Instructions for Side by Side Printing
- Print the notecards
- Fold each page in half along the solid vertical line
- Cut out the notecards by cutting along each horizontal dotted line
- Optional: Glue, tape or staple the ends of each notecard together
Molecular Toxicology Exam 2 Review
front 1 What is oxidative stress | back 1 Imbalance of pro-oxidizing compounds and antioxidants pivotal mechanism for many xenobiotics |
front 2 What are the two mechanisms for which oxidative stress occur | back 2 1) Increased ROS ---> oxidative stress 2) Depletion of antioxidant pool ---> oxidative stress |
front 3 How is molecular oxygen reduced (draw the stepwise mechanism) Label what antioxidant works on what | back 3 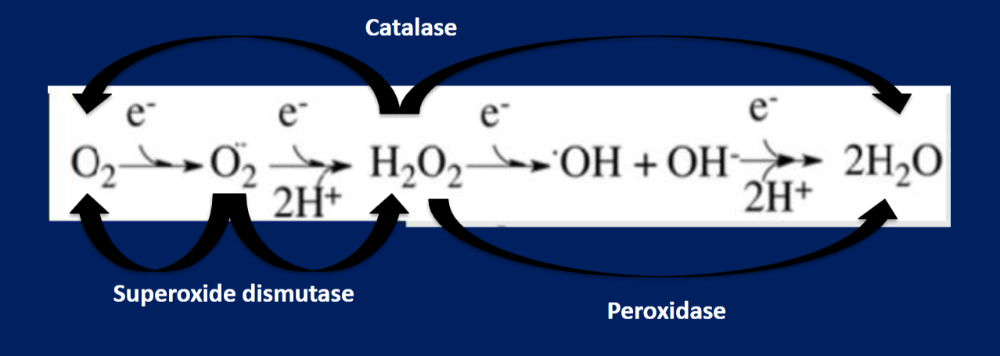 |
front 4 How much ROS usually escapes the mitochondria | back 4 Usually less than 1% |
front 5 What do toxins do regarding oxidative stress? | back 5 Increase ROS or decrease antioxidant pool |
front 6 What produces extracellular ROS and give an example | back 6 Generated by phagocytes or lymphocytes Example: NADPH oxidase - dormant, membrane bound protein which is activated by surface cell receptors and can produce ROS |
front 7 What are 4 important things antioxidants do | back 7 1) Provide alternative substrate for ROS: gives it something else to bind to - Most antioxidants have a lot of thiol groups (sulfur groups) to bind ROS 2) Keep cellular thiol in its reduced form (not oxidized) 3) Prevent/repair oxidation of cellular components 4) Sequester redox active metals - Metallothionine: has lots of sulfurs to neutralize ROS with binding |
front 8 Are antioxidants enzymatic or non-enzymatic? | back 8 They can be either |
front 9 How does antioxidant potential work (give an example comparison) | back 9 It differs between organs ex: Liver/kidney have high antioxidant potential since they the natural detoxifiers of the body. They are the first to be exposed to xenobiotics and poisons unlike your CNS/cardiac which has a low antioxidant potential |
front 10 Answer these next few questions: What antioxidants act on hydrogen peroxide? What antioxidant acts on the superoxide radical? What antioxidant acts on the hydroxyl radical? | back 10 1) Catalase and peroxidase 2) Superoxide dismutase (SoD) 3) it doesn't have one; it is scavenged by endogenous compounds to be bound up and excreted |
front 11 Define superoxide dismutase | back 11 - SoD -Enzymatic - most important antioxidant mutant - |
front 12 What three genes code for superoxide dismutase? | back 12 SoD1 = cytosolic SoD2 = mitochondrial Sod3 = extracellular |
front 13 What makes SoD critical? | back 13 Every aerobic organism processes SoD Mutations of SoD linked to lou gehrigs disease |
front 14 Where is catalase found | back 14 Peroxisomes |
front 15 Where is gultathion peroxidase found | back 15 cytosol |
front 16 Name off what you know about Glutathione (GSH) | back 16 tripeptide of glutamide, cystine, and glycine by itself it is the most important non-enzymatic antioxidant it has a large number of cystines GSH is found in mM concentration in many tissues Has three pools within cells: Nuclear, mitochondrial, and cystolic |
front 17 What are glutathione's two mechanisms? | back 17 1) Non-enzymatic scavenging where GSH turns into GSSH 2) Enzymatic where thiol reductase reduces disulfide bonds in oxidized proteins and glutathione peroxidase is found |
front 18 What are the major ways glutathione pools are depleted and give one example of an effect | back 18 1) chronic exposure to pro-oxidants 2) Depletion of a necessary source like nutrition ie. fasting/dieting (toxicity may occur due to low glutathione ex. GGPD Deficency: most common pharmacogenic polymorphism |
front 19 What happens with moderate increases of intracellular Ca | back 19 Activates Ca dependent caspases (low concentration of xenobiotics) |
front 20 What happens with high increases of intracellular Ca | back 20 Release from intracellular Ca stores |
front 21 4 important things that are affected by high Ca and what happens? | back 21 1) Proteases and Calpain activation - Activity is regulated by Ca concen. + calpain inhibitor - Can facilitate apoptosis by assisting caspases 2) Endonucleases - Role is to cleave DNA - Result in single/double bond breaks resulting in apoptosis - ie. acetominophen 3) Lipases and membranes - Phospholipase A2 is activated which causes Arachidonic Acid production - AA activates mpt which causes a large pore to form in the mitochondria 4) Mitochondria -3 important parts are Ca transport pumps, proton gradient, and ATP production -CC in mitochondria can move out into extracellular space after pore is produced facilitating fast apoptosis already occuring |
front 22 What is cell death caused by | back 22 oxidative stress, covalent binding, or mitochondrial injury |
front 23 how is necrosis v apoptosis determined | back 23 extent of cellular damage or cellular energy status |
front 24 Necrosis information | back 24 -cells swell to rupture - cells lose ability to osmoregulate |
front 25 5 steps of necrosis activation | back 25 1) oxi stress, mito damage, or Ca influx 2) Changes in plasma membrane permeability (loss of ion control) 3) cytoskeleton breaks down 4) ATP is depleted (pumps break, loses ability to maintain things like Na, Ca) 5) swelling and burst |
front 26 Progression of necrosis | back 26 - propagation across cells - does not require toxin to be present anymore - spilled cellular contents cause ROS to be produced in extracellular space where Ca is very present, causes dormant lipases and proteases to be activated affecting neighboring cells |
front 27 Apoptosis information | back 27 - cells packaged for disposal - cell membrane does no lyse |
front 28 Steps of apoptosis | back 28 1) initiating event ( cell signaling event etc) 2) Activation of caspases (one caspase is an amplifier used to activate the rest of the caspases which break down cellular components) 3)DNA condenses and is cleaved into 180bp fragments (nucleus is very apparent, activated by nucleases) 4)More caspases break down cell proteins (leads to rapid collapse in cell functionality) 5) Cell body shrinks and produces apoptotic bodies 6) apop bodies are phagocytized by macrophages until the cell is gone |
front 29 What are death receptors and their three domains (draw death receptor) | back 29 large group of cell membrane receptors that activate apoptosis 3 domains - extracellular domain ( cystine rich (sulfurs)) - membrane signalling domain -Intracellular death sequence domain |
front 30 How do death receptors work? give an example | back 30 - DR's trimerize through cellular interactions - trimerized complex can bind with specific DR's to activate - Recruitment of accessory proteins results in disc formation - DISC activates caspases Ex. FAS: DR typically stored intracellularly normally binds to fasL for activation, can bind to itself to initiate apoptosis |
front 31 What is cytochrome C | back 31 - very large molecule found inside mitochondrial membrane, has to be transported out of the mitochondria - can directly activate apoptotic caspases - apoptotic signaling proteins or oxidative damage can open pore and allow cyt C out into cytosol |
front 32 What are the regulators of Cytochrome C | back 32 Bcl-2: produced as an anti-apoptotic factors, forms dimers and prevents mpt from opening BAX protein: upregulated by DR's, causes mpt pore opening and release of cyt-c Bid: Activated by caspases to form tbid and migrates to nucleus, increases ROS production in mitochondria, damages cell membrane, promotes cyt-c leakage |
front 33 What is mitogenesis | back 33 Repairing of lost cells for low-level apoptosis |
front 34 What is cell proliferation | back 34 increased mitotic activity in response to toxic insult; used to restore tissue to normal mass and function Toxins can inhibit or promote this process leading to no cell regeneration or tumor growth |
front 35 what is a direct mitogen | back 35 Compounds that directly push cells into mitotic cycle w/out previous damage leads to tumor growth ex.lead: Pb2+ activates Ca2+ sensitive proteins and pkc phosphorylates proteins which induce DNA synthesis |
front 36 What is an antimitogen and give an example | back 36 Inhibit cell cycle progression and blocks mitosis Taxol: anticancer drug that effects formation of mitotic spindle apparatus - it does not allow the spindle to disassemble , preventing mitosis and eventually causing apoptosis |