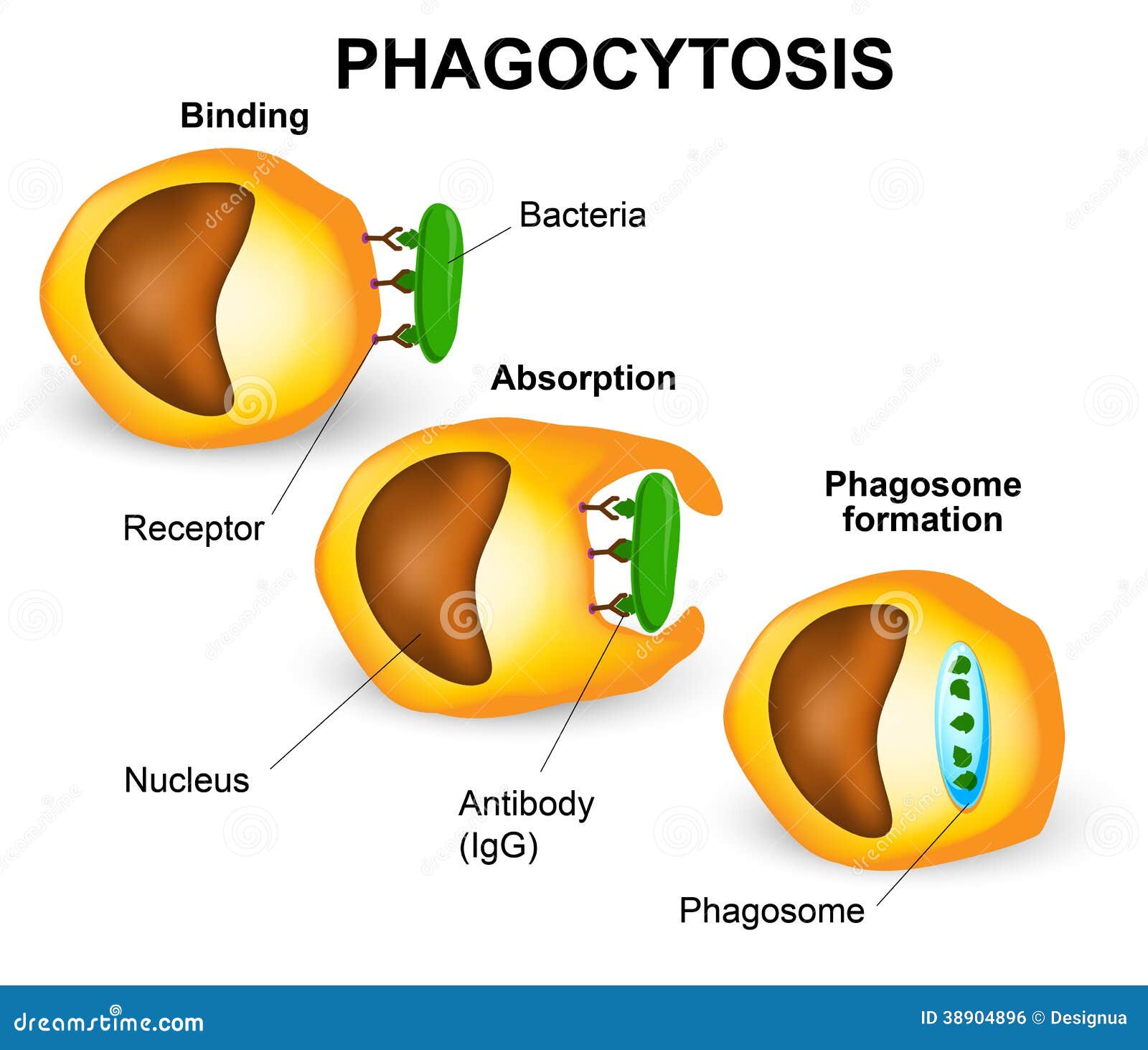
- Neutrophils phagocytize
bacteria
- Macrophages (mature monocytes) leave the
bloodstream and phagocytose microbes
|
| back 14 - When tissue injury occurs, the damaged mast cells and platelets
release chemical mediators into the interstitial fluid and
blood.
- examples of chemical mediators:
- histamine
- serotonin
- prostaglandins
- leukotrienes
- Chemical mediators affect
blood vessels and nerves in the damaged area
-
Cytokines
- serve as communication in the
tissue fluids sending messages to induce fever
|
| back 15 - released immediately from granules in mast cells and exert
their effects at once
- immediate vasodilation and increase
capillary permeability to form exudate
|
| back 16 - synthesized from arachidonic acid in mast cells
- responsible for the later effects
- prolongs
inflammation
- vasodilation
- increased capillary
permeability
- chemotaxis
|
| back 17 - increased blood flow to a particular area
|
front 18 Increase in Capillary Permeability | back 18 - allows plasma proteins to move into interstitial space along
with fluid.
- Increased fluid dilutes any toxic material,
while globulins serve as antibodies, and fibrinogen forms fibrin
mesh around the area to localize the injurious agent
|
| back 19 - attract cells of the immune system
- first Neutrophils
and later monocytes and macrophages
|
| back 20 - relaxation of smooth muscles causing an increase in the
diameter of arterioles
|
| back 21 - release of histamine, leading to inflammation
|
| back 22 - numbers are increased in allergic responses
|
| back 23 - active in cell-mediated immune response
|
| |
| |
| back 26 - active in phagocytosis
- mature monocytes that have
migrated into tissues from the blood
|
| back 27 - The movement or passage of blood cells, especially white blood
cells, through intact capillary walls into surrounding body
tissue.
|
front 28 Redness and Warmth
(inflammation symptom) | back 28 - caused by increased blood flow into the damaged area
|
front 29 Swelling or Edema
(inflammation symptom) | back 29 - caused by the shift of protein and fluid into the interstitial
space
|
front 30 Pain
(inflammation symptom) | back 30 - results from increased pressure of fluids on the nerves;
release of chemical mediators (ex: Bradykinin &
prostaglandins)
|
front 31 Loss of Function
(inflammation symptom) | back 31 - may develop if cells lack nutrients
- edema may
interfere with movement
|
| back 32 - a collection of interstitial fluid formed in an inflamed
area
|
| back 33 -
watery
- consists primarily of:
- fluid
- some proteins
- and some white blood
cells
-
occurs with allergic reactions and burns
|
| back 34 - thick and sticky
- high cell and fibrin content
- increases the risk of scar tissue in the area
|
| back 35 - thick, yellow-green
-
contains more leukocytes, cell debris, and
microorganisms
- indicates bacterial infection
-
aka "pus"
|
| back 36 - localized pocket of purulent exudate in a solid tissue
|
front 37 Other General Manifestations of Inflammation | back 37 - mild fever (pyrexia)
- if inflammation is extensive
- malaise
- fatigue
- headache
- anorexia
|
| back 38 - fever-producing substances
- circulate in the blood and
cause the body temperature control system in the hypothalamus to be
reset at a higher level
|
| back 39 - increased white blood cells in the blood
- especially
neutrophils
|
| back 40 - the proportion of each type of WBC
- may be helpful in
distinguishing viral from bacterial infection
|
| back 41 - may be elevated in the blood in the presence of severe
inflammation and necrosis
- helpful in locating the site of
necrotic cells
|
| |
| back 43 - infection may develop in an inflamed tissue b/c microorganisms
can more easily penetrate when the skin is damaged and blood supply
is impaired
- some microbes resist phagocytosis
- inflammatory exudate provides an excellent medium for
microorganisms to reproduce and colonize the inflamed area
|
| back 44 - may develop following an acute inflammation, when causative
agent is not completely eradicated
|
front 45 Characteristics of Chronic Inflammation | back 45 - less swelling and exudate
- presence of more
lymphocytes, macrophages, and fibroblasts than acute inflam
- more tissue destruction occurs
- more collagen is
produced resulting in more fibrous scar tissue
|
| back 46 - small mass of cells with a necrotic center covered by
connective tissue
- may develop around foreign objects such
as splinter
|
front 47 Acetylsalicylic Acid (ASA) | back 47 - an anti-inflammatory agent
- decrease prostaglandin
synthesis, reducing the inflammatory response
- decrease pain
and fever
- DO NOT GIVE TO CHILDREN WITH VIRAL INFECTIONS DUE
TO RISK OF LEADING TO REYES SYNDROME
- aspirin
|
| back 48 - decreases fever and pain
- does not diminish the
inflammatory response
- TYLENOL or PARACETAMOL
|
front 49 Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) | back 49 - has anti-inflammatory, analgesic, antipyretic activities
- act by reducing production of prostaglandins
- used to
treat inflammation in musculoskeletal system
|
front 50 Anti-Inflammatory Effects of Glucocorticoids | back 50 - act as an anti-inflammatory by decreasing capillary
permeability
- enhance effectiveness of epinephrine and
norepinephrine
- reduced number of leukocytes and mast cells,
decreasing the release of histamine and prostaglandins
- reduces immune response
|
front 51 RICE Therapy for Injuries | back 51 -
Rest
-
Ice
- cold causes vasoconstriction,
decreasing edema and pain
-
Compression
- reduces the accumulation of
fluid
-
Elevation
- improve fluid flow away from
damaged area
|
| back 52 - the process that occurs when there is minimal tissue
damage
- the damage cells recover and tissue returns
to normal within a short period
- ex: sunburn
|
| back 53 - the healing process that occurs in damaged tissue in which the
cells are capable of mitosis
- the damaged tissue is replaced
by identical tissue from the proliferation of nearby cells
|
| back 54 - takes place when there is extensive tissue damage
- cells are incapable or mitosis
- functional tissue
replaced by scar tissue
- loss of function
|
| back 55 - the process of tissue repair begins following injury when a
blood clot forms and seals the area
- after 3 to 4 days
foreign material and cell debris has been removed granulation tissue
grows into the gap
|
front 56 Complication due to Scar Formation | back 56 - loss of function
- results from the loss of normal cells
and lack of specialized structures or normal organization in
scar tissue
- ex: hair follicles, nerves, receptors
|
front 57 Contractures and Obstructions | back 57 - scar tissue is nonelastic
- shrinks over time
- contracture
- An abnormal, often
permanent shortening, as of muscle or scar tissue, that results
in distortion or deformity, especially of a joint of the
body
|
| back 58 - bands of scar tissue joining two surfaces that are normally
separated
|
| back 59 - overgrowth of fibrous tissue
- leads to hard ridges of
scar tissue or keloid formation
|
| back 60 - blood supply may be impaired around scar
- results in
further tissue breakdown and ulceration at future time
|
| back 61 - a thermal (heat) or nonthermal (electrical or chemical) injury
to the body, causing acute inflammation and tissue destruction
- may be mild or severe
- classified by the depth of skin
damage and the percentage of body surface area involved
|
front 62 Superficial Partial-Thickness Burns (First Degree) | back 62 - involves epidermis and may involve upper part of dermis
- little, if any, blister formation
- usually appears red
and painful but readily healed without scar tissue
|
front 63 Deep Partial-Thickness Burn (second degree) | back 63 - involve the destruction of the epidermis and part of the
dermis
- area is red, edematous, blistered, and often
hypersensitive
- easily infected
|
front 64 Full Thickness Burns (third and fourth degree) | back 64 - destruction of all skin layers and underlying tissues
- burn area may be painless b/c of destruction of the nerves
|
| back 65 - both local and systemic
- shock
- dehydration and
edema
- respiratory problems
- pain
- infection
|
| back 66 - the percentage of RBCs in a volume of blood
|