BMD 315: Module 7 Learning Objectives
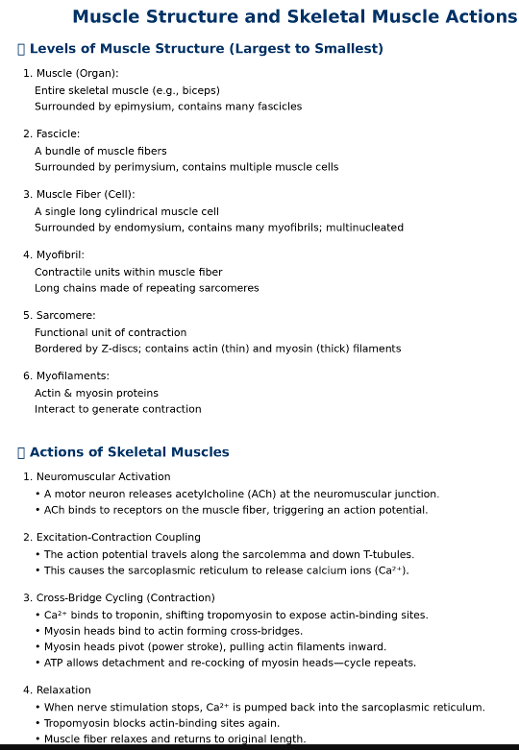
Describe the different levels of muscle structure and the actions of skeletal muscles.
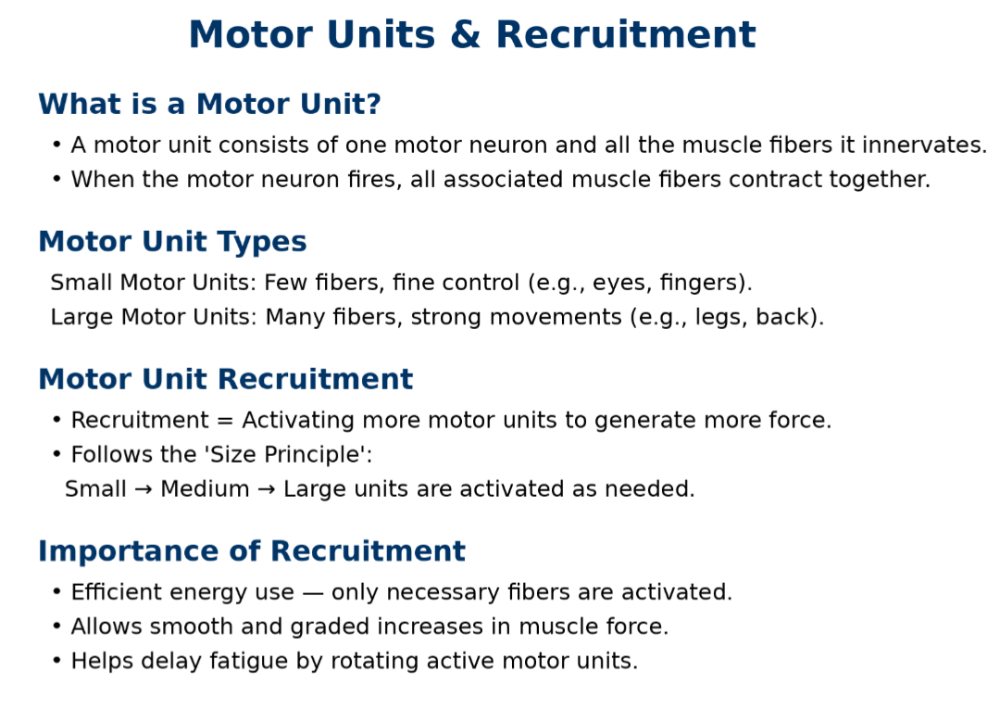
Describe motor units and explain the significance of recruitment of motor units.
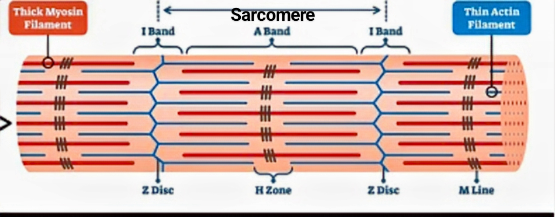
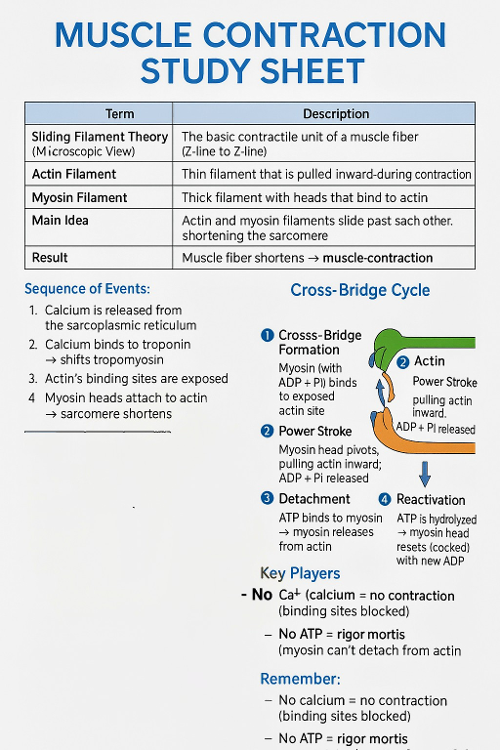
Describe the banding pattern of a myofibril and how these bands change length during muscle contraction.
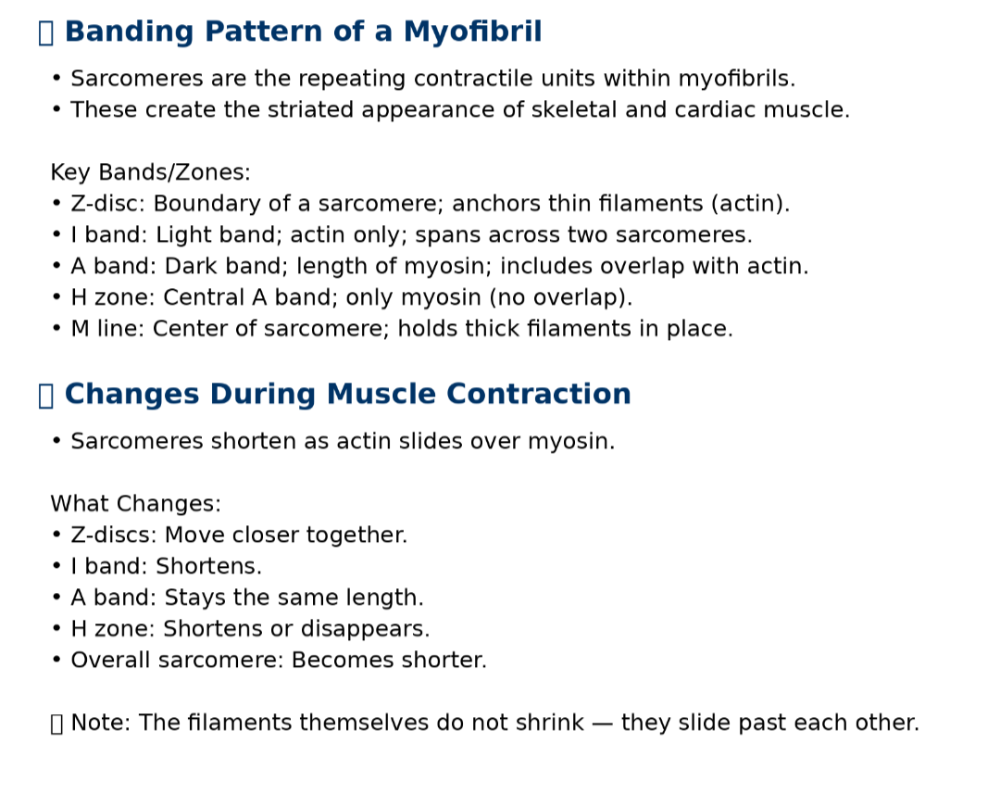
Zones of the Sacromere
Explain the cross-bridge cycle and the sliding filament theory of contraction.
Explain excitation-contraction coupling in skeletal muscle.
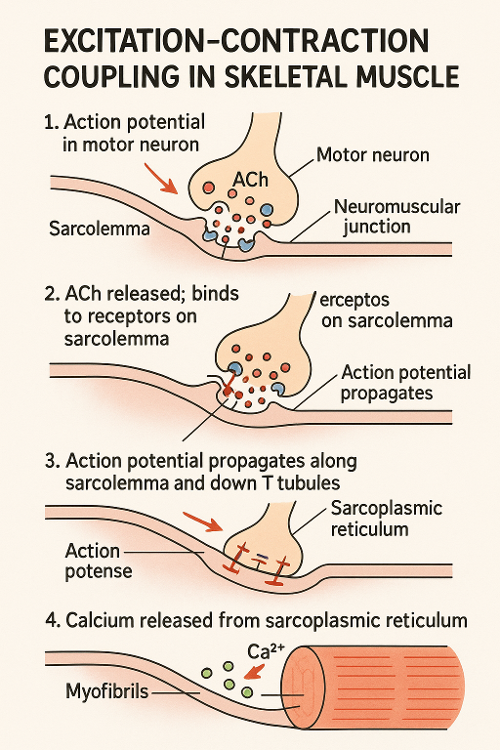
1. Action Potential Arrives: A nerve impulse (action potential) travels down a motor neuron to the neuromuscular junction.
2. ACh Release: The motor neuron releases acetylcholine (ACh) into the synaptic cleft.
3. ACh Binds Receptors: ACh binds to receptors on the muscle cell membrane (sarcolemma), triggering an action potential in the muscle fiber.
4. AP Travels Down T-Tubules: This action potential spreads along the sarcolemma and down T-tubules.
5. Calcium Release: The signal causes the sarcoplasmic reticulum to release Ca²⁺ ions.
6. Muscle Contraction Begins: Calcium binds to troponin, shifting tropomyosin and exposing actin binding sites for myosin, initiating contraction via the cross-bridge cycle.
Distinguish between the different types of muscle contractions and the differences for in vivo versus in vitro.
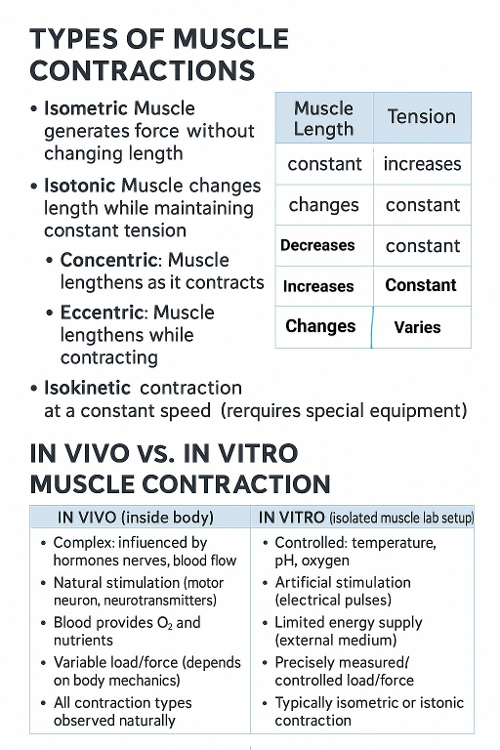
Describe what factors determine if a contraction will be isometric or isotonic.
What Determines If a Contraction Is Isometric or Isotonic?
1. Load vs. Force Generated
- If muscle tension = load ➝ Isometric (no movement)
- If muscle tension > load ➝ Isotonic (movement occurs)
2. Muscle Activation and Neural Input
Higher frequency and intensity of stimulation can increase tension and allow movement (isotonic).
3. Muscle Condition
Fatigued or weak muscles may fail to produce enough force → may become isometric even when attempting isotonic contraction
4. Mechanical Constraints
If the muscle is fixed or the joint is locked, contraction will be isometric regardless of effort.
5. Intended Function
Some actions (like stabilization) are designed to be isometric, while others (like lifting) are inherently isotonic.
Describe the relationship between the resting muscle length and the strength of its contraction.
The relationship between resting muscle length and the strength of its contraction is described by the length-tension relationship in skeletal muscle physiology:
Length-Tension Relationship
Optimal Resting Length = Maximum Force Generation
- When a muscle fiber is at its ideal resting length (typically around 100–120% of its resting length), the actin and myosin filaments overlap in a way that allows the greatest number of cross-bridges to form.
- This results in the strongest possible contraction.
Too Short (Overly Contracted) = Weaker Contraction
If the sarcomere is too short:
- Actin filaments overlap excessively.
- Myosin heads have fewer sites to bind.
- Internal crowding interferes with contraction.
- → Reduced force.
Too Long (Overstretched) = Weaker Contraction
- If the sarcomere is too stretched:
- There is minimal overlap between actin and myosin.
- Fewer cross-bridges can form.
- → Reduced force.
> There is an optimal muscle length at which contraction is strongest. Too much stretch or too much shortening reduces the muscle’s ability to generate force.
Explain the roles of creatine and creatine phosphate in muscle physiology.
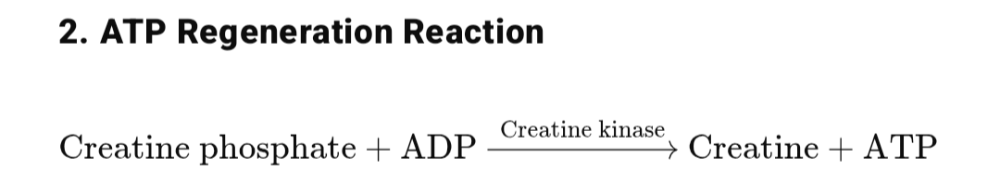
Creatine Phosphate (Phosphocreatine)
- Acts as a rapid energy buffer for regenerating ATP in muscle cells.
- Stores high-energy phosphate groups that can be donated to ADP.
ATP Regeneration Reaction: This reaction is very fast and supplies ATP for the first 10–15 seconds of intense activity (e.g., sprinting, lifting).
Creatine
- Once creatine phosphate donates its phosphate, it becomes creatine.
- Creatine can be rephosphorylated (restored) during rest using ATP produced by aerobic metabolism.
Distinguish the different types of skeletal muscle fibers.
Type I (Slow-twitch)
- Lots of mitochondria, myoglobin, and capillaries
- Generates less force but sustains activity longer
- Suited for aerobic, long-duration tasks
Type IIa (Intermediate fast-twitch)
- Has features of both Type I and IIb
- More adaptable based on training
- Suited for mixed activities (e.g., soccer, rowing)
Type IIb / IIx (Fast-twitch glycolytic)
- Few mitochondria, low myoglobin, high glycogen stores
- High power output but fatigue quickly
- Best for explosive, anaerobic efforts
Describe aerobic capacity
Aerobic Capacity (VO₂ max): The maximum amount of oxygen the body can use during intense exercise.
- Indicator of: Cardiovascular fitness and endurance potential.
- Measured in: mL O₂ / kg / min
- Higher aerobic capacity → better ability to sustain prolonged aerobic exercise.
Influenced by: Heart & lung function, Blood flow to muscles, and Mitochondrial density and enzyme activity
Describe lactate threshold.
The exercise intensity at which lactic acid begins to accumulate in the blood faster than it can be cleared.
- Occurs when: Muscle cells switch more to anaerobic metabolism.
- Significance: Marker of sustainable endurance performance. Athletes with a higher lactate threshold can perform at a higher intensity for longer.
- Can be improved with: Interval training and aerobic conditioning
Describe muscle fatigue
The decline in a muscle’s ability to generate force.
Causes: ATP depletion, Ion imbalances (e.g., Ca²⁺, K⁺, H⁺), Lactic acid accumulation (lowers pH, affects enzyme function), and Neuromuscular fatigue (reduced signaling)
Types:
- Central fatigue: Originates in the CNS (mental/nerve-based)
- Peripheral fatigue: Originates in muscle fibers (metabolic)
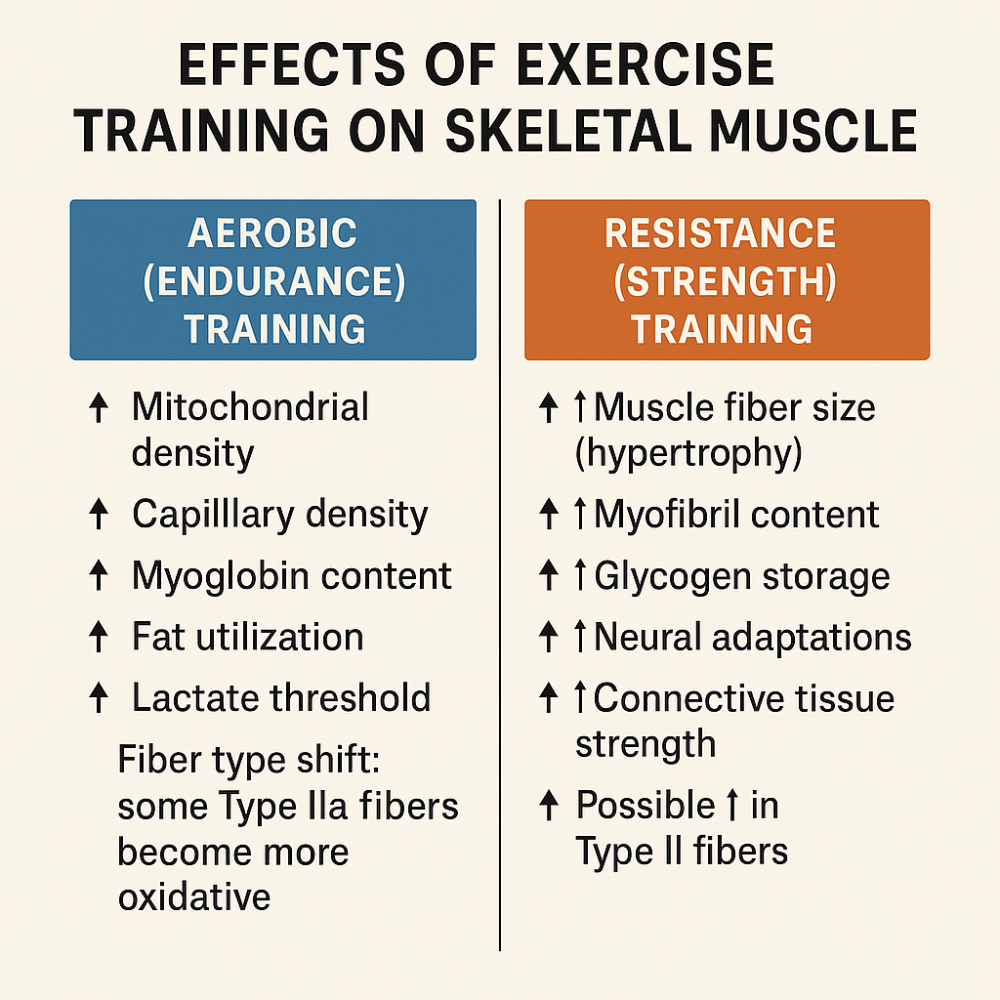
Explain how exercise training affects skeletal muscle.
Describe the components of monosynaptic muscle stretch reflexes.
The monosynaptic muscle stretch reflex is a simple reflex arc that helps maintain muscle tone and postural stability. It involves one synapse between the sensory and motor neurons in the spinal cord and is the basis for reflexes like the knee-jerk (patellar) reflex.
Keys components
1. Muscle Spindle (Stretch Receptor)
Located within the muscle
- Detects changes in muscle length (stretch)
- Sends sensory (afferent) signals to the spinal cord via Ia afferent fibers
2. Ia Afferent Sensory Neuron:
Carries the stretch signal directly to the spinal cord and Synapses directly (monosynaptically) with the alpha motor neuron
3. Alpha (α) Motor Neuron
Receives input from the Ia afferent, Sends motor output to the same (homonymous) muscle, and Causes contraction, counteracting the stretch
4. Effector Muscle (Same Muscle): Contracts reflexively to resist the stretch
The role of gamma motor neurons
- Innervate the intrafusal fibers (inside the muscle spindle), not the contractile muscle fibers themselves
- Maintain sensitivity of the muscle spindle during muscle contraction
- Adjust spindle tension so it remains responsive during both stretch and contraction
- Work in parallel with alpha motor neurons during coactivation to keep feedback loop active even when the muscle shortens
Describe the effects of Golgi tendon organs.
Golgi tendon organs are sensory receptors located at the junction between a muscle and its tendon. They monitor muscle tension, not length like muscle spindles.
Main Effects of Golgi Tendon Organs
1. Detect Excessive Muscle Tension: When a muscle contracts forcefully, the GTO senses the increased tension in the tendon.
2. Send Inhibitory Signals to the Spinal Cord: The GTO sends a signal through Ib afferent neurons to the spinal cord.
These neurons connect to inhibitory interneurons, which inhibit the alpha motor neuron supplying the same muscle.
3. Result: Muscle Relaxes: This prevents damage from too much force by causing the muscle to reduce contraction or relax.
Protective Function
- Acts as a safety mechanism against muscle or tendon injury.
- Prevents tearing by reducing tension when it gets too high.
Ex: If you try to lift a weight that’s too heavy, GTOs may reflexively inhibit the muscle to stop you from injuring yourself.
Explain reciprocal innervation of skeletal muscles.
a neural mechanism that allows one muscle to contract while its opposing (antagonist) muscle relaxes, so movement is smooth and coordinated.
1. Muscle is stimulated to contract: A reflex (like the stretch reflex) activates a motor neuron for a muscle (e.g., the quadriceps).
2. At the same time, the sensory neuron also activates an inhibitory interneuron in the spinal cord.
3. Inhibitory interneuron blocks the antagonist muscle: It prevents the opposite muscle (e.g., the hamstrings) from contracting.
4. Result: Agonist muscle contracts, antagonist muscle relaxes → smooth movement.
Ex: When you kick your leg, the quadriceps contract while the hamstrings relax.
Explain the functions of alpha and gamma motor neurons during the voluntary control of muscle contraction.
During voluntary movement, alpha and gamma motor neurons work together to coordinate force and maintain feedback sensitivity.
1. Alpha (α) Motor Neurons: Control the main contraction of skeletal muscles.
- Innervate: Extrafusal muscle fibers (the force-generating fibers).
- Result: Muscle shortens and produces movement.
Ex: When you lift a cup, alpha motor neurons activate the biceps to contract.
2. Gamma (γ) Motor Neurons: Keep muscle spindles sensitive during movement.
- Innervate: Intrafusal muscle fibers inside the muscle spindle (not force-generating).
- Maintain tension in the spindle so it can still detect stretch, even while the muscle is contracting.
- Prevents loss of proprioceptive feedback during muscle shortening.
Alpha-Gamma Coactivation
- Occurs during voluntary movement.
- Both alpha and gamma motor neurons are activated simultaneously.
- Ensures the muscle contracts while keeping the stretch receptors (spindles) active → smooth, coordinated motion and feedback.
Explain how cardiac muscle differs from skeletal muscle in its structure and regulation of contraction.
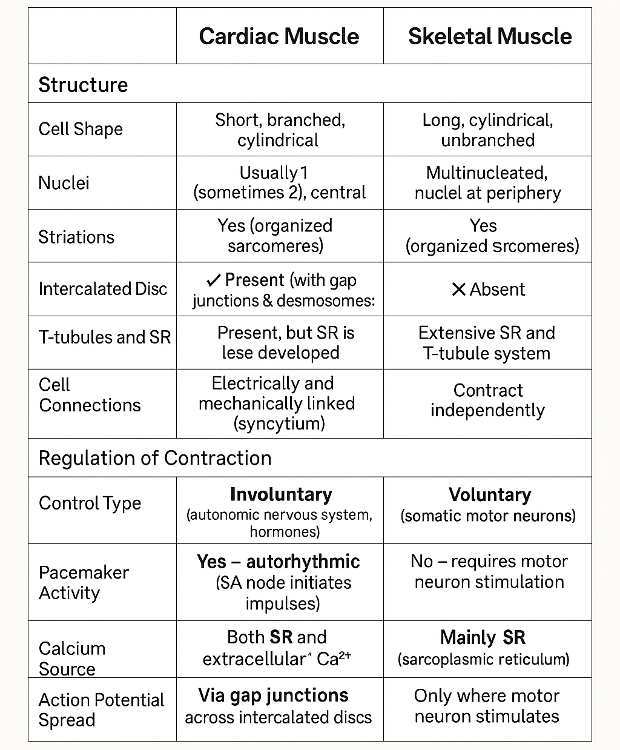
Refractory Period:
- Cardiac: Long (prevents tetanus)
- Skeletal: Short (allows summation and tetanus)
Contrast the structure of a smooth muscle cell with that of a skeletal muscle fiber and discuss the advantages of each type of structure.
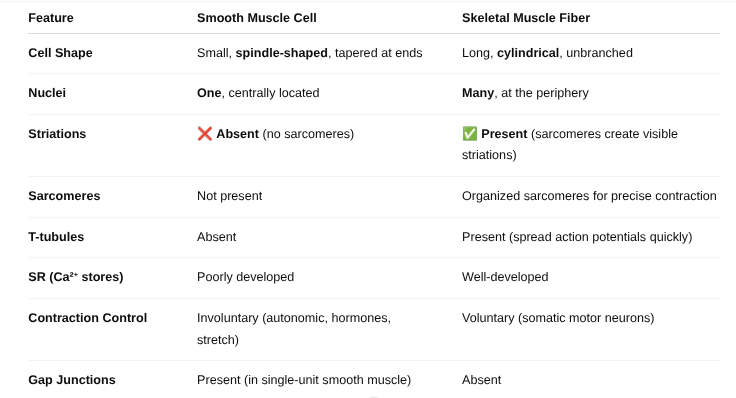
Advantages of Each Structure
Smooth Muscle (e.g., intestines, blood vessels):
- Efficient for long, sustained contractions (e.g., peristalsis, blood pressure control)
- Uses less energy than skeletal muscle
- Contracts in multiple directions due to lack of sarcomeres
- Can be stretched greatly and still contract (e.g., bladder, uterus)
- Self-regulating: Can contract in response to stretch or hormones without neural input
Skeletal Muscle (e.g., biceps, quads):
- Fast, powerful contractions due to organized sarcomeres
- Precisely controlled via motor neurons
- Multinucleation allows for high protein production and repair
- T-tubule system allows rapid electrical signal distribution for synchronized contraction
Distinguish between single-unit and multiunit smooth muscles.
Single-Unit Smooth Muscle (Visceral Smooth Muscle)
- Cell Coordination: Cells contract together as a unit
- Gap Junctions: Present → allow direct electrical communication
- Location: Walls of hollow organs (e.g., intestines, uterus, bladder, small blood vessels)
- Stimulation: Can contract spontaneously (myogenic); regulated by autonomic input, hormones, and stretch
- Function: Coordinated, wave-like contractions (peristalsis)
- Control: Involuntary, automatic
Multiunit Smooth Muscle
- Cell Coordination: Each cell contracts independently
- Gap Junctions: Absent or few → cells are not electrically connected
- Location: Found in precise-control areas (e.g., iris, ciliary muscle, large airways, large arteries, arrector pili)
- Stimulation: Requires individual nerve input (neurogenic)
- Function: Fine control and graded responses
- Control: Involuntary, but more neuron-dependent
Single-unit smooth muscle: Contracts as a team, ideal for moving contents through organs.
Multiunit smooth muscle: Acts like independent workers, giving precise control in specialized areas.
Describe the events by which depolarization of a smooth muscle cell results in contraction
1. Depolarization Begins
- Triggered by nerve signals, hormones, stretch, or spontaneous activity.
- Causes Ca²⁺ channels in the cell membrane to open.
2. Calcium Enters the Cell
- Extracellular Ca²⁺ enters through voltage-gated or ligand-gated calcium channels.
- Also, some Ca²⁺ may be released from the sarcoplasmic reticulum (SR).
3. Calcium Binds Calmodulin
Ca²⁺ binds to a regulatory protein called calmodulin (NOT troponin as in skeletal muscle).
4. Activates Myosin Light Chain Kinase (MLCK)
The Ca²⁺–calmodulin complex activates MLCK.
5. Myosin is Phosphorylated
MLCK phosphorylates myosin heads, allowing them to bind to actin.
6. Cross-Bridge Cycling
Myosin and actin interact → contraction occurs.
Smooth muscle contracts after Ca²⁺ activates MLCK via calmodulin, not troponin.
Explain why smooth muscle contractions are slow and sustained.
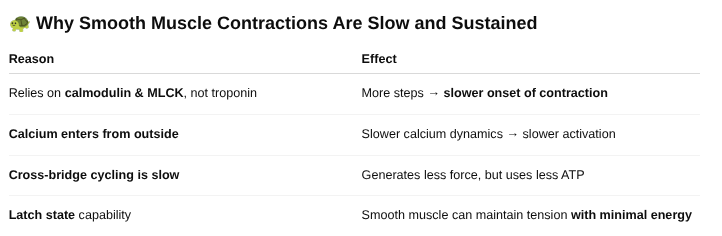
These contractions are slow to start, but sustained with minimal energy—perfect for roles like maintaining blood vessel tone or digestive movement.