Instructions for Side by Side Printing
- Print the notecards
- Fold each page in half along the solid vertical line
- Cut out the notecards by cutting along each horizontal dotted line
- Optional: Glue, tape or staple the ends of each notecard together
Vascular 1
front 1 Where does the CCA bifurcate? | back 1 at the level of the superior thyroid cartilage |
front 2 What is the first branch of the subclavian artery? | back 2 vertebral |
front 3 What does systemic system on each side of the neck imply? | back 3 waveform should be the same on each side. |
front 4 What is the function of the extracranial cerebrovascular system function? | back 4 Supply blood flow to cerebral hemispheres eyes face muscles forehead scalp |
front 5 Where does the vertebrals supply blood to? | back 5
|
front 6 Where does the carotid artery supply blood to? | back 6
|
front 7 Name the branches of the aortic arch | back 7
|
front 8 Where does the ECA supply blood to? | back 8 face neck scalp |
front 9 Name the branches of the ECA. | back 9
|
front 10 Name the 4 divisions of the ICA. | back 10
|
front 11 Explain the location of the ICA compared to the ECA. | back 11 posterior and lateral |
front 12 What type of flow is expected in the bulb of the carotid? | back 12 turbulent |
front 13 What is the flow of the vertebral arteries? | back 13 Posterior circulation
|
front 14 What do the two vertebrals form? | back 14 Basilar artery |
front 15 What is the diameter of the CCA? | back 15 5-6 mm |
front 16 What is the diameter of the ICA? | back 16 4-5 mm |
front 17 What is the diameter of the ECA? | back 17 3-4 mm |
front 18 What is the diameter of the vertebral artery? | back 18 2-3 mm |
front 19 How much of the carotid's blood enters the brain via the ICA? | back 19 80% |
front 20 How much of the carotid's blood supplies the face and neck via the ECA? | back 20 20% |
front 21 Explain the waveform of the CCA | back 21 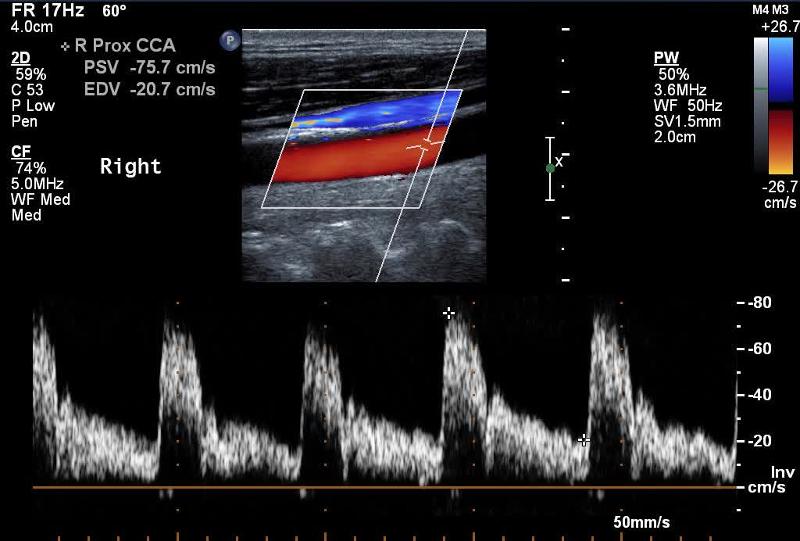 Mimics both ICA and ECA waveforms |
front 22 Explain the waveform of the ICA | back 22 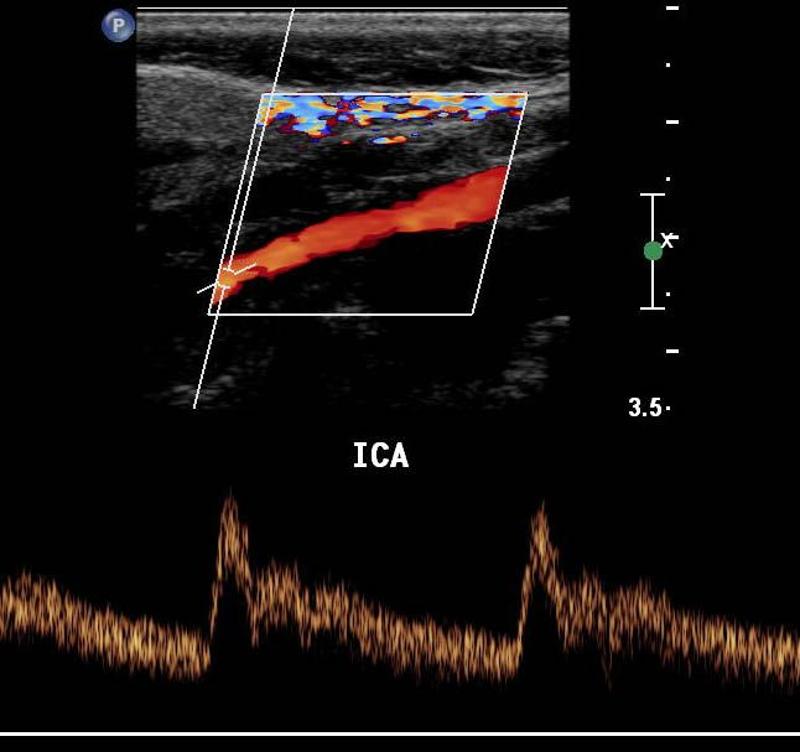 low resistant - constant forward flow Forward flow throughout the cardiac cycle |
front 23 Explain the waveform of the ECA | back 23 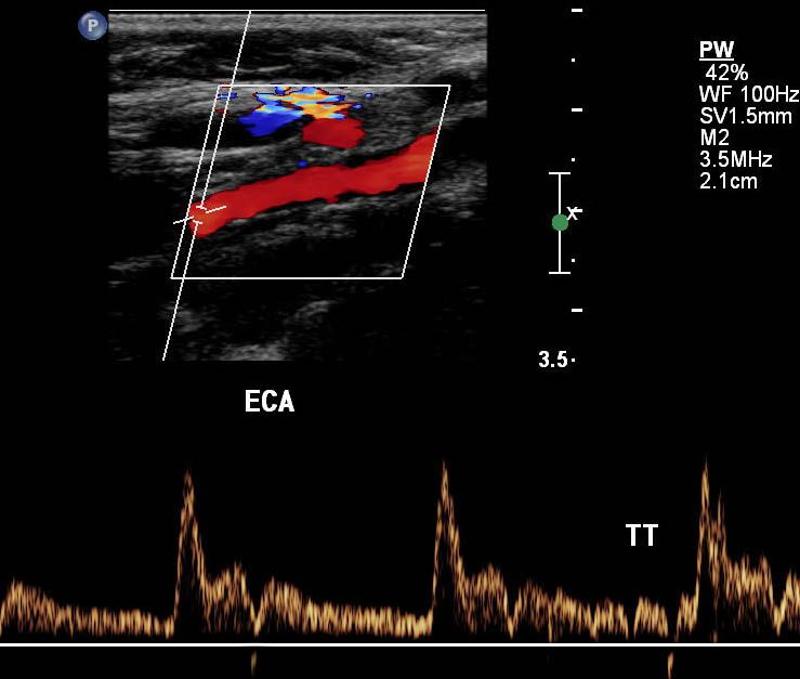 high resistant steep forward stroke Forward flow during systole, low or reverse diastolic component |
front 24 Explain the waveform of the vertebral artery | back 24 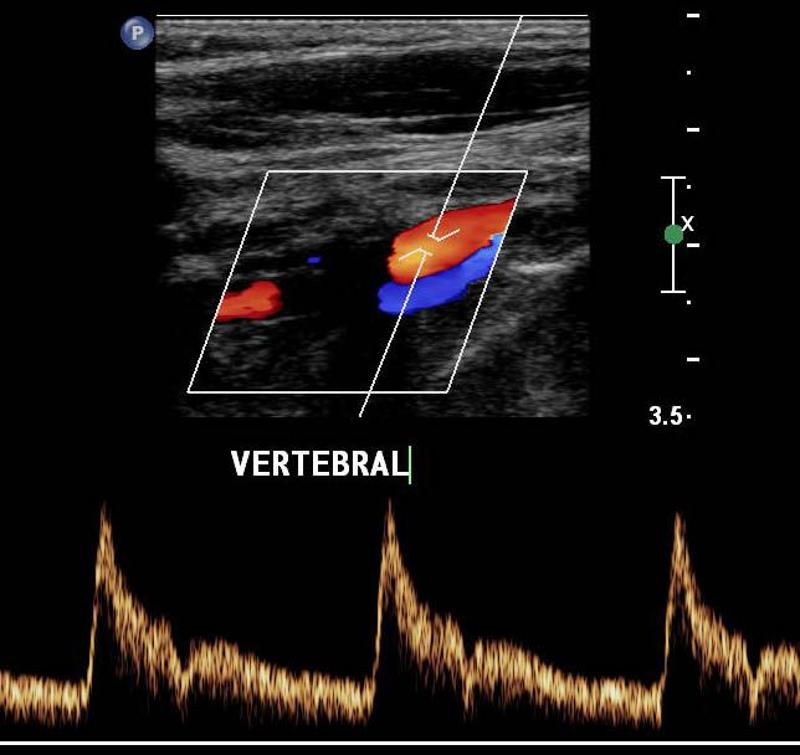 low resistant |
front 25 What is resistance determined by? | back 25 diastole less diastole = high resistance |
front 26 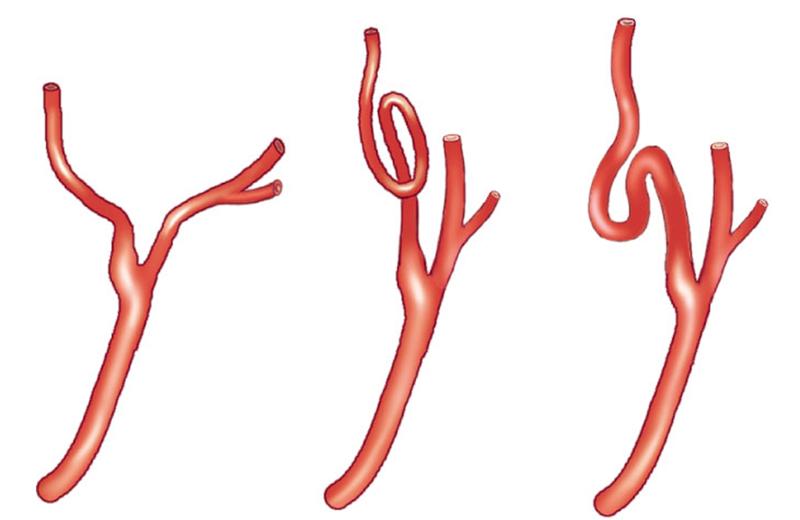 What causes tortuous vessels? | back 26 can be born this way can happen over time as people age they shrink *elevation can result but state that vessel was tortuous |
front 27  Which is the left CCA? | back 27 right |
front 28 On what side is the notch in long? | back 28 superior |
front 29 On what side is the notch in transverse? | back 29 patient right |
front 30 Where is the notch when imaging the right cerebrovascular system in transverse, | back 30 posterior |
front 31 When imaging the left cerebrovascular system in transverse, where will the notch be? | back 31 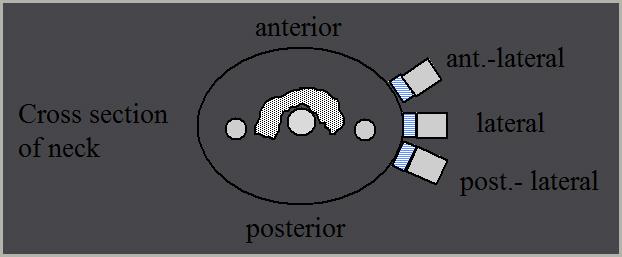 anterior |
front 32 How should plaque be measured? | back 32 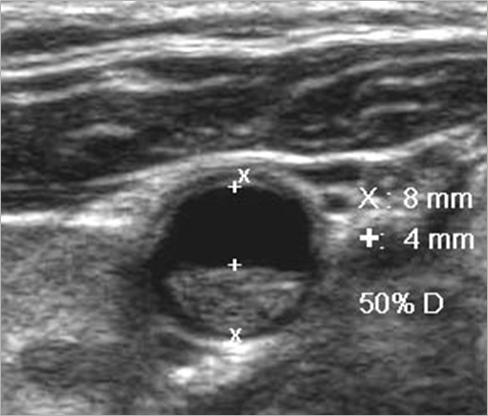 transverse measurement lumen vs true lumen |
front 33 Why is plaque measured in transverse? | back 33 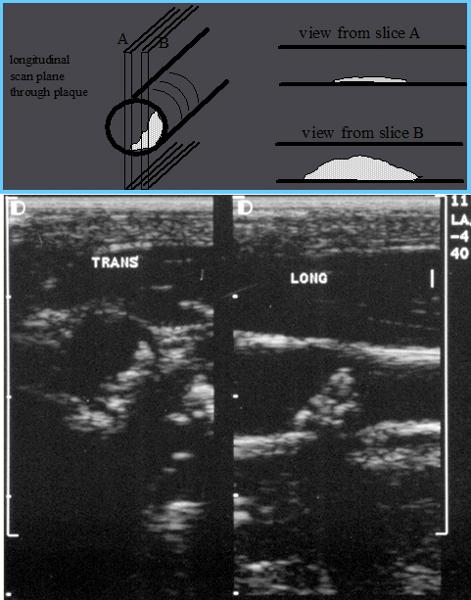 Longitudinal estimation of stenosis from B-mode image is usually unreliable, use transverse image. *This minor plaque can be made to appear more or less stenotic in longitudinal view |
front 34 Plaque Morphology | back 34 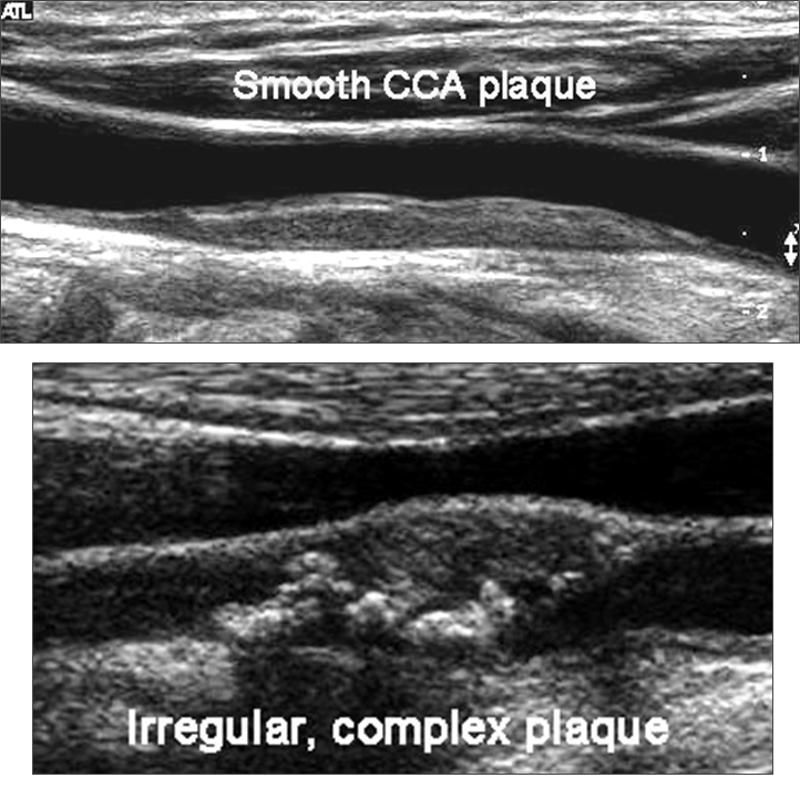 |
front 35 How do you tell the difference between the ICA and ECA? | back 35
|
front 36 ICA lies _________ in the neck (95%) | back 36 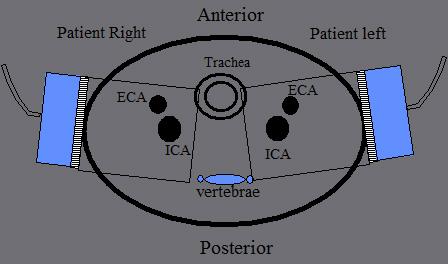 ICA lies posterior in the neck (95%) |
front 37 ECA position, whether lateral, anterior or medial, is _________. | back 37 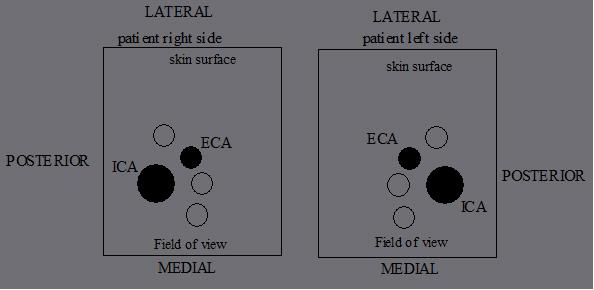 ECA position, whether lateral, anterior or medial, is variable |
front 38  | back 38 no data |
front 39 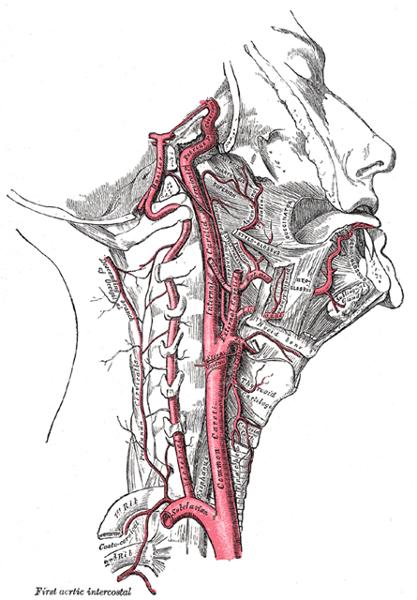 | back 39 no data |
front 40  | back 40 no data |
front 41 What are the four sets of the ECA branches? | back 41 Anterior Posterior Ascending terminal |
front 42 What are the anterior branches of the ECA? | back 42
|
front 43 What are the posterior branches of the ECA? | back 43
|
front 44 What are the ascending branches of the ECA? | back 44 Ascending Pharyngeal |
front 45 What are the terminal branches of the ECA? | back 45
|
front 46 What is Plaque? | back 46 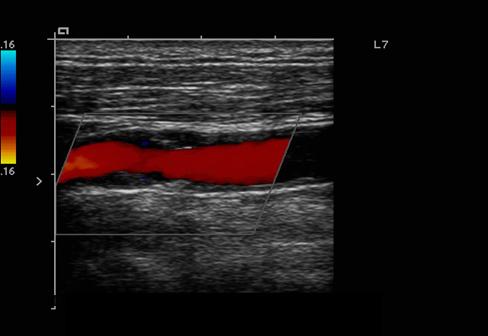 Atherosclerotic material that builds up on the walls of arteries
|
front 47 What is a lumen? | back 47 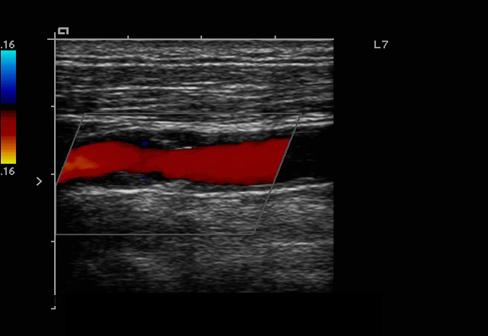 The flow space within a vessel |
front 48 What is residual lumen? | back 48 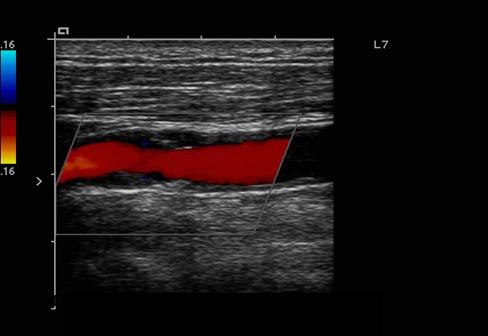 amount of flow space after accounting for the plaque |
front 49 What is a Bifurcation? | back 49 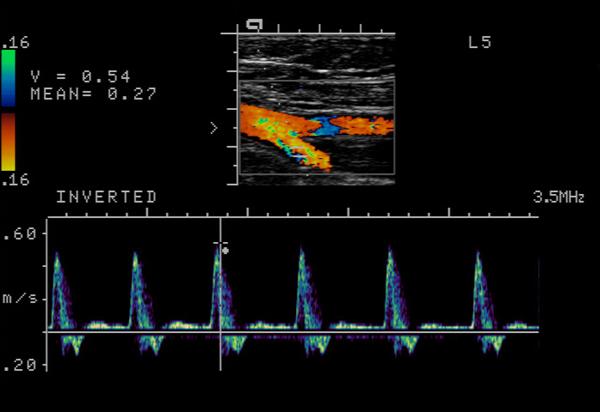 The point of vessel division
|
front 50 What are Collateral Circulation? | back 50
|
front 51 What is an Embolus? | back 51 An object traveling through the circulation that can cause occlusion |
front 52 What are the different types of an Embolus? | back 52 air tumor fat bullets foam clot |
front 53 What is hemodynamics? | back 53 blood flow characteristics |
front 54 What is the Doppler angle? | back 54 The angle of the Doppler beam with respect to the angle of blood flow Angle of Incidence Angle theta q |
front 55 What is the best Doppler angle? | back 55 0 o |
front 56 What is the Optimal Doppler angle? | back 56 45o to 60o |
front 57 What is the worst Doppler angle? | back 57 90o |
front 58 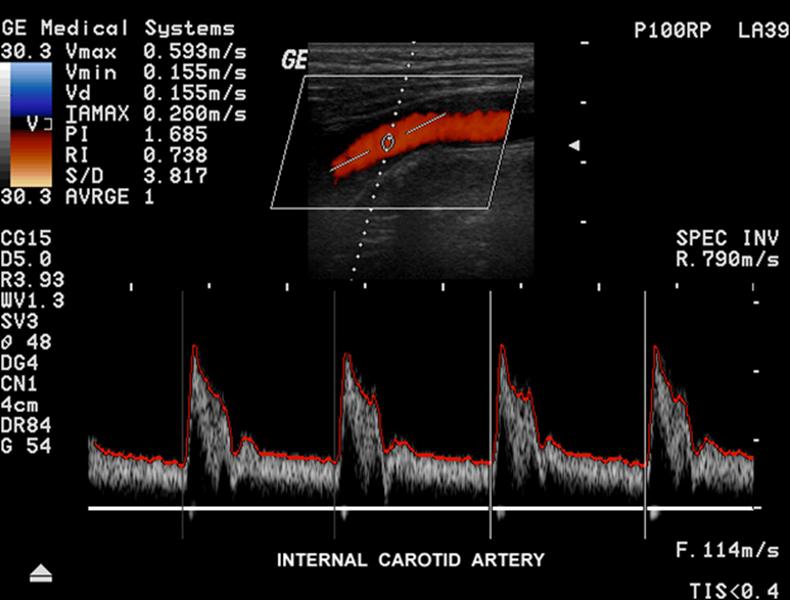 | back 58 no data |
front 59 Explain angle correct? | back 59 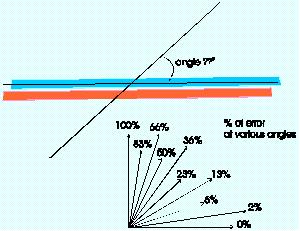 Visually adding a correction factor to the Doppler angle so that correct velocities can be calculated |
front 60 What is Spectral Analysis? | back 60 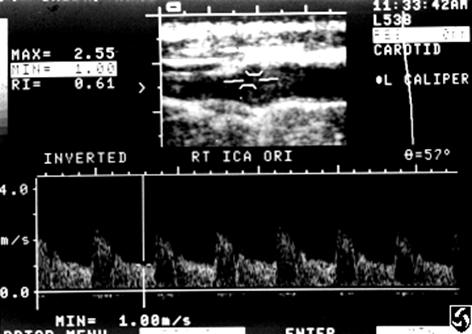
|
front 61 Explain velocity? | back 61
|
front 62 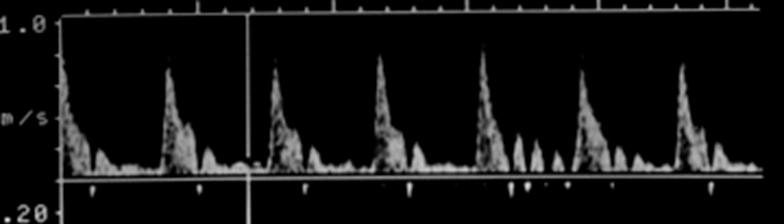 Where is peak systole? | back 62  The highest point on the wave form |
front 63  Where is end diastole? | back 63 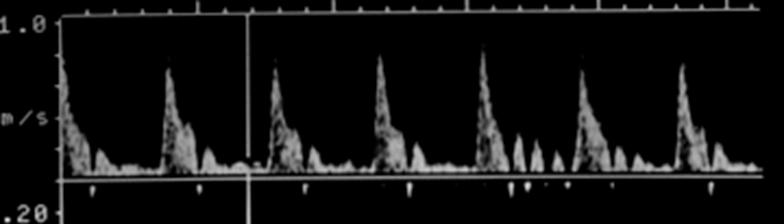 The point just prior to the systolic upstroke |
front 64 Beam Steering | back 64 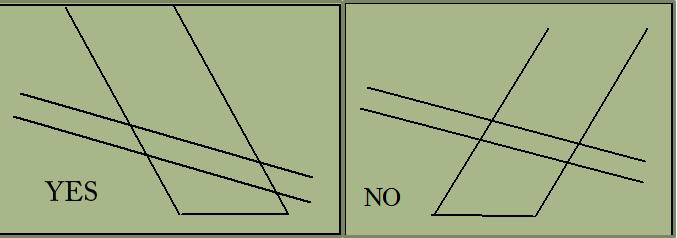 |
front 65 Depth penetration may be improved by _____________________ . | back 65 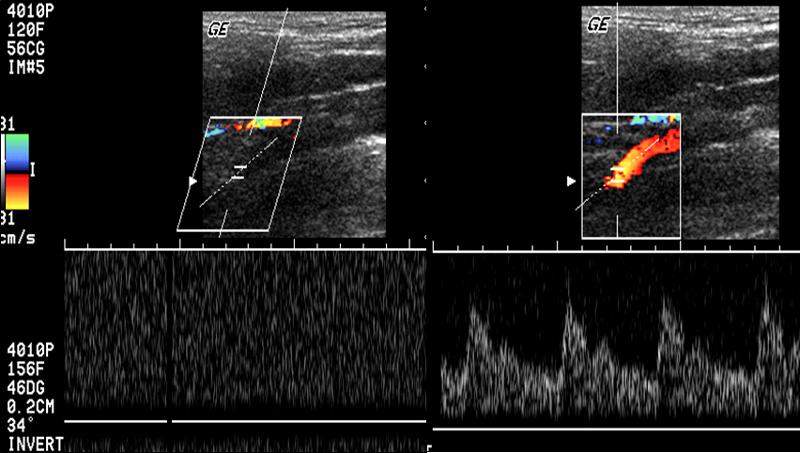 Depth penetration may be improved by not steering the Doppler |
front 66 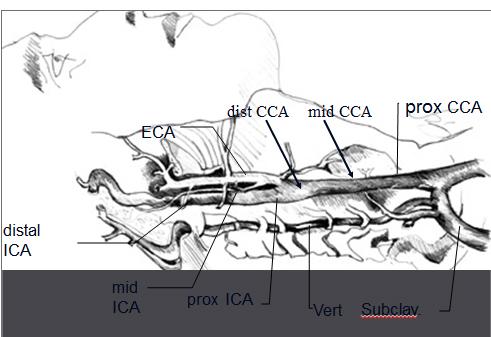 | back 66 no data |
front 67 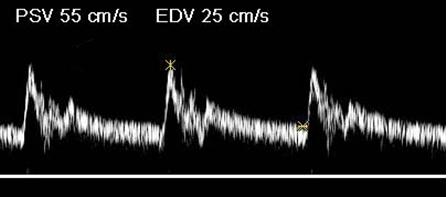 Where is the waveform? | back 67 ICA |
front 68 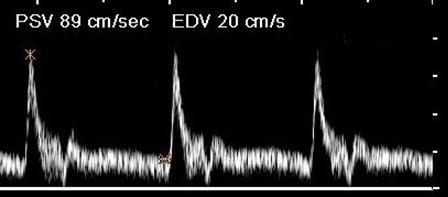 Where is the waveform? | back 68 CCA |
front 69 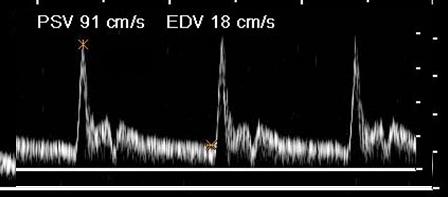 Where is the waveform? | back 69 ECA |
front 70 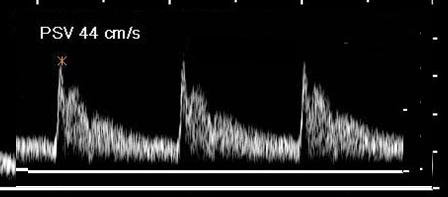 Where is the waveform? | back 70 vertebral |
front 71 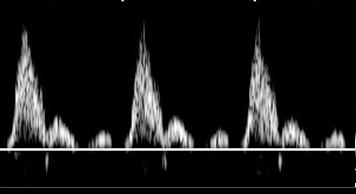 Where is the waveform? | back 71 subclavian |
front 72 Hypoechoic / Anechoic | back 72 Dark or black areas on the image caused by objects with little or no reflectivity |
front 73 Echodense/ Echogenic | back 73 Bright areas on the image caused by highly reflective material |
front 74 Distal / Proximal Limits | back 74 The farthest and closest region that can be visualized |
front 75 Plaque | back 75 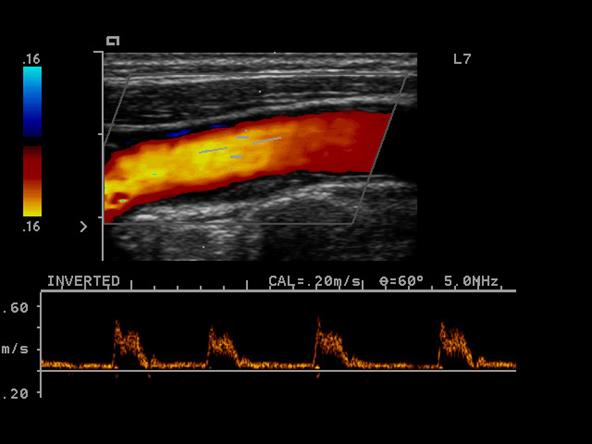 A swollen area of the lining of an artery formed by the deposition of lipids |
front 76 Calcific Plaque | back 76 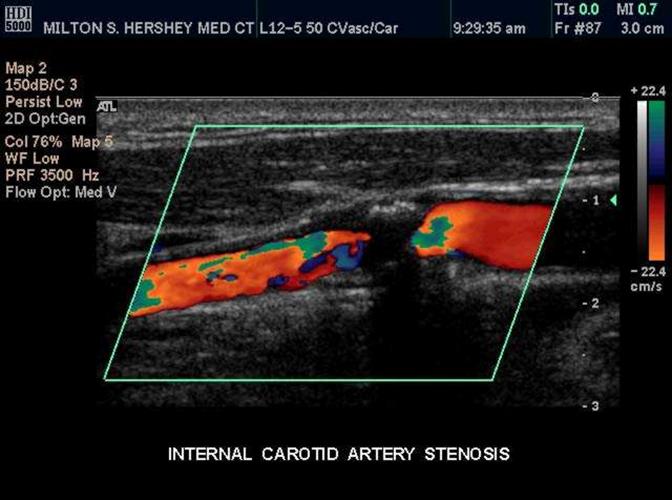 Bright echogenic plaque which creates shadowing |
front 77 Dense Plaque | back 77 Bright echogenic plaque which does not produce shadowing |
front 78 Soft / Fibrous Plaque or Thrombus | back 78  Plaque which produces echoes (not hypoechoic) but not as bright as dense or calcific plaque |
front 79 Intimal thickening or Fatty streak | back 79 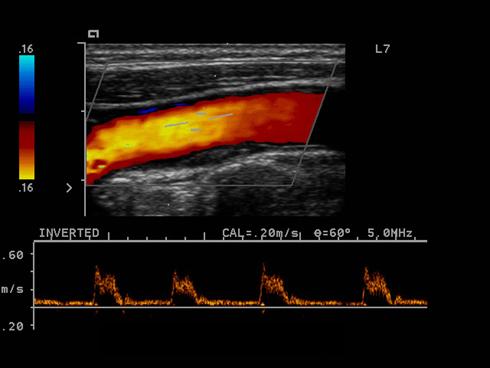 Plaque that is along the wall of the vessel as a minimal amount |
front 80 What is minimal degree of plaque? | back 80 10% |
front 81 What is moderate degree of plaque? | back 81 60% |
front 82 What is severe degree of plaque? | back 82 90% |
front 83 What is Circumferential plaque? | back 83 Plaque along the entire lumen - all the way around |
front 84 What is extensive plaque? | back 84 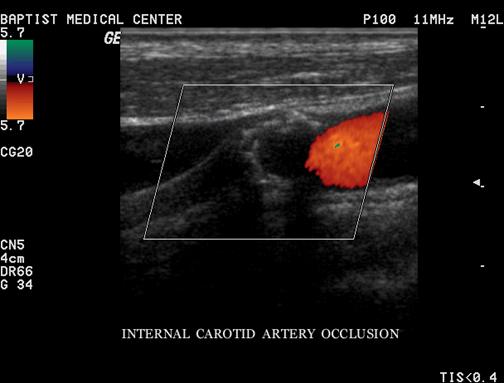 Plaque along a lengthy segment of the artery |
front 85 What is scattered plaque? | back 85 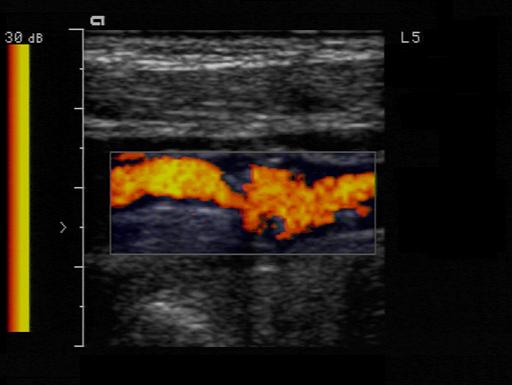 Plaque found at several locations which are not connected |
front 86 True Lumen | back 86 True Lumen is the original internal diameter of the vessel |
front 87 Residual Lumen | back 87 Residual Lumen is the current internal diameter of the vessel
|
front 88 Homogenous plaque | back 88 less likely to ulcerate
|
front 89 Heterogeneous plaque | back 89 more likely to ulcerate
|
front 90 Smooth vs Irregular plaque | back 90 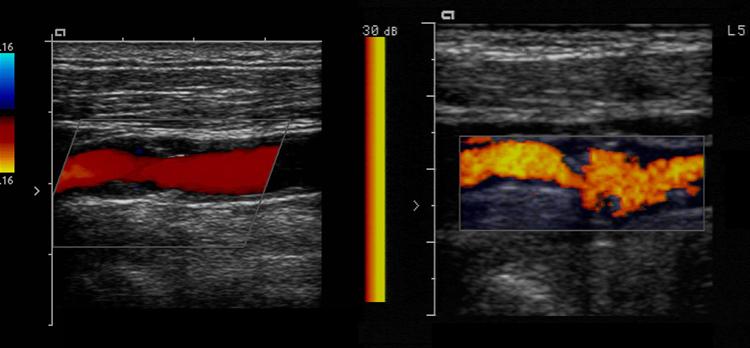
|
front 91 Ulcerative Plaque | back 91 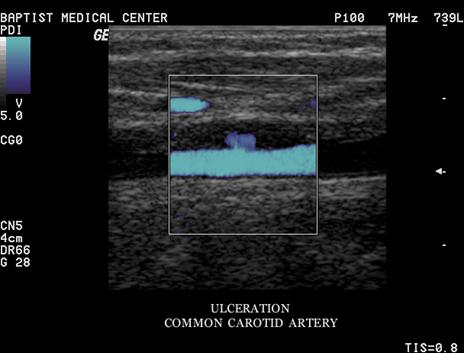 A scooped out appearance shelf like projections |
front 92 Occlusion | back 92 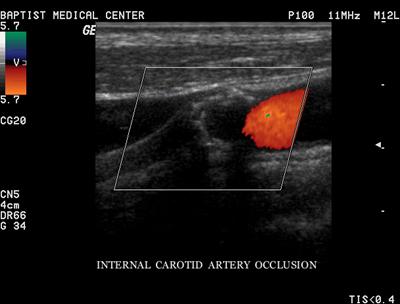 Complete blockage
|
front 93 What must one do in calling an occlusion | back 93 sensitize the equipment before doing so Decrease PRF Increase color gain, use power Doppler |
front 94 laminar flow | back 94 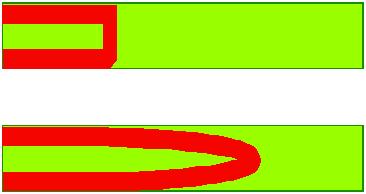 Orderly non-turbulent |
front 95 Sharp flow | back 95 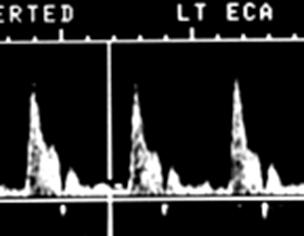 Indicating a swift upstroke Sharp peaks |
front 96 Damped flow | back 96 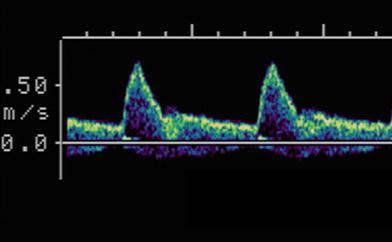 Slow upstroke Rounded Peaks |
front 97 Monophasic | back 97 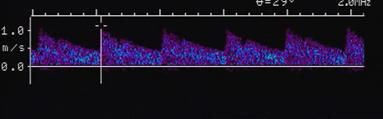 One upstroke within one cardiac cycle |
front 98 Multiphasic | back 98 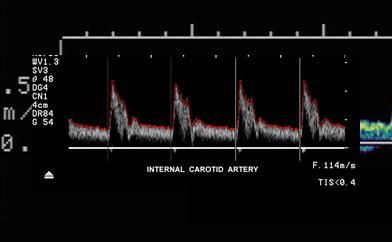 Multiple upstrokes within one cardiac cycle |
front 99 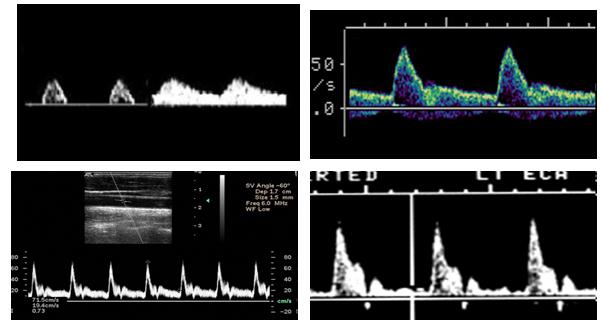 Which is monophasic? | back 99 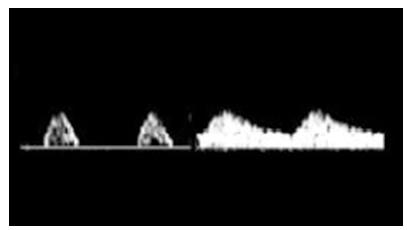 |
front 100 Antegrade | back 100 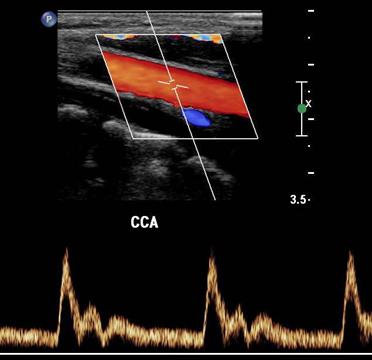 Flow in the direction that is expected from that specific vessel |
front 101 Retrograde | back 101 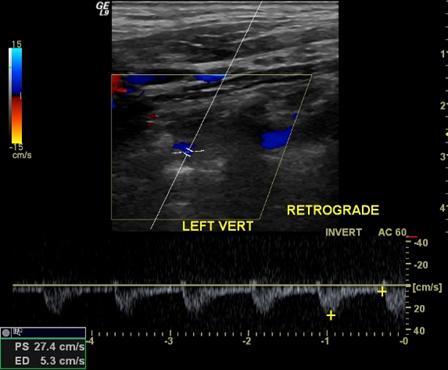 Flow that is reversed from the expected direction for that vessel |
front 102 Characterization of flow disturbances | back 102 Turbulence Spectral Broadening Disturbed flow Window Filling Gross Turbulence |
front 103 Aliasing | back 103 A Spectral Doppler Artifact of Pulsed Doppler systems Spectral Doppler displays the peaks wrapped in the reverse direction Color Doppler displays as a reversed color |
front 104 Mosaic | back 104 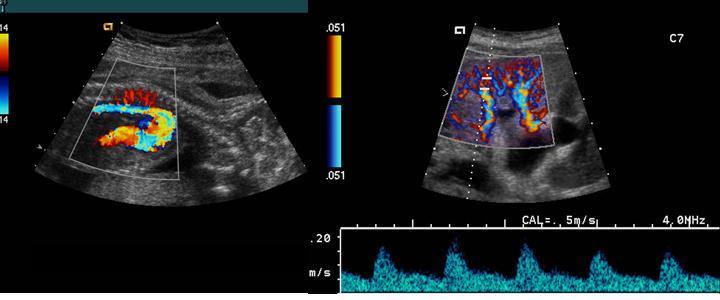 A mottled appearance caused by turbulent flow |
front 105 Jet | back 105 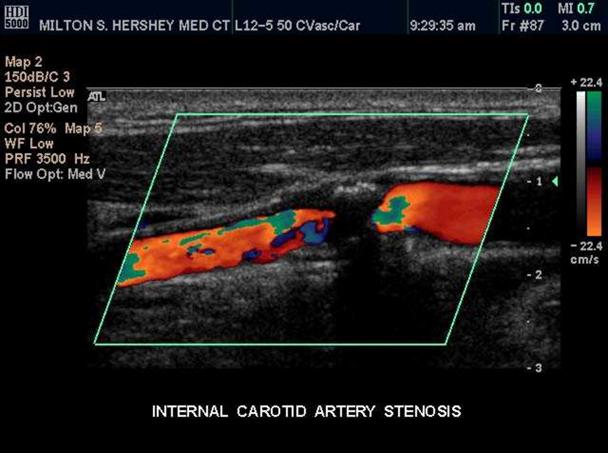 A localized area of higher flow through and after an area high grade stenosis |
front 106 Diploplia | back 106 double vision |
front 107 Drop attack | back 107 falling to the ground without other symptoms |
front 108 Syncope | back 108 transient loss of consciousness |
front 109 Bruits | back 109 abnormal flow sounds caused by turbulent patterns |
front 110 Subclavian steal | back 110 abnormal flow direction into the subclavian from the vertebral artery caused by stenosis of the subclavian
|
front 111 What side does subclavian steal syndrome usually occur? | back 111 left |
front 112 Amaurosis fugax | back 112 temporary partial or total blindness |
front 113 Homonymous hemianopia | back 113 Blindness in the outer half of the visual field |
front 114 Vertigo | back 114 difficulty in maintaining equilibrium movement that is not real |
front 115 Ataxia | back 115 inability to control gait or touch an article |
front 116 Paresis | back 116 weakness or slight paralysis on one side of the body |
front 117 Paresthesia | back 117 numbness or lack of feeling |
front 118 Dysphasia | back 118 impaired speech |
front 119 Aphasia | back 119 inability to speak |
front 120 What is a Carotid body tumor? | back 120 A small mass of vascular tissue that adjoins the carotid sinus. It functions as a chemoreceptor sensitive to changes in oxygen tension of the blood and signals necessary changes in respiratory activity |
front 121 Nonatherosclerotic lesions | back 121 Trauma Fibromuscular Dysplasia (FMD)
Collagen vascular connective tissue disorders |
front 122 Where does a Nonatherosclerotic lesions usually occur? | back 122 mid to distal renal or carotid |
front 123 What are the Mechanisms of disease? | back 123
|
front 124 What are the Risk Factors & | back 124
|
front 125 What is a Cerebrovascular Accident (CVA)? | back 125 Produces a permanent neurological deficit |
front 126 What is an acute CVA? | back 126 symptoms of sudden onset unstable |
front 127 What is a Stroke in evolution? | back 127 symptoms come and go unstable |
front 128 What is a Completed stroke? | back 128 No progression or resolution of the symptoms stable |
front 129 What are the symptoms of Vertebrobasilar Insufficiency? | back 129
|
front 130 What is a Reversible Ischemic Neurologic Deficit (RIND)? | back 130
|
front 131 What is a TIA? | back 131 Transient Ischemic Attack - TIA A fleeting neurological dysfunction without lasting effects |
front 132 What are the symptoms of a TIA? | back 132 last minutes - hours never more than 24 hours sensory, motor, speech impairment, monocular visual disturbance |
front 133 What is the Etiology of a TIA? | back 133 heart or carotid artery emboli |
front 134 What is NASCET? | back 134 North American Symptomatic Carotid Endarterectomy Trial |
front 135 What is ECET? | back 135 European Carotid Endarterectomy Trial (ECET) |
front 136 What is ACAS? | back 136 Asymptomatic Carotid Atherosclerosis Trial (ACAS) |
front 137 What was the endpoint for all 3 Carotid Endarterectomy Trials? | back 137 Reduction of hemispheric stroke & death |
front 138 In the Carotid Endarterectomy Trials what showed long term benefits? | back 138 surgery in pt’s with >60 – 70% stenosis for both symptomatic & asymptomatic over medical treatment |
front 139 What are the key points of spectral broadening? | back 139
|
front 140 What can we expect from post stenotic flow? | back 140 turbulent – nonlaminar
|
front 141 What Factors cause abnormal Low PSV? | back 141
|
front 142 What Factors cause abnormal High PSV? | back 142 Hypertension |
front 143 Why do we calculate Systolic Velocity Ratio? | back 143
|
front 144 Why do we take the End Diastolic Velocity? | back 144
|
front 145 When does the PSV drop off? | back 145 Stenosis starts to exceed Approximately 90 % |
front 146 What affects the PSV | back 146 length of the stenosis
|
front 147 What are the Cardinal Doppler Parameters? | back 147 Peak Systole End Diastole ICA/CCA Ratio
|
front 148 Explain the velocity increase in a stenosis. | back 148 The amount of velocity increase is small until the stenosis exceeds 50% |
front 149 What is velocity proportional to? | back 149 Velocity will be proportional to the amount of stenosis. By measuring the velocity we measure the stenosis |
front 150 In vascular what is everything weighed by? | back 150 Everything that we do in Vascular is weighed by the velocity more so than the Bmode measurement |
front 151 What happens when no cause of asymmetry can be found? | back 151 other modalities should be used to find the cause. Major asymmetry between right & left should be a red flag |
front 152 If the CCA is normal what do we say about the waveform? | back 152 Should be low resistance |
front 153 If the Distal CCA is obstructed what happens to the waveform? | back 153 High resistance ECA waveform |
front 154 If the proximal CCA is obstructed what happens to the waveform? | back 154 Dampened Waveform
|
front 155 What is the best method of Best method of quantification of the CCA | back 155 comparison with the contralateral side |
front 156 CCA Pulsatility | back 156
|
front 157 What are the three critical areas? | back 157
|