Instructions for Side by Side Printing
- Print the notecards
- Fold each page in half along the solid vertical line
- Cut out the notecards by cutting along each horizontal dotted line
- Optional: Glue, tape or staple the ends of each notecard together
Liver
front 1 What is the function of the falciform ligament? | back 1 Connects the liver to the anterior diaphragm and the anterior abdominal wall. |
front 2 What is the echo texture of the liver? | back 2 homogeneous |
front 3 Name the abdominal organs in order from Hyperechoic to hypoechoic | back 3 Renal sinus > Pancreas > spleen > renal cortex |
front 4 Where is the porta hepatis to the caudate lobe? | back 4 lies anterior |
front 5 Where is the bare area of the liver? | back 5 The bare area comes in direct contact with the diaphragm |
front 6 What is riedel's lobe? | back 6 congenital variant extension of the right lobe of the liver beyond the lower pole of the right kidney. |
front 7 What is the major problem with riedel's lobe? | back 7 It can be mistaken for hepatomegaly |
front 8 What are the measurements of the right lobe of the liver? | back 8 20 cm / 15 cm |
front 9 What are the hepatic veins key to? | back 9 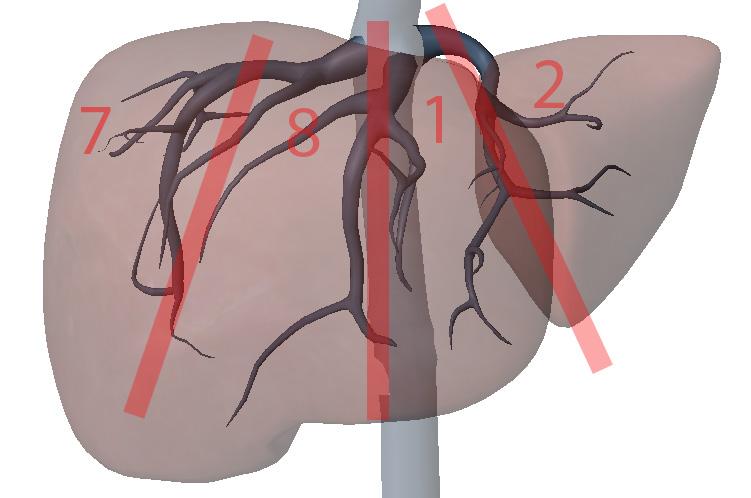 division of the liver longitudinally |
front 10 What are the portal veins key to? | back 10 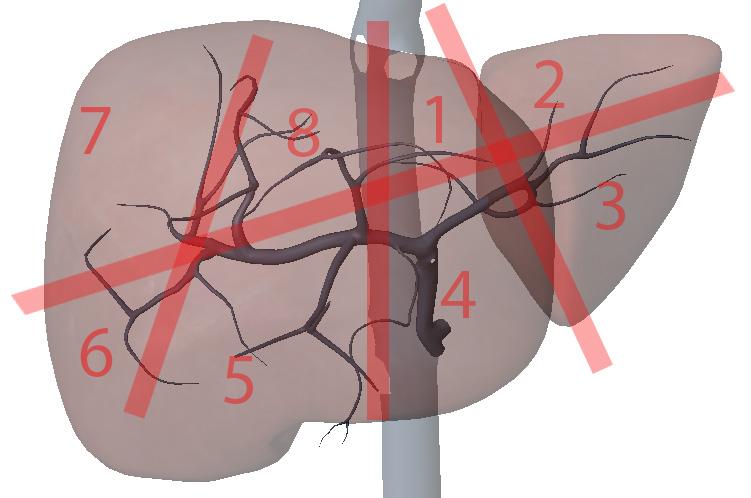 transverse division of the liver |
front 11 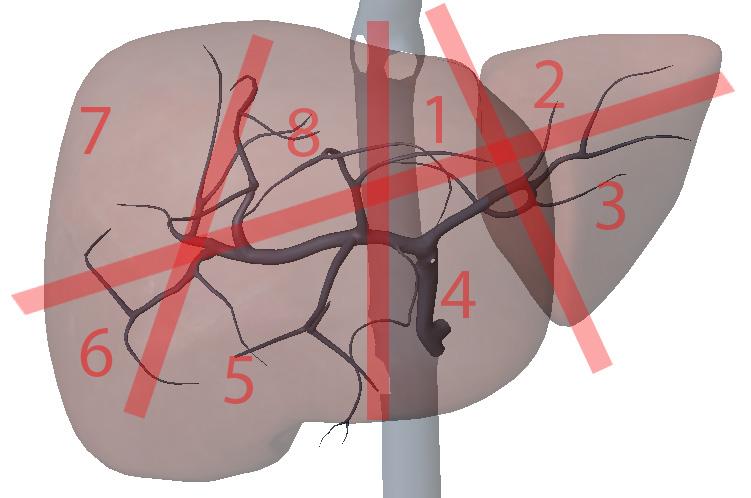 What is section 1? | back 11 Left Medial superior |
front 12 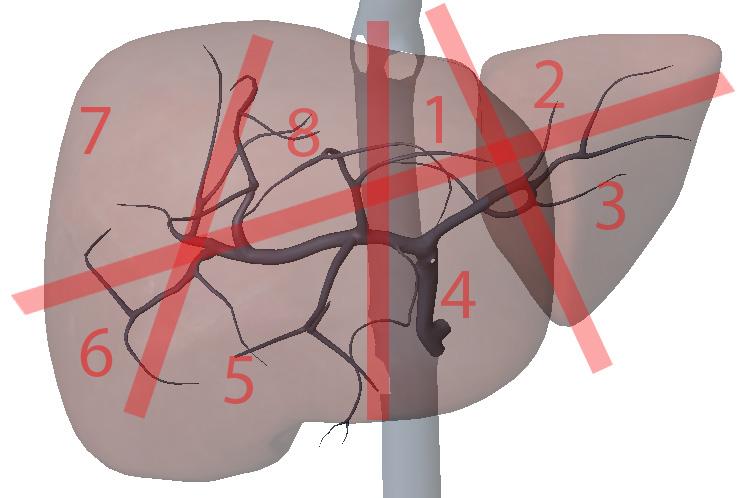 What is section 2? | back 12 Left lateral superior |
front 13 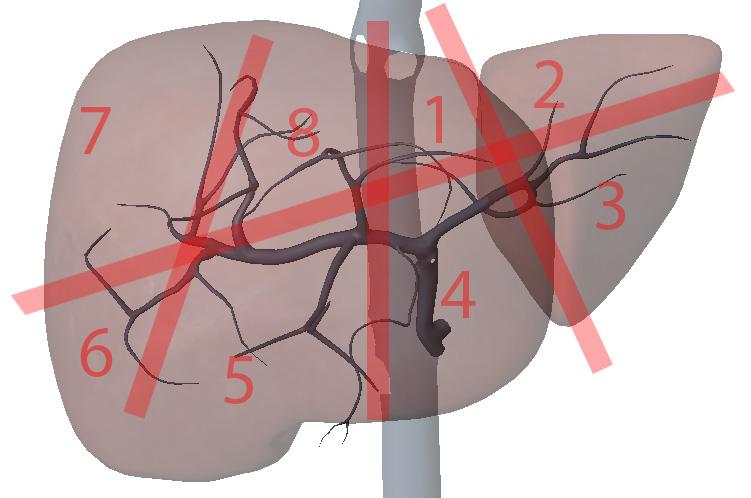 What is section 3? | back 13 Left lateral inferior |
front 14 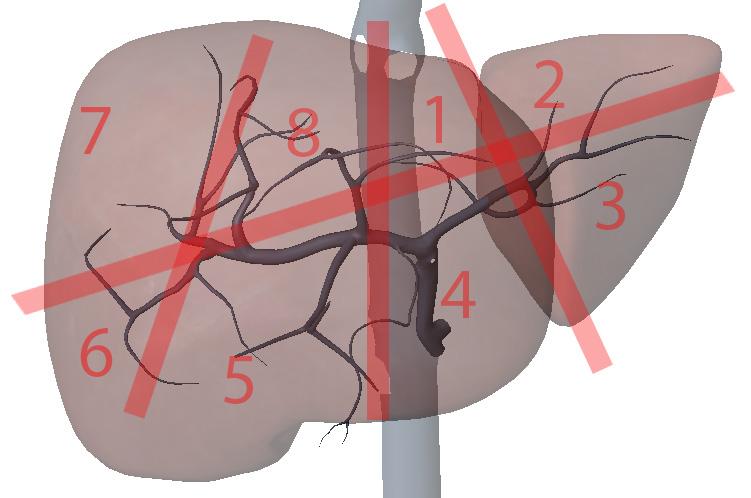 What is section 4? | back 14 Left medial inferior |
front 15 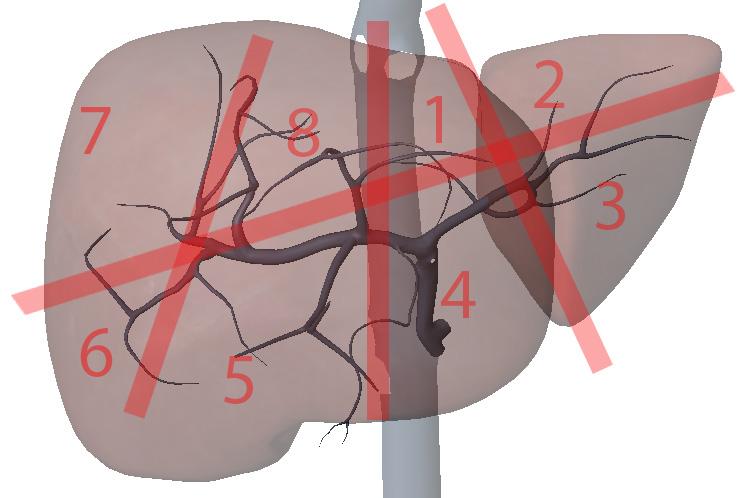 What is section 5? | back 15 Right anterior inferior |
front 16 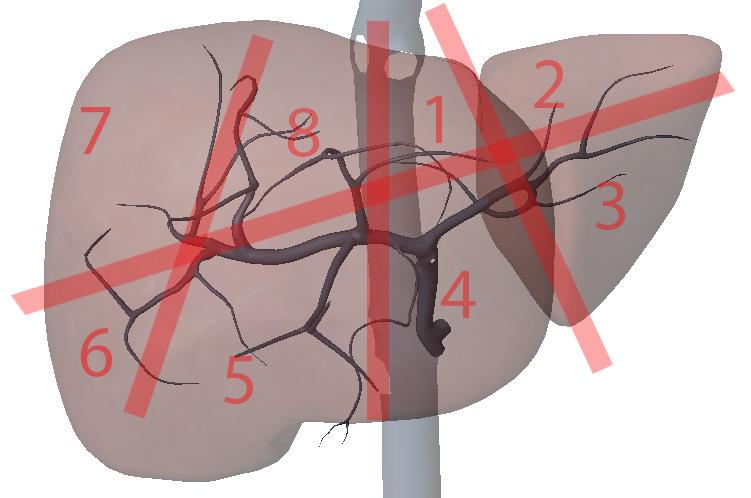 What is section 6? | back 16 Right posterior inferior |
front 17 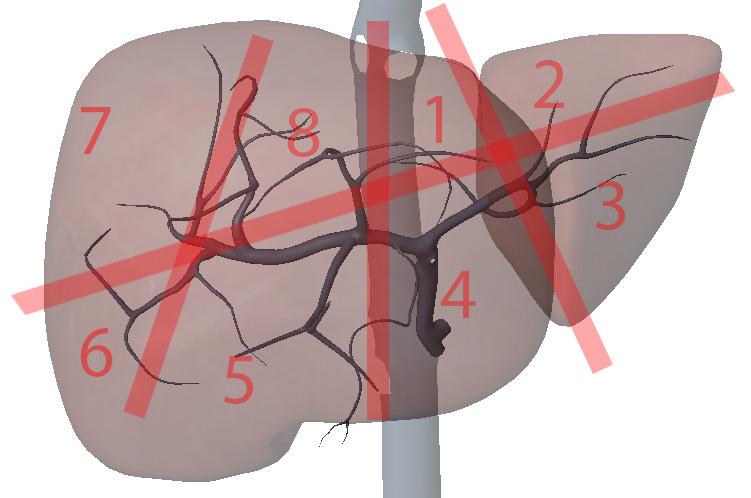 What is section 7? | back 17 Right posterior superior |
front 18 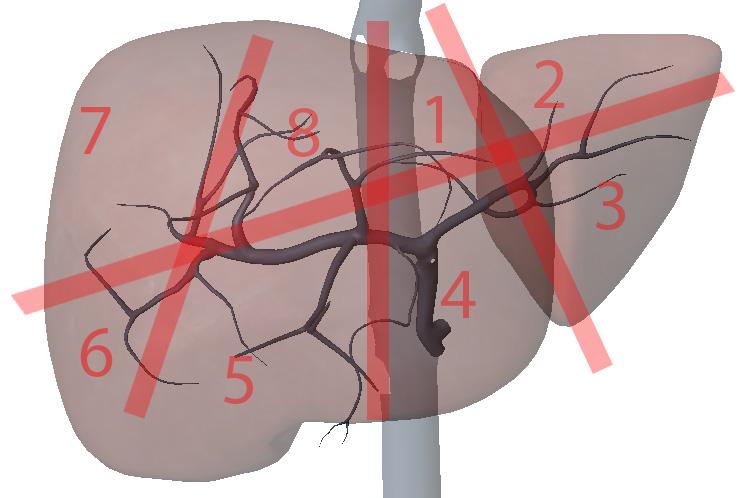 What is section 8? | back 18 Right anterior superior |
front 19 Explain where the liver lies in the abdomen | back 19 right hypochondriac epigastrium Left hypochondriac to the left mammary line |
front 20 What covers the liver? | back 20 Glisson's capsule Fibrous peritoneum - covers all but bare area |
front 21 How is the left lobe divided? | back 21 medial / lateral |
front 22 How is the right lobe divided? | back 22 posterior / anterior |
front 23 How is the liver oxygenated? | back 23 portal veins - 80% Hepatic arteries - 20% |
front 24 Explain the inferior liver. | back 24 sits on the mesentery |
front 25 medial left lobe lies to the portal hepatis? | back 25 anterior to the portal hepatis |
front 26 medial left lobe lies between? | back 26 ligament terres and the gallbladder fossa. |
front 27 What lies at the anterior border of the caudate lobe? | back 27 left portal vein |
front 28 What supplies the caudate lobe with blood? | back 28 hepatic artery branches of the left portal vein branches of the right portal vein |
front 29 What drains the caudate lobe? | back 29 small veins to the IVC |
front 30 What is the seagull? | back 30 Celiac axis |
front 31 Explain the neonatal flow. | back 31 umbilical vein ductus venosum IVC heart |
front 32 Umbilical vein turns into what after birth? | back 32 ligament teres |
front 33 Ductus venosum turns into what after birth? | back 33 ligament venosum |
front 34 What is a possible problem with portal hypertension? | back 34 recanalization of the ligament teres |
front 35 Why are portal veins echogenic? | back 35 they lie in fibrofatty tracks |
front 36 Where is the ligament teres? | back 36 runs long outside of falciform ligament? |
front 37 What is another name for the ligament teres? | back 37 round ligament |
front 38  | back 38 ligament teres |
front 39 How do we locate the porta hepatis? | back 39 MPV kisses the IVC |
front 40 Explain the direction of the main portal vein. | back 40 courses superiorly toward the right then posteriorly at the liver hylum |
front 41 | back 41 Main lobar fissure |
front 42 A groove that divides the Rt lobe of the liver into anterior and posterior segment | back 42 Rt intersegmental fissure |
front 43 Which anatomical structure is located within the Rt Intersegmental fissure? | back 43 Right hepatic vein |
front 44 Which anatomical structure is located within the Lt Intersegmental fissure? | back 44 Left hepatic vein Left Portal Vein Ligamentum Teres |
front 45 A groove that divides the Lt lobe of the liver into medial and lateral segment | back 45 Lt Intersegmental fissure |
front 46 What seprates the caudate from the left liver lobe? | back 46 ligament venosum |
front 47 What is the measurement of the MPV? | back 47 less than 13 mm |
front 48 What is the # 1 cause of Portal Hypertension? | back 48 cirrhosis |
front 49 What is possible if the MPV is more than 13 mm? | back 49 portal hypertension |
front 50 Where is the right portal vein? | back 50 separates the right liver lobe into anterior and posterior sections |
front 51 What does the horizontal segment of the left portal vein separate? | back 51 caudate from the medial left lobe |
front 52 What does the ascending segment of the left portal vein separate? | back 52 separates the medial left lobe from the lateral left lobe. |
front 53 What are the three major functions of the liver? | back 53 metabolism detoxification storage |
front 54 What are the two types of metabolism in the liver? | back 54 gluconeogenesis glucolysis |
front 55 What is Hepatocellular? | back 55 hepatocytes are affected treated medically |
front 56 How is obstruction treated? | back 56 surgically |
front 57 What does acute or chronic liver disease affect? | back 57 liver metabolism |
front 58 Define metabolism. | back 58 chemical process that occur in the body that are necessary for matenance of life catabolic - meow anabolism - build |
front 59 What happens to carbs in the liver? | back 59 catobolized to glucose to use as energy |
front 60 What happens to the extra glucose not used as energy? | back 60 sent to the liver converted to glycogen stored |
front 61 What happens to glycogen when energy is needed? | back 61 liver converts glycogen back to glucose |
front 62 What is a possible cause of hyperglycemia and hypoglycemia? | back 62 liver disease |
front 63 What happens to fats in the liver? | back 63 converted by hepatocytes to lipoproteins |
front 64 What is a lipoproteins? | back 64 fats broken down to monoglycerides and diglycerides |
front 65 What makes lipoproteins so fabulous? | back 65 they are soluble in plasma and may be transported by the blood. |
front 66 What happens to stored fats sent to the liver? | back 66 liver converts them to glucose and cholesterol |
front 67 What happens during liver disease to monoglycerides and diglycerides? | back 67 they are unable to convert to lipoproteins instead are converted to triglycerides |
front 68 Why are triglycerides not fabulous? | back 68 they are not soluble so they get stuck in the liver FATTY LIVER disease |
front 69 What is PT | back 69 Prothrombin time - the amount of time it takes for blood to clot |
front 70 What is PTT? | back 70 partial thromboplastin is the time it takes for plasma to clot |
front 71 Cogulopathy | back 71 disease condition of cogulation |
front 72 Does IV therapy fix liver disease? | back 72 No |
front 73 What is hypoalbuminemia? | back 73 not enough albumin |
front 74 What can hypoalbuminemia cause? | back 74 edema & ascites |
front 75 What is the primary cause of ascites? | back 75 portal hypertension |
front 76 What happens to proteins when they are digested? | back 76 they are converted to amino acids then sent to the liver |
front 77 What does the liver do with amino acids? | back 77 makes proteins |
front 78 What is albumin? | back 78 important protein produced in large quantities in the liver. |
front 79 What is albumin responsible for? | back 79 vascular fluid pressure |
front 80 What are the fat soluble vitamins? | back 80 ADEK |
front 81 What is the production source of proteins for blood coagulation? | back 81 The liver |
front 82 What is needed for blood coagulation? | back 82 fibrinogen prothrombin factors V, VII, IX, X |
front 83 What do you have to do before any invasive procedure? | back 83 check labs for PT PTT INR |
front 84 What is INR | back 84 international normalized ratio only used when the patient is taking blood thinner |
front 85 Why is vitamin K important | back 85 precursor to the production of factors V, VII, IX, X No K no factors V, VII, IX, X, No clotting |
front 86 True or False? liver disease can decrease production of clotting factors V, VII, IX, X. | back 86 True |
front 87 What will low clotting factors cause? | back 87 inadequate coagulation which results in uncontrolable hemorrhage. |
front 88 How does biliary obstruction affect coagulation? | back 88 Bile emulsifies fat No bile = no fat will be broken down if fat is not broken down, fat soluble vitamins are not absorbed (K) No K = No clotting factor. |
front 89 True or False? Protein ingestion plays a role in nitrogen metabolism | back 89 True |
front 90 What is the importance of hepatic enzymes? | back 90 detection of liver disease when hepatocytes are damaged hepatic enzymes leak into the blood and can be detected with lab tests. |
front 91 What is NH4 Ammonia? | back 91 toxic byproduct of nitrogen metabolism |
front 92 What happens if the detoxification does not exist? | back 92 toxic levels will rise Ex. Ammonia NH4 |
front 93 What happens to to Ammonia NH4? | back 93 it is converted to urea then sent to then excreted by the kidneys |
front 94 What is an accumulation of ammonia called? | back 94 Fetor Hepaticus |
front 95 How can we tell if a patient has Fetor Hepaticus? | back 95 fruity breath confusion coordination loss coma tremor |
front 96 Fetor Hepaticus What are the two most important lab values to look at? | back 96 BUN creatin |
front 97 What is BUN? | back 97 Blood Urea Nitrogen |
front 98 What happens when drugs are not detoxified? | back 98 drug dosages may need to be lowered because they are not removed by the liver |
front 99 What happens when hormones are not detoxified? | back 99 hormones rise |
front 100 What happens in men with cirrhosis? | back 100 liver can't break down estrogen gynecomastia testicular atrophy |
front 101 What is in bile? | back 101 water bile salts bile pigments cholesterol lecithin protein |
front 102 What does the Liver function test consist of? | back 102 AST ALT LDH Alkaline Phosphatase Bilirubin (direct, indirect, total) Prothrombin time Albumin & Globlins |
front 103 Aspartase Aminotransferase | back 103 AST present in tissue but only released in blood when tissue is damaged |
front 104 What is an old name for AST | back 104 SGOT |
front 105 What would be a common cause for elevation of AST? | back 105 Acute hepatitis Cirrhosis Infectious Mononucleosis |
front 106 What can cause splenomegaly? | back 106 Infectious Mononucleosis |
front 107 True or False? AST is elevated before jaundice occurs | back 107 True |
front 108 What is one draw back with AST lab? | back 108 AST is non specific it can be produced by any organ with a high metabolism rate. |
front 109 Alanine Aminotransferase | back 109 ALT tends to be used to monitor patients after jaundice has occured liver specific |
front 110 What are some causes of low levels of ALT? | back 110 acute cirrhosis hepatic metastasis pancreatis |
front 111 What are some causes of mid levels of ALT? | back 111 obstruction |
front 112 What are some causes of high levels of ALT? | back 112 hepatocellular disease toxic hepatitis |
front 113 Lactic Acid Dehydogenase | back 113 LDH present in tissue but not released unless there has been cell death or damage |
front 114 Why is LDH not a good liver test? | back 114 detects heart attacks elevated in myocardial infarction & pulmonary infarction |
front 115 What could be the cause of elevation of Alkaline Phosphatase | back 115 obstruction caused by gallstones |
front 116 What is the patient prep for a liver exam? | back 116 fast for at least 6 hours |
front 117 What should be explained to the patient for a liver exam? | back 117 The sonographer should explain to the patient that the exam is being performed to visualize the liver and interdependent organs. |
front 118 How should the patient be dressed for the exam? | back 118 The patient should remove any restrictive clothing above the waist. A towel should be tucked around clothing to protect them from gel. |
front 119 What transducer should be used to visualize the liver? | back 119 3.25 MHz sector or curved linear array. |
front 120 What transducer should be used to visualize the liver in an obese patient? | back 120 2.25 MHz sector or curved linear array. |
front 121 What transducer should be used to visualize the liver on a pediatric patient? | back 121 5.0 MHz sector or curved linear array. |
front 122 What transducer should be used to visualize the liver on a neonate? | back 122 7.4 MHz sector or curved linear array. |
front 123 Explain the procedure of a liver exam. | back 123 Begin doing a full sweep through the liver. Starting sagittal,
slightly to the left of midline. Change to a transverse view and sweep
up and down the left lobe from a subcostal approach. Look in
transverse through the right lobe subcostally or
intercostally.
Start taking images. |
front 124 What is important medical history? | back 124 Sex Age Weight Prior Hepatic Conditions Family History of Hepatic Conditions |
front 125 What position should be used for an exam on the liver? | back 125 Supine |
front 126 What are the scan plans used during a liver exam? | back 126 Sagittal and Transverse |
front 127 Explain the Sagittal plane for the liver exam. | back 127 The transducer may be swept under the intercostal margin to image the liver parenchyma from the anterior abdominal wall to the diaphragm. |
front 128 Explain the Transverse plane for the liver exam. | back 128 The transducer should be angled in a steep cephalic direction to be as parallel to the diaphragm as possible. The transverse plan allows images of liver parenchyma, vascularity and ductal structures. |
front 129 What are the Techniques used for the liver exam? | back 129 Deep inspiration and held. Push belly out. Alternate positions can be used to displace the bowel out of the field of view. Place right arm above head to open intercostal spaces |
front 130 Give an anatomical description of the liver. | back 130 The liver is the largest internal organ. It lies in the right upper quadrant, from the right hypochondria, extending through the epigastrum to the mammary line of the left hypochondria. Generally it lies from the diaphragm to the level of the 8th rib. Size and shape is variable. The liver is covered by the Glisson’s capsule (fibrous peritoneum), except for the bare area that is in contact with the diaphragm. The liver is dived into four lobes. |
front 131 Give an anatomical description of the left liver lobe. | back 131 further divided into lateral and medial segments by the left intersegmental fissure. |
front 132 Give an anatomical description of the right liver lobe. | back 132 divided from the left lobe by the main lobar fissure which passes from the gallbladder fossa to the inferior vena cava. The right lobe is further divided into anterior and posterior segments by the right intersegmental fissure. |
front 133 Give an anatomical description of the caudate liver lobe. | back 133 found on the inferior, posterior side of the liver. The caudate lobe is bordered by the inferior vena cava posteriorly and the ligament venosum anteriorly. The hepatic veins run between the lobes and segments. The portal veins run centrally within the segments. The ascending portion of the left portal runs in the left intersegmental fissure. |
front 134 Give an anatomical description of the medial left liver lobe. | back 134 also called the Quadrate lobe, is bordered by the porta hepatis posteriorly, laterally by the gallbladder fossa and ligament terres. |
front 135 What are appropriate reasons to perform a liver exam? | back 135 Jaundice Decreased appetite Dark urine Cholecystectomy Congestive heart failure |
front 136 What are some appropriate history questions? | back 136 When was the last time you had something to eat or drink? Are you in pain? Where is your pain located? How long have you been in pain? How long does the pain last and does it go away? Have you had a nausea or vomiting? Are you experiencing any other symptoms? Do you have a family history of cancer? Have you had any lab work done? |
front 137 What is the liver protocol? | back 137 Sagittal Transverse Other Images |
front 138 What are the normal variants of the liver? | back 138 Riedel’s lobe Absence of left lobe Multiple sizes Multiple shapes |
front 139 What are proper measurements for the liver exam? | back 139 Liver size may be measured sagittal from the inferior tip of the liver to the dome Length: 20 cm Anterior Posterior: 15 cm C/RL: <0.6 |
front 140 What are common pitfalls for the liver exam? | back 140 Obesity The patient ate before the study Metabolic disorders such as fatty infiltration will reduce detail Shadowing Gas |
front 141 What is the liver function tests? | back 141 Aspartate aminotransferase (AST): 5 – 40 units per liter of
serum |
front 142 What are important labs used for a liver exam? | back 142 White blood count (WBC): 4,500 – 10,000 Red blood count (RBC): 4.5 – 5.5 Hemoglobin (hbg): 13.5 – 16.5 Hct: 41 – 50 Creatine: 0.5 – 1.4 mg/dl Cholesterol: <200 mg/dl Glucose: 60-110 mg/dl Urinary bile and bilirubin: 1.2 mg/dl Urinary urobilinogen: 0 – 8 mg/dl Fecal urobilinogen: 57 to 200 mg./24 hours |
front 143 Diffuse Hepatocellular disease | back 143  Affects the hepatocytes and interferes with liver function |
front 144 What is the sonographic appearance of the Diffuse Hepatocellular disease? | back 144  Increased echogenicity |
front 145 What are the presenting symptoms of Diffuse Hepatocellular disease? | back 145  Asymptomatic jaundice nausea vomiting abnormal tenderness |
front 146 What are the presenting symptoms of acute Diffuse Hepatocellular disease? | back 146  Abnormal Liver Function Test |
front 147 What is Fatty infiltration? | back 147  Fatty liver is an acquired but reversible disorder of metabolism. Fatty filtration implies increased lipid accumulation in the hepatocytes. |
front 148 What is the sonographic appearance of fatty filtration? | back 148  Increased echogenicity |
front 149 What are the presenting symptoms of fatty filtration? | back 149  Asymptomatic jaundice nausea vomiting abnormal tenderness. |
front 150 What lab values would suggest fatty filtration? | back 150  ↑Hepatic Enzymes ↑Alk Phos ↑Direct Bilirubin |
front 151 What are common causes of fatty filtration? | back 151 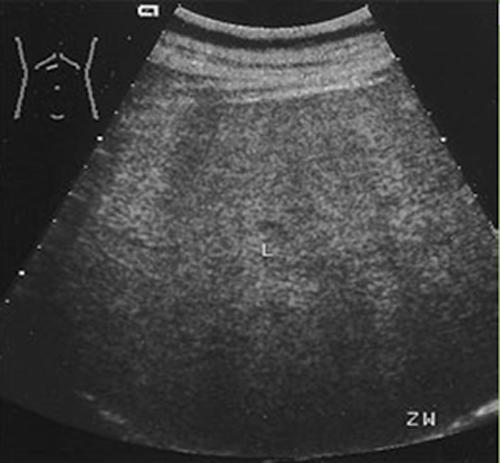 ETOH abuse Diabetes Mellitis Obsesity steroids |
front 152 What is acute hepatitis? | back 152  Inflammatory and infectious disease of the liver caused by complications of liver damage. May be mild to severe. |
front 153 What is the sonographic appearance of acute hepatitis? | back 153  Mild: Normal echogenicity |
front 154 What are the presenting symptoms of acute hepatitis? | back 154  Asymptomatic jaundice nausea vomiting abnormal tenderness. |
front 155 What are the lab values that would suggest acute hepatitis? | back 155  ↑AST ↑ALT ↑Bilirubin Leukopenia |
front 156 What is Chronic hepatitis? | back 156 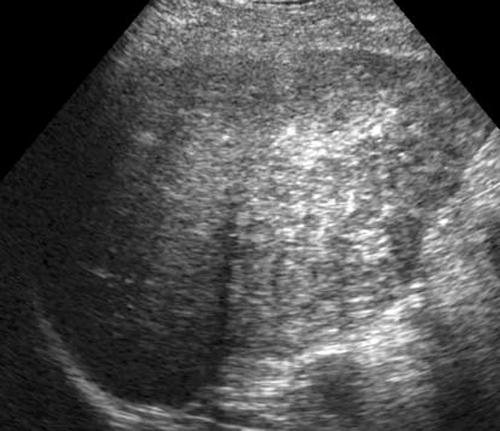 Hepatitis becomes chronic when the inflammation lasts longer than 6 months. |
front 157 What is the sonographic appearance of chronic hepatitis? | back 157 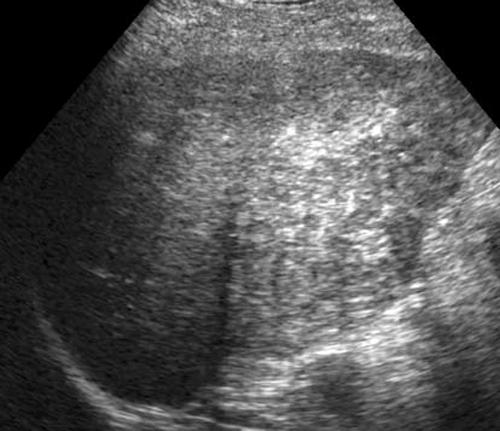 Increased echogenicity |
front 158 What are the presenting symptoms of chronic hepatitis? | back 158 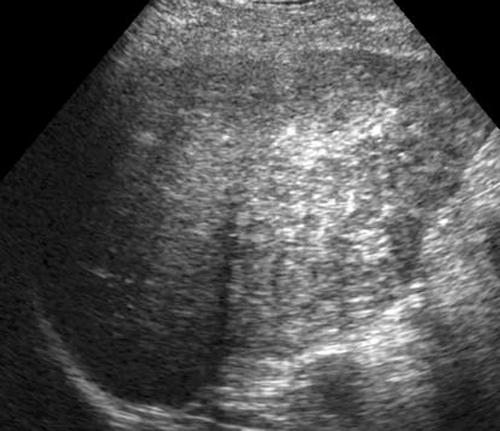 nausea vomiting anorexia weight loss tremors jaundice dark urine fatigue varicosities |
front 159 What are the lab values that would suggest chronic hepatitis? | back 159 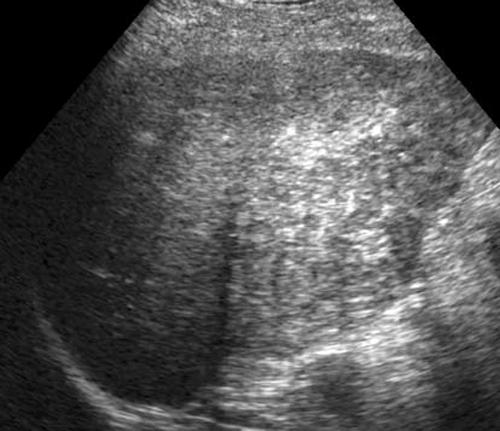 ↑AST ↑ALT ↑Bilirubin Leukopenia |
front 160 What is Cirrhosis? | back 160  A chronic degenerative disease in which there is parenchymal necrosis, regeneration and fibrous tissue resulting in disorganization of lobular architecture. Lobules are infiltrated with fat. Commonly caused by alcoholism. |
front 161 What is the sonographic appearance of Cirrhosis? | back 161  Hepatomegaly |
front 162 What are the presenting symptoms of Cirrhosis? | back 162  fatigue bruises jaundice edema dark urine blood in stool fever Echogenic portal radicals flatulence. |
front 163 What are the lab values that would suggest Cirrhosis? | back 163  ↑Alk Phos ↑Direct Bilirubin ↑AST ↑ALT Leukopenia |
front 164 What is Glycogen storage disease? | back 164  Characterized by the abnormal storage and collection of glycogen in the tissue of the liver and kidneys. Most common type I – Von Gierke’s |
front 165 What is the sonographic appearance of Glycogen storage disease? | back 165  Hepatomegaly |
front 166 What are the presenting symptoms of Glycogen storage disease? | back 166  Non-Specific |
front 167 What are the lab values that would suggest Glycogen storage disease? | back 167  Disturbances in Acid-Base Balance |
front 168 What is Hemochromatosis? | back 168  This is a rare disease involving excess iron deposits. May lead to cirrhosis and portal hypertension |
front 169 What is the sonographic appearance of Hemochromatosis? | back 169  Hepatomegaly |
front 170 What are the presenting symptoms of Hemochromatosis? | back 170  Bronze skin |
front 171 What are the lab values that would suggest Hemochromatosis? | back 171  ↑Iron levels |
front 172 What is Portal venous hypertension? | back 172  This is an increase in portal venous pressure (above 10mmHg) or hepatic venous gradient (above 5mmHg). |
front 173 What is the sonographic appearance of Portal venous hypertension? | back 173  Portal vein measures greater than 13mm |
front 174 What are the presenting symptoms of Portal venous hypertension? | back 174  Gastrointestinal bleeding blood in the stools vomiting of blood Encephalopathy |
front 175 What are the lab values that would suggest Portal venous hypertension? | back 175  ↑Liver Enzymes ↓Platelet Count |
front 176 What is Portal Venous Thrombosis? | back 176 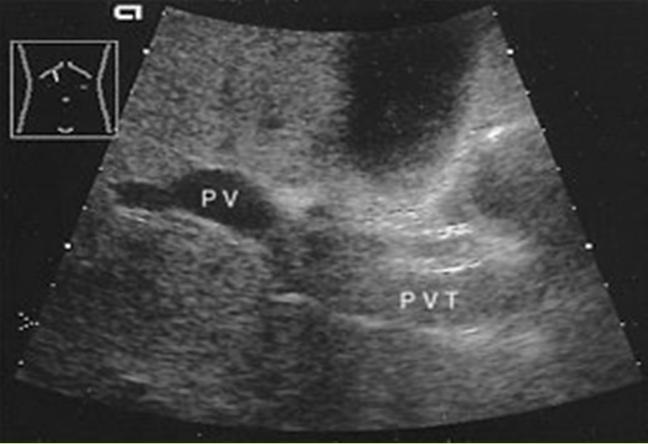 Portal Venous Thrombosis |
front 177 What is the sonographic appearance of Portal Venous Thrombosis? | back 177 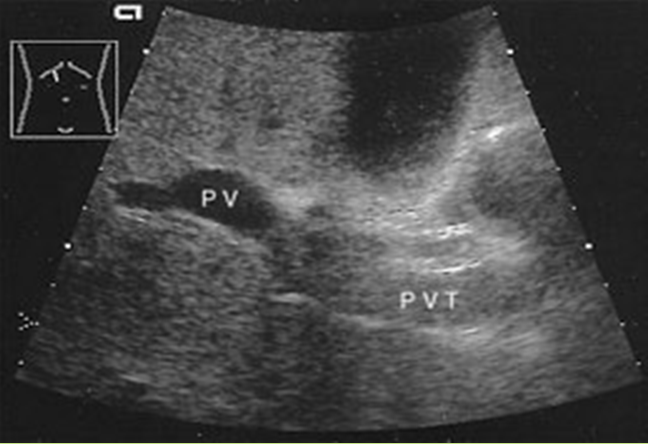 Portal flow absence |
front 178 What are the presenting symptoms of Portal Venous Thrombosis? | back 178 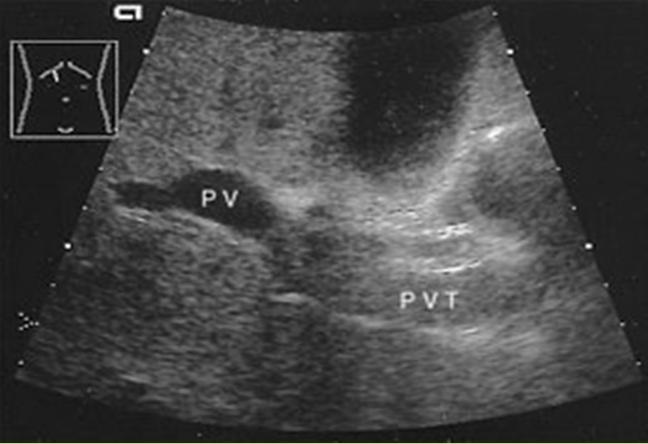 vague and non-specific |
front 179 What is Budd-Chiari Syndrome? | back 179  A rare disease which is caused by a thrombosis of the hepatic veins or IVC. Has a high mortality rate. |
front 180 What is the sonographic appearance of Budd-Chiari Syndrome? | back 180  Ascites |
front 181 What are the presenting symptoms of Budd-Chiari Syndrome? | back 181  non-specific abdominal pain |
front 182 Where is Budd-Chiari syndrome most common? | back 182 asia |
front 183 What are the lab values that would suggest Budd-Chiari Syndrome? | back 183 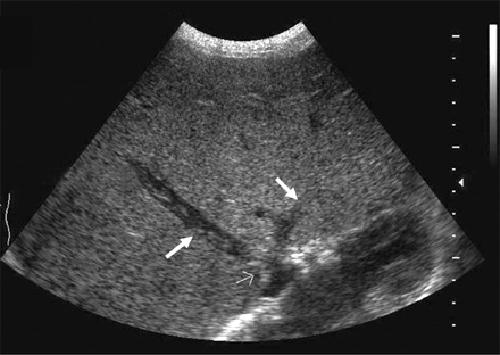 Albuminuria ↑Alk Phos ↑AFT |
front 184 What is Proximal Biliary obstruction? | back 184 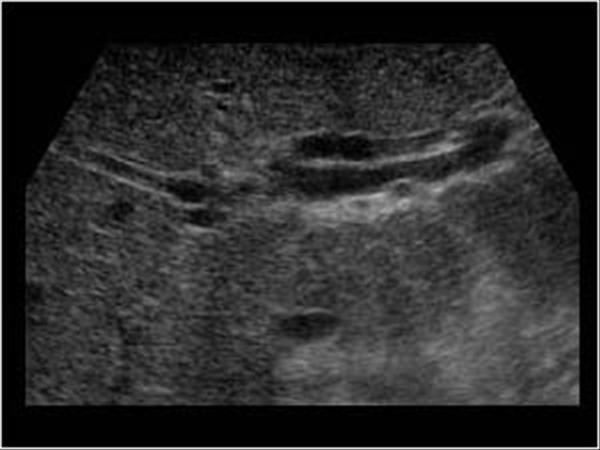 Proximal Biliary obstruction proximal to the cystic duct can be caused by gallstones. |
front 185 What is the sonographic appearance of Proximal Biliary obstruction? | back 185 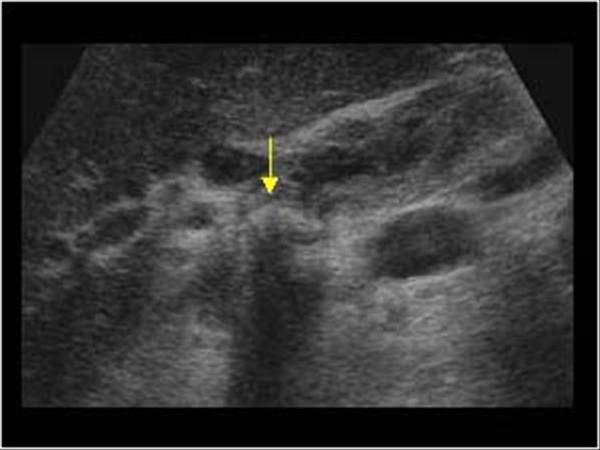 Dilated intrahepatic ducts |
front 186 What are the presenting symptoms of Proximal Biliary obstruction? | back 186 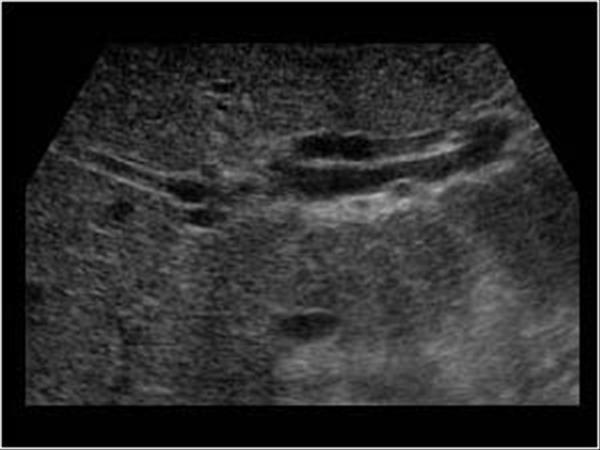 Jaundice pruritus |
front 187 What are the lab values that would suggest Biliary obstruction? | back 187 ↑Direct Bilirubin ↑Alk Phos |
front 188 What is Distal Biliary obstruction? | back 188 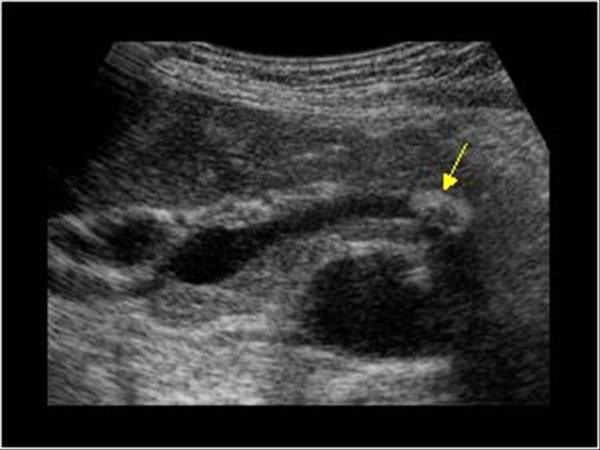 Biliary obstruction distal to the cystic duct |
front 189 What is the sonographic appearance of Distal Biliary obstruction? | back 189  Stone in the common duct |
front 190 What are the presenting symptoms of Distal Biliary obstruction? | back 190  Jaundice pruritus |
front 191 What are the lab values that would suggest Distal Biliary obstruction? | back 191 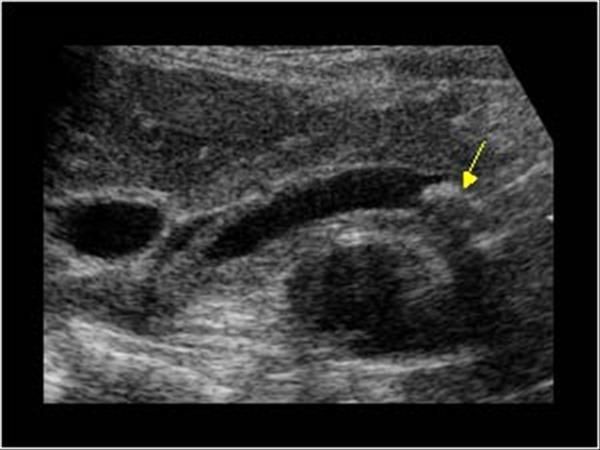 ↑Direct Bilirubin ↑Alk Phos |
front 192 What is Extrahepatic mass? | back 192  A mass in the area of the porta hepatis |
front 193 What is the sonographic appearance of Extrahepatic mass?? | back 193  Stone in the common duct |
front 194 What are the presenting symptoms of Extrahepatic mass?? | back 194  Jaundice pruritus |
front 195 What are the lab values that would suggest Extrahepatic mass?? | back 195  ↑Direct Bilirubin ↑Alk Phos |
front 196 What is Common Duct Stricture? | back 196  Sonographic Appearance: |
front 197 What is the sonographic appearance of Common Duct Stricture? | back 197 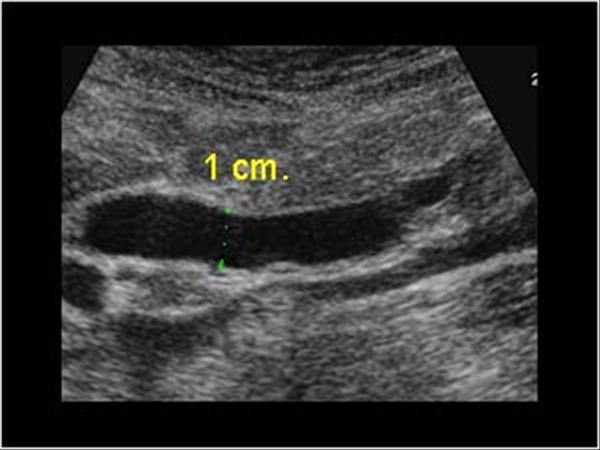 Common Duct Stricture |
front 198 What are the presenting symptoms of Common Duct Stricture? | back 198 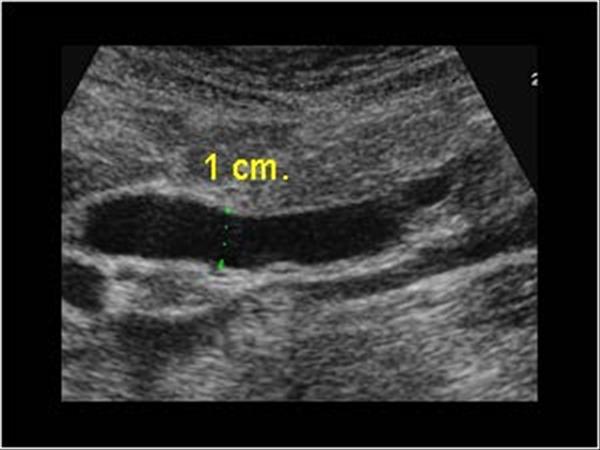 jaundice past cholecystectomy increase in direct bilirubin |
front 199 What are the lab values that would suggest Common Duct Stricture? | back 199  ↑Direct Bilirubin ↑Alk Phos |
front 200 What is Passive hepatic congestion? | back 200 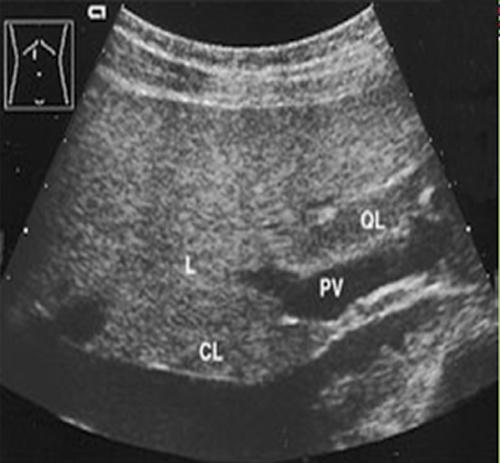 develops secondary to congestive heart failure. |
front 201 What is the sonographic appearance of Passive hepatic congestion? | back 201  Dilated IVC, SMV, Portal and Splenic veins Hepatomegaly |
front 202 What are the presenting symptoms of Passive hepatic congestion? | back 202  congestive heart failure. |
front 203 What are the lab values that would suggest Passive hepatic congestion? | back 203  ↑ LFT |
front 204 What is Simple hepatic cysts? | back 204 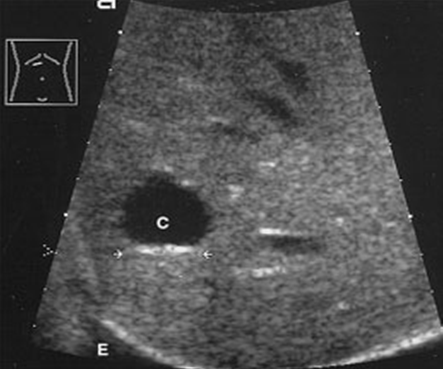 A hepatic cyst is usually a solitary, non-parasitic cyst of the liver. solitary or multiple. More common in females. |
front 205 What is the sonographic appearance of hepatic cysts? | back 205 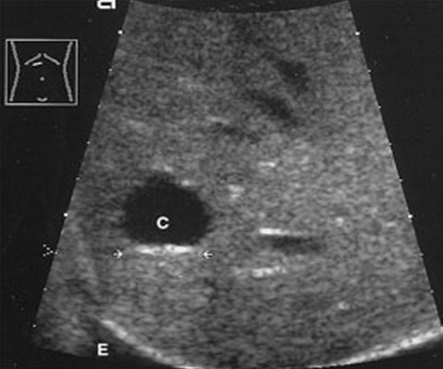 Solitary or multiple |
front 206 What are the presenting symptoms of hepatic cysts? | back 206 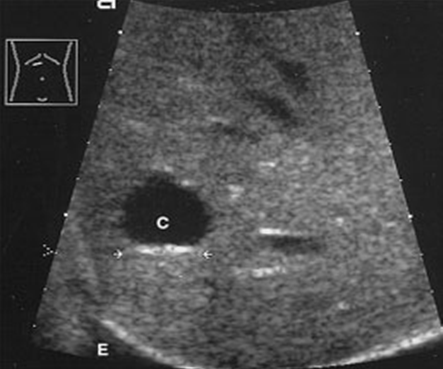 Asymptomatic localized pain |
front 207 What is Congenital hepatic cysts? | back 207  A rare lesion that caused by developmental defects in the formation of bile ducts. |
front 208 What is the sonographic appearance of Congenital hepatic cysts? | back 208  Usually solitary |
front 209 What is Peribiliary Cysts? | back 209 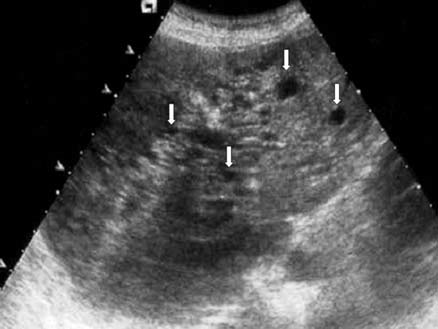 Very small cysts that range from .2 to 2.5 cm. They are most common in patients with severe liver disease. |
front 210 What is the sonographic appearance of Peribiliary Cysts? | back 210 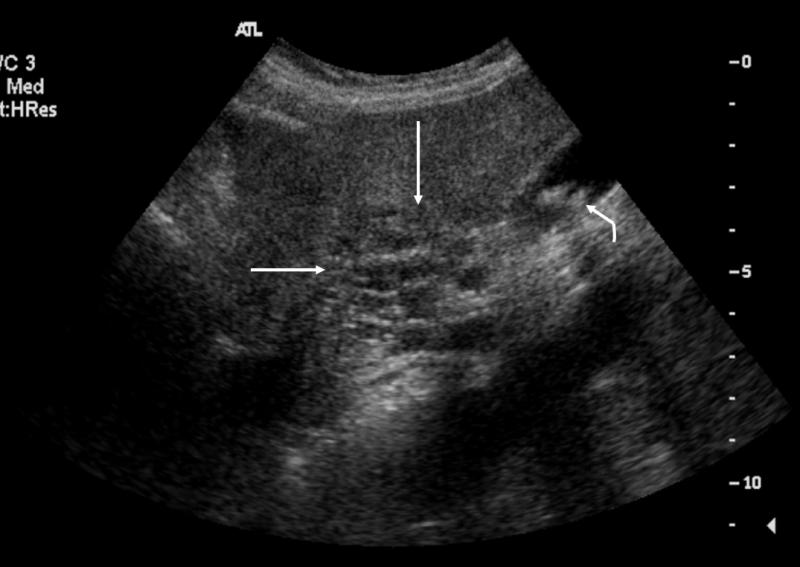 clusters with a tubular appearance |
front 211 What is Polycystic liver disease? | back 211 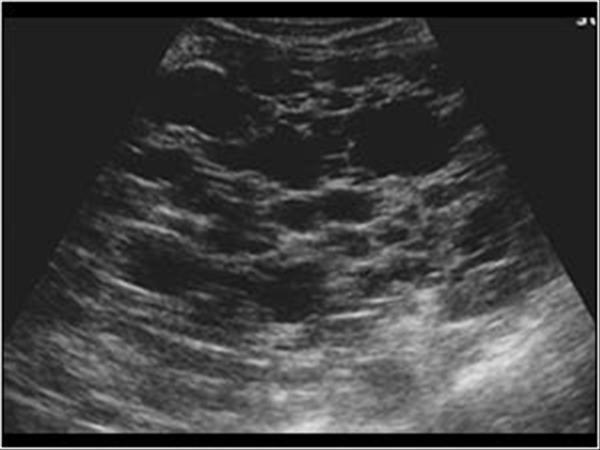 This is an autosomal dominant genetic disease in which multiple small cysts cover the liver. 60% of patients with polycystic liver disease will have polycystic kidney disease. |
front 212 What is the sonographic appearance of Polycystic liver disease? | back 212  Anechoic |
front 213 What are the presenting symptoms of Polycystic liver disease? | back 213 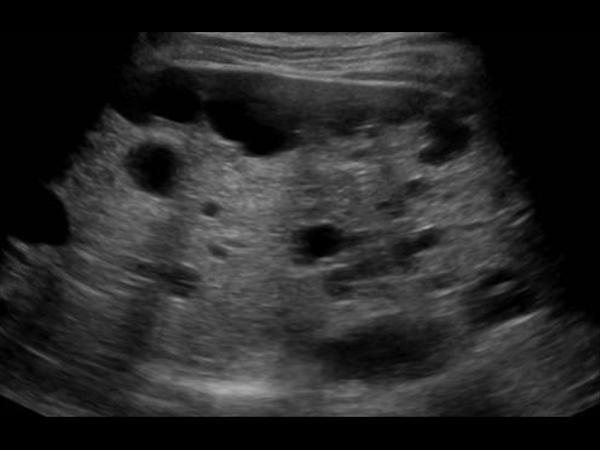 abdominal pain bloating or swelling in the abdomen feeling full |
front 214 What are the lab values that would suggest Polycystic liver disease? | back 214  ↑WBC |
front 215 What is Pyogenic abscess? | back 215  A pus-forming abscess caused by bacteria. The most common bacteria is Escherichia coli and anaerobes. The most frequent organism causing the infection is Escherichia coli or anaerobes |
front 216 What is the sonographic appearance of Pyogenic abscess? | back 216  Sonographic Appearance: |
front 217 What are the presenting symptoms of Pyogenic abscess? | back 217  fever pain pleutitis nausea vomiting diarrhea |
front 218 What are the lab values that would suggest Pyogenic abscess? | back 218  ↑WBC LFT |
front 219 What is Hepatic candidiasis? | back 219  This is caused by a type of Candida fungus usually in immunocompromised patients. |
front 220 What is the sonographic appearance of Hepatic candidiasis? | back 220  Multiple |
front 221 What are the presenting symptoms of Hepatic candidiasis? | back 221  persistent fever and localized pain |
front 222 What are the lab values that would suggest Hepatic candidiasis? | back 222  ↑WBC |
front 223 What is Chronic granulomatous disease? | back 223  a genetic disorder in which phagocytes are unable to kill certain bacteria. |
front 224 What is the sonographic appearance of granulomatous disease? | back 224  Sonographic Appearance: |
front 225 What are the presenting symptoms of granulomatous disease? | back 225  reoccurring respiratory infections |
front 226 What are the lab values that would suggest granulomatous disease? | back 226  |
front 227 What is Amebic abscess? | back 227  A collection of pus formed by disintegrated tissue. Primarily a disease of the colon |
front 228 What is the sonographic appearance of Amebic abscess? | back 228  Hypoechoic |
front 229 What are the presenting symptoms of Amebic abscess? | back 229  asymptomatic abdominal pain diarrhea leukocytosis fever. |
front 230 What are the lab values that would suggest Amebic abscess? | back 230  ↑Leukocytes |
front 231 What is Echinococcal cyst? | back 231  Infectious cystic disease common in sheep herders, a tapeworm that infects. |
front 232 What is the sonographic appearance of Echinococcal cyst? | back 232  Simple |
front 233 What are the presenting symptoms of Echinococcal cyst? | back 233  asymptomatic abdominal pain abnormal abdominal tenderness hepatomegaly abdominal mass jaundice fever anaphylactic reaction |
front 234 What are the lab values that would suggest Echinococcal cyst? | back 234  ↑WBC |
front 235 What is Cavernous hemangioma? | back 235  Benign congenital tumor of the liver. Most common and most frequent in females. |
front 236 What is the sonographic appearance of hemangioma? | back 236  Hyperechoic |
front 237 What are the presenting symptoms of hemangioma? | back 237  RUQ pain |
front 238 What are the lab values that would suggest hemangioma? | back 238  |
front 239 What is Liver cell adenoma? | back 239  tumor of glandular epithelial tissue. More commonly in women taking oral contraceptives. |
front 240 What is the sonographic appearance of Liver cell adenoma? | back 240  Sonographic Appearance: |
front 241 What are the presenting symptoms of Liver cell adenoma? | back 241  RUQ pain |
front 242 What are the lab values that would suggest Liver cell adenoma? | back 242  |
front 243 What is Hepatic cystadenoma? | back 243 rare neoplasm in middle aged women |
front 244 What is the sonographic appearance of Hepatic cystadenoma? | back 244 Multi – loculated lesion |
front 245 What are the presenting symptoms of Hepatic cystadenoma? | back 245 palpable mass |
front 246 What are the lab values that would suggest Hepatic cystadenoma? | back 246 no data |
front 247 What is Focal nodular hyperplasia? | back 247  This is the second most common benign liver mass in women over 40 years of age. |
front 248 What is the sonographic appearance of Focal nodular hyperplasia? | back 248  Sonographic Appearance: |
front 249 What are the presenting symptoms of Focal nodular hyperplasia? | back 249  Asymptomatic |
front 250 What are the lab values that would suggest Focal nodular hyperplasia? | back 250  |
front 251 What is Hepatocellular carcinoma? | back 251  HCC - This is the most common primary malignant neoplasm. |
front 252 What is the sonographic appearance of Hepatocellular carcinoma? | back 252  Sonographic Appearance: |
front 253 What are the presenting symptoms of Hepatocellular carcinoma? | back 253  palpable mass appetite disorder fever |
front 254 What are the lab values that would suggest Hepatocellular carcinoma? | back 254  ↑alpha-protein test Liver function test ↑Alk Phos ↑Direct Bilirubin ↑AST, ↑ALT Leukopenia |
front 255 What is Metastatic disease? | back 255  This is the most common form of neoplastic involvement of the liver. The primary sites include colon, breast, and lung. |
front 256 What is the sonographic appearance of Metastatic disease? | back 256  Appearance varies |
front 257 What are the presenting symptoms of Metastatic disease? | back 257  jaundice hepatomegaly weight loss decreased appetite |
front 258 What are the lab values that would suggest Metastatic disease? | back 258  Abnormal LFT |
front 259 What is Lymphoma? | back 259  This is a malignant neoplasm which involves a rapid increase of lymphocytes in the lymph nodes. Hodgkins, and Non-Hodgkins lymphoma. |
front 260 What is the sonographic appearance of Lymphoma? | back 260  hepatomegaly |
front 261 What are the lab values that would suggest Lymphoma? | back 261  abnormal LFTs |
front 262 What is Hepatic trauma? | back 262  injury |
front 263 What is the sonographic appearance of Hepatic trauma? | back 263  Hyperechoic hematomas |
front 264 What are the presenting symptoms of Hepatic trauma? | back 264  varies |
front 265 What is Liver transplantation? | back 265  A liver transplant is performed when other conventional and surgical methods have failed the patient. The most common reason for a transplant is cirrhosis. Scans should be performed 24, 48, and biweekly post operative |
front 266 What is the sonographic appearance of transplantation? | back 266  Examine the portal venous system, hepatic arteries, the IVC, and
parenchymal patterns |
front 267 What is the cause of the most common complication of a liver transplant? | back 267 hepatic arteries |
front 268 What are the lab values that would suggest transplantation? | back 268 no data |
front 269 What is lymphadenopathy? | back 269 Swollen lymph nodes |
front 270 What is lymphosarcoma? | back 270 lymphadenopathy in multiple organs |
front 271 Pediatrics What is Neuroblastomeas? | back 271 tumor of the adrenal densely reflective |
front 272 Pediatrics What is Wilms tumor? | back 272 reflective with central lucency from necrosis |
front 273 Pediatrics What is Leukemia? | back 273 cancer of blood reflective with central lucency from necrosis |