Instructions for Side by Side Printing
- Print the notecards
- Fold each page in half along the solid vertical line
- Cut out the notecards by cutting along each horizontal dotted line
- Optional: Glue, tape or staple the ends of each notecard together
Wound Healing & Sutures, Chapter 11 (Nicola)
front 1 What is a abnormal attachment of two surfaces or structures that are normally separate | back 1 Adhesion |
front 2 What is the surgical removal of a foreign body or of tissue (cut out) | back 2 Excision |
front 3 What is surgical cut made in skin or flesh (cut in) | back 3 Incision |
front 4 What is a pathological, surgical, or traumatic formation of an opening between two normally separate organs or spaces | back 4 Anastomosis |
front 5 What is defined as returned to proximity; brought together sides or edges | back 5 approximated |
front 6 Classification for a wound that persists for an extended period of time | back 6 Chronic wounds |
front 7 Medical name for a scar | back 7 cicatrix |
front 8 What is a space that remains in the tissues as a result of failure of proper closure of a surgical wound | back 8 dead space |
front 9 What is the removal of devitalized tissue and contaminants | back 9 debridement |
front 10 What is a partial or total separation of a layer or layers of tissue after closure of the wound | back 10 Dehiscence |
front 11 What is an interruption of a closed wound or traumatic injury that exposes the viscera | back 11 Evisceration |
front 12 What is a type of healing that occurs with primary union that is typical of an incision opened under ideal conditions; healing occurs from side to side, dead space has been eliminated, and the wound edges are accurately approximated | back 12 first intention |
front 13 What is a type of needle in which the suture must be threaded by pulling the strand into a V-shaped area just above the eye | back 13 French-eyed needle |
front 14 What is defined as easily torn or crumbled | back 14 friable |
front 15 What is an abnormal protrusion of an organ or other body structure through an opening in a covering membrane or muscle | back 15 herniation |
front 16 A patient whose immune system has decreased due to disease, or intentionally decreased with immunosuppressive drugs for organ transplant patients to prevent organ rejection | back 16 immunosuppressed patient |
front 17 What is the body’s protective response to injury or tissue destruction | back 17 inflammation |
front 18 What is a cut or tear | back 18 laceration |
front 19 What is the placement of a suture tie around a vessel or other anatomical structure for the purpose of constriction (i.e., to control hemorrhage from a blood vessel) | back 19 ligated |
front 20 What is a suture that is manufactured from one strand of natural or synthetic material | back 20 monofilament |
front 21 What is sterile fine-mesh gauze that is loosely placed in a chronic wound or one that has been left open to heal by second intention | back 21 packing |
front 22 What is a main suture that approximates the wound edges for first intention healing to occur | back 22 primary suture line |
front 23 What is a versatile polymer used in a broad range of medical, industrial, and high technology applications | back 23 Polytetrafluoroethylene (PTFE) |
front 24 Which healing occurs when a wound fails to heal by primary union, or the wound is left open and allowed to heal from the inside to the outside by filling with granulation tissue | back 24 second intention |
front 25 What is a strand of suture material with an eyeless needle attached by the manufacturer; the needle is continuous with the suture strand | back 25 swaged |
front 26 What is the amount of pull or tension that a suture strand will withstand before breaking; expressed in pounds | back 26 tensile strength |
front 27 Which healing occurs when two granulated surfaces are approximated; also referred to as delayed primary closure | back 27 third intention |
front 28 What are thin strips made of silicone that can be placed around a vessel, nerve, or duct for the purposes of retracting or isolating; the loops are colored for easy identification of the retracted structures | back 28 vessel loops |
front 29 What is and accidental wound called | back 29 traumatic |
front 30 What is a surgical wound called | back 30 intentional |
front 31 What does ideal wound healing involve | back 31 restoration of continuity, strength, function, and appearance |
front 32 What word is described as any tissue that has been damaged by surgical or traumatic means. | back 32 The word wound |
front 33 Incision made under ideal surgical conditions; No break in sterile technique during procedure; Primary closure; No wound drain; No entry to aero digestive or genitourinary tract
| back 33 CLASS I-CLEAN-INFECTION RATE 1-5% |
front 34 Uninfected operative wound; respiratory, alimentary, genital, or urinary tract is entered under controlled circumstances without unusual contamination
| back 34 CLASS II-CLEAN CONTAMINATED-INFECTION RATE 8-11% |
front 35 Open traumatic wound (less than 4 hours old); Major break in sterile technique occurred; Acute inflammation present; Entry to aero digestive (includes billary tract) or genitourinary tract with spillage
| back 35 CLASS III-CONTAMINATED-INFECTION RATE 15-20% |
front 36 Open traumatic wound (more than 4 hours old); Microbial contamination prior to procedure; Perforated viscus, traumatic wounds with retained necrotic tissue
| back 36 CLASS IV-DIRTY/INFECTED-INFECTION RATE 27-40% |
front 37 When is the final wound classification assigned and is included in the intraoperative documentation | back 37 At the end of the procedure |
front 38 What are classified in several different ways according to severity. A single wound may fall into more that one category. | back 38 Traumatic wounds |
front 39 What is the name of the wound then the skin remains intact, but underlying tissues suffer damage | back 39 Closed wound |
front 40 What is the name of the wound when integrity of the skin is damaged. | back 40 Open wound
|
front 41 What is the name of the wound when integrity of the skin is compromised. There is no loss or destruction of tissue and there is no foreign body in the wound. | back 41 Simple wound |
front 42 What is the name of the wound when tissue is lost or destroyed, or a foreign body remains in the wound. | back 42 Complicated wound
|
front 43 What is the name of the wound when wound edges can be approximated and secured, and is expected to heal by first intention | back 43 Clean wound |
front 44 What is the name of the wound when a dirty object damages the integrity of the skin, infected within a short period of time. Debridement of infected and/or necrosed tissue may be necessary, followed by thorough irrigation of the wound to further clean and wash out the contaminants, a procedure commonly referred to as an irrigation and debridement (I and D). | back 44 Contaminated wound |
front 45 Define abrasion:
| back 45 Scrape |
front 46 Define contusion:
| back 46 Bruise |
front 47 Define Laceration:
| back 47 Cut or tear |
front 48 Define Puncture:
| back 48 Penetration |
front 49 What are the classic signs of an inflammatory process = body’s protective response to injury or tissue destruction | back 49 1. pain (dolar)
|
front 50 Define Thermal:
| back 50 Heat or cold (can be chemical) |
front 51 What occurs when injured tissues release histamine from the damaged cells. The histamine causes the small blood vessels in the area to dilate, increasing the blood flow to the area, resulting in heat, redness, and swelling. | back 51 An inflammatory reaction |
front 52 First intention
| back 52 Primary union |
front 53 Second intention
| back 53 Granulation |
front 54 Third intention
| back 54 Delayed primary closure |
front 55 Which healing occurs with an incision that was opened under ideal conditions. Healing occurs from side to side in a sterile wound in which dead space has been eliminated and the wound edges have been accurately approximated. Wound tensile strength at third month 78-80% after suturing. | back 55 First intention healing
|
front 56 What are the 3 distinct phases of first intention healing | back 56 (A) Phase 1, inflammatory response and debridement process
|
front 57 What are the 3 distinct phases of first intention healing | back 57 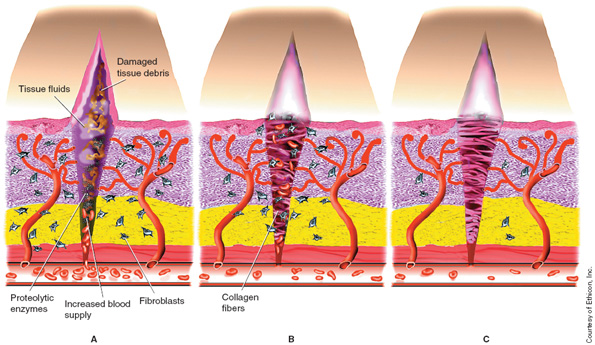 |
front 58 • This stage begins within minutes of injury and lasts approximately 3–5 days.
| back 58 Phase 1: Lag Phase or Inflammatory Response Phase |
front 59 • This stage begins around the 3rd postoperative day for up to 20 days.
| back 59 Phase 2: Proliferation Phase |
front 60 • This stage begins on the l4th postoperative day, until the wound is completely healed (up to l2 months).
| back 60 Phase 3: Maturation or Differentiation Phase |
front 61 Heals from the outside in. Packaging material used following the removal of necrotic tissue or after a wide debridement. The wound is left open and the tissue starts to "granulate" this contains myofibroblasts forms in the wound, causing closure by contraction. | back 61 Second Intention (Granulation)
|
front 62 Excessive granulation tissue, sometimes referred to as ............ may protrude above the defect margins and block re-epithelialization. | back 62 “proud flesh,”
|
front 63 What will occur if a weak union and a wide, irregular scar is left at the wound site | back 63 Herniation |
front 64 • This stage occurs when two granulated surfaces are approximated.
| back 64 Third Intention (Delayed Primary Closure) |
front 65 What is one of the factors influencing wound healing that include:
| back 65 First consideration is the physical condition of the patient
|
front 66 What is one of the factors influencing wound healing that include:
| back 66 First consideration is the physical condition of the patient
|
front 67 What is one of the factors influencing wound healing that include:
| back 67 Second consideration is intraoperative tissue handling
|
front 68 What is one of the factors influencing wound healing that include:
| back 68 Third consideration is the application of the principles of asepsis through the use of sterile technique
|
front 69 What frequently occurs between the 5th and 10th postoperative day and is seen most often in debilitated patients with friable (easily torn) tissue. "Popping sensation" | back 69 Dehiscence
|
front 70 What is a rare but severe surgical complication where the surgical incision opens (dehiscence) and the abdominal organs then protrude or come out of the incision | back 70 Evisceration |
front 71 What may be concealed or evident and occurs most frequently in the first few postoperative hours. and can result in postoperative shock. Surgery is frequently required to achieve hemostasis. | back 71 Hemorrhage |
front 72 What occurs in the wound when microbial contamination overrides the resistance of the host. It results in increased morbidity and mortality. In addition to antibiotic therapy, additional surgery may be required as part of the treatment regimen | back 72 Infection |
front 73 What is an abnormal attachment of two surfaces or structures that are normally separate. Fibrous tissue can develop within the peritoneal cavity because of previous surgery, infection, improper tissue handling, or the presence of a foreign body The fibrous tissue that develops can cause abnormal attachments of the abdominal viscera that may cause pain and/or bowel obstruction. | back 73 adhesion |
front 74 What is a result of wound dehiscence and occurs most often in lower abdominal incisions, and is discovered 2–3 months postoperatively and could result in bowel incarceration. Surgery may be required to correct this condition. | back 74 Herniation |
front 75 What is an abnormal tract between two epithelium-lined surfaces that is open at BOTH ends. It occurs most often after bladder, bowel, and pelvic procedures. Abnormal drainage is a prevalent sign. Surgery is required for correction. | back 75 Fistula |
front 76 What is an abnormal tract between two epithelium-lined surfaces that is open at ONE END only. Its occurrence is highest in bladder, bowel, and pelvic procedures. Abnormal drainage is a common sign. Surgery is often required to correct this condition. | back 76 Sinus tract |
front 77 What can occur because of either a failure to properly absorb the material or an irritation caused by the material that results in inflammation. It occurs most frequently with silk and is characterized by an evisceration (referred to as “spitting”) of the material from the wound or sinus tract formation. | back 77 Suture complications |
front 78 What formation is a hypertrophic scar formation and occurs most frequently in dark-skinned individuals. Corticoid injections and use of pressure dressings can help reduce the size of the scar, but plastic surgery may be required for correction. | back 78 Keloid scar |
front 79 What is the separation of wound layers that have not been closely approximated or air that has become trapped between tissue layers. The space may allow for serum or blood to collect and provide a medium for microbial growth, resulting in a wound infection. It is eliminated by use of proper suturing techniques, wound drains, and/or pressure dressings. | back 79 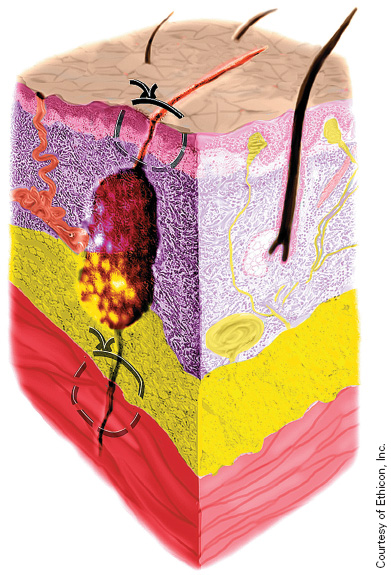 Dead space |
front 80 What is the prevention of infection and other complications, it may include the use of drains and protection of the wound with different types of dressings. | back 80 Postoperative wound care |
front 81 When are the skin and subcutaneous tissues generally left open and packed loosely with fine mesh gauze, such as Iodoform. Packaging is removed after 4–5 days and, if no infection is present, the wound may be closed at that time | back 81 With a contaminated wound |
front 82 Which suture is digested by the body enzymes that attack the suture strand, eventually destroying it | back 82 Natural - Absorbable |
front 83 Which suture is hydrolyzed by the body | back 83 Synthetic - Absorbable |
front 84 What is capable of being absorbed by tissue within a given period of time, | back 84 Absorbable suture
|
front 85 What resists enzymatic digestion or absorption by tissue | back 85 Nonabsorbable suture
|
front 86 What is made of a single thread-like structure | back 86 Monofilament suture
|
front 87 What consists of multiple thread-like structures braided or twisted into a single strand.
| back 87 Multifilament suture
|
front 88 What are relatively inert and do not readily harbor bacteria, and glide through tissues more easily resulting in minimal tissue damage because they encounter little resistance within the tissue.
| back 88 Monofilament suture
|
front 89 What exhibit a characteristic called capillarity "to harbor bacteria, retain tissue fluids that can be communicated along the length of the strand". Great tensile, pliability, knots securely.
| back 89 Multifilament suture
|
front 90 What are digested by body enzymes that attack the suture strand, eventually destroying it. | back 90 Natural absorbable sutures |
front 91 What are hydrolyzed by the body. Water within the tissue penetrates the strand and breaks down the their fiber’s polymer chain, resulting in minimal tissue reaction | back 91 Synthetic absorbable sutures |
front 92 What is referred to as the suture diameter | back 92 gauge of the suture |
front 93 Who specifies diameter range for suture materials | back 93 The United States Pharmacopeia (USP) |
front 94 The diameter of stainless steel sutures is identified by the ................commercial wire gauge numbers | back 94 Brown and Sharpe (B and S) |
front 95 Modern sutures range from #5 heavy braided suture for orthopedics to #11-0 fine monofilament suture for ophthalmics. As the number of 0’s increase, the smaller the diameter | back 95 Suture sizes |
front 96 What are the most commonly used suture sizes | back 96 USP suture sizes #1 through 4-0 |
front 97 What sutures are used frequently for closure of orthopedic wounds and abdominal fascia | back 97 Suture sizes #1 and #0 |
front 98 What sutures are typically used for aortic anastomosis | back 98 Suture sizes 4-0 and 5-0 |
front 99 What suture are used for smaller vessel anastomoses, such as those on the coronary or carotid arteries | back 99 Suture sizes 6-0 through 7-0 |
front 100 What sutures are used for microvascular and eye procedures | back 100 Suture sizes 8-0 through 11-0 |
front 101 What sutures are used to close dural incisions | back 101 Suture sizes 4-0 sutures |
front 102 What sutures are used for most sub-cuticular skin closures | back 102 Suture sizes 3-0 and 4-0 |
front 103 What are the suture lengths ranges available | back 103 Suture lengths 5 in. to 59 in |
front 104 Which sutures are used where continued strength is necessary, for instance, to close abnormal openings in the heart, typically used to close dura over the brain, used to close fascia and skin closure, silk commonly used for ligating vessels | back 104 Nonabsorbable sutures |
front 105 Which sutures are often the 1st choice for tissue that does not need continued support. Often used for subcutaneous tissue and the mucosal layer of the intestine | back 105 Absorbable sutures |
front 106 What important factor determines suture choice | back 106 Knot tensile strength. |
front 107 What is measured by the force in pounds that the suture strand can withstand before it breaks | back 107 Knot tensile strength |
front 108 What could be a factor when choosing a suture: Fascia and skin are strong but heal slowly, Gastrointestinal tissue is relatively weak but heals quickly | back 108 General Factors Affecting Choice of Suture |
front 109 What could be a factor when choosing a suture:
| back 109 General Factors Affecting Choice of Suture |
front 110 What are some individual disease processes affecting suture choice that ST should be aware of:
| back 110 Conditions for suture choice ST needs to be aware of that plain gut and other sutures can not be used on: |
front 111 What has these characteristics: configuration, capillarity, ability to absorb fluid, size (diameter), tensile strength, knot strength, elasticity, and memory. | back 111 Suture materials |
front 112 What is the most important information that the surgical technologist should learn to look for on a suture box | back 112 Suture size
|
front 113 What information does the suture packet identify | back 113 Product code
|
front 114 What also referred to as controlled release (CR), are designed to “pop off” the suture strand after a single suture has been placed. | back 114 Rapid release needles |
front 115 What are used to occlude vessels for hemorrhage control or for organ or extremity removal | back 115 Ligatures or ties |
front 116 What is removed as single strands from the package and placed into the open hand of the surgeon
| back 116  Free tie |
front 117 What are used to occlude large vessels to prevent slippage. The suture is placed through the center of a large vessel after a hemostat is placed | back 117 Suture ligature
|
front 118 What are used to occlude superficial bleeders, typically chromic, plain, or polyglactin 910 sutures | back 118 Ligature reel |
front 119 What are used to occlude deep bleeding vessels | back 119 Instrument Tie (Tie-on-a-Pass) |
front 120 What are best practices for suture use | back 120 Only open what is needed
|
front 121 Ligature reels should be removed from their packets and placed onto the .......with the strand end extended slightly. | back 121 Mayo stand |
front 122 Free-ties should be opened at the end of the packet and placed on the ........ with the suture strands protruding for easy access. | back 122 Mayo stand |
front 123 (A) Needle holder is clamped onto the needle approximately one-third the distance from the swage.
| back 123 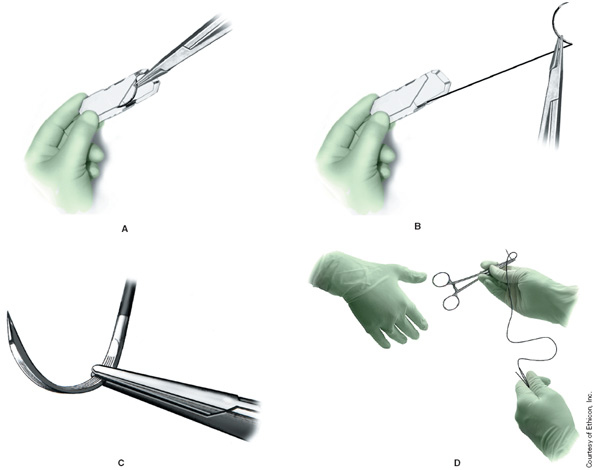 Loading the suture: |