front 5 NUMBERS OF INVADING MICROBES
LD50 | back 5 Lethal dose (of a toxin) for 50% of the test population. |
| back 6 1) PORTAL OF ENTRY: Skin
ID50: 10–50 endospores
2) PORTAL OF ENTRY: Inhalation
ID50: 10,000–20,000 endospores
3) PORTAL OF ENTRY: Ingestion
ID50: 250,000–1,000,000 endospores |
| back 7 1) Portal of Entry: Botulinum
ID50: 0.03 ng/kg
2) Portal of Entry: Shiga toxin
ID50: 250 ng/kg
3) Portal of Entry: Staphylococcal enterotoxin
ID50: 1350 ng/kg |
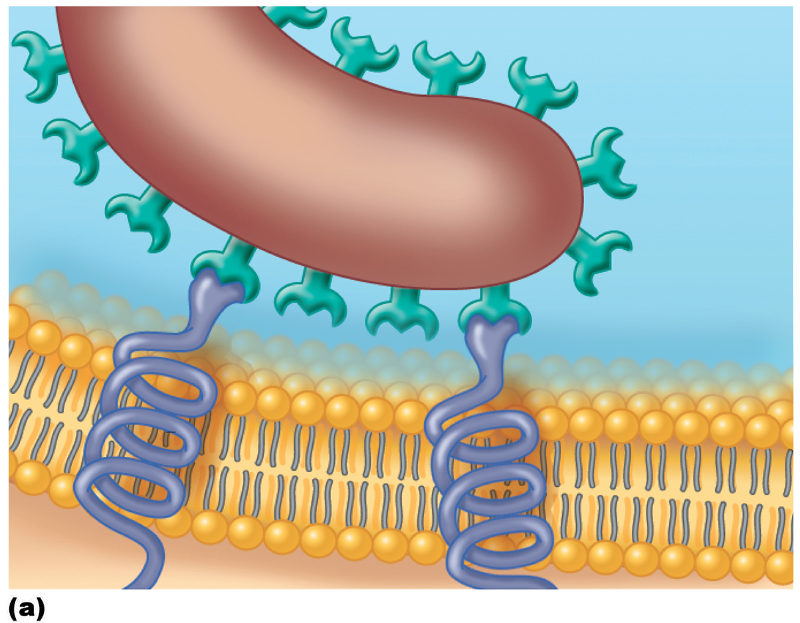
| back 8 1. ADHESINS/LIGANDS bind to receptors on host cells
a) Glycocalyx: Streptococcus mutans
b) Fimbriae: Escherichia coli
c) M protein: Streptococcus pyogenes
2. Form biofilms |
| back 9 Surface molecules on a pathogen, called adhesins or ligands, bind specifically to complementary surface receptors on cells of certain host tissues. |
| back 10 PREVENT PHAGOCYTOSIS:
1. Streptococcus pneumonia
2. Haemophilus influenza
3. Bacillus anthracis |
| back 11 1. M PROTEIN resists phagocytosis
a) Streptococcus pyogenes
2. OPA PROTEIN inhibits T helper cells
b) Neisseria gonorrhoeae
3. MYCOLIC ACID (waxy lipid) resists digestion
c) Mycobacterium tuberculosis |
| back 12 1. COAGULASE: coagulates fibrinogen
2. KINASES: digest fibrin clots
3. HYALURONIDASE: hydrolyzes hyaluronic acid
4. COLLAGENASE: hydrolyzes collagen
5. IgA PROTEASES: destroy IgA antibodies |
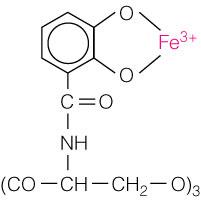
front 13 USING THE HOST'S NUTRIENTS
SIDEROPHORES | |
| back 14 1. Disrupt host cell function
2. Produce waste products
3. Toxins |
| back 15 1. TOXIN: substance that contributes to
pathogenicity
2. TOXIGENICITY: ability to produce a toxin
3. TOXEMIA: presence of toxin in the host’s blood
4. TOXOID: inactivated toxin used in a vaccine
5. ANTITOXIN: antibodies against a specific toxin |
front 16 MECHANISMS OF EXOTOXINS AND ENDOTOXINS
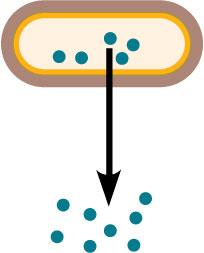
Figure 15.4 | back 16 EXOTOXINS:
Exotoxins are proteins produced inside pathogenic bacteria, most commonly gram-positive bacteria, as part of their growth and metabolism. The exotoxins are then secreted into the surrounding medium during log phase.
Exotoxin: toxic substances released outside the cell.
Clostridium botulinum, an example of a gram-positive bacterium that produces exotoxins. |
front 17 MECHANISMS OF EXOTOXINS AND ENDOTOXINS
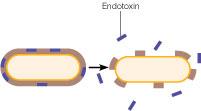
Figure 15.4 | back 17 ENDOTOXINS:
Endotoxins are the lipid portions of lipopolysaccharides (LPS) that are part of the outer membrane of the cell wall of gram-negative bacteria (lipid A; see Figure 4.13c). The endotoxins are liberated when the bacteria die and the cell wall breaks apart.
Endotoxins: toxins composed of lipids that are part of the cell membrane.
Salmonella typhimurium, an example of a gram-negative bacterium that produces endotoxins. |
| back 18 Specific for a structure or function in host cell. |
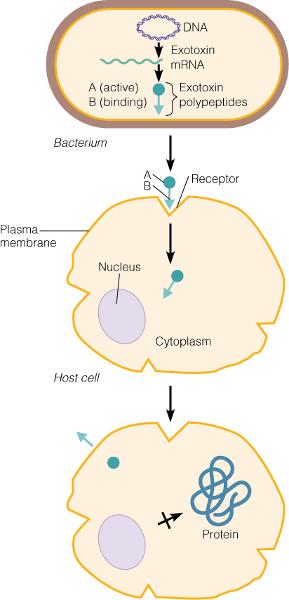
front 19 THE ACTION OF AN A-B EXOTOXIN
Figure 15.5 | back 19 STEPS:
1) Bacterium produces and releases exotoxin.
2) B (binding) component of exotoxin attaches to
host cell receptor.
3) A-B exotoxin enters host cell by receptor-
mediated endocytosis.
4) A-B exotoxin enclosed in pinched-off portion of
plasma membrane during pinocytosis.
5) A-B components of exotoxin separate. The A
component alters cell function by inhibiting
protein synthesis. The B component is released
from the host cell and the host cell receptor
is moved back into the plasma membrane to be
re-used. |
front 20 MEMBRANE-DISRUPTING TOXINS
Lyse host’s cells by | back 20 1. Making protein channels in the plasma membrane
a) Leukocidins
b) Hemolysins
c) Streptolysins
2. Disrupting phospholipid bilayer |
| back 21 1. Cause an intense immune response due to release
of cytokines from host cells
2. Symptoms: fever, nausea, vomiting, diarrhea,
shock, and death |
| back 22 Source:
Mostly gram-positive
Relation to microbe:
By-products of growing cell
Chemistry:
Protein
Fever?:
No
Neutralized by antitoxin?:
Yes
LD50:
Small |
front 23 EXOTOXINS AND LYSOGENIC CONVERSION | back 23 CORYNEBACTERIUM DIPHTHERIAE
Exotoxin: A-B toxin
Lysogeny: +
STREPTOCOCCUS PYOGENES
Exotoxin: Membrane disrupting erythrogenic toxin
Lysogeny: +
CLOSTRIDIUM BOTULINUM
Exotoxin: A-B toxin; neurotoxin
Lysogeny: +
C. TETANI
Exotoxin: A-B toxin; neurotoxin
Lysogeny:
VIBRIO CHOLERAE
Exotoxin: A-B toxin; enterotoxin
Lysogeny: +
STAPHYLOCOCCUS AUREUS
Exotoxin: Superantigen
Lysogeny: + |
| back 24 Source:
Gram-negative
Relation to microbe:
Outer membrane
Chemistry:
Lipid A
Fever?:
Yes
Neutralized by antitoxin?:
No
LD50:
Relatively large |
front 25 ENDOTOXINS AND THE PYROGENIC RESPONSE
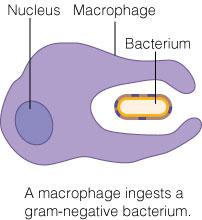
Figure 15.6 | back 25 STEPS:
1) A macrophage ingests a gram-negative bacterium.
2) The bacterium is degraded in a vacuole,
releasing endotoxins that induce the macrophage
to produce cytokines IL-1 and TNF-α.
3) The cytokines are released into the bloodstream
by the macrophages, through which they travel
to the hypothalamus of the brain.
4) The cytokines induce the hypothalamus to
produce prostaglandins, which reset the body’s
“thermostat” to a higher temperature, producing
fever. |
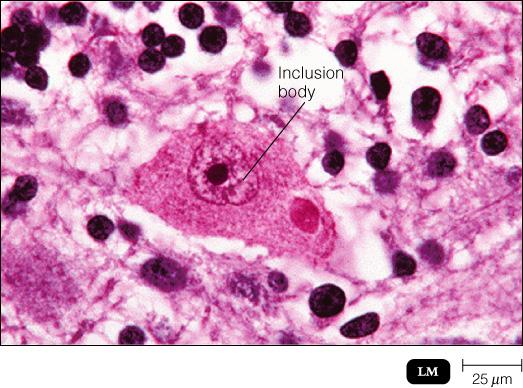
front 26 CYTOPATHIC EFFECTS OF VIRUSES | back 26 1. Cell lysis
2. Inclusion bodies
3. Stop macromolecular synthesis in host cell
4. Cause cell fusion (syncytium)
5. Interfere with cell functions
6. Cause antigenic changes on host cell surface
leading to cell being destroyed by the immune
system
7. Chromosomal changes (possibly activation of
oncogenes)
8. Transformation of host cells- loss of contact
inhibition leading to unregulated cell growth |
front 27 PATHOGENIC PROPERTIES OF FUNGI | back 27 1. Fungal waste products may cause symptoms
2. Chronic infections provoke an allergic response
3. Trichothecene toxins inhibit protein synthesis
a) Fusarium
4. Proteases
a) Candida, Trichophyton
5. Capsule prevents phagocytosis
a) Cryptococcus |
front 28 PATHOGENIC PROPERTIES OF FUNGI | back 28 1. Ergot toxin
a) Claviceps
2. Aflatoxin
a) Aspergillus
3. Mycotoxins
a) Neurotoxins: phalloidin, amanitin
- Amanita |
front 29 PATHOGENIC PROPERTIES OF PROTOZOA | back 29 1. Presence of protozoa
2. Protozoan waste products may cause symptoms
3. Avoid host defenses by
a) Growing in phagocytes
b) Antigenic variation |
front 30 PATHOGENIC PROPERTIES OF HELMINTHS | back 30 1. Use host tissue
2. Presence of parasite interferes with host
function
3. Parasite’s metabolic waste can cause symptoms |
front 31 PATHOGENIC PROPERTIES OF ALGAE | back 31 1. Paralytic shellfish poisoning
a) Dinoflagellates
b) SAXITOXIN |
| back 32 1. Respiratory tract
a) Coughing and sneezing
2. Gastrointestinal tract
a) Feces and saliva
3. Genitourinary tract
a)Urine and vaginal secretions
4. Skin
5. Blood
a) Arthropods that bite; needles or syringes |
front 33 MICROBIAL MECHANISMS OF PATHOGENICITY
Figure 15.9 | back 33 When the balance between host and microbe is tipped in favor of the microbe, an infection or disease results. Learning these mechanisms of microbial pathogenicity is fundamental to understanding how pathogens are able to overcome the host’s defenses.
PORTALS OF ENTRY:
Mucous membranes
• Respiratory tract
• Gastrointestinal tract
• Genitourinary tract
• Conjunctiva
Skin
Parenteral route
***THE NUMBER OF INVADING MICROBES + ADHERENCE****
PENETRATION AND EVASION OF HOST DEFENSES:
Capsules
Cell wall components
Enzymes
Antigenic variation
Invasins
Intracellular growth
DAMAGE TO HOST CELLS:
Siderophores
Direct damage
Toxins
• Exotoxins
• Endotoxins
Lysogenic conversion
Cytopathic effects
PORTALS OF EXIT:
Generally the same as
the portals of entry for a
given microbe:
• Mucous membranes
• Skin
• Parenteral route |
front 34 Which disease is correctly matched with the common portal of entry?
A) Chlamydia : skin
B) Influenza : mucous membranes of genitourinary
tract
C) Measles : parenteral route
D) Poliomyelitis : mucous membranes of
gastrointestinal tract
E) Hookworm : mucous membranes of genitourinary
tract | back 34 Poliomyelitis : mucous membranes of gastrointestinal tract |
front 35 If a patient has a deep tissue infection as the result of an animal bite on the arm, the portal of entry is described as the:
A) connective tissue.
B) gastrointestinal route.
C) respiratory route.
D) skin.
E) parenteral route. | |
front 36 The ID50 for cutaneous anthrax due to Bacillus anthracis is 10-50 endospores, while the ID50 for inhalation anthrax is 10,000 to 20,000 endospores. This means that:
A) inhalation anthrax is easier to acquire than
cutaneous anthrax.
B) both cutaneous and inhalation anthrax can
easily acquired.
C) neither cutaneous or inhalation anthrax can be
acquired easily.
D) cutaneous anthrax is easier to acquire than
inhalation anthrax.
E) not enough information is available to answer
this question. | back 36 cutaneous anthrax is easier to acquire than inhalation anthrax. |
front 37 Which would be the most unlikely location to find adhesin molecules on a newly discovered bacterium?
A) cell wall
B) glycocalyx
C) capsule
D) ribosomes
E) fimbriae | |
front 38 What cell structure does Neisseria gonorrhoeae use to attach and enter host epithelial cells?
A) M proteins
B) fimbriae
C) flagella
D) cell wall waxes
E) capsules | |
front 39 Which of the following would not affect the ability of Streptococcus mutans to attach to teeth?
A) The lack of glucose.
B) The lack of a glycocalyx.
C) The absence of Actinomyces/i>, a bacterium that
can be part of dental plaque.
D) The inability to form dextran.
E) The lack of the enzyme glucosyltransferase. | back 39 The absence of Actinomyces/i>, a bacterium that can be part of dental plaque. |
front 40 Which of the following is not true for bacterial capsules?
A) The importance of the capsule to virulence for
Streptococcus pneumoniae can be determined
because there are strains both with and without
the capsule.
B) Capsules related to virulence are produced by
the causative agents of anthrax and bubonic
plague.
C) Antibodies produced against a capsule cannot
affect whether disease will occur.
D) Pathogenic and non-pathogenic bacteria can
produce capsules.
E) For Streptococcus pneumoniae, the encapsulated
strain is more virulent. | back 40 Antibodies produced against a capsule cannot affect whether disease will occur. |
front 41 Capsules play a role in the virulence of all of the following except:
A) Mycobacterium tuberculosis
B) Yersinia pestis
C) Haemophilus influenzae
D) Bacillus anthracis
E) Klebsiella pneumoniae | back 41 Mycobacterium tuberculosis |
front 42 Which of the following is not an A-B exotoxin?
A) Tetanus toxin
B) Diphtheria toxin
C) Staphylococcus aureus enterotoxin
D) Streptolysin O
E) Cholera toxin | |
front 43 Which one of the following pairs is not correctly matched?
A) Leukocidin : lyses WBC membranes
B) IgA protease : digest antibodies
C) Siderophore : traps iron
D) Collagenase : breaks down connective tissue
E) Coagulase : lyses fibrin clots | back 43 Coagulase : lyses fibrin clots |
front 44 Which of the following eukaryotic molecules/structures can be responsible for movement of bacteria within host cells?
A) cilia
B) actin molecules
C) pseudopods
D) flagella
E) invasins | |
front 45 All of the following are true of A-B exotoxins except:
A) Many exotoxins are A-B toxins.
B) They consist of two polypeptide components.
C) The A portion of the toxin is the active
component.
D) They are only produced by gram-negative
bacteria.
E) The B portion of the toxin binds to surface
receptors on host cells. | back 45 They are only produced by gram-negative bacteria. |
front 46 Which of the following bacterial toxins binds to nerve cells, preventing chemical communication between nerve and muscle cells?
A) Erythrogenic toxin
B) Botulinum toxin
C) E. coli endotoxin
D) Staphylococcal enterotoxin
E) Diphtheria toxin | |
front 47 Which is true of endotoxins?
A) They are released upon cell lysis.
B) They are proteins.
C) They increase blood pressure.
D) They are disease-specific.
E) They are produced by gram-positive bacteria. | back 47 They are released upon cell lysis. |
front 48 Which is not true of exotoxins?
A) They rarely have enzymatic activity.
B) They can be converted to toxoids.
C) They can cause toxemia.
D) The genetic material that encodes most of them
is plasmid or prophage associated.
E) The exotoxin can work by binding and entering
the host cell. | back 48 They rarely have enzymatic activity. |
front 49 Which is not true of endotoxins?
A) They are more resistant to heat than
exotoxins.
B) They can be produced by Streptococcus.
C) They can lyse amoebocytes found in crab
hemolymph.
D) They can induce chills, fever, aches, clotting,
shock and miscarriage.
E) They are eliminated from the body as a result
of antitoxin production. | back 49 They are eliminated from the body as a result of antitoxin production. |
front 50 Which of the following is not a cytopathic effect of viruses?
A) Leukocidins lysing WBCs.
B) Cell fusion.
C) Inclusion bodies.
D) Cell death.
E) Loss of contact inhibition. | |
front 51 Which of the following events leads to all of the others in a pyrogenic (fever) response?
A) The body's thermostat is set to a higher level,
and fever occurs.
B) IL-1 is released by macrophages.
C) IL-1 travels via the blood to the
hypothalamus.
D) Endotoxin is released from the cell wall of
gram-negative bacteria.
E) The hypothalamus releases prostaglandins. | back 51 Endotoxin is released from the cell wall of gram-negative bacteria. |
front 52 The pathogenicity of which of the following is not the result of lysogeny?
A) Vibrio cholerae
B) Streptococcus pyogenes
C) Clostridium tetani
D) Clostridium botulinum
E) Corynebacterium diphtheriae | |
front 53 Saxitoxin is produced by:
A) dinoflagellates.
B) fungi.
C) bacteria.
D) helminths.
E) protozoa. | |
front 54 All of the following are correct regarding siderophores, like the one shown in the figure, EXCEPT:
A) They are produced by the host cells and
directly kill bacteria.
B) They can bind to hemoglobin.
C) They take iron away from the host.
D) They are proteins secreted by some pathogens. | back 54 They are produced by the host cells and directly kill bacteria. |
front 55 Which substance, released by the ingested gram-negative bacteria, can lead to a higher body temperature?
A) Endotoxin
B) Siderophore
C) Enterotoxin
D) A-B toxin | |
front 56 All of the following toxins are A-B toxins like the one in the figure EXCEPT:
A) Botulinum toxin
B) Diphtheria toxin
C) Streptolysin toxin
D) Tetanus toxin | |
front 57 In addition to the cytoplasmic inclusion body seen in the figure, what other cytopathic effects are possible outcomes due to viral infections?
A) Syncytium formation
B) Stopping mitosis irreversibly
C) Release of lysosomal contents in the cell
D) Chromosomal changes in the host cell
E) All of the above | |
front 58 All of the following are correct concerning endotoxin EXCEPT:
A) They are liberated if the bacterial cell wall
breaks apart.
B) They can lead to disseminated intravascular
clotting.
C) They are part of the outer portion of the cell
wall.
D) They are only present in gram positive cells. | back 58 They are only present in gram positive cells. |
front 59 Exotoxins have all the following characteristics EXCEPT:
A) A small dose can be lethal.
B) They are usually destroyed by heat.
C) They can be converted to toxoids.
D) They are present in the LPS of the outer cell
membrane. | back 59 They are present in the LPS of the outer cell membrane. |
front 60 Which of the following is not a cytopathic effect of viruses?
A) cell surface antigens change
B) host cells fuse to form multinucleated syncytia
C) none of the above.
D) inclusion bodies are found in the cytoplasm or
nucleus | |
front 61 Which of the following effects is most likely to occur if a pathogen enters the body by a portal of entry other than the preferred one?
A) A milder disease will result.
B) A different disease of the same severity will
result.
C) Pathogens cannot enter by alternate routes.
D) A more severe disease will result. | back 61 A milder disease will result. |
front 62 Which of the following virulence factors does not contribute to the spread of a disease in the body?
A) hyaluronidase
B) fibrinolysin
C) hemolysin
D) collagenase | |
front 63 The presence of endotoxins in a sterile fluid indicates:
A) the presence of gram-negative cell walls.
B) gram-positive bacteria are growing.
C) gram-negative bacteria are growing.
D) the fluid is not sterile. | back 63 The presence of gram-negative cell walls. |
front 64 Botulism can be prevented by taking which of the following precautions?
A) boiling food prior to consumption
B) avoiding canned food
C) administering antibiotics before eating
D) preventing fecal contamination of food | back 64 Boiling food prior to consumption. |
front 65 Which of the following organisms does not produce a neurotoxin?
A) Clostridium botulinum bacteria
B) Clostridium tetani bacterium
C) rabies virus
D) Alexandrium algae | |
front 66 Which of the following organisms does not produce an enterotoxin?
A) Staphylococcus aureus
B) Shigella spp.
C) Clostridium botulinum
D) Vibrio cholerae | |
front 67 Given the following LD50 values for Bacillus anthracis, through which portal of entry is it easiest to get anthrax?
A) Ingestion - 1,000,000 endospores
B) All are equal
C) Inhalation - 20,000 endospores
D) Cutaneous - 50 endospores | back 67 Cutaneous - 50 endospores |
front 68 Which of the following is not an enzyme associated with invasiveness?
A) leukocidin
B) kinase
C) toxemia
D) hyaluronidase | |
front 69 Which one of the following bacterial proteins can take iron from human lactoferrin?
A) siderophore
B) kinase
C) protease
D) hyaluronidase | |
front 70 Based on these LD50 values, which microbe is the most virulent? Assume each bacterium enters through the appropriate portal of entry.
A) E. coli O157 - 1000 cells
B) Vibrio cholerae - 108 cells
C) Cryptosporidium - 50 cells
D) Shigella - 10 cells | |
front 71 Which of the following is a cell wall component that contributes to invasiveness?
A) endotoxin
B) M protein
C) hemolysin
D) coagulase | |
front 72 Which of the following diseases cannot be prevented by toxoids?
A) diphtheria
B) botulism
C) tetanus
D) Gram-negative septic shock | back 72 Gram-negative septic shock |
front 73 Which one of the following should not be produced at the same time as coagulase?
A) fimbriae
B) capsules
C) hemolysin
D) fibrinolysin | |
front 74 The LD50 of Vibrio cholerae is 108 cells when taken orally. The LD50value is 104 if the bacteria are ingested with bicarbonate. This indicates that stomach acid:
A) is not an important factor in determining
virulence.
B) decreases the virulence of V. cholerae.
C) has no effect on virulence.
D) increases the virulence of V. cholerae. | back 74 Decreases the virulence of V. cholerae. |
front 75 Which of the following is not an example of the parenteral route?
A) hair follicle
B) cut
C) insect bite
D) injection | |
front 76 The symptoms of protozoan diseases are usually due to:
A) exotoxins.
B) endotoxins.
C) capsules.
D) metabolic waste products. | back 76 Metabolic waste products. |
front 77 Hepatitis B virus transmitted by a finger-stick device is transmitted by which portal of entry?
A) adherence
B) skin
C) mucous membrane
D) parenteral | |
front 78 Which of the following does not protect a bacterium from phagocytosis?
A) leukocidins
B) capsule
C) M protein
D) sterptolysin S (SLS) | |
front 79 Symptoms of helminthic diseases are usually due to:
A) the helminth eating its host.
B) toxins.
C) the parasite eating the host's food.
D) the presence of the parasite. | back 79 The presence of the parasite. |