Human A&P exam 2
Introduction
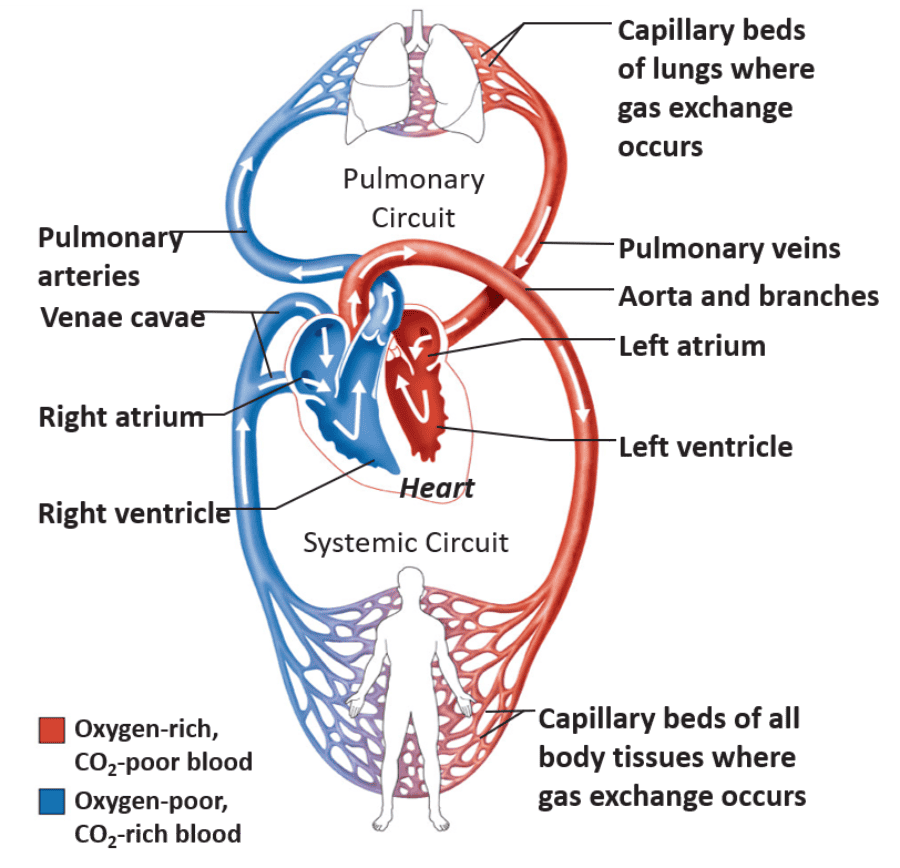
- The heart – a muscular double pump with two circuits:
–Pulmonary circuit— takes blood to and from the lungs
–Systemic circuit—vessels transport blood to and from body tissues
- Atria (‘entranceway’)— receive blood from the pulmonary and systemic circuits
- ventricles (‘hollow belly’)—the pumping chambers pumps blood around the two circuits
The Heart...
- Heart pumps blood through 120,000 km (75,000 miles) of blood vessels (BVs)
–Beats 100,000 times/day or 35 million times/year
–Pumps 5 liters of blood/minute
Pulmonary and Systemic Circuits
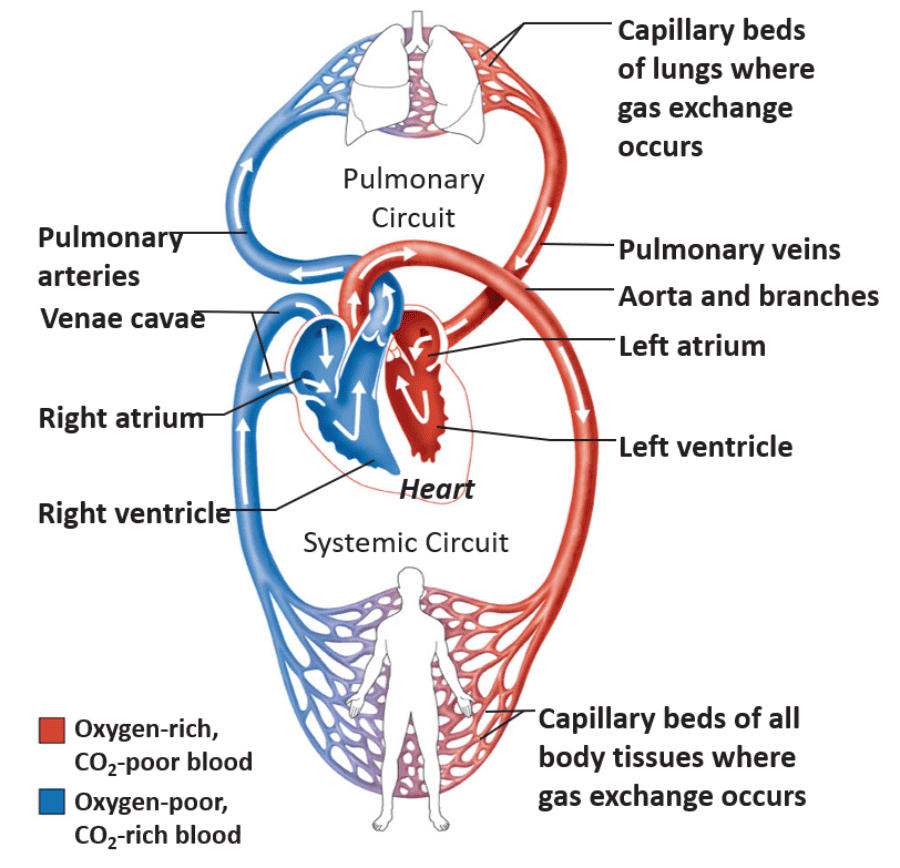
- Pulmonary Circuit:
–Right side receives oxygen-poor blood from the body tissues
–Pumps this blood to the lungs
–Picks up oxygen and dispels CO2
- Systemic Circuit:
–Left side receives oxygen-rich blood returning from the lungs
–Pumps this blood throughout the body
–Supplies O2 and nutrients to the body tissues
Location and Orientation within the Thorax
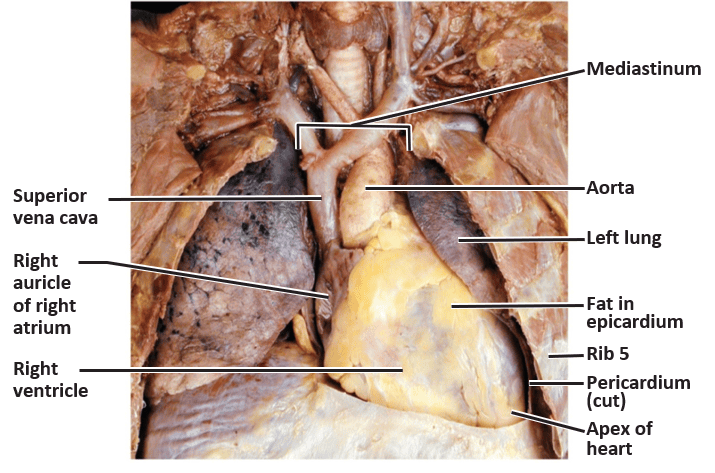
- Heart: hollow and cone-shaped
–About the size of your fist
- Largest organ of the mediastinum (central compartment of the thoracic cavity)
–Located between the lungs
–Apex lies to the left of the midline
–Base is the broad posterior surface
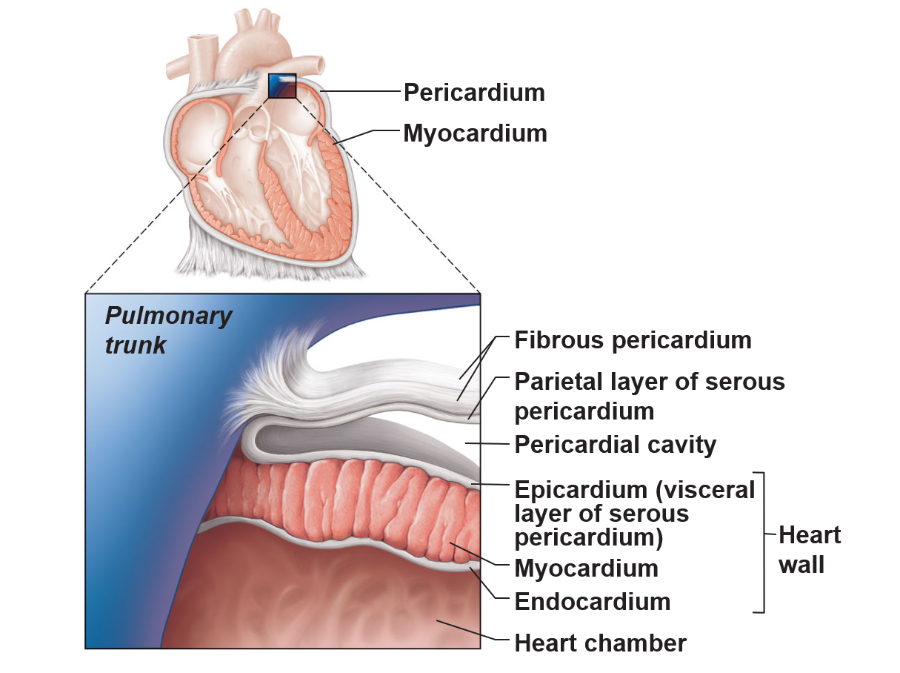
Pericardium of the Heart—Coverings
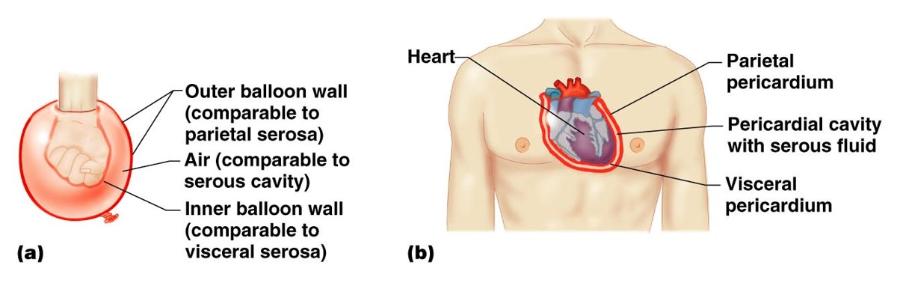
- Pericardium—triple-layered sac that encloses the heart
- Two primary layers
–fibrous pericardium: strong layer of dense connective tissue
–Serous pericardium: formed from two layers
- parietal layer of the serous pericardium
- Visceral layer of the serous pericardium
- Pericardial cavity – between the primary layers
–Epithelial cells secrete lubricating serous fluid that reduces friction
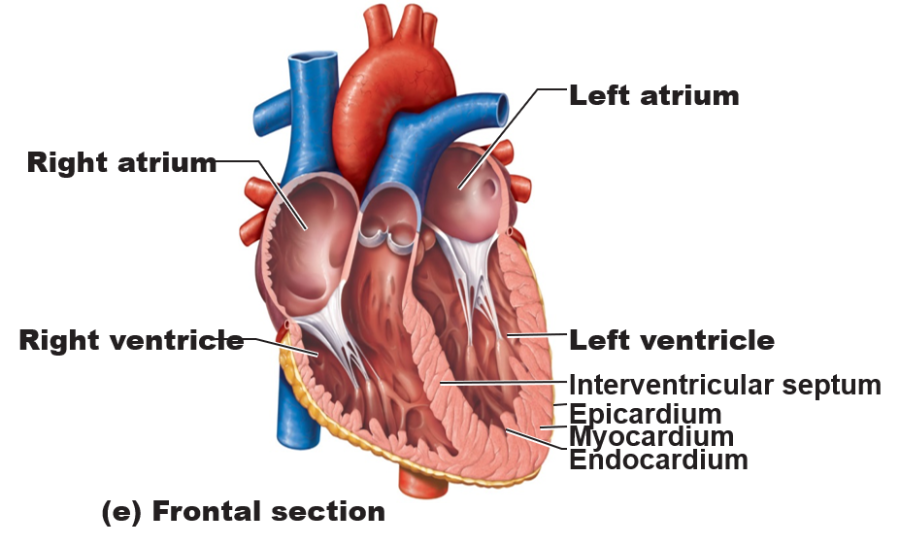
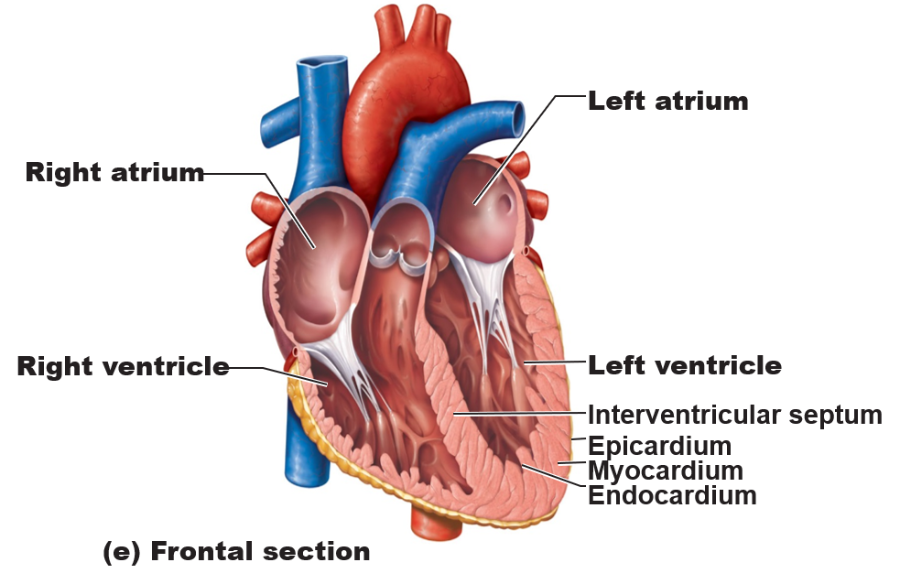
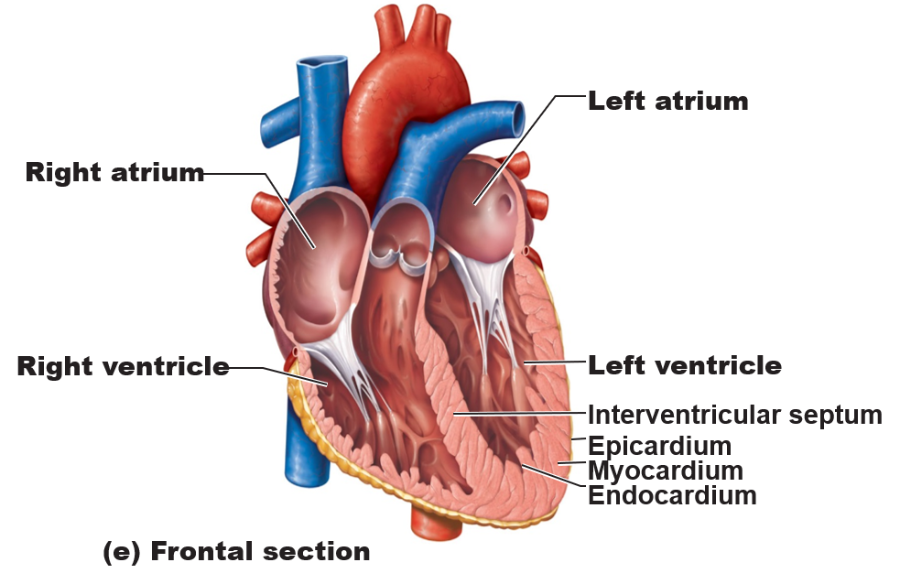
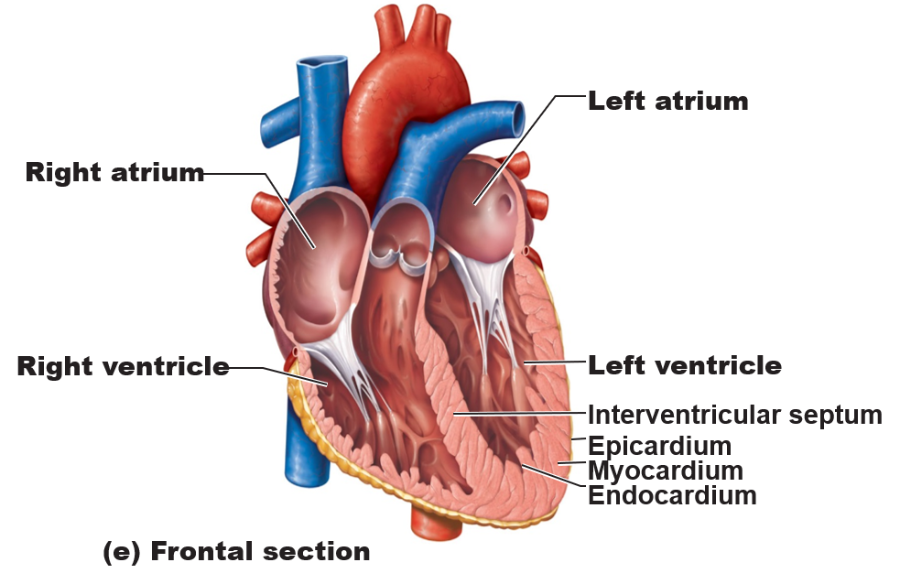
Three Layers of the Heart Wall
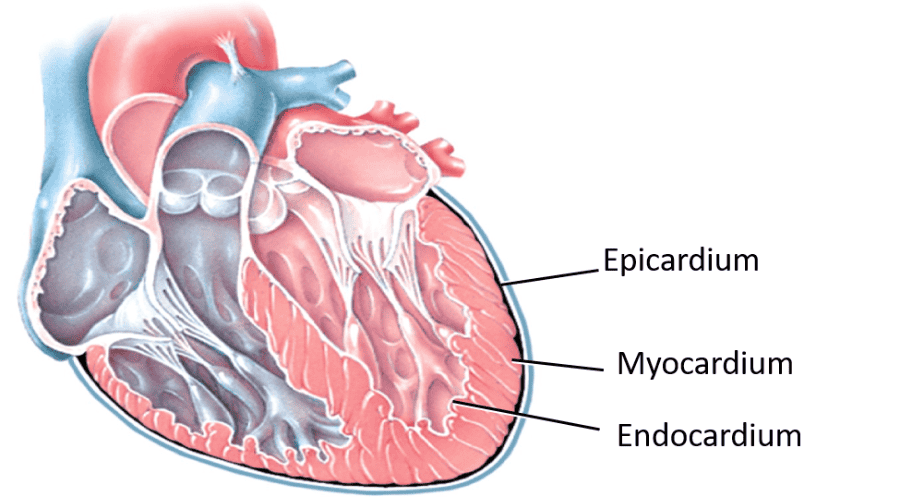
- Epicardium
- Myocardium
- endocardium
Epicardium:
- outer layer of heart wall (and inner visceral layer of serous pericardium)
–Thin, transparent layer
Myocardium:
- middle layer of heart wall
–Cardiac muscle, responsible for pumping action
Endocardium:
- innermost, thin layer of heart wall
–Simple squamous epithelium
–Lines inside of the myocardium
–Covers heart valves and tendons attached to the valves
–Continuous with the epithelial lining of large blood vessels
Layers of the Pericardium and of the Heart Wall
Arrangements of Cardiac Muscle Bundles
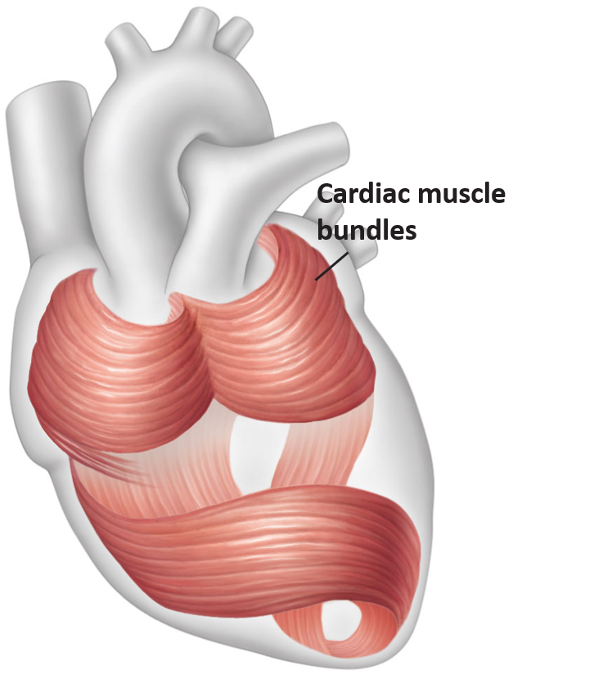
- Myocardium organized in crisscrossing bundles
- Function to squeeze blood through the heart in the proper directions
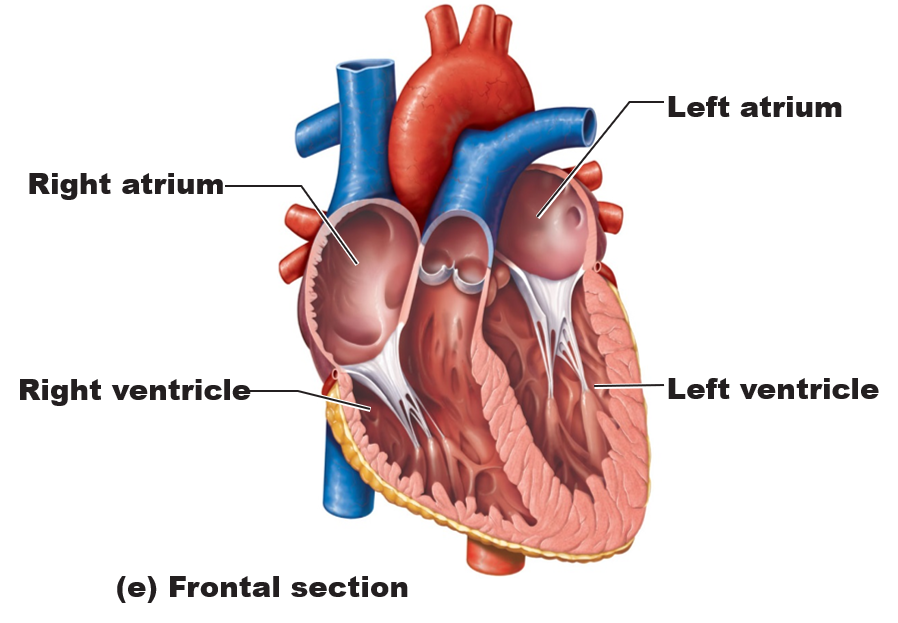
Heart Chambers
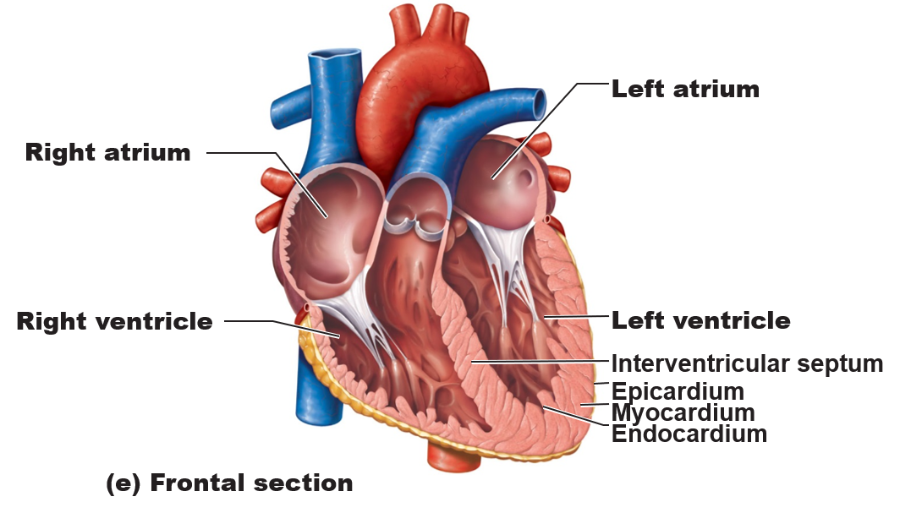
- Right and left atria – superior chambers
- Right and left ventricles – inferior chambers
- Internal divisions – interventricular and interatrial septa
External Markings
–Coronary sulcus forms a crown encircling a boundary between atria and ventricles
–Anterior interventricular sulcus
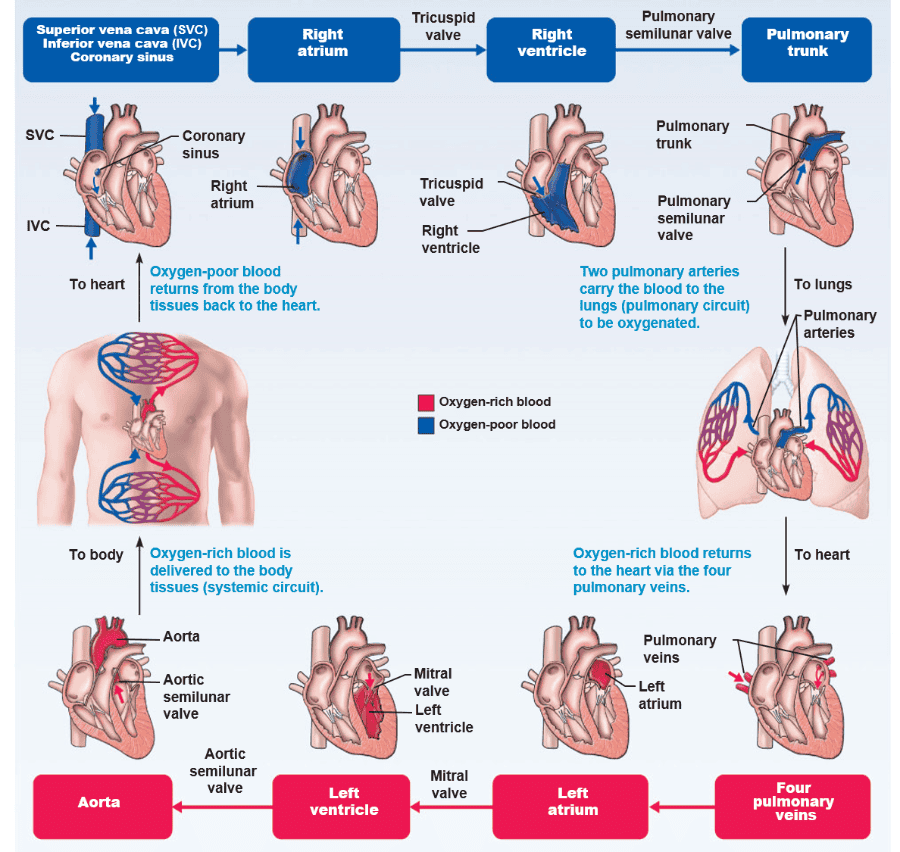
Right Atrium
- Forms right border of heart: receives oxygen-poor blood returning from systemic circuit via veins
–Superior and inferior vena cava and coronary sinus
Right Ventricle
- Receives blood from right atrium through the tricuspid valve or right atrioventricular (AV) valve
- Pumps blood into pulmonary circuit via pulmonary trunk
- Internal walls of right ventricle
–Chordae tendineae: bands attached to cusps of right tricuspid valve
–papillary muscles: attached to chordae tendineae
Pulmonary semilunar valve:
- located at opening of right ventricle and pulmonary trunk
Left Atrium
- Makes up heart’s posterior surface: receives oxygen-rich blood returning from lungs
-Through two right and two left pulmonary veins
- Opens into the left ventricle through the bicuspid or mitral valve (aka the left atrioventricular valve)
Left Ventricle
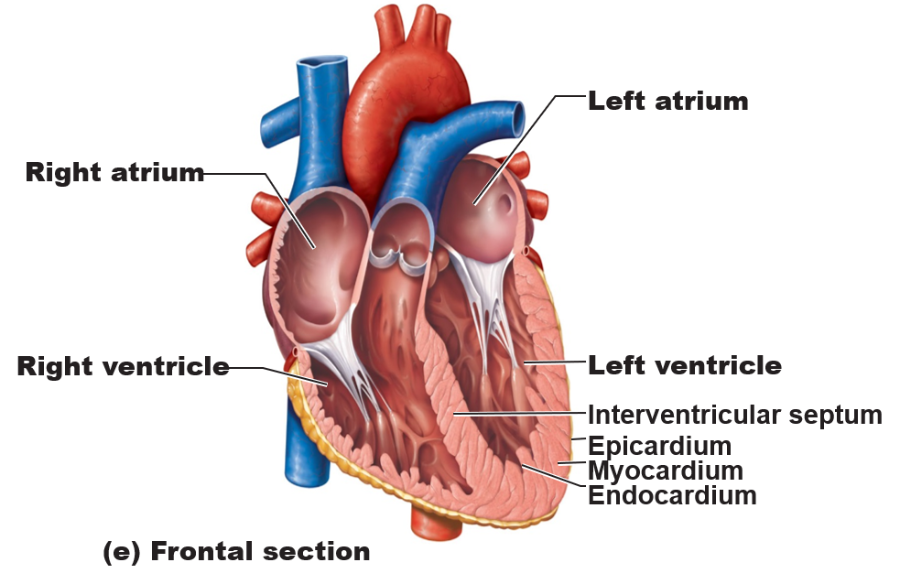
- Forms apex of the heart
- Internal walls of left ventricle
–Chordae tendineae: attached to cusps of left mitral valve
–Papillary muscles
- Superiorly opens into the aorta
–Pumps blood through systemic circuit via aortic semilunar valve (aortic valve)
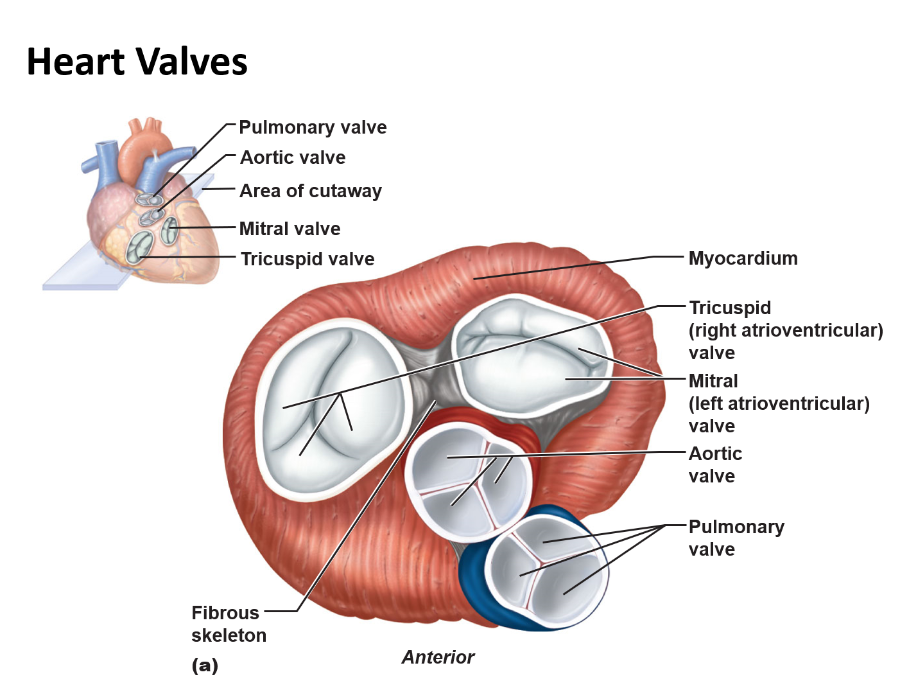
Heart Valves—Valve Structure
- Paired atrioventricular (AV) and semilunar valves enforce one-way flow of blood through the heart
–Designed to prevent back flow in response to pressure changes in the heart chambers
- Each valve
–Two or three cusps
Heart Valves—Valve Structure
- Atrioventricular (AV) valves lie between atria and ventricles
–Right tricuspid valve (3 cusps)
–left bicuspid valve (2 cusps)
- Aortic and pulmonary (semilunar) valves lie at the junction of the ventricles and great arteries
–3 cusps
Heart Valves
Function of the Atrioventricular (AV) Valves
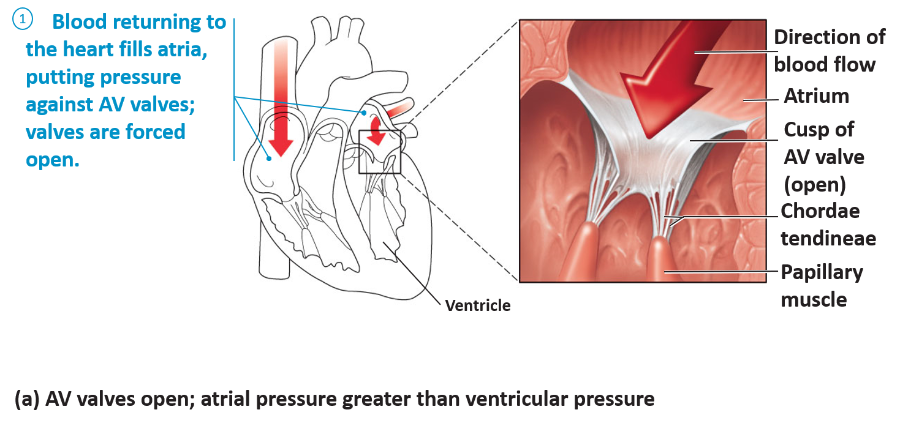
(a) AV valves open; atrial pressure greater than ventricular pressure
Function of the Atrioventricular (AV) Valves
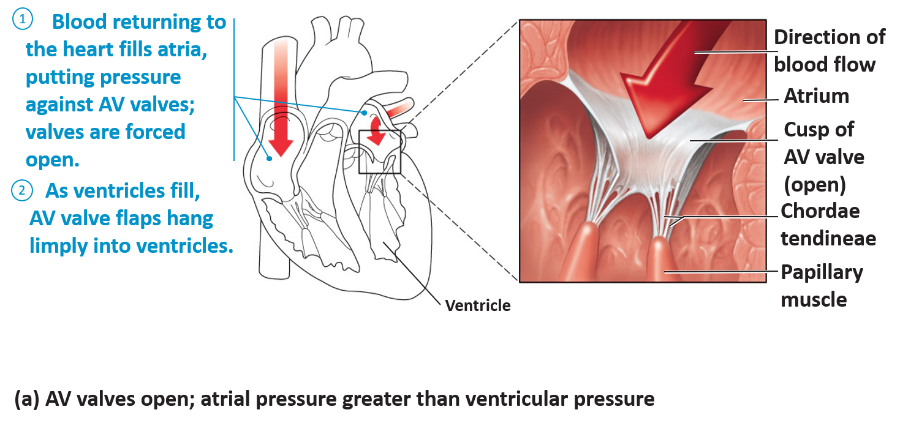
(a) AV valves open; atrial pressure greater than ventricular pressure
Function of the Atrioventricular (AV) Valves
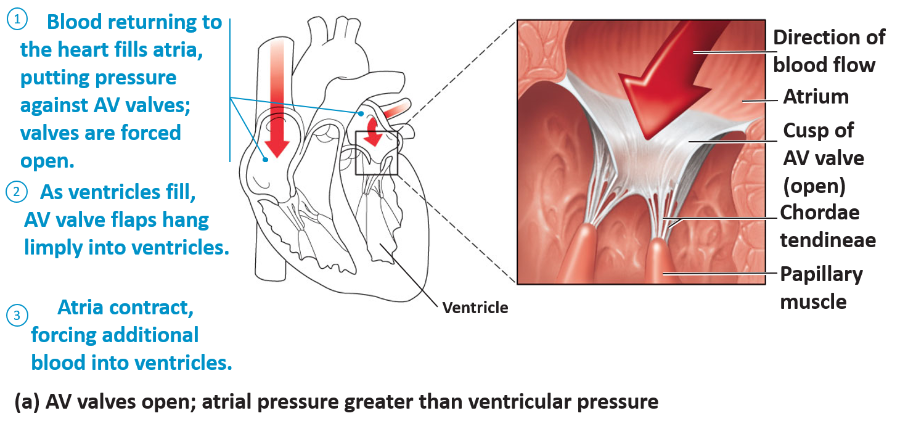
(a) AV valves open; atrial pressure greater than ventricular pressure
- Ventricles relaxed --> valves forced open by blood pressure exerted on their atrial side
Function of the Atrioventricular (AV) Valves
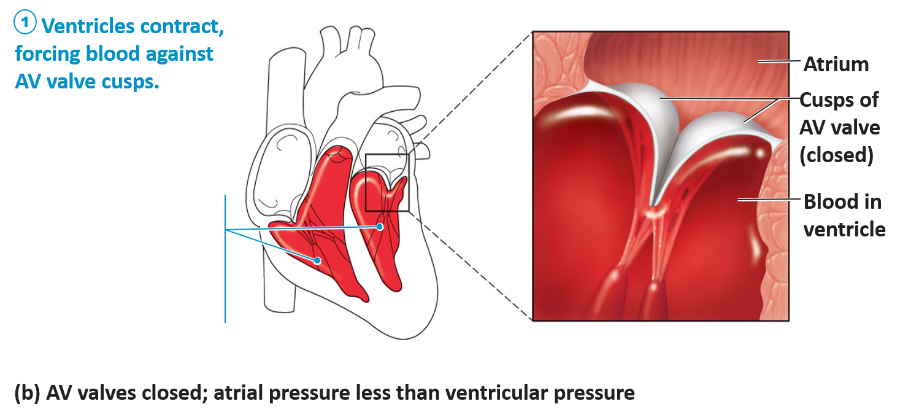
(b) AV valves closed; atrial pressure less than ventricular pressure
Function of the Atrioventricular (AV) Valves
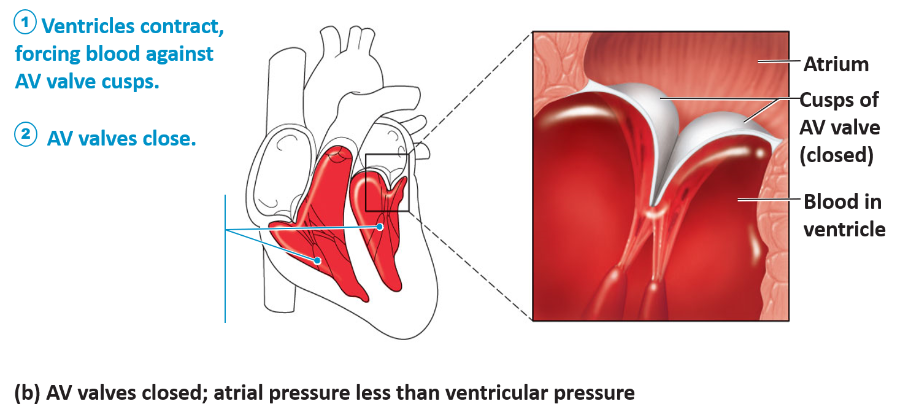
(b) AV valves closed; atrial pressure less than ventricular pressure
Function of the Atrioventricular (AV) Valves
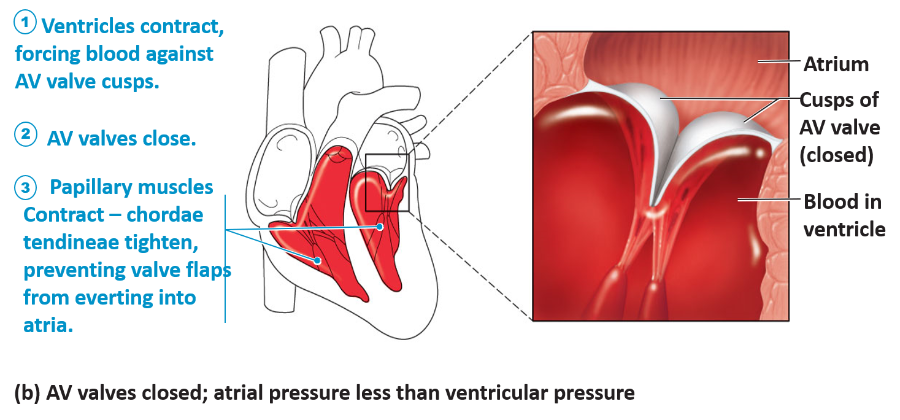
(b) AV valves closed; atrial pressure less than ventricular pressure
- Contraction of ventricles force contained blood superiorly --> valves are pushed shut
Function of the Semilunar Valves
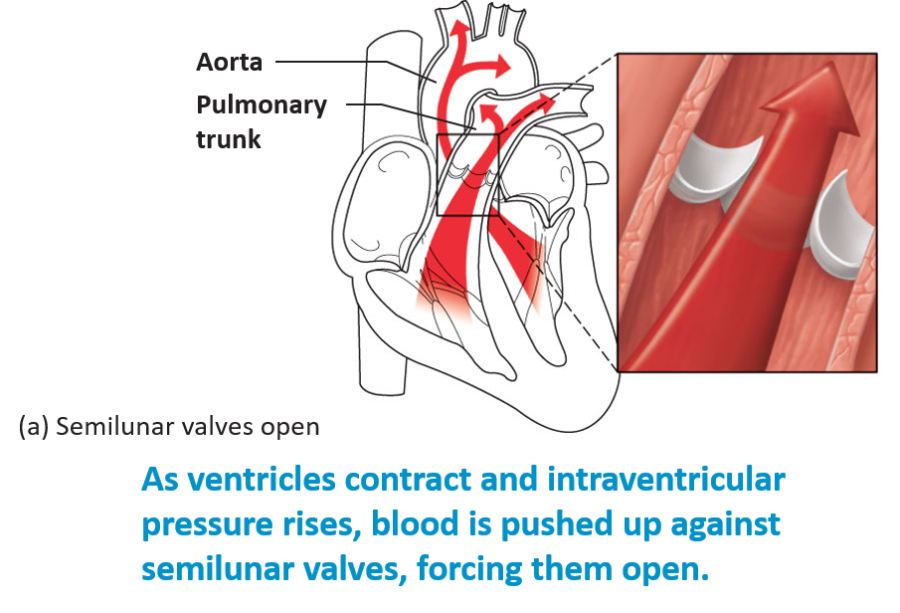
- Ventricular contraction
–Valves pushed open
–Cusps flattened against artery walls
Function of the Semilunar Valves
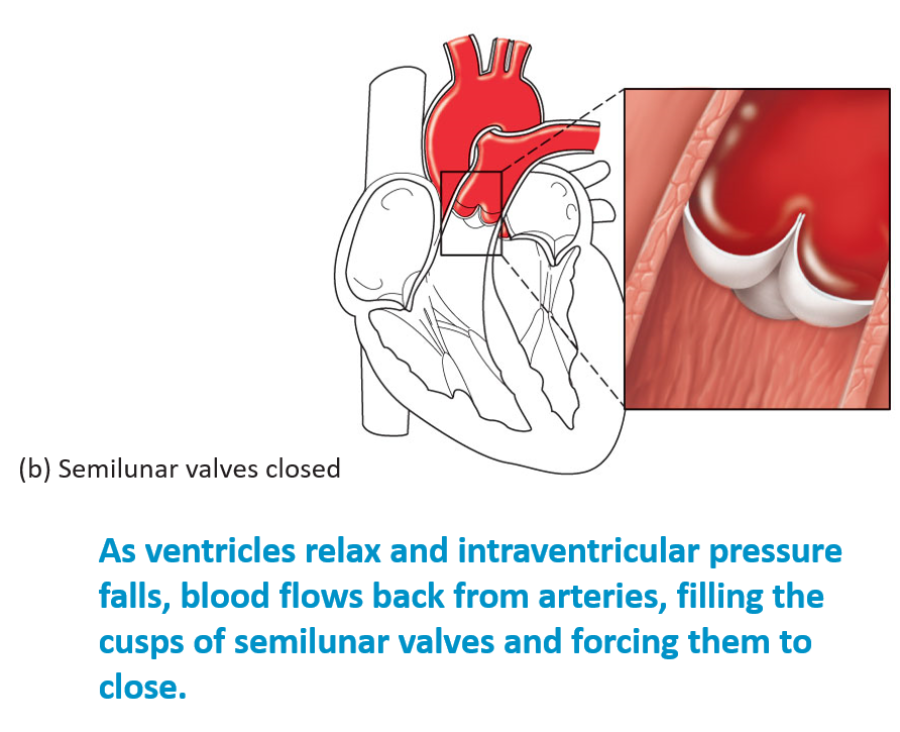
- Ventricular relaxation
–Back flowing blood closes valves
Pathway of Blood Through the Heart
- Beginning with oxygen-poor blood from the superior and inferior venae cavae (coronary sinus)
–Go through pulmonary and systemic circuits
–A drop of blood passes through all structures in sequence
- Atria contract together
- ventricles contract together
Blood flow through the heart.
Structure of Heart Wall
- Walls differ in thickness
–atria—thin walls
–Ventricles—thick walls
- left ventricle generates more force and pumps blood at a higher pressure
–Systemic circuit longer than pulmonary circuit
–Offers greater resistanceto blood flow
Structure of Heart Wall
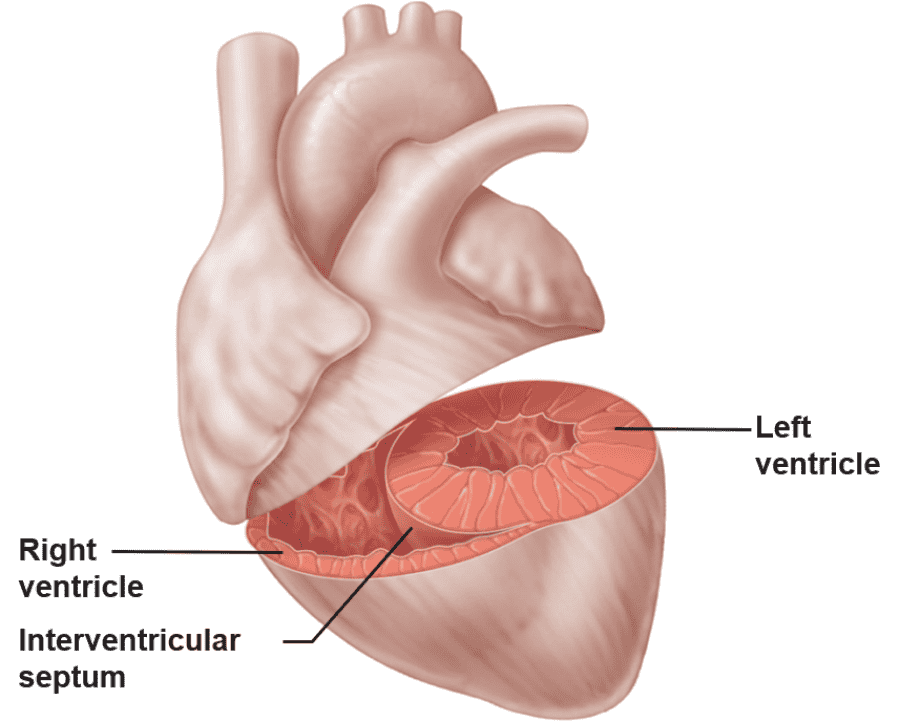
-
Left ventricle—
three times thicker than right
–Exerts more pumping force
–Flattens right ventricle into a crescent shape
Cardiac Muscle Tissue
- Forms a thick layer called myocardium – contains cardiac muscle cells and connective tissue
–Cardiac muscle cells
- Short, branching, 1 or 2 nuclei
- Cells joined at intercalated discs (complex junctions)
- Striated like skeletal muscle
–Contractions
- Pump blood through the heart and into blood vessels
- Sliding filament mechanism
Cardiac Muscle Tissue
- Intercalated discs – complex junctions between cardiac muscle cells - form cellular networks
–Adjacent cells interlock through meshing ‘fingers’
–Fasciae adherens
- Long junctions bind adjacent cells and transmit contractile force
–Gap junctions
- Allow ions to pass between cells, transmitting contractile signal to adjacent cells
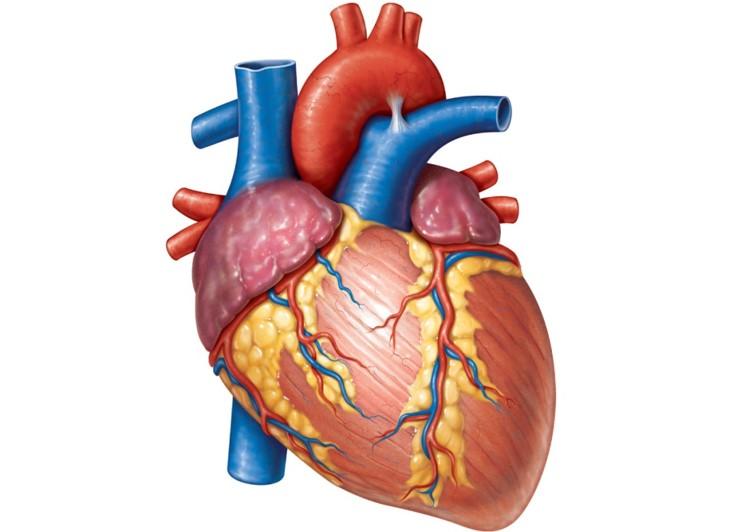
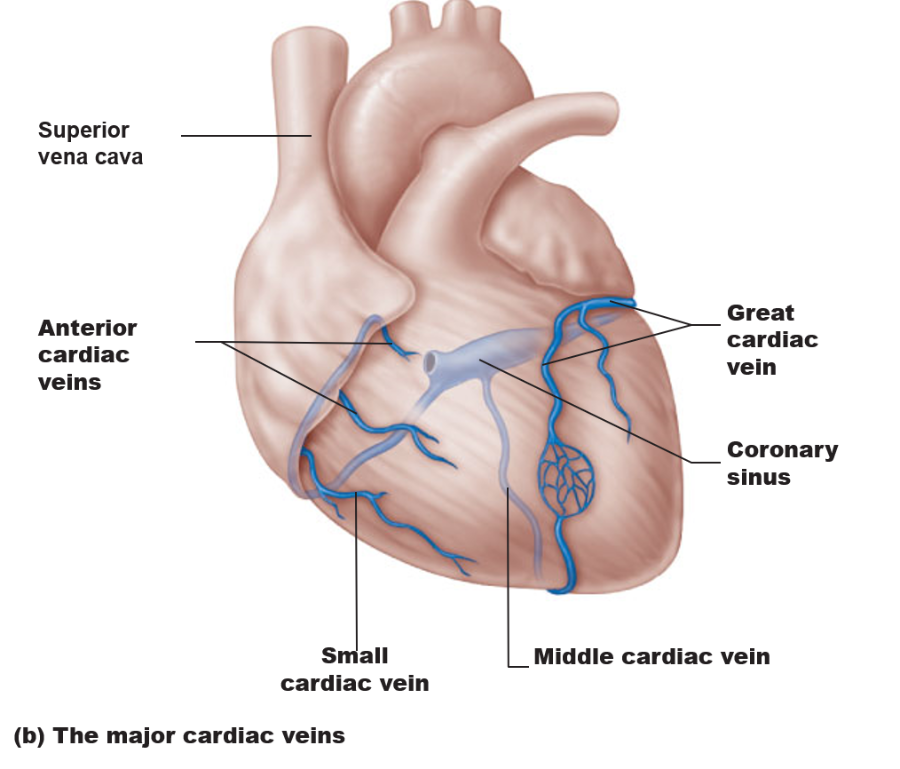
Blood Supply to the Heart
- Heart walls – too thick to obtain oxygen and nutrients from contained blood—heart needs those substances to beat!
- Functional blood supply – coronary arteries
–Left and right coronary arteries
–Arise from the aorta
–Located in the coronary sulcus
Blood Supply to the Heart – Coronary Arteries
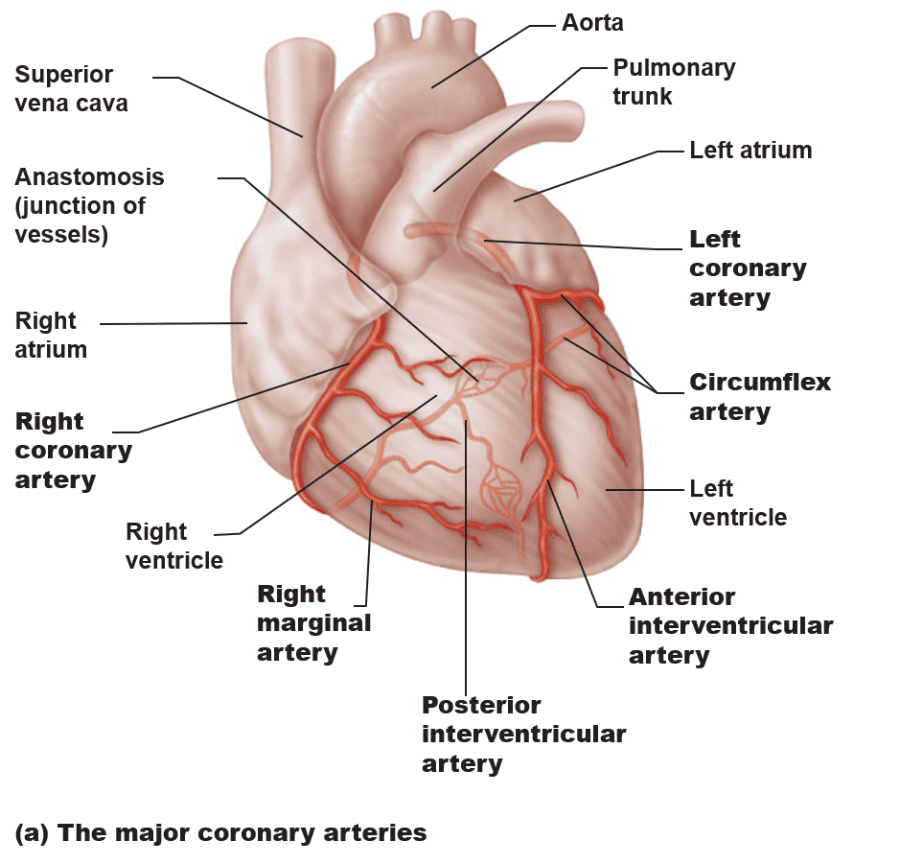
Blood Supply to the Heart
- Deoxygenated blood from heart wall
–Into right atrium
–Occupy sulci on the heart surface
- Coronary sinus – Returns most venous blood from the heart to the right atrium
Blood Supply to the Heart – Cardiac Veins
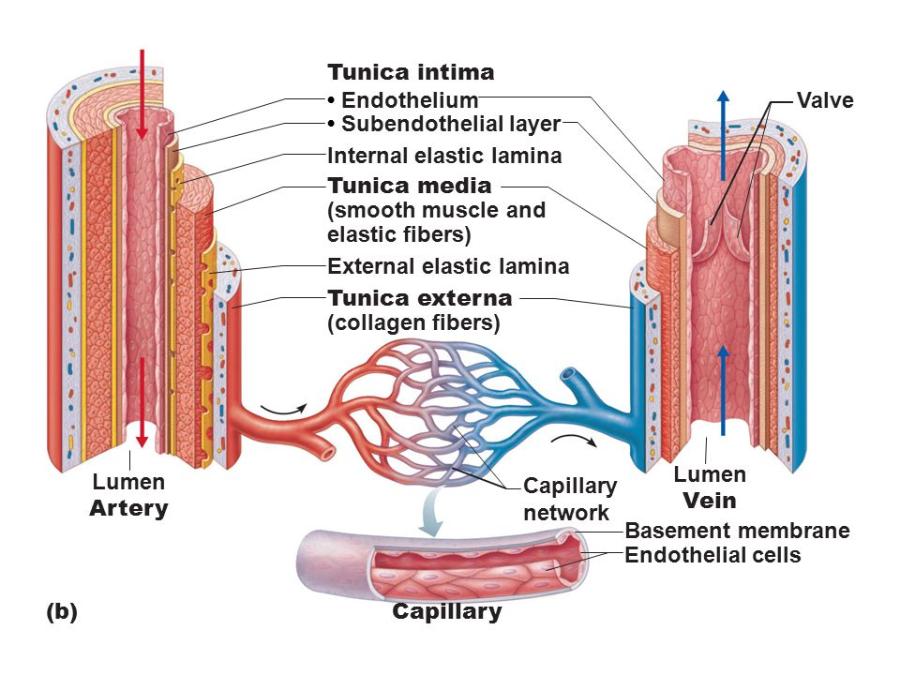
Blood Vessels
Delivery system of dynamic structures that begins and ends at heart
- Arteries
Carry blood away from heart
Oxygenated except for pulmonary circulation & umbilical vessels of fetus
- Capillaries
Contact tissue cells
Directly serve cellular needs
- Veins
Carry blood toward heart
Deoxygenated except for pulmonary circulation
Generalized structure of arteries, veins, and capillaries
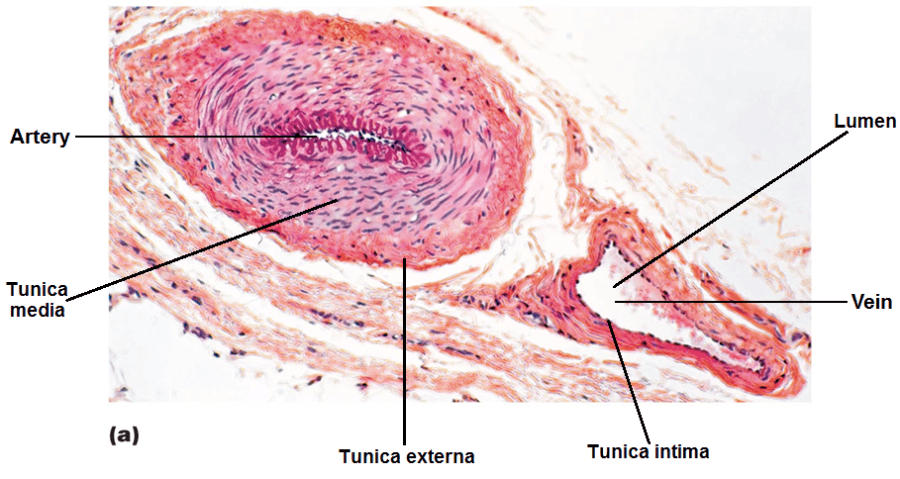
Structure of Blood Vessels
Except for the smallest, composed of three layers (tunics)
Innermost -> outermost
- Tunica intima: Endothelium lines lumen of all vessels
(simple squamous epithelium)
Smooth surface; Continuous with endocardium of heart
“Intimate” contact with blood
- Tunica intima: sheets of smooth muscle & elastic fibers
Contraction causes vasocontriction (smaller vessel diameter)
Relaxation causes vasodilation (larger vessel diameter)
Influence blood flow and blood pressure
- Tunica externa—composed of connective tissue
Contains many collagen and elastic fibers
Cells and fibers run longitudinally
Vasa vasorum (vessels to the vessels): tiny arteries, capillaries, veins
Generalized structure of arteries, veins, and capillaries
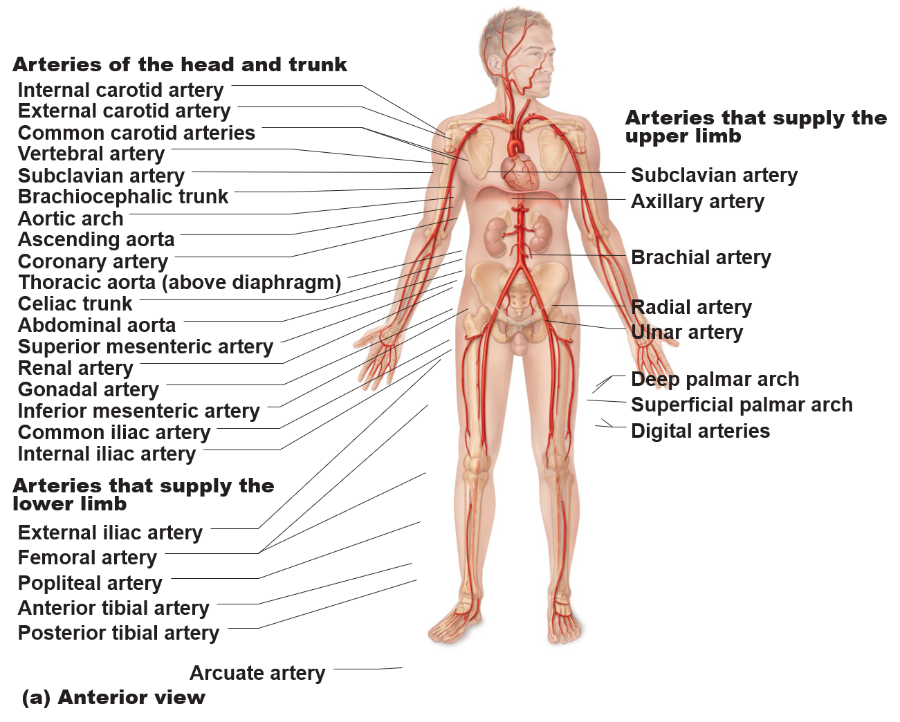
Types of Arteries
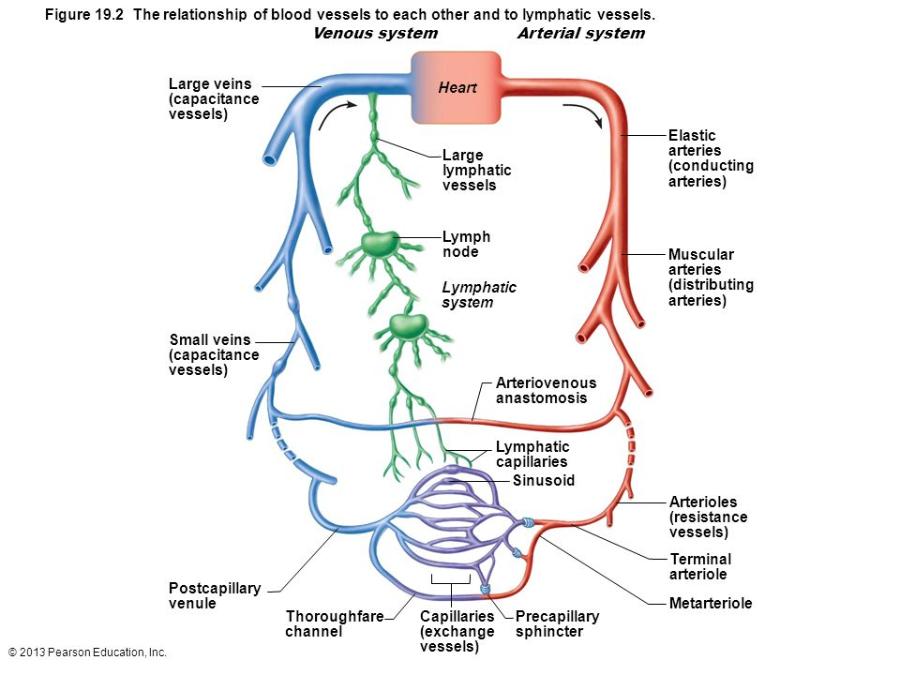
- Passage of blood through the arteries:
Elastic arteries --> Muscular arteries --> Arterioles
The relationship of blood vessels to each other and to lymphatic vessels
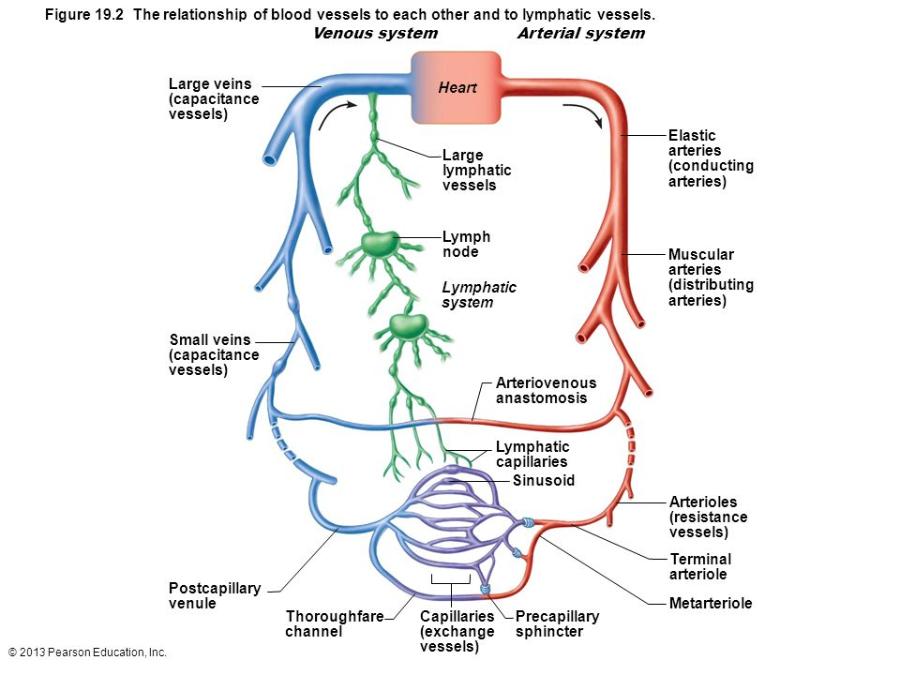
Types of Arteries
- Elastic Arteries
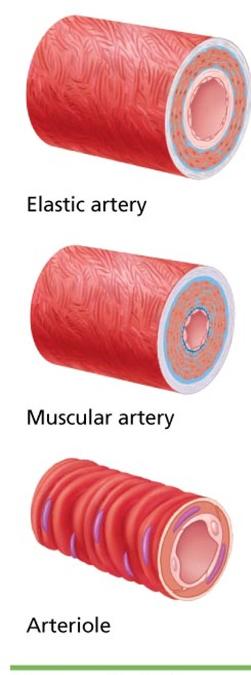
- elastin in all three tunics
- Ex. aorta & its major branches
- Large lumen = low resistance
- Inactive in vasoconstriction
- Act as pressure reservoirs—expand and recoil as blood ejected from heart
Types of Arteries
- Muscular Arteries
- Distal to elastic arteries
- Deliver blood to body organs
- thick tunica media with more smooth muscle
- Active in vasoconstriction
Types of Arteries
- Arterioles
- smallest type of artery
- Lead to capillary beds
- Control flow into capillary beds via vasodilation and vasoconstriction
Capillaries
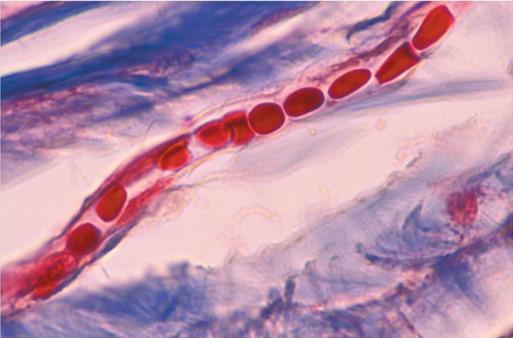
smallest blood vessels – diameter from 8–10 µm
- A single layer of endothelial cells surrounded by a basement membrane
- Most important vessels
- red blood cells pass through single file
Site-specific functions of capillaries
Lungs: oxygen enters blood, carbon dioxide leaves
Small intestines: receive digested nutrients
Endocrine glands: pick up hormones
Kidneys: removal of nitrogenous wastes
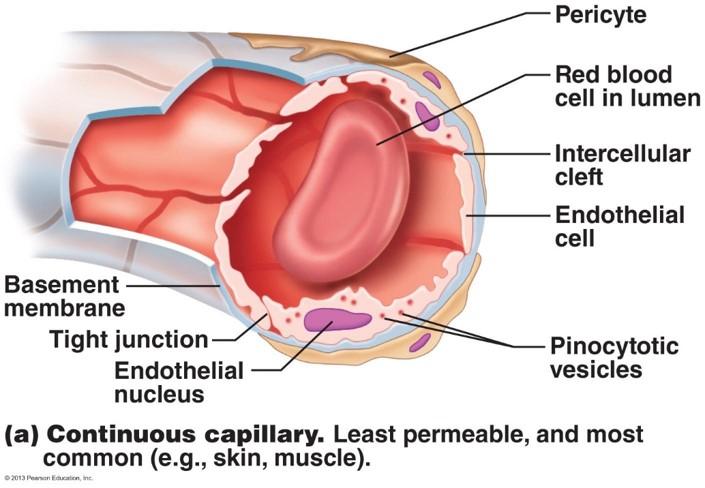
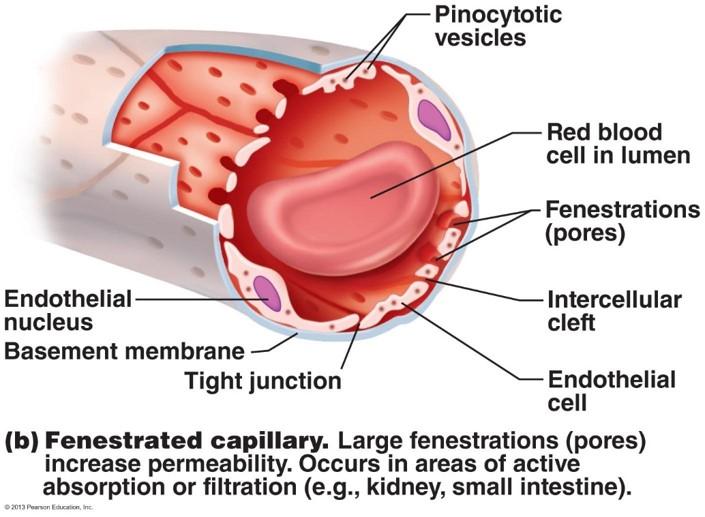
Capillary Permeability
- Endothelial cells held together by tight junctions and desmosomes - block passage of small molecules
But junctions are incomplete…
- Intercellular clefts: gaps of unjoined membrane
Passageway for small molecules to enter and exit
- Fenestrations (pores): holes through endothelial cells
Increases permeability
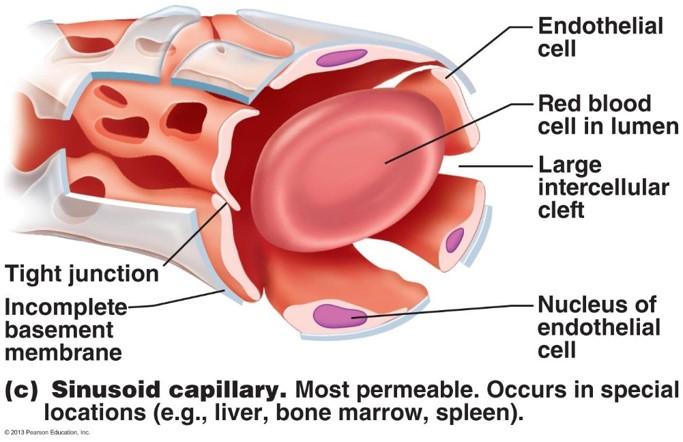
Types of capillaries- based on structure:
- Continuous: most common, lack pores
Found in most organs (skeletal muscle, lungs, skin, CNS)
- Fenestrated: large pores; increasedpermeability
Occur where high exchange rates are needed (kidney, small intestines)
- Sinusoids: many pors and clefts; most permeable
Occur in limited locations (liver, bone marrow, spleen)
1.Continuous capillaries
1.Fenestrated capillaries
1.Sinusoid capillaries (sinusoids)
The relationship of blood vessels to each other and to lymphatic vessels.
Capillary Beds
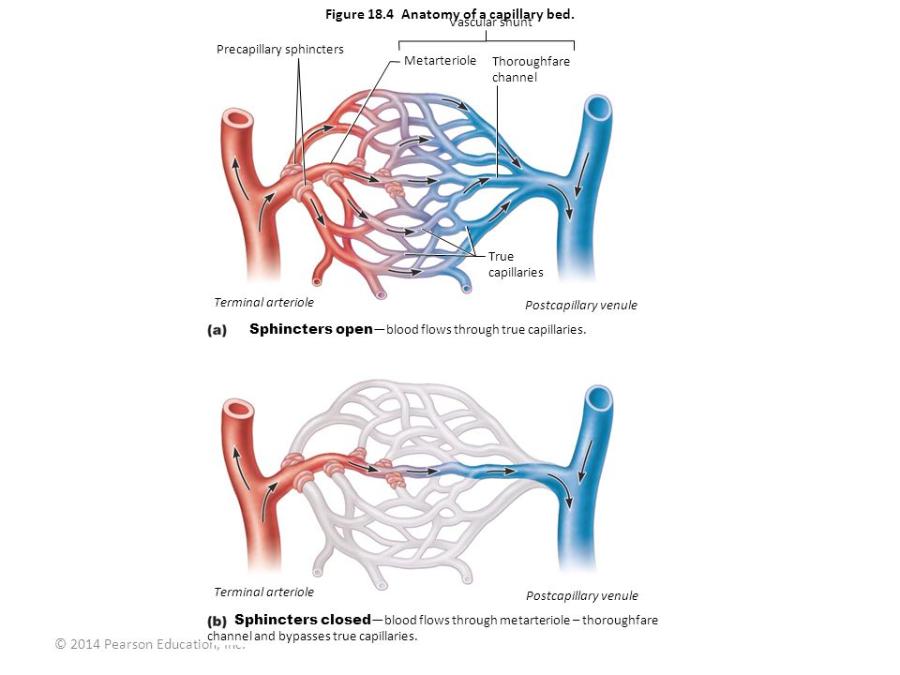
- Network of capillaries running through most tissues
- Precapillary sphincters – regulate the flow of blood to tissues
Composed of smooth muscle cells
Regulated by local chemical conditions and vasomotor nerves
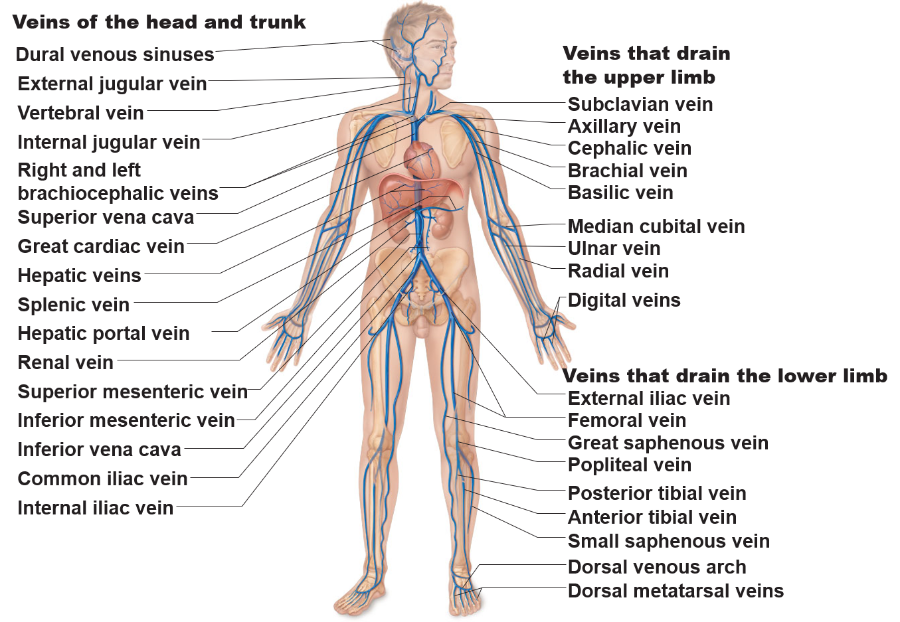
Veins
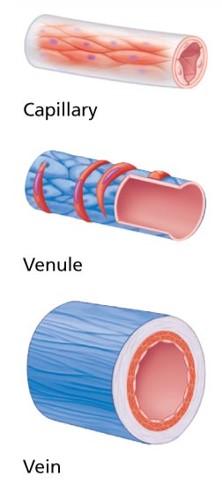
Venules: smallest veins
Form when capillaries unite
- Postcapillary venules: smallest venules
- Venules join to form veins
Veins
Conduct blood from capillaries toward the heart
- Range in size from 0.5mm to 3 cm (venae cavae)
- Blood pressure is much lower than in arteries
- Walls are thinner
- lumen of a vein is larger
Capacitance vessels
i.e. blood reservoir
Contain up to 65% of blood supply
Valves
Vascular sinus
Veins: Adaptations for Blood Flow Return
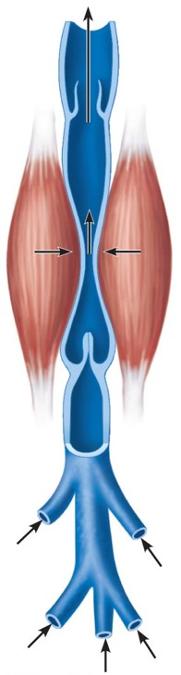
Large-diameter lumens offer little resistance
Venous valves prevent backflow of blood
- Most abundant in veins of limbs
Venous sinus
- Flattened veins with extremely thin walls
- E.g., coronary sinus of the heart and dural sinuses of the brain
- Collect blood
Circulatory Routes
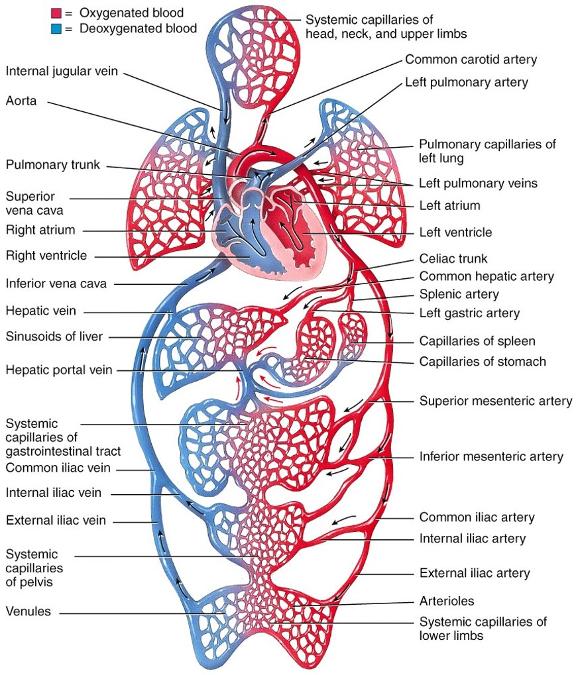
Parallel blood flow
Each organ receives its own supply of oxygenated blood
Two basic routes for blood flow:
- Systemic circulation
- Pulmonary circulation
Systemic Circulation
- Carries oxygen and nutrients to body tissues
- Removes carbon dioxide and other wastes and heat from the tissues
- All systemic arteries branch from the aorta
- All veins of systemic circulation drain into superior vena cava, inferior vena cava, or coronary sinus
- The blood vessels are organized according to regions of the body
Major Arteries
Major Veins of the Systemic Circulation
Physiology of Circulation
- Blood flow
volume of blood flowing through vessel, organ, or entire circulation in given period
- Measured as ml/min
- Equivalent to cardiac output (CO) for entire vascular system
- Relatively constant when at rest
- varies widely through individual organs, based on needs
Physiology of Circulation
- Blood pressure (BP)
blood pressure per unit area exerted on wall of blood vessel by blood
Measured as millimeters of Mercury (mm Hg)
Pressure gradient: blood moves from higher to lower pressure areas
Physiology of Circulation
- resistance
Opposition to flow; generally in systemic circulation
Measure of amount of friction blood encounters with vessel walls
Physiology of Circulation
- Three important sources of resistance
Constant:
1.Blood viscosity
- ¨The "stickiness" of blood due to formed elements and plasma proteins; Increased viscosity = increased resistance
2.Total blood vessel length
- ¨Longer vessel =greater resistance encountered
Variable:
3.Blood vessel diameter
- ¨Constantly changing; important influence on resistance
- ¨Smaller vessel diameter, high resistance
- ¨large vessel diameter, less resistance
Relationship Between Blood Flow, Blood Pressure, and Resistance
Blood flow(F) directly proportional to blood pressure gradient (change in P)
- If change in P increases , blood flow decreases
Blood flow inversely proportional to resistance (R)
- If R increases , blood flow decreases
Resistance more important in influencing local blood flow
- Easily changed by altering blood vessel diameter
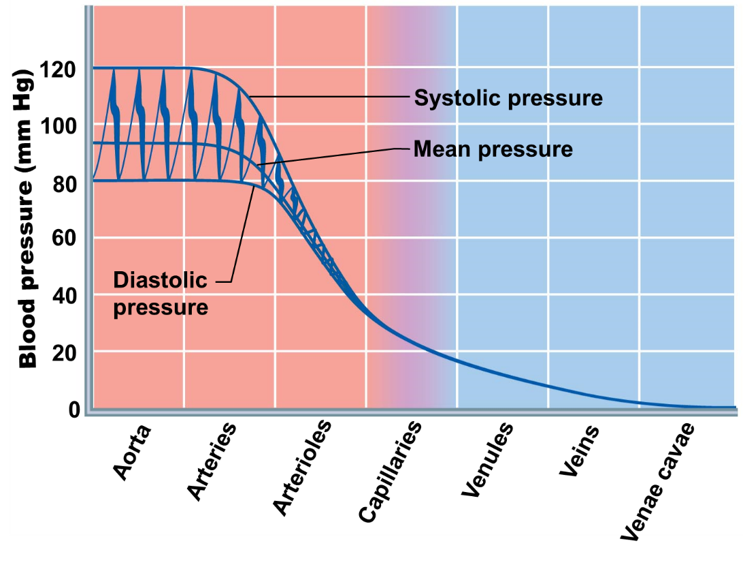
Systemic Blood Pressure
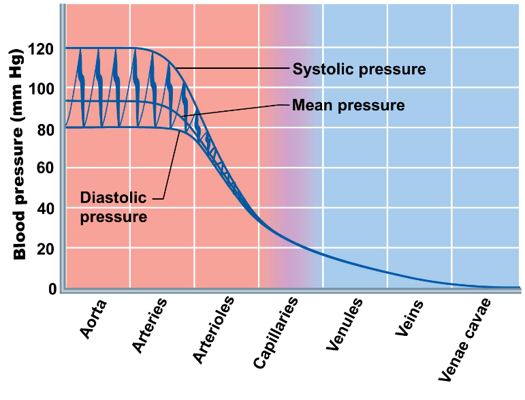
Blood Flow
- Generated by pumping of heart
Blood flow opposed by resistance -->Pressure
Blood Pressure
- highest in the aorta and declines throughout the pathway (0 mm Hg in the right atrium)
Arteries close to the heart are flexible and accommodate high volume
Arterial Blood Pressure
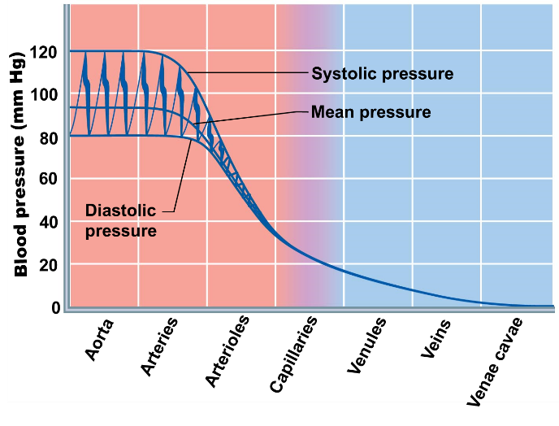
systolic pressure: pressure exerted in aorta during contraction of left ventricle (systole)
- Blood is forced into the aorta
- Averages 120 mm Hg in normal adult
Diastolic pressure: lowest level of aortic pressure
- When blood is prevented from flowing back into the ventricles by the closed semilunar valve (diastole, relaxing of ventricle)
- 70–80 mm Hg