Instructions for Side by Side Printing
- Print the notecards
- Fold each page in half along the solid vertical line
- Cut out the notecards by cutting along each horizontal dotted line
- Optional: Glue, tape or staple the ends of each notecard together
A&P Exam 3 Material (Final)
front 1 A typical bone has these 2 distinct regions of bone | back 1 Compact & spongy bone |
front 2 The inside of the bone; important function is hematopoiesis | back 2 Marrow cavity |
front 3 Difference r/t hematopoiesis in children vs. adults | back 3 Children - all bones make blood cells Adults - only some parts of certain bones make blood cells |
front 4 Region of long bone: Head of bone | back 4 Epiphysis |
front 5 Region of long bone: Shaft of bone | back 5 Diaphysis |
front 6 Bones found in the limbs | back 6 Long bones |
front 7 In the femur, as in the humerus, hematopoiesis occurs only in 1) this region of the bone, which is composed of 2) this type of bone | back 7 1. Head & neck (proximal portion) 2. Spongy bone |
front 8 In adult bones that don't participate in hematopoiesis, 1) what change occurs, 2) what is it due to, and 3) where does it occur? | back 8 1. Red marrow is replaced with yellow marrow 2. Yellow = fat (red was due to RBC production) 3. Spongy part of the bone |
front 9 Most of bone is encased within this layer, which has 2 sublayers | back 9 Periosteum |
front 10 The periosteum, which encases most bone, consists of these 2 layers | back 10 1. Tough fibrous outer layer w/collagen 2. Inner cellular layer playing key role in bone formation |
front 11 Layer of periosteum w/collagen fibers | back 11 Tough fibrous outer layer |
front 12 Layer of periosteum that plays key role in bone formation | back 12 Inner cellular layer |
front 13 The periosteum is replaced by _____ 1 _____ on the _____ 2 _____ of the bone | back 13 1. articular cartilage 2. articular surface |
front 14 Articular cartilage, which replaces the periosteum on the articular surface of bones, is composed of this glassy, very smooth cartilage | back 14 Hyaline cartilage |
front 15 Glassy, very smooth cartilage that replaces the periosteum on articular surfaces of bones | back 15 Hyaline cartilage |
front 16 This type of bone has an orderly structure & contains a series of tunnels | back 16 Compact bone |
front 17 Series of tunnels within compact bone; contain blood vessels | back 17 Central canals |
front 18 The layer lining the central canals within compact bone | back 18 Endosteum |
front 19 2 layers within bone that participate in new bone formation | back 19 1. Inner cellular layer of periosteum 2. Endosteum (lining central canals of compact bone) |
front 20 Completely encloses spongy bone | back 20 Compact bone |
front 21 -Thin layer -Accounts for smaller volume of given bone -Higher density, so 75% of bone by weight | back 21 Compact bone |
front 22 What would happen if all of your bone was compact bone? | back 22 Too heavy to move or even sit up!!! |
front 23 The circular structure surrounding one central canal; includes rings marked with osteocytes | back 23 Osteon |
front 24 Cells in concentric rings within an osteon; trapped inside the matrix of compact bone | back 24 Osteocytes |
front 25 1. Where are osteoblasts located? 2. What substance do they secrete? 3. What is this substance? | back 25 1. Endosteum & inner cellular layer of periosteum 2. Osteoid 3. Precursor of bone |
front 26 Making the bone matrix (and thus bone formation) is a 2-step process. What are these 2 steps? | back 26 1. Secretion of the bone precursor, osteoid, from osteoblasts 2. Crystallization of hydroxyapatite (Ca++, Phosphorus) onto collagen fibers of osteoid |
front 27 Where do the minerals that form hydroxyapatite and complete the 2nd step of bone matrix formation come from? | back 27 Osteoblasts - as does the osteoid that comprises the 1st step in bone matrix formation |
front 28 What happens to some osteoblasts that get trapped in matrix? | back 28 -Stop secreting osteoid -Turn into osteocytes |
front 29 What function do the tiny canals that connect osteocytes serve? | back 29 Passage of nutrients & wastes |
front 30 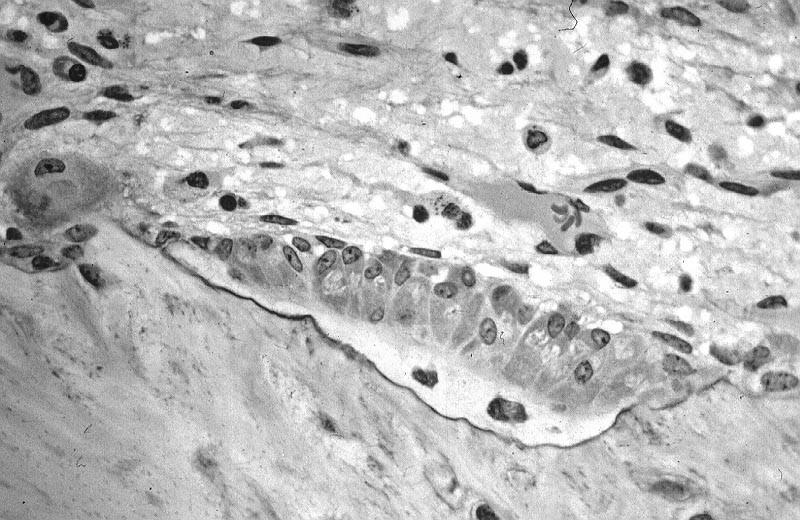 Identify which cells are osteoblasts (depositing osteoid) & which are osteocytes (trapped in osteoid) | back 30 1. White layer with 2 cells = osteocytes 2. Cells above white layer = osteoblasts |
front 31 Precursor cells, forming osteocytes; responsible for bone formation | back 31 Osteoblasts |
front 32 Multinucleate cells made from fusion of many macrophages; role is bone resorption | back 32 Osteoclasts |
front 33 When an osteoblast becomes an osteocyte (normal life cycle), does the activity increase or decrease? | back 33 Decreases (structure simplifies as well, since no need for organelles to secrete osteoid) |
front 34 Sequence of events for bone remodeling (3 steps) | back 34 1. Osteoclast attaches to bone & secretes acid (H+ ions) to dissolve bone underneath it 2. Osteoclast detaches from bone & moves on 3. Osteoblasts move into pit, secreting osteoid to build new bone |
front 35 Cluster of cells functioning as "Cutting Cones", like Big Bertha; tunneling machine | back 35 Osteoclasts |
front 36 Follow behind, zipping up & resealing tunnel left behind (bone formation) | back 36 Osteoblasts |
front 37 Can cause significant lag in between bone breakdown & bone formation | back 37 Insufficient building blocks (Ca++, phosphorus) |
front 38 Insufficient Ca++/phosphorus, which can create a lag between bone breakdown & formation, can lead to a situation not unlike what disease process? | back 38 Osteoporosis |
front 39 Induces more bone growth as a response | back 39 Chronic stress (i.e. exercise) - whereas a person who leads a sedentary lifestyle would have less bone growth/remodeling |
front 40 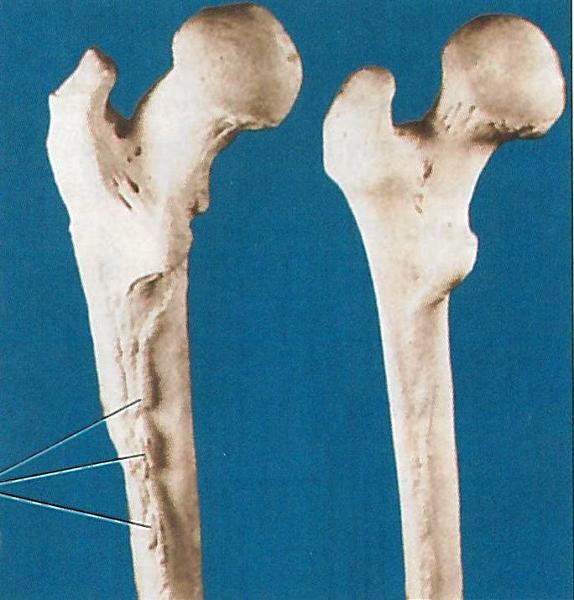 Which femur, left or right, is reflective of an individual who lived a sedentary lifestyle? | back 40 Right femur - less use of quads, which are attached to bone's ridge where growth is expansive on left femur |
front 41 Made up of lots of tiny struts of bone; space between struts filled with marrow | back 41 Spongy bone |
front 42 Tiny struts that form the composition of spongy bone | back 42 Trabeculi |
front 43 Since trabeculi surfaces are covered by endosteum, bone is deposited in __1__ layers, with the __2__ bone being the outermost layer | back 43 1. circular 2. youngest |
front 44 How do the trabeculi of spongy bone line up in relation to direction? How is this different in adults vs. infants/toddlers? | back 44 -Parallel to the direction of force (i.e. along stress lines) -Infants/toddlers don't put ambulatory stress on bones until much later in development |
front 45 Bone density condition increasing risk of fractures | back 45 Osteoporosis |
front 46 Bone disorder characterized by vitamin D deficiency in children; uncommon in developed countries | back 46 Rickets |
front 47 Caused by vitamin D or Ca++ deficiency in adults | back 47 Osteomalacia |
front 48 2 bone disorders which can result in bone deformations which aren't reversible | back 48 Rickets & osteomalacia |
front 49 Repair of broken bone is similar to bone development, but requires these 2 components | back 49 -Blood vessels -Chondrocytes |
front 50 4 steps of bone remodeling following fracture: | back 50 1. Blood forms hematoma - angiogenesis 2. Collagen deposited 3. Osteoblasts deposit temporary bone to stabilize break 4. Blasts & clasts work together to breakdown/rebuild |
front 51 After a fracture, after spongy bone is converted to compact bone, these cells perform the final "editing" | back 51 Osteoclasts |
front 52 Even though skeleton is bone, it still requires this as the foundation for its development | back 52 Cartilage |
front 53 Type of fracture caused by overuse r/t repetition | back 53 Stress FX |
front 54 Type of fracture where bone isn't broken all the way through | back 54 Incomplete FX |
front 55 Type of fracture where bone is broken all the way across | back 55 Complete FX |
front 56 Type of fracture where 2 pieces are still together | back 56 Nondisplaced FX |
front 57 Type of fracture where 2 pieces, or ends, are apart | back 57 Displaced FX |
front 58 Type of fracture that is broken or splintered into 3 or more fragments | back 58 Comminuted FX |
front 59 List fracture types from least to most severe | back 59 -Stress -Incomplete -Complete -Nondisplaced -Displaced -Comminuted |
front 60 Most common fracture site in body - due to a medial forceful thrust | back 60 Clavicle FX |
front 61 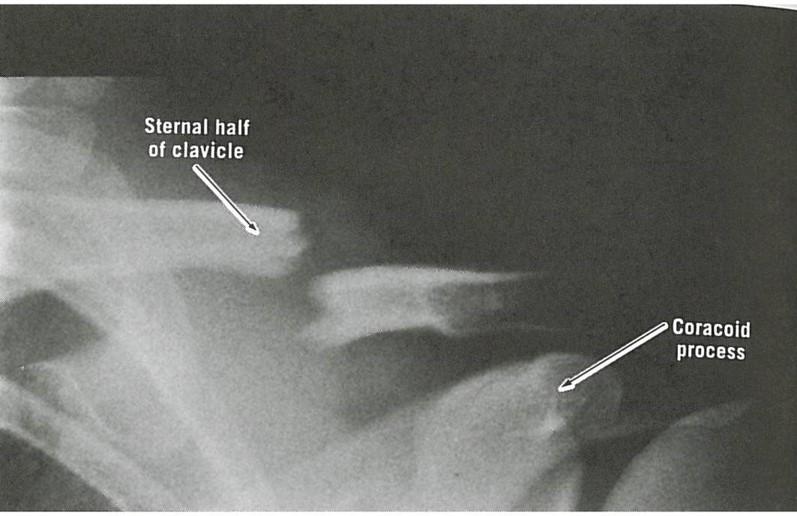 Note that distal end of clavicle sags, while proximal end is displaced upwards | back 61 No information... |
front 62 4 most clinically relevant bones | back 62 -Femur -Vertebrae -Radius -Ulna |
front 63 "Porous bone" - disease of the aged; more common in women | back 63 Osteoporosis |
front 64 Most common sites of FX's r/t osteoporosis | back 64 Neck of femur (hip) & spine |
front 65 DX tool for bone health; can be used to assess bone density for both hip & spine, which can predict risk of future FX's | back 65 DEXA scan (Dual-energy X-ray absorptiometry) |
front 66 Excellent DX tool to detect early signs of osteoporosis & estimate risk of future FX's | back 66 DEXA scan |
front 67 The World Health Organization (WHO) has adopted standards for bone health, called T & Z scores. While Z scores are measured in a percentile based on age & gender (similar to physical development of children), where having a Z score of 80% is better than 40%, T scores have 4 different classifications. What are these 4 classifications? | back 67 1. Normal bone: Better than -1 (w/in 10% of average) 2. Osteopenia: Between -1 & -2.5 (about 10-25% less) 3. Osteoporosis: Less than -2.5 (about 25% less) 4. Established (severe) osteoporosis includes presence of non-traumatic FX |
front 68 Under ideal circumstances, what's the best treatment for osteoporosis? Once diagnosed, what's the treatment regimen? | back 68 *Prevention (DEXA scan can show early density issues) -Diet high in vitamin D & Ca++ -Bisphosphonates (drug) -Exercise (stress = strength) |
front 69 18-month training program designed to add bone density to hips & vertebrae & strengthen lower extremities, mostly through resistance exercise, education & diet. This will reduce the risk of falls. | back 69 Osteo-cise |
front 70 Why does aging result in bone loss? | back 70 Balance shifts to bone resorption, & osteoclast activity isn't matched as well by osteoblast activity |
front 71 Abnormal spine curvature r/t compression FX's of multiple vertebrae | back 71  Kyphosis |
front 72  Normal MRI of spine vs. => | back 72  MRI of compression FX (see white arrow) |
front 73 Why is osteoporosis more common in women? | back 73 -Lower starting bone density -Loss of estrogen following menopause reduces bone deposition |
front 74 What 2 features complicate vertebral compression FX's? | back 74 1. Tilts superior vertebrae anteriorly (most common) 2. Ligaments adjust to shortened vertebrae, cinching down & locking it into place *Only SX can correct this |
front 75 The majority of vertebral FX's are located where? | back 75 Lumbar region |
front 76 As recent as 25 years ago, this FX was tantamount to a death sentence r/t how it was treated | back 76 Hip FX |
front 77 In a bad ankle sprain, this ligament is almost always the first to rupture | back 77 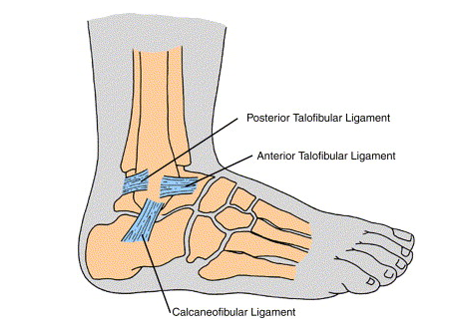 Anterior Talofibular Ligament (ATL) |
front 78 Ligaments do what when rested (opposite of muscles)? This means initially we'll passively rest, & then actively rest by doing resistance training in the foot (muscles & tendons of foot are strengthened, taking "load" off ligaments) | back 78 Shorten |
front 79 A ligament in this state, which usually occurs following injury, places the person at greater risk of another sprain | back 79 "Lax" ligament (loose, not allowed to shorten back to normal thru rest) |
front 80 3 of these; attach to ischial tuberosity; can avulse from bone (usually not all 3 due to amount of force required) at high speeds & with rapid acceleration & deceleration | back 80 Hamstrings |
front 81 Bone d/o of young adolescents; chronic injury characterized by painful lump just below knee; usually resolves w/rest | back 81 Osgood-Schlatter |
front 82 If you're considering Osgood-Schlatter as a DX, but a patient's symptoms are acute, what else must you consider? | back 82 Avulsion injury (Osgood-Schlatter has slow onset) |
front 83 Painful condition from irritation of the anterior tibia region; can involve posterior tibialis muscle; rapid increase in activity level increases risk, & rest is the treatment | back 83 Shin splints (medial tibial stress syndrome) |
front 84 What's the stress FX continuum? | back 84 Progression from chronic tendinitis => stress reaction => stress FX => bone FX (if S/S are ignored) |
front 85 Approximately 85% of body's metabolic activity & heat production come from these | back 85 Muscles |
front 86 Muscle repair is __1__ controlled and __2__ directed | back 86 1. Hormone 2. Blood |
front 87 Hormones involved in muscle remodeling | back 87 -GH (initiates repair) -Insulin-like growth factor-1 (IGF-1): finalizes repair |
front 88 Prime mover; muscle primarily responsible for given joint's action; if more than one muscle is involved, this is supplying the most force | back 88 Agonist (muscle) |
front 89 Muscle that opposes prime mover (agonist) at a joint | back 89 Antagonist (muscle) |
front 90 Muscle that works w/agonist to further muscle action | back 90 Synergist |
front 91 This muscle type is found on the opposite side of a limb or the body | back 91 Antagonist (muscle) |
front 92 Muscles must overcome these 3 forces | back 92 1. Gravity 2. Inertia 3. Force of opposing muscle group |
front 93 How is a joint, say the knee, stabilized during exercise or activity? | back 93 Agonist & antagonist muscles cooperate to stabilize it |
front 94 How do muscles show efficiency of patterned movement, such as when running? | back 94 Quads are first activated when running, then hamstrings *Cooperating by not getting in each other's way |
front 95 What are the 3 types of skeletal muscle? | back 95 Type I: Slow twitch Type IIa: Fast twitch endurance (FO) Type IIb: Fast twitch power (FG) |
front 96 Between the 3 skeletal muscle types (ST/FO/FG), give the size of each | back 96 ST: small FO: medium FG: large |
front 97 1. Which of the 3 skeletal muscle types would be called upon for minimal work? 2. What about for a heavy load or when other fibers are fatigued? | back 97 1. Slow twitch (ST) 2. Fast twitch power (FG) |
front 98 Attach muscle to bone | back 98 Tendons |
front 99 Attach bone to bone | back 99 Ligament |
front 100 Why does healing take so long with ligament/tendon damage? | back 100 Blood vessels absent or sparse |
front 101 A muscle tear; usually graded | back 101 Strain |
front 102 Injury to a ligament r/t overstretching | back 102 Sprain |
front 103 Classic tendon structure | back 103 Tendon => muscle => tendon |
front 104 What's the name for a mild Achilles injury? What's the treatment? | back 104 -Peritendinosis -Ice & grabbing cord from base & pulling up several times to break up adhesions |
front 105 Longest tendon of the body | back 105  IT band (connects from hip to lateral knee) |
front 106 Tendons with wide, sheet-like attachments in which the attachment of a broad, flat muscle occurs over a wide area; found primarily in the lower back, ABD wall, skull, palms of hands & soles of feet | back 106 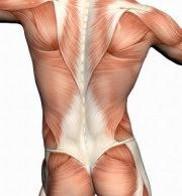 Aponeuroses |
front 107 Muscle that acts to flex the spine; important for posture; encased in a sheath formed from 3 aponeuroses | back 107 Rectus abdominus |
front 108 Prime flexor of the elbow; contributes most force to flexion | back 108 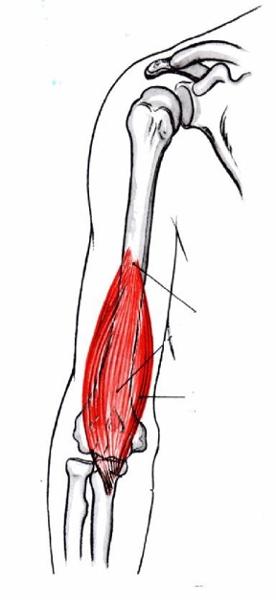 Brachialis |
front 109 Synergistic flexor of elbow; supinates forearm | back 109 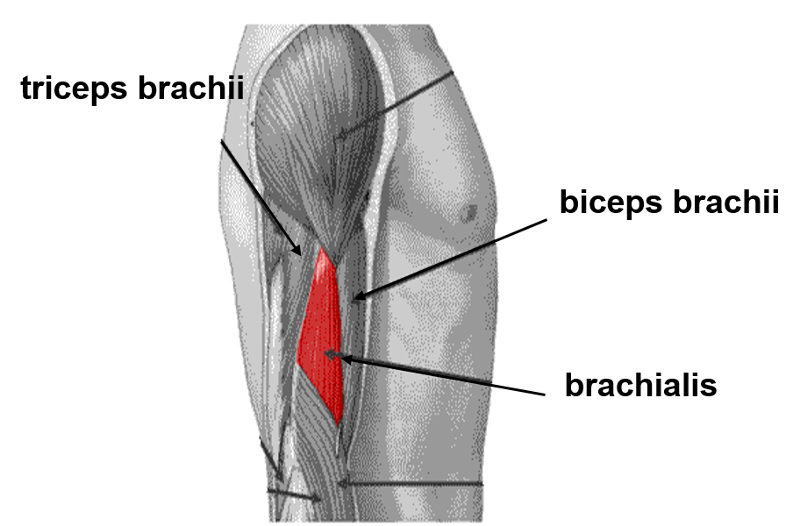 Biceps brachii |
front 110 Extensor; extends elbow | back 110 Triceps brachii |
front 111 Muscle group (4); extend knee & flex hip | back 111 Quadriceps |
front 112 The quads are innervated solely by this nerve | back 112 Femoral nerve |
front 113 Muscle group (3); flex knee & extend hip | back 113 Hamstrings |
front 114 The __1__ is the prime move of plantar flexion, while the __2__ is the prime mover when the knee is extended | back 114 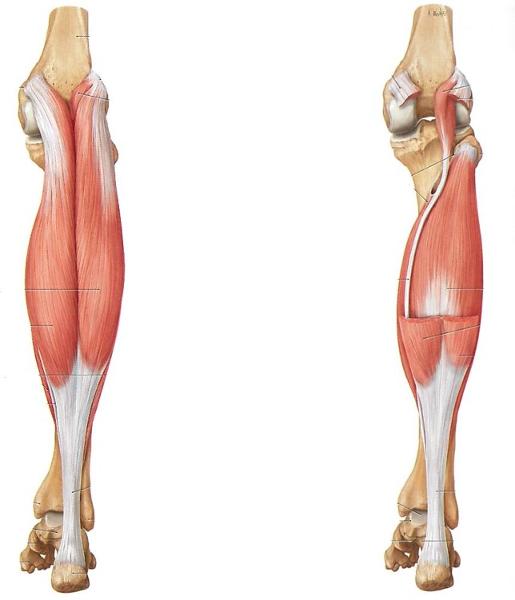 1. Soleus (right) 2. Gastrocnemius (left) |
front 115 Prime mover of dorsiflexion; flexes big toe; sometimes source of shin splints | back 115 Tibialis anterior |
front 116 What's the concept of "remote control" in relation to muscles, and what are some examples? | back 116 -Muscles having role in multiple joints -TFL, plantaris, & peroneus longus |
front 117 Leading cause of lateral knee pain | back 117 IT Band Syndrome |
front 118 Two muscles which become one (level of the femur); strongest of muscles that flex hip | back 118 Iliacus & psoas (iliopsoas - hip flexors) |
front 119 Muscle that sits over sciatic notch that causes sciatica when inflamed | back 119 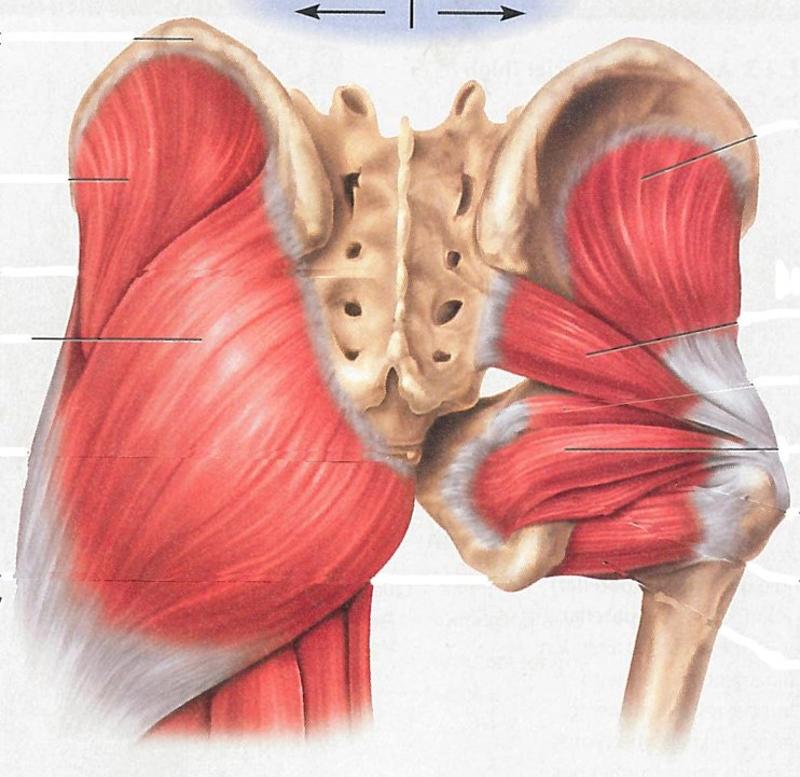 Piriformis (middle right attaching to mid-sacrum) |
front 120 Longest nerve in body - extending from hip to foot | back 120 Sciatic nerve |
front 121 What are some causes of back pain resulting from straining the paraspinal muscles? | back 121 -Lifting/twisting -Poor fitness -Overuse |
front 122 1. Piriformis syndrome can lead to this 2. Treatments include... | back 122 1. Sciatica (lower back pain) 2. RICE, NSAID's, rolling out area, ultrasound TX |
front 123 Thin membrane lining joint cavity; nourishes & lubricates articular cartilage | back 123 Synovial membrane |
front 124 Deepens socket (labrum) or acts as wedges for a better fit between bones | back 124 Fibrocartilage |
front 125 Fluid-filled sac that cushions space between tendons & bones | back 125 Bursa |
front 126 Sleeve-like, loose fibrous layer attached to articulated surfaces | back 126 Capsule |
front 127 Provides GLASSY surface to reduce friction between bones | back 127 Articular cartilage |
front 128 "Shrink-wrapping" tissue which prevents tendons from bowstringing away from bone | back 128 Retinaculum |
front 129 Arrangement of ligaments along most joints for directional support | back 129 Cross-stitch |
front 130 Perforating fibers of periosteum, which penetrate bone & help attach tendon | back 130 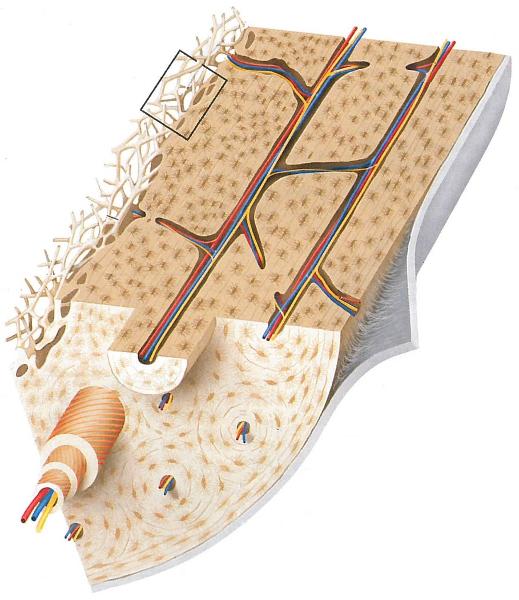 Sharpey fibers (under flap) |
front 131 When bursa are wrapped around a tendon, what are they called? | back 131 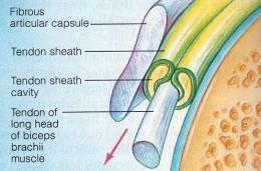 Tendon sheath |
front 132 Bursitis is most common in this joint | back 132 Shoulder |
front 133 Increased amount of joint fluid in response to infection, inflammation, crystals, or increased friction is called: | back 133 Effusion |
front 134 Consists of fibrous connective tissue; lined inside with synovial membrane | back 134 Capsule |
front 135 Large class of inflammatory disorders in synovial joints | back 135 Arthritis |
front 136 Chronic degenerative disease caused by loss of articular cartilage; distinguished by its lack of inflammation, despite the "itis" suffix | back 136 Osteoarthritis |
front 137 TX for bursitis | back 137 RICE, NSAID's (ABX if infection present) |
front 138 Carpal tunnel TX | back 138 -Wrist brace to limit movement -Cortisone injections -SX (last resort) |
front 139 Joint designed for ROM, not stability | back 139 Shoulder |
front 140 Clinically significant joint; very mobile, yet unstable, gets dislocated often | back 140 Glenohumeral joint (shoulder) |
front 141 Strongest joint of the body | back 141 Hip joint (more than 1/2 of femoral head in acetabulum) |
front 142 A shoulder dislocation occurs when the __1__ comes out of its __2__ socket; 95% of the time, the shoulder is dislocated __3__; treatment is a __4__, followed by immobilization (sling) and rest | back 142 1. Humerus 2. Glenoid 3. Anteriorly 4. Reduction (replacing arm in shoulder joint) |
front 143 Largest, most complex joint in body; strength depends mostly on ligaments, muscles, and tendons | back 143 Knee (femur & tibia - not fibula) |
front 144 This bone is a sesamoid bone, meaning it's within a tendon | back 144 Patella |
front 145 How can you test for an ACL injury? | back 145 Move tibia forward (drawers test) |
front 146 "Unhappy triad" of ACL injuries | back 146 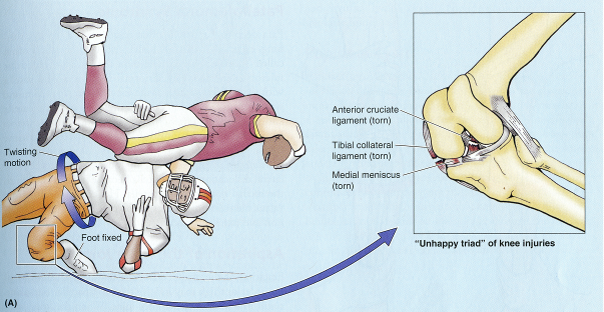 Tear of ACL, tibial collateral ligament, & medial meniscus |
front 147 Articular cartilage & bone wear away; common in weight bearing joints, distal finger joints, & hips | back 147 Osteoarthritis (OA) |
front 148 1. What activities reduce symptoms r/t osteoarthritis? 2. What medications are helpful? | back 148 1. Exercise - such as swimming & aquajogging 2. Embrel (cytokine inhibitor) and/or NSAID's |
front 149 Autoimmune form of arthritis | back 149 Rheumatoid arthritis (RA) |
front 150 The ligaments that stabilize the __1__ joint stretch during pregnancy due to secretion of __2__ | back 150 1. Sacroiliac (SI) joint 2. Relaxin |
front 151 This huge, superficial group of 3 muscles are the common site of back strains r/t heavy lifting, twisting, or sudden movement | back 151 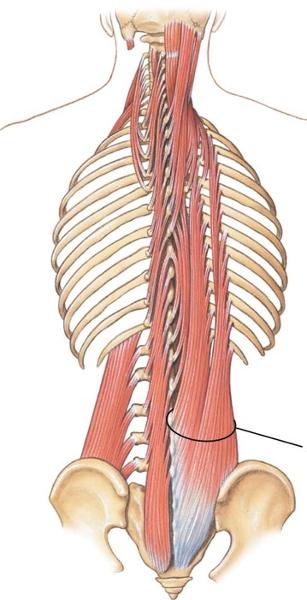 Erector spinae |
front 152 Technical name for "runner's knee" | back 152 Patellofemoral Syndrome |
front 153 The peripheral nervous system consists of these 2 components | back 153 -Nerves (bundles of axons) -Ganglia (groups of neuronal cell bodies) |
front 154 A neuron consists of these 3 parts | back 154 -Dendrite (receives input from other neurons) -Axon body -Axon terminal (releases neurotransmitter) |
front 155 Part of neuron that receives information from other neurons | back 155 Dendrite |
front 156 Part of neuron that releases neurotransmitter | back 156 Axon terminal |
front 157 The message being transmitted by neurotransmitters is a mix of these two types of messages | back 157 Excitatory & inhibitory |
front 158 What determines whether a neuron will fire? | back 158 Sum of excitatory & inhibitory neurons (more excitatory = fire) |
front 159 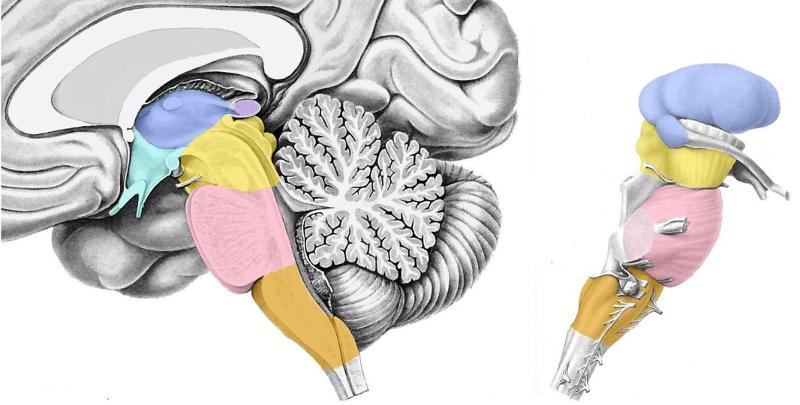 Locate the following: -Thalamus -Hypothalamus -Midbrain -Pons -Medulla | back 159 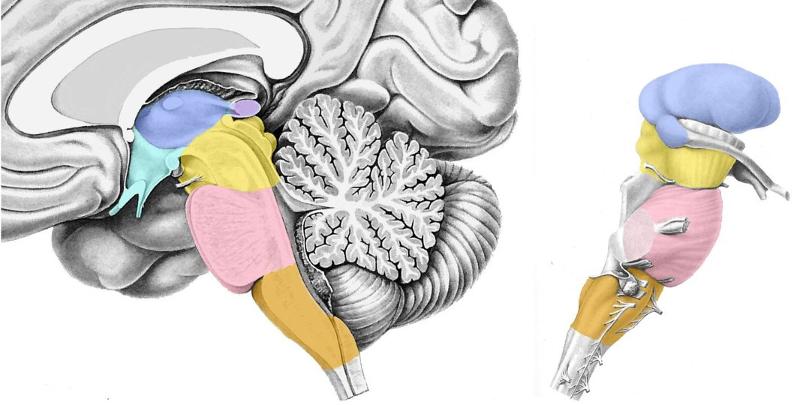 In order of descending colors (hypothalamus is under & to right of thalamus - colored green) *Lateral view to right is also descending, but hypothalamus not pictured - so skip |
front 160 Relays information to cerebral cortex; a left & right side, which are completely independent of each other | back 160 Thalamus |
front 161 Deals with "housekeeping"; temp control, BP, thirst/appetite, sex drive, & lactation | back 161 Hypothalamus |
front 162 The brainstem is divided into these 3 parts | back 162 -Midbrain -Pons -Medulla |
front 163 Posterior & inferior to cerebral cortex; mostly involved in motor control | back 163 Cerebellum |
front 164 Largest part of brain | back 164 Cerebral cortex |
front 165 Depression or fissure in the surface of the brain | back 165 Sulcus |
front 166 Ridge on the surface of the brain | back 166 Gyrus |
front 167 This colored matter forms the exterior of the cerebral cortex | back 167 Gray matter surrounds white matter |
front 168 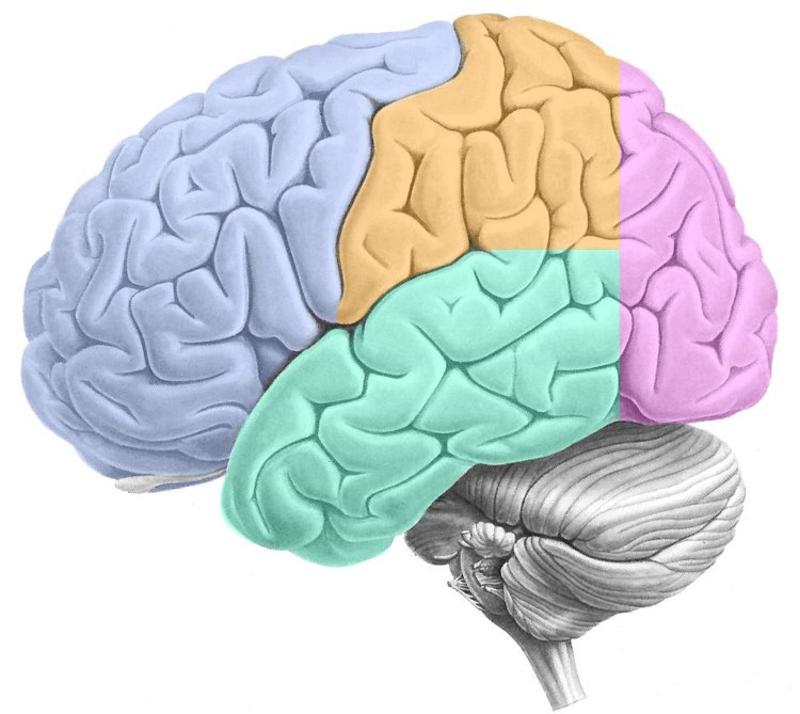 ID the following: -Frontal lobe -Parietal lobe -Occipital lobe -Temporal lobe -Central sulcus | back 168 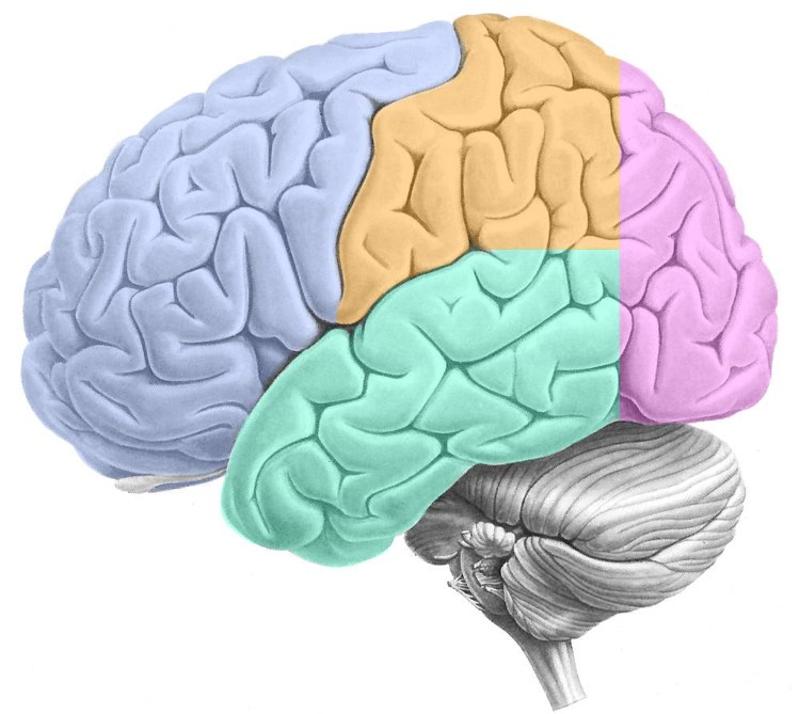 Frontal: Purple opposite side of cerebellum Parietal: Orange behind frontal Occipital: Purple above cerebellum Temporal: Green under frontal/parietal Central sulcus: Crease between frontal & parietal |
front 169 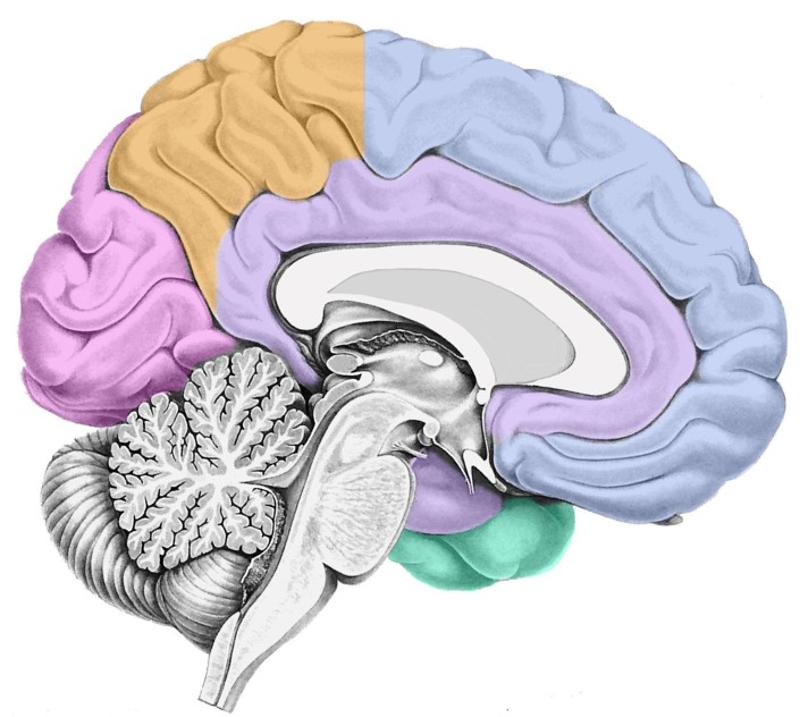 Locate the limbic lobe | back 169  Surrounds corpus callosum |
front 170 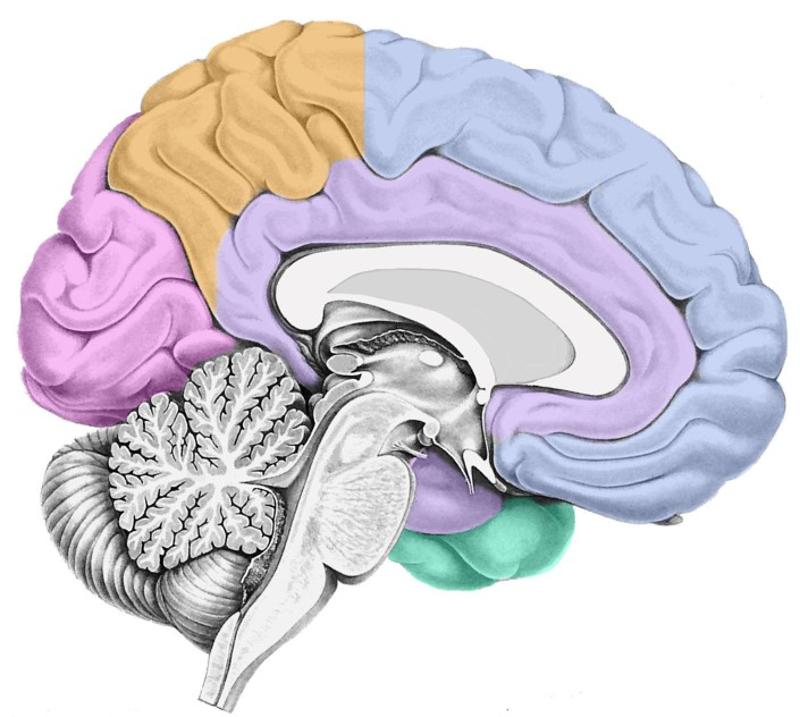 Locate the hippocampus *What lobe is it part of? | back 170  Inferior portion of limbic lobe that swings back & under corpus callosum towards cerebellum |
front 171 Generally considered the part of the cortex most susceptible to seizures | back 171 Hippocampus |
front 172 Responsible for forming long-term memories (not storing!) | back 172 Hippocampus |
front 173 Tube embedded in temporal bone; filled with fluid; receives sound waves which excite auditory receptor cells (hair cells) | back 173 Cochlea |
front 174 Therapy for total deafness; excite auditory neurons in the auditory relay nucleus (cochlea) directly | back 174 Cochlear implant (hearing aid) |
front 175 Where does auditory information go once it's received by the cochlea & transferred to CN VIII? | back 175 -Sent to nucleus at junction of pons & medulla -Travels up to Thalamus -Then to both left & right primary auditory cortices (AI) |
front 176 Why would a person suffering damage to one hemisphere of the auditory cortex (left or right) not necessarily experience deafness in either ear? | back 176 Signals from each side are collected bilaterally, so damage to the right wouldn't stop information from left reaching right cortex |
front 177 Essential for language comprehension (spoken or written); damage here causes _____'s aphasia, resulting in inability to comprehend language, although individual can still speak | back 177 Wernicke's area (Wernicke's aphasia) |
front 178 Type of aphasia resulting in patient being unable to comprehend language, although they're still able to speak | back 178 Wernicke's aphasia (lesion to Wernicke's area) |
front 179 Essential for language production (speech or writing); damage here will result in speech production being limited, from modest deficits in sentence generation to complete inability to speak | back 179 Broca's area (Broca's aphasia) |
front 180 Probably more r/t language comprehension than production; located posterior & superior to Wernicke's area | back 180 Angular gyrus |
front 181 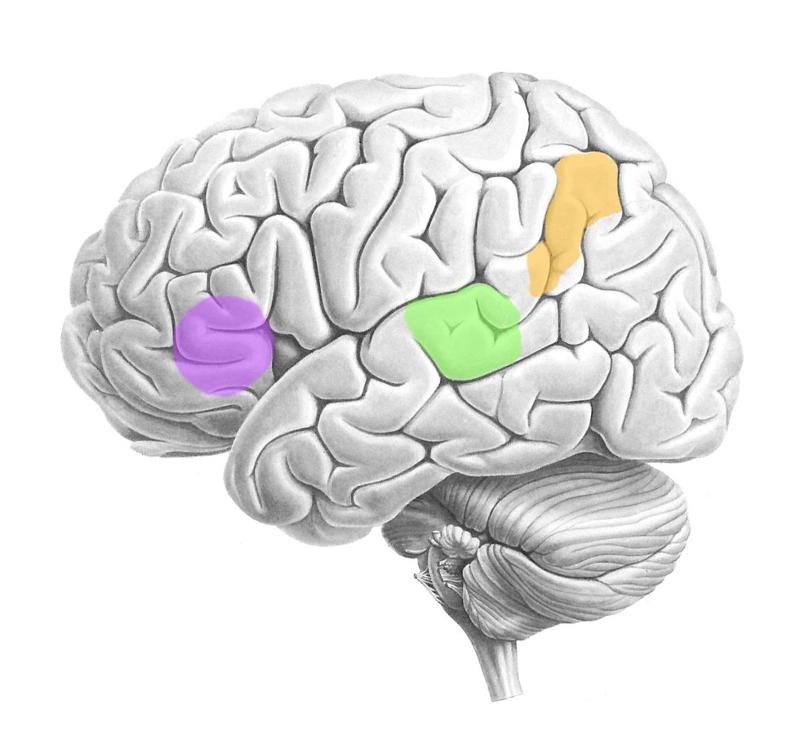 ID the following: -Wernicke's area -Broca's area -Angular gyrus | back 181 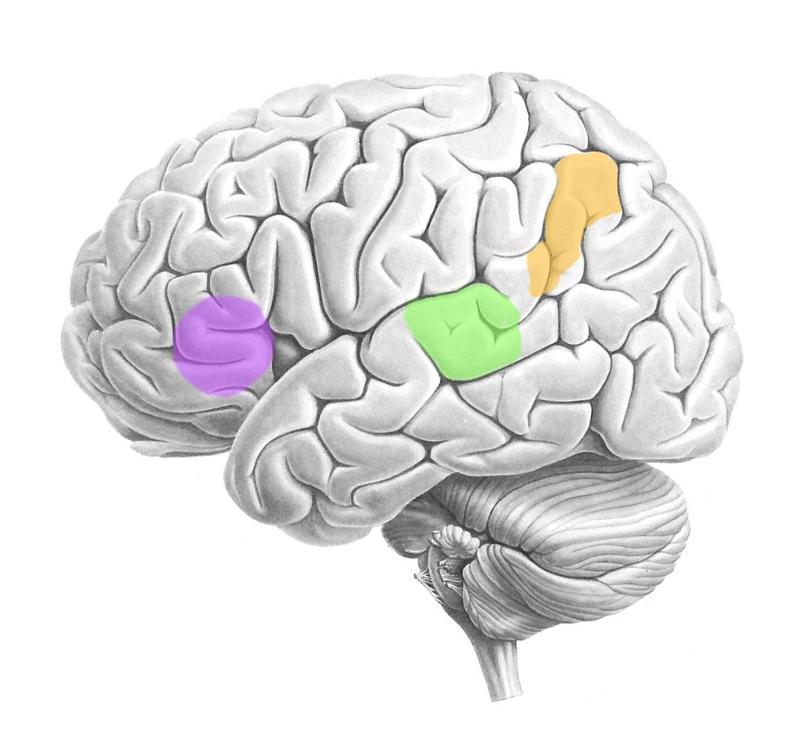 Wernicke's area: Green (temporal lobe) Broca's area: Purple (frontal lobe) Angular gyrus: Orange (parietal lobe) |
front 182 These areas are found only in the left hemisphere in almost all right-handed people & about 70% of left-handed people | back 182 Wernicke's, Broca's, Angular gyrus |
front 183  A person with a lesion in this region may suffer from what disorder? | back 183  Anomia - patient can't remember names of common objects or famous people |
front 184 If a person suffering from anomia (caused by lesion of temporal lobe), and they were shown a comb, how would they describe it? | back 184 They'd be able to describe what it's used for, but not be able to remember its name |
front 185 Where's the primary visual cortex (VI) located? | back 185 Occipital lobe |
front 186 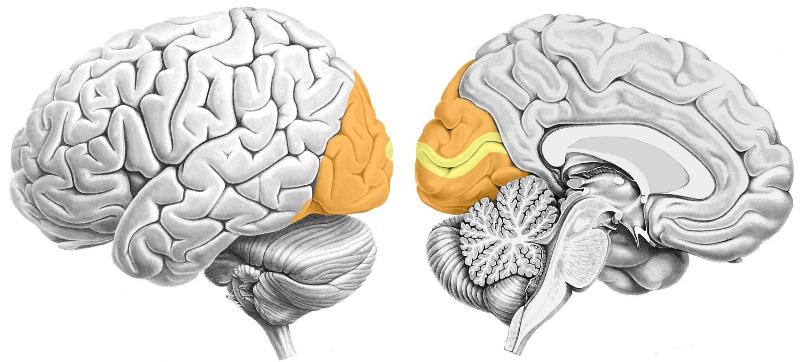 What sensory cortex is part of this lobe? | back 186 Primary visual cortex & higher-order visual cortex (occipital lobe) |
front 187 Sheet of neurons lining 2/3 of the eye | back 187 Retina |
front 188 Outermost layer of the retina | back 188 Rods & cones |
front 189 Innermost layer of the retina | back 189 Relay neurons whose axons form the optic nerve |
front 190 Where is the first visual relay in the brain? | back 190 Thalamus |
front 191 Where do axons cross in the visual pathway? | back 191 Optic chiasm |
front 192 Optic nerve axons (50%) that cross the optic chiasm send information to this cortex | back 192 Contralateral visual cortex |
front 193 Optic nerve axons (50%) that don't cross the optic chiasm send information to this cortex | back 193 Ipsilateral visual cortex |
front 194 Rule for visual system: 1. Information from the right half of the visual field goes to what half of the brain? 2. Info from the left half of visual field goes to what half? | back 194 Right visual => left half brain Left visual => right half brain |
front 195 Sees right visual field | back 195 Left visual cortex (occipital lobe) |
front 196 Sees left visual field | back 196 Right visual cortex (occipital lobe) |
front 197 1. What would happen if a lesion occurred along the optic nerve prior to the optic chiasm? 2. What if the lesion occurred after the optic chiasm (closer to visual cortex in occipital lobe)? *Picture on reverse side | back 197 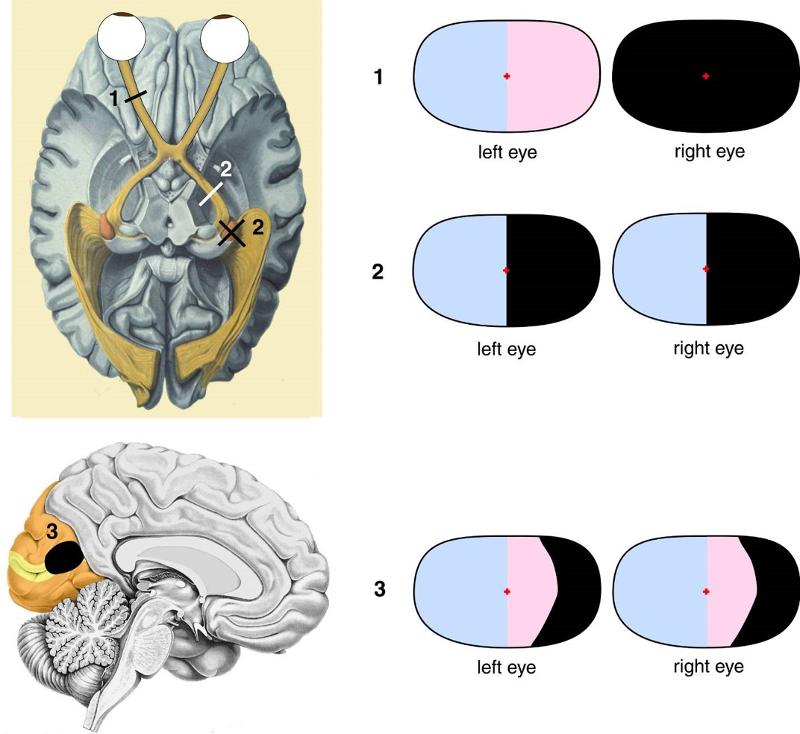 1. The side of the lesion would be blind 2. If the left tract had a lesion, the right half of each eye's field of vision would be gone |
front 198 Caused by atherosclerotic-like deposits that build up behind the retina on the central region; responsible for high visual acuity (foveal vision) needed to read books, look at pictures, & other fine detail activities | back 198 Macular degeneration |
front 199 While the spinal cord is part of the CNS, its projections, the _____ _____ _____, are part of the peripheral nervous system | back 199 Dorsal root ganglia |
front 200 The spinal cord is shorter than the vertebral column: 1. What's the space inferior to the spinal cord called? 2. What's it useful for? | back 200 1. Lumbar cistern 2. Injecting drugs or drawing CSF for testing |
front 201 Color of the outer layer of the spinal cord | back 201 White matter surrounding gray matter |
front 202 Part of peripheral nervous system containing cell bodies of somatosensory neurons | back 202 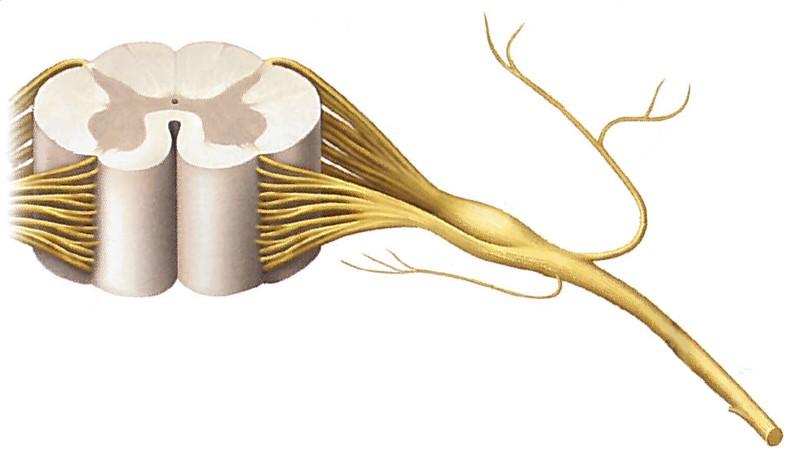 Dorsal root ganglion (just before dorsal roots connecting to spinal cord) |
front 203 The central axonal branch of each __1__ neuron runs up the spinal cord in the __2__ matter; these axons make up a tract called the _____ 3 _____ | back 203 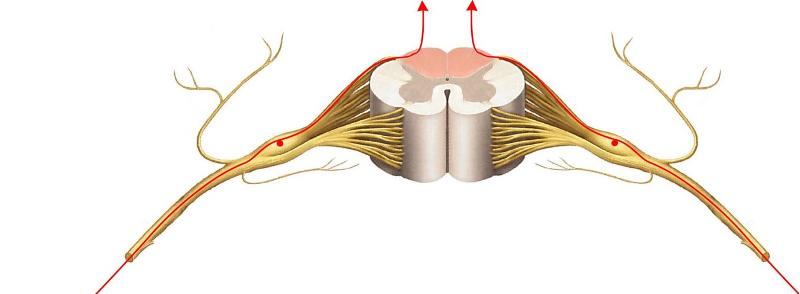 1. Touch 2. White 3. Dorsal columns (pink highlights between dorsal horns) |
front 204 How does touch pathway convey information? | back 204 1. One axonal branch to skin detects touch 2. One axonal branch through white matter to brain stem (medulla) 3. Goes to 2nd relay in thalamus 4. Cross on way primary somatosensory cortex (SI) |
front 205 Touch information from the left side of the body will terminate where? | back 205 Right primary somatosensory cortex (SI) - pathway crosses after thalamus |
front 206 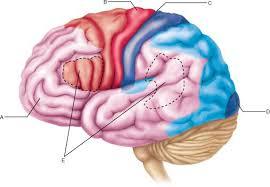 1. What's the red area? 2. What's the blue area behind it? 3. What separates the two? | back 206 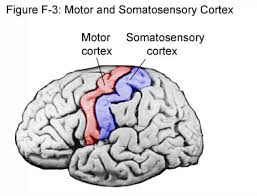 1. Primary motor cortex (red) 2. Primary somatosensory cortex (SI - blue) 3. Central sulcus |
front 207 As the touch relay pathway travels up the axonal branch in the white matter of the spinal cord, what 2 relay points does it hit before reaching the primary somatosensory cortex (SI)? | back 207 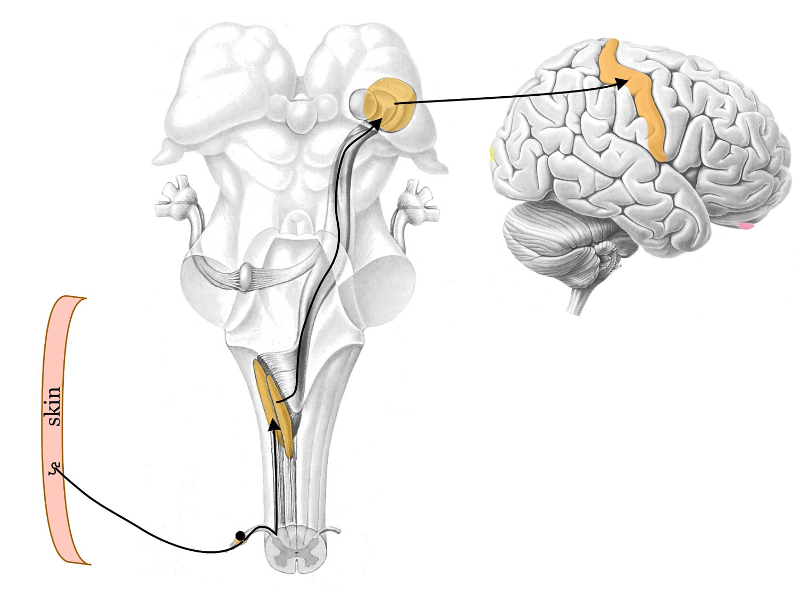 1. Relay nucleus in brainstem (medulla) 2. Relay nucleus in thalamus |
front 208 Pathway for touch relay pathway is same for face with one exception - touch neurons have cell bodies in the __1__ ganglion, and the 1st relay occurs in the __2__ of the brainstem, not the __3__ | back 208 1. Trigeminal 2. Pons 3. Medulla |
front 209 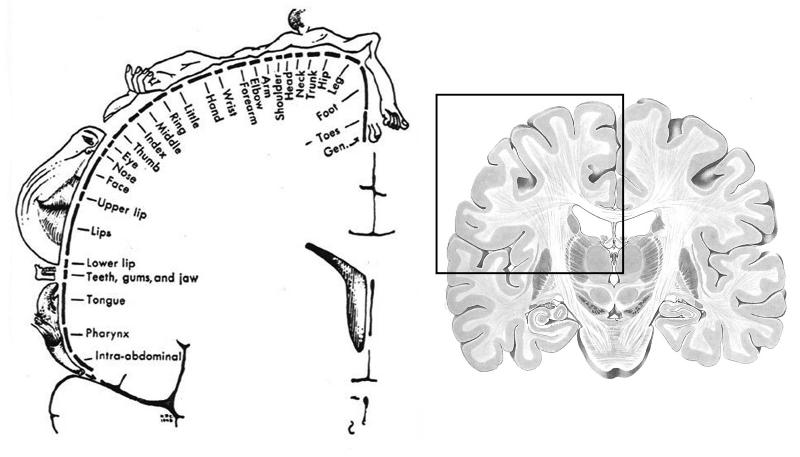 1. What's the image on the left depicting? 2. If this is an anterior view, what would happen if a lesion occurred where "leg" is mapped? | back 209 1. Somatotopic "touch" map for SI (primary somatosensory cortex) 2. This would depict right side of SI, so there would be touch deficit in left leg |
front 210 Deficits resulting from a lesion in the primary somatosensory cortex (SI), which would be localized to opposite side using somatotopic "touch" map (i.e. leg, arm, GI, etc.), would produce what potential deficits? | back 210 -Lose ability to accurately locate touch/pinprick -Lose ability to ID objects by feel -Lose ability to ID a letter/number drawn by an examiner on hand |
front 211 Most of the axons in the pain/temperature pathway are of this variety | back 211 Nociceptive |
front 212 Believed to be the major pain-processing area in the cortex | back 212 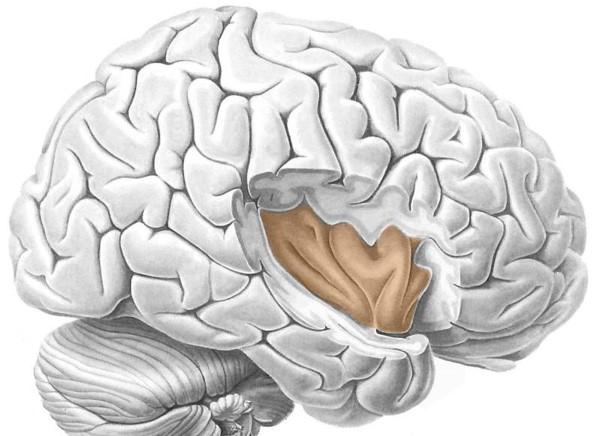 Insula |
front 213 1. All pain/temp neurons in the face & head have cell bodies in what ganglion? 2. Where does information travel to from this ganglion? 3. What's different from touch relay pathway? | back 213 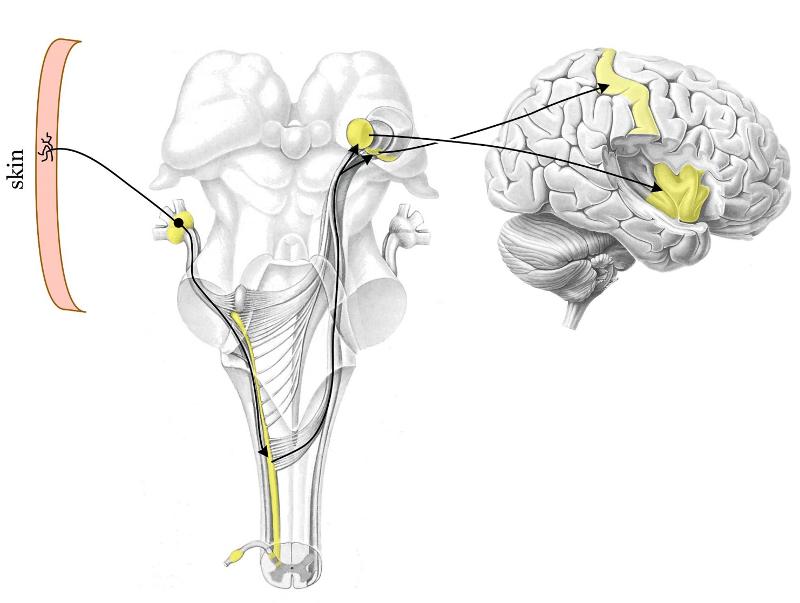 1. Trigeminal 2. Thalamus (not same part as touch pathway) 3. Some info goes to SI for general pain location, but most goes to insula to process pain |
front 214 Whereas the face/head nociceptors have their cell bodies in the trigeminal ganglion, the body's nociceptors house their cell bodies in the _____ ganglia | back 214 Dorsal root |
front 215 1. First "relay nucleus" for body's pain reception 2. Message then travels along this highway 3. The highway ends here | back 215 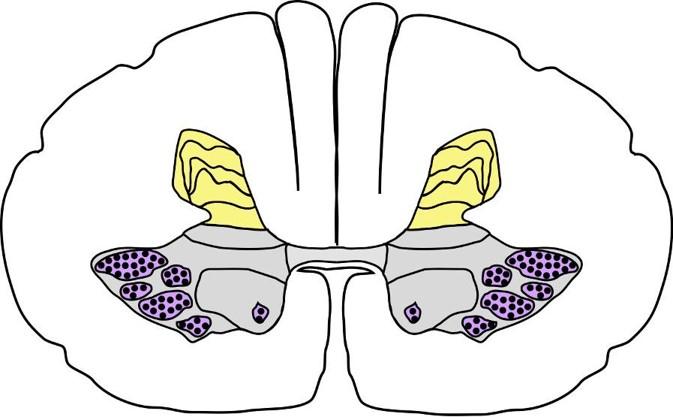 1. Dorsal horn (yellow) 2. Spinothalamic tract (through entire brainstem) 3. Thalamus |
front 216 Dull pain nociceptors are activated by strong mechanical stimulation, intense heat/cold, & these substances | back 216 -Histamine -Prostaglandin -Serotonin |
front 217 When a dull pain nociceptor is activated, it not only fires spikes, but also releases a peptide, __1__ from its own endings; this peptide stimulates __2__ cells, producing __3__. Substances (histamine, prostaglandin, serotonin) further stimulate nociceptor, which continues to fire even after stimulus is gone; this is why dull pain nociceptors generate prolonged pain & contribute to inflammation | back 217 1. Substance P 2. Mast cells 3. Histamine |
front 218 A person with a herniated disc will have these 2 kinds of pain | back 218 1. Low back pain from trauma/inflammation of local connective tissue (ligaments, etc.) 2. Pain radiating down associated dermatome (squeezing causes axons to fire - brain interprets as pain from dermatome) |
front 219 Why do narcotic drugs relieve pain? | back 219 Mimic pain suppression neurotransmitters coming from midbrain, which inhibit nociceptors in dorsal horn (neurotransmitters similar to opiates) |
front 220 "Unhealthy" pain; not caused by tissue injury, but CNS changes, such as damage to part of pathway; chronic & not easily controlled | back 220 Neuropathic pain |
front 221 All motor neurons send their axons out to where? | back 221 Skeletal muscles (cause contraction) |
front 222 Cell bodies of motor neurons are located where? | back 222 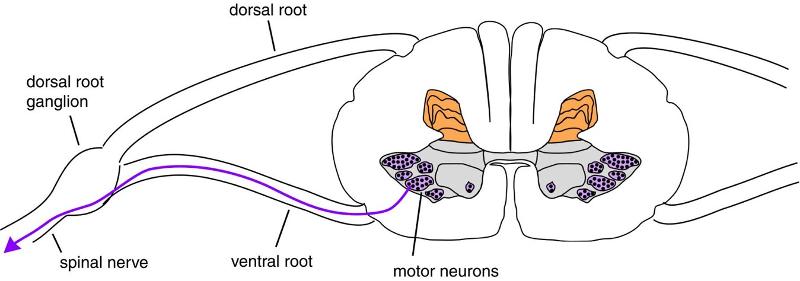 Ventral horn of the spinal cord (blue) |
front 223 How are motor neurons arranged in the spinal cord? | back 223 In groups - each group corresponds to a particular muscle |
front 224 Motor neurons that control muscles of the face/head have their cell bodies in the __1__; their axons go out to their muscle targets via _____ 2 _____. | back 224 1. Brainstem 2. Cranial nerves |
front 225 The descending motor pathway crosses over to the contralateral side of the spinal cord just below this structure | back 225 Medulla (bottom of brainstem) |
front 226 Corticospinal tract carrying signals from the right motor cortex will run through the spinal cord on which side? | back 226 Left side |
front 227 A patient with damage to their left motor cortex will have motor symptoms appear on what side of their body? | back 227 Right side of body (opposite) |
front 228 There is an elaborate mechanism in the brainstem & cortex for controlling eye movements. The master controller in the brainstem is a large bulge on the dorsal surface of the midbrain, called the: | back 228 Superior colliculus |
front 229 Information from vestibular hair cells, located in the otolith organs, send information to brainstem via 1) what ganglion, and 2) where do they travel? | back 229 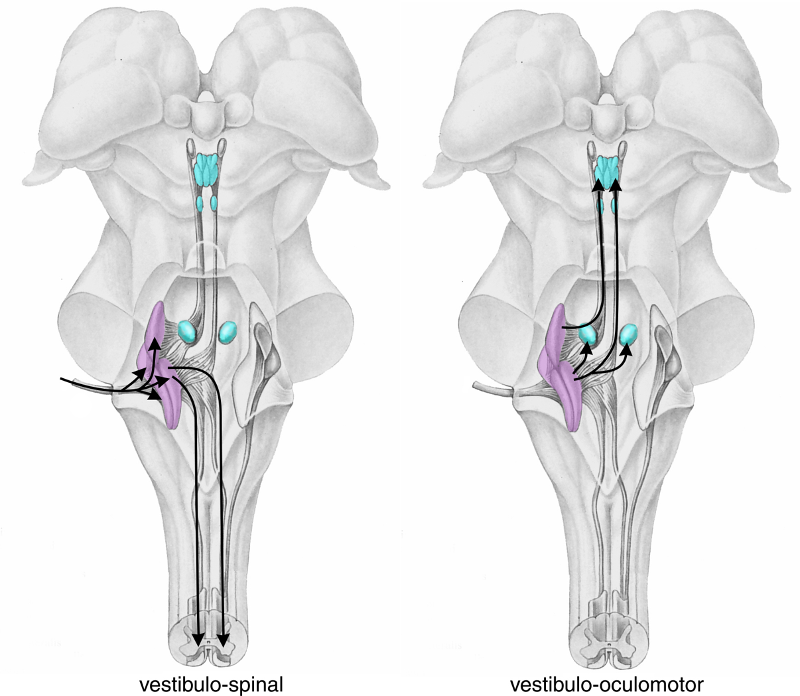 1. Scarpa's ganglion 2. Vestibular nuclei (purple - middle) |
front 230 This reflex cancels out the unintended head rotation that results from activities such as walking (foot strikes ground), causing eyes to rotate in opposite directions to stabilize image on retinas; suppressed during intentional head rotation | back 230  Vestibulo-ocular reflex |
front 231 Damage to cerebellum causes what type of problems? | back 231 Motor (largest input by far to cerebellum is from gray matter forming base of pons - which deals heavily with motor response) |
front 232 An information loop exists between the motor cortex & cerebellum; since the motor cortex is a crossed system, but the cerebellum isn't, how many times do the connections in the loop cross the midline? | back 232 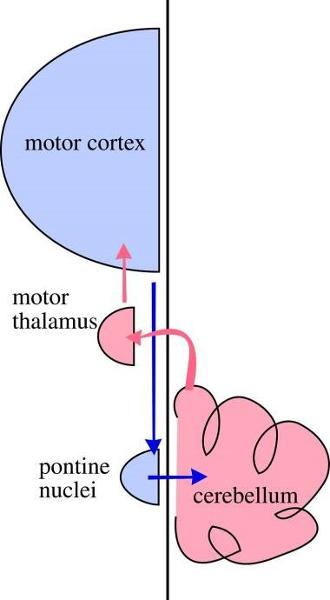 Twice |
front 233 Damage to the medial portion of the cerebellum, or vernis, may cause this motor problem | back 233 Instability when standing (i.e. swaying when stationary, or when eyes are closed, patient unable to stay upright) |
front 234 1. What test, when performed, will yield these results if positive? -Movements too large -Patient has intentional tremor - hand oscillates with extension, but no tremor at rest -Movement broken down into smaller movements (sequential) 2. What is the probable diagnosis? | back 234  1. Asking patient to alternately touch provider's finger & then own nose 2. Cerebellar ataxia (bottom of pic) |
front 235 Patient's with cerebellar disease will exhibit what characteristic r/t their gait? | back 235 Wide-base with staggering & reeling |
front 236 The function of this brain region is to encourage or strengthen movements - gives a "boost" to commands from motor cortex, lest they miss this area & be weak/feeble | back 236 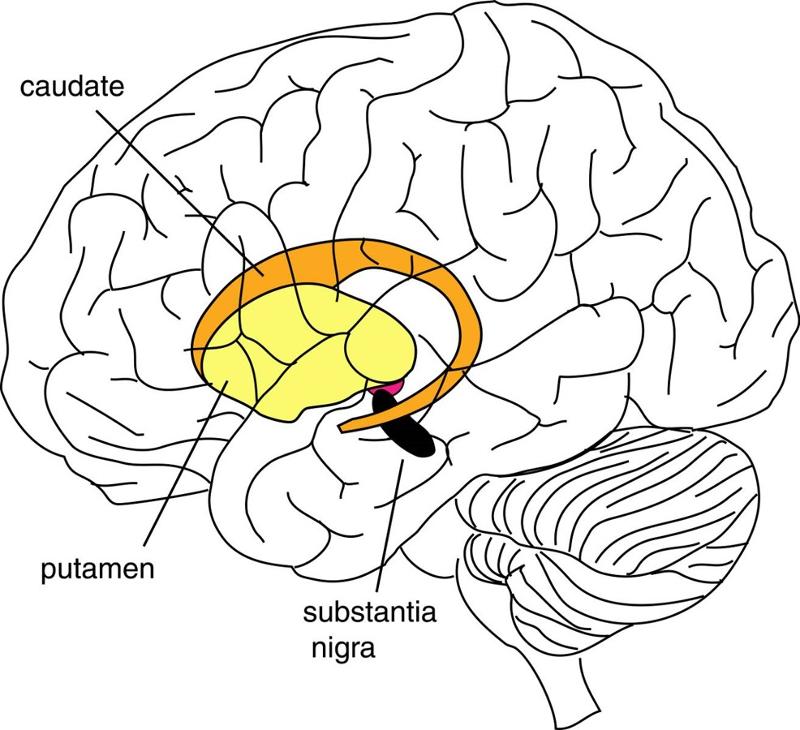 Basal ganglia |
front 237 The substantia nigra, part of the basal ganglia, enhances movement through exciting the striatum (and other parts of basal ganglia). Its neurons use __1__ as its neurotransmitter, and in __2__ disease, these neurons mostly die, resulting in difficulty moving and weakness; slow & progressive | back 237 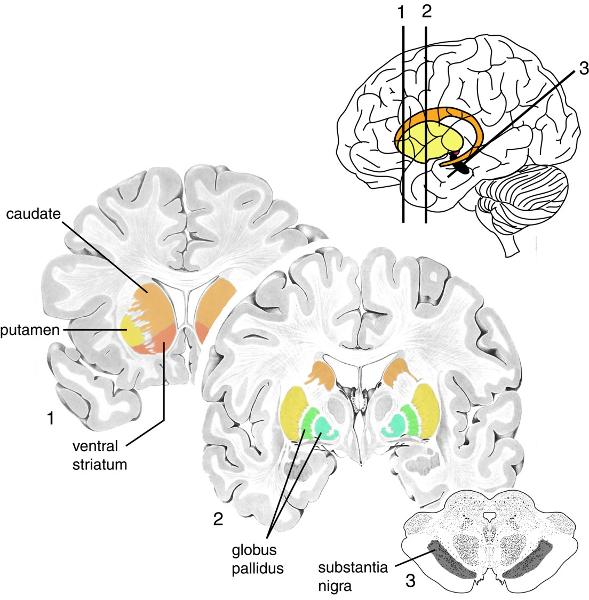 1. Dopamine 2. Parkinson's disease |
front 238 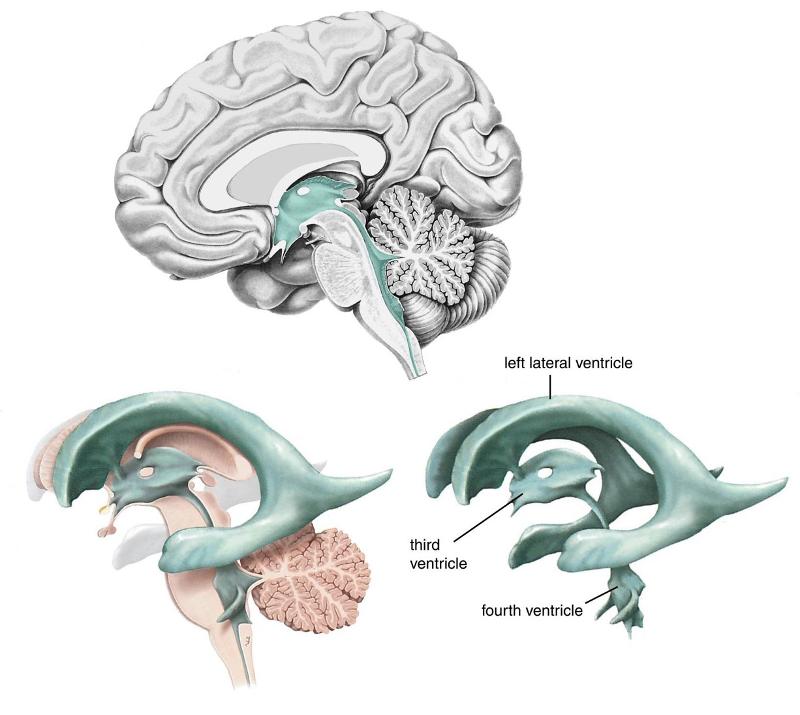 ID the following: -Left lateral ventricle (right hidden) -4th ventricle -3rd ventricle | back 238 No information |
front 239 CSF flow starts in the __1__ ventricles, then thru the __2__ ventricle & into a tube that leads to the __3__ ventricle, also called the _____ 4 _____; it then exits to bathe the brain & spinal cord | back 239 1. Lateral 2. 3rd 3. 4th 4. Cerebral aqueduct |
front 240 Which 2 routes of blood into the brain are essential for it to function? | back 240 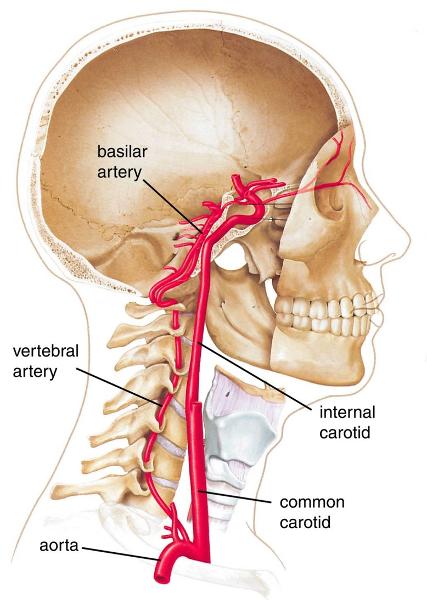 1. Vertebral arteries (threaded through cervical vertebrae) 2. Internal carotid |
front 241 This vessel is clinically important because a rupture of one of its branches may result in a hematoma, which can compress the cortex | back 241 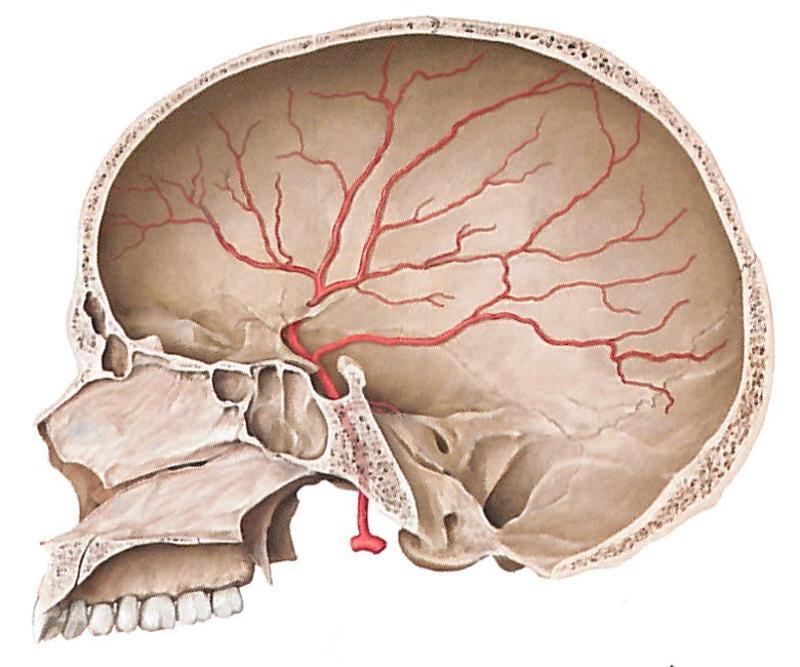 Middle meningeal (main artery of dura covering lateral & superior part of cerebral cortex) |
front 242 This pathology is characterized by slow, oozing accumulation of blood with vague, nonspecific symptoms such as headache, cognitive impairment, unsteady gait | back 242 Subdural hematoma |
front 243 Most common, and catastrophic, cause of this pathology is an aneurysm; can cause an extremely severe headache ("thunderclap") | back 243 Subarachnoid hemorrhage |
front 244 Characterized by a "thunderclap" headache | back 244 Subarachnoid hemorrhage |
front 245 Common location of an aneurysm | back 245 Where middle cerebral artery arises from internal carotid |
front 246 These substances can get past the blood-brain barrier | back 246 -Glucose -Amino acids -Some ions -Lipid soluble substances (i.e. ETOH) |
front 247 Form blood-brain barrier; provide structure & sustenance in CNS | back 247 Astrocytes |
front 248 Make glia wrapping (myelin sheath) in CNS | back 248 Oligodendrocytes |
front 249 Autoimmune disease where myelin wrappings in some regions of white matter are attacked; these regions are subsequently termed "plaques"; plaques heal, but there remains unhealed damage that adds up over time; eventually patient may not be able to walk | back 249 Multiple Sclerosis (MS) |
front 250 1. What difference would you see if you cut both an axon in the CNS & an axon in the PNS? 2. Why? | back 250 1. CNS - no regeneration PNS - regenerates (very slowly) 2. Glia in CNS hostile to axonal regrowth, but Schwann cells (glia of PNS) actively promote axonal regrowth |
front 251 Glia in this region are special; have been used to culture & grow more for injection into the spinal cord for regenerative purposes | back 251 Olfactory bulb |
front 252 The peripheral nervous system can be divided into these 2 parts | back 252 Somatic & autonomic nervous systems |
front 253 Nervous system that innervates skeletal muscles; r/t motor controls, such as voluntary movements & involuntary reflexes (i.e. patellar reflex, or knee jerk) | back 253 Somatic nervous system |
front 254 In addition to innervating skeletal muscle for motor purpose, the somatic nervous system also has __1__ nerve fibers that are responsible for communicating __2__ information to the CNS, such as touch, temperature, & pressure | back 254 1. Afferent 2. Sensory |
front 255 The autonomic nervous system is further divided into these 3 systems | back 255 -Sympathetic NS -Parasympathetic NS -Enteric NS |
front 256 This nervous system is self-governed; innervates viscera (i.e. smooth muscle, cardiac) to adjust their functions | back 256 Autonomic nervous system |
front 257 The __1__ coordinates ANS function with both the __2__ & __3__ systems, and circadian rhythmic activity (i.e. sleep-wake cycles) | back 257 1. Hypothalamus 2. Endocrine 3. Limbic (emotional) |
front 258 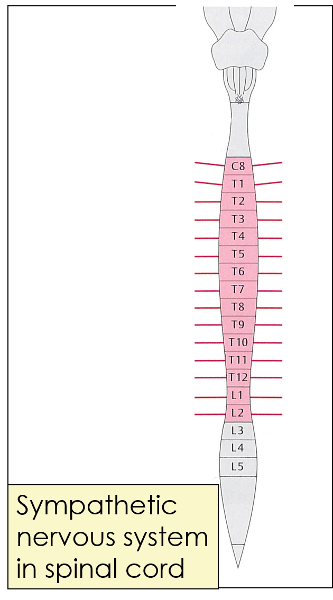 What does this picture represent? | back 258 Sympathetic nervous system in spinal cord (projecting lines represent nerves going out to sympathetic ganglia) |
front 259 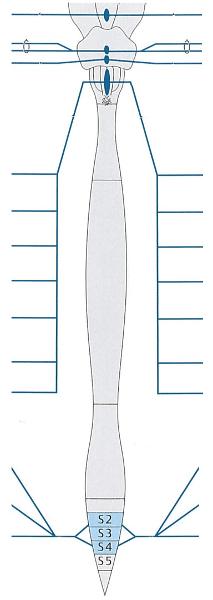 What does this picture represent? | back 259 Parasympathetic nervous system in brainstem & spinal cord |
front 260 Where do the cell bodies of neurons belonging to the ANS reside? | back 260 Outside brain & spinal cord (mostly) |
front 261 Organ involved in "sympathetic activation" | back 261 Adrenal gland (epinephrine) |
front 262 BP is monitored by __1__ located in an enlarged part of the _____ 2 _____; information is sent to the __3__ center in the __4__ | back 262 1. Baroreceptors 2. Carotid artery 3. Vasomotor 4. Medulla |
front 263 If BP is too high, the __1__ nerve transmits __2__ activity to the heart to slow rate & reduce force; if BP is too low, signals from __3__ center go to __4__ cells in the spinal cord, which are then relayed to neurons in the _____ 5 _____, which accelerate HR & increase force of contraction | back 263 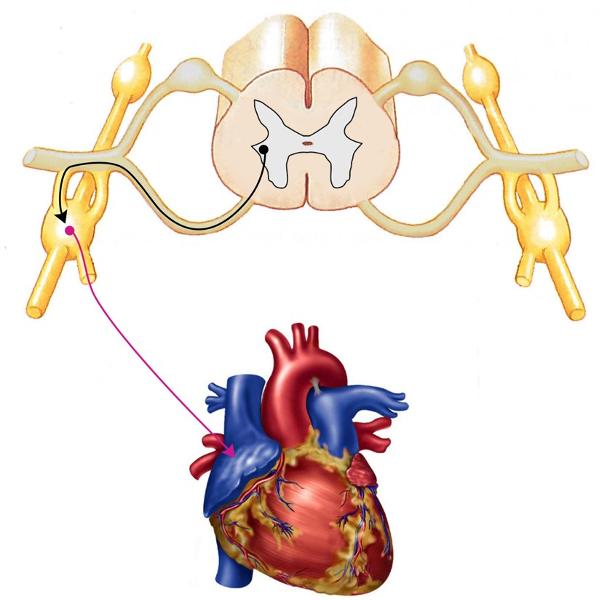 1. Vagus 2. Parasympathetic 3. Vasomotor 4. Sympathetic 5. Sympathetic chain (picture above) |
front 264 Orthostatic hypotension is caused by these 2 factors | back 264 -Venous pooling -Decreased venous return |
front 265 Viral disease of spinal ganglia; dermatomally distributed skin lesions | back 265 Herpes Zoster (herpes virus) |
front 266 Patients most at risk of developing a subdural hematoma | back 266 Young & elderly |