1. The film record produced to visualize the internal structures of the body is called.
radiograph
2. Any process by which a neutral atom gains or loses an electron is called.
ionozation
3. In radiology, which discipline uses high-energy radiation to treat cancer?
radiation therapy
4. To image a blood vessel in the body the introduction of what is used?
Contrast medium
5. What is mammography?
Radiography of the breast
6. What is CT imaging?
Computed Tomography (CT ) - recording of a predetermined plane in the body using an x-ray beam that is measured, recorded, and them processed by a computer form display on a monitor
7. What is MRI imaging?
Magnetic Resonance Imaging (MRI) - Process of using a magnetic field and radio-frequencies to create sectional images of the body
8. What is the main difference between CT and MRI imaging?
CT's use a x-ray beam which causes ionization where the MRI uses a magnetic field and radiofrequencies which does not.
9. Who discovered X-Rays?
Wilhem C. Rongten
10. When were x-rays discovered?
November 8, 1895
11. What is the relationship between MRI and CT?
diagnostic imaging
12. Who is the AHRA?
American Healthcare Radiology Administrators - organized to promote management practice in the administration of imaging services. approx 4000 members/ journal Radiology Management/ offer Certified RAdiology Administrator (CRA) examination
13. What is the purpose of the ARRT registry?
American Registry of Radiologic Technologists - Encouraging the study and elevating the standards of radiologic technology, examining and certifying eligible candidates, and periodically publishing a listing of registrants
14. What is the purpose of the ACR?
American College of Radiology - to advance the science of radiology, improve service to the patient, study the socioeconomic aspects of the proactive of radiology, and encourage continuing education for radiologists and persons practicing in allied professional fields.
15. What modalities does the ARRT certify?
- radiography
- nuclear medicine
- radiation thereapy
- cardiovascular interventional technology
- mammography
- CT/MRI
- dosimetry
- QM
16. What does the title of RT (R) represent?
Registered Technologist - Radiographer
17. For Registered Technologist, the required CE credits per two year period is how many?
24 hours
18. What behaviors does the psychomotor domain include?
process of doing an action
19. What behaviors does the cognitive domain include?
process of thinking (analysis) of an action
20. What behaviors does the affective domain include?
analyzing personal values and feelings and managing ethicl situations
21. What is the beam of radiation that exits the tube called?
primary radiation
22. What is the beam of radiation that exits the patient called?
remnant radiation
23. What is the non-diagnostic radiation either exiting the patient or prior to the patient is called?
scatter radiation
24. The process of altering the beam of radiation as it passes through the patient is termed what?
attenuation
25. What is Radiopaque?
NOT easily penetrable by x-rays or other forms of radiant energy
26. What is Radiolucent?
Permitting the passage of x-rays or other forms of radiant energy with tittle attenuation
27. What is SID?
Source-to-Image Distance - distance between the source of x-rays (usually the focal spot of the x-ray tube) and the image receptor
- greater the SID, the better the recorded detail will be.
28. What is OID?
Object-to-Image Distance
- When the object is moved closer to the image receptor, penumbras decreases and the image sharpness increases.
- The smaller the OID is, the better the recorded detail will be.
29. What is a Collimator used for?
Controls the size and shape of the x-ray field coming out of the x-ray tube.
- 2 adjusting knobs adjust length and width of the rectangular x-ray field
30. Positive Beam Limitation refers to what?
(PBL) form of x-ray collimation of field size that ensures the x-ray exposure field is no larger than the receptor size
31. What are exposure factors?
Influence and determine the quantity and quality of radiation a patient is exposed to
32. Why do we utilize a grid?
A grid is a device that is designed to remove as many scattered photons exiting the patient as possible before they reach the IR.
33. The device that a cassette is placed in prior to exposure of the patient is termed what?
bucky tray
34. List everything you know about mAs.
- mAs IS A PRIMARY FACTOR OF DENSITY
- mAs represents the quantity of x-ray production
- Direct relationship
- Calculated by simple multiplication of milliamperage (mA) and exposure time (S)
- Regardless of the mA and time combinations, the same mAs value will yield the same exposure (mAs Reciprocity Law).
35. What can be done by the technologist to control Compton scattering?
use rule of ALARA
36. List everything you know about KVP.
- Controls x-ray beam penetration
- Direct relationship
- X-ray beam is polyenergetic or heterogeneous
- 15% Rule
37. What is density?
The degree of darkening or blackness of exposed and processed photographic or radiographic film
38. What is contrast?
Difference between adjacent densities on a radiographic image
39. Does the degree of attenuation depend on the tissue characteristics? Explain.
Yes, depending on the type of body tissue irradiated. EX. bone tissue, being more densely packed and made of harder material, attenuates the beam to a greater degree than sof tissue of the same thickness.
40. The misrepresentation of true image size and shape on an image is termed what?
Distortion
41. What is the control panel?
Control console is the interface between the radiographer and the sophisticated electronics of the x-ray machine
42. The control panel consists of what?
- Most are microprocessor- controlled and use a simple computer interface
- Generator consoles permit selection of kVp, mA, exposure time (S), and mAs
- May be operated in the mAs mode or timer mode
- Technique selection is critical to good radiography
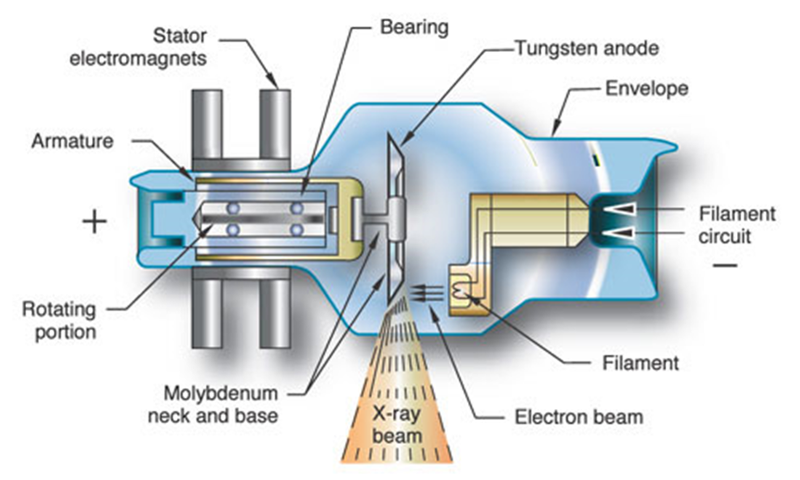
43. Draw a basic X-Ray tube and label the parts.
44. The automatic collimator of an x-ray machine is used to do what and is termed what?
Performs positive beam limitation (PBL) and allows the x-ray unit to detect the size of the image receptor the radiographer is using and automatically collimates to a size not larger than the image receptor.
45. What does the rotor switch do?
Part of the rotor-exposure switch which activates the rotor, or prep, and causes the anode to rotor and prepares the x-ray tube for the exposure factors that have been selected. After the tube has been properly prepared, the second switch is activated to begin the exposure.
46. When x-ray equipment is taken to a patient room that equipment is termed what?
mobile
47. Who is JRCERT and what is the purpose of JRCERT?
Joint Review Committee on Education in Radiologic Technology (JRCERT)
- Concerned with compliance with education standards developed by and for the profession of radiologic technology
- Governed by a Board of Directors known as the Joint Review Committee
- JRCERT accreditation requires demonstrated compliance with minimum requirements known as
- Essentials and Guidelines or Standards
- Established in 1969
- Board members nominated by four professional organizations concerned with radiology education
- Currently accredits
approx. 750 programs in:
- Radiography
- Radiation Therapy Technology
- Medical Dosimetry
- Magnetic Resonance Imaging
48. Who is JCAHO and what is the purpose of JCAHO?
JCAHO is an abbreviation for Joint Commission on Accreditation of Healthcare Organizations. It is an organization made up of individuals from the private medical sector to develop and maintain standards of quality in medical facilities in the United States. The JCAHO has no official connection to United States government regulatory agencies, and has no legal enforcement power; however, since many medical facilities rely on JCAHO accreditation procedures to indicate to the public that their particular institution meets quality standards, JCAHO and its policies has taken on a real importance in the medical field, despite the lack of official government sanction.
49. Who is ASRT and what is the purpose of the ASRT?
American Society of Radiologic Technologists (ASRT)
- represent indiviudual ppractitioners, educators, managers, and theadministrators, and students in radiography, radiation therapy, and muclear medicine, as well as the many specialties.
- >140,000 memebers
- Goals are to advance the professions of radiologic technology and imaging specialties, to maintain high standars of education, to enhance the quality of patient care, and to further the welfare and socioeconomics of RTS.
50. What is the CARE bill?
The CARE bill is a bill that seeks to protect patients from over exposure to radiation and pursues basic education and certification standards for healthcare workers who administer radiologic procedures. CARE stands for Consistency, Accuracy, Responsibility, and Excellence in Medical Imagining and Radiation Therapy.
51. What are some specifications of the CARE Bill?
The bill was first introduced to the U.S. Senate in 2012 and pressed on the fact that it would save the government large amounts of money as well as improve overall patient care. It would be applicable to every state in the union and limit, if not eliminate, inconsistencies with formal education. The CARE bill is not a licensure bill, so states are not required to license anyone as a result. Once the bill is passed, it will take three years to implement it nationwide.
52. How is Radiation to the RT measured?
Dosimeter
- Optically stimulated luminescence dosimeter(OSL)
- film badge
- thermoluninescent dosimeter (TLD)
- Pocket dosimeter
53. What is gonadal shielding?
process of placing protection (lead shield) over the reproduction organs during when beam is 4 to 5 cm away. Especially important in children and adults of reproductive age.
54. Why would someone use gonadal shielding?
minimizes reproductive organ exposure to radiation
55. What is the term used to define the science of rightness and wrongness of human conduct and character?
Ethics
56. What are the three types of medical law?
- Constitutional Law (system of checks and balances)
- Legislative/Administrative Law – system of statutes and regulations (local level, state,etc)
- Case Law – derived from the Common Law of England (case-by-case basis) decisions can be made as to what happened before in such situations.
57. Which type of law defines individual rights?
Constitutional Law
58. What would cause you to use a grid with the IR instead of just the IR only for imaging?
minimize scatter radiation and create a sharper image without the "fog" and creating greater contrast
59. What is an image receptor used for?
Medium used to capture the image for the recording, such as x-ray film or a digital imaging plate
60. How does the film become exposed during an x-ray exam using an IR?
- X-ray beam energy is produced using high-voltage electricity.
- X-rays pass through matter and strike an image receptor.
- Image receptor converts the energy of x-rays into an image.
61. The “boiling off of Electrons” by the Cathode is termed what?
thermionic emission
62. How are x-rays produced?
X-ray beam energy is produced using high-voltage electricity.
63. What is ALARA?
as low as reasonably achievable (ALARA)
64. Who follows ALARA?
Radiologic Technologist and those preforming x-rays
65. How is mAs calculated?
Calculated by simple multiplication of milliamperage (mA) and exposure time (S)
- mA x time = mAs
Regardless of the mA and time combinations, the same mAs value will yield the same exposure (mAs Reciprocity Law).
66. How can a technologist be accused of fraud?
generally defined as a willful and intentional misrepresentation of facts that may cause harm to an individual or result in loss of an individual right or property.
- error by destroying or altering images or records
- altering personnel records, changing patients medical records, incorrect billing, misleading or covering up some form of wrongdoing
67. What are the results of a technologist telling someone about a patient’s exam?
- HIPPA violoation
- possible lawsuit, suspension, loss of job
- Rules of ethic violation and possible barring from ARRT
68. What is the electromagnetic spectrum?
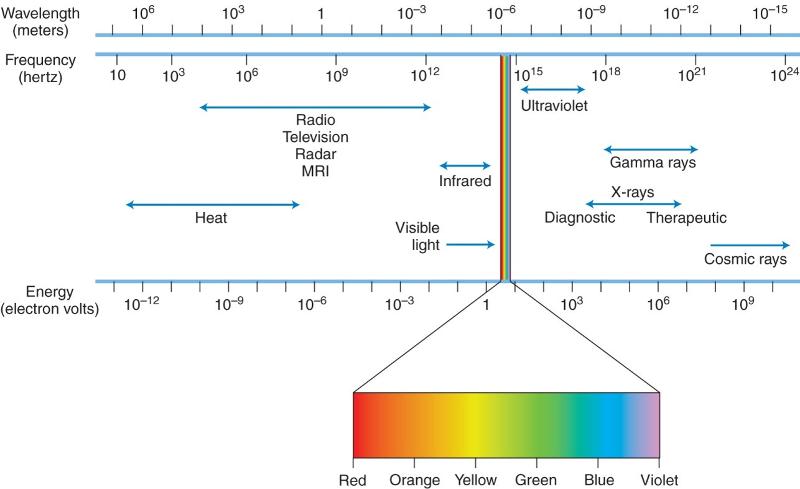
the full range of frequencies of electromagnetic radiation including TV/Radio, infrared, visible light, gamma rays, x-rays, and cosmic rays.
69. What are the different ethical theories and their main principles?
- Consequentialism - evaluates the rightness or wrongness of ethical decision by assessing the consequences of these decisions on the patient, thus producing a good effect or at least avoiding some potential harm (may lie to patient if they believe the lie might benefit the patient)
- Non-consequentialism - belief that actions themselves rather than consequences, determine the worth of actions
70. What is the advantage of using the fluoroscopic unit over the standard radiographic exposure equipment?
studies internal activities,processes, and presents images in "real time". - GI movement and structure, blood vessels, genitorurianry function, and joints
71. Where is the x-ray tube located in the fluoroscopic unit?
the x-ray tube is located above the patient
72. In analog imaging, the film is processed in what way?
developed to see the latent image.
73. What three things must be present for x-rays to be produced?
- Source of electrons
- Method to accelerate electrons to great speed
- Method to stop electrons
74. Why is there a vacuum in the glass x-ray tube?
for optimal production of an x-ray. Vacuum contained in enclosed special heat resistant glass.
75. Why are there two filaments, large and small, in the cathode?
Positive and negative terminals?...
76. What is the actual focal spot?
Focal spot is the area of the anode surface which receives the beam of electrons from the cathode.
77. What is the effective focal spot?
Focal spot is the area of the anode surface which receives the beam of electrons from the cathode.
78. What are some career options in the radiology profession?
- Radiography
- CT Scanning
- Medical Sonography
- Radiation Therapy
- MRI Scanning
- Mammography
- DEXA Scanning
- Radiologist Assistant
- Nuclear Medicine Cardiovascular Interventional Technology
- PACS Administrator
- Radiology Administration
- Education
- Research
- Commercial Firms
79. List an overview of the history of medicine.
o Early Years
>5000 years Egypt and Mesopotamia were using
medicine in combination with religious beliefs – deliberate removal of
bone and skulls
Hippocrates (460-370 BC)
• Greek physician
considered the father of Western Medicine
• Emphasized the
importance of carefully observing the patient and prevention thru diet
and exercise
• Responsible for the Hippocratic Oath which is the
standard for ethical treatment between a physician and a
patient
Romans recognized the importance of proper sanitation –
aqueducts, baths, sewers, etc.
o 17th Century
Edward
Jenner (1749-1832) introduced a vaccine to prevent smallpox in 1796
and was the foundation for the field of immunology
o 19th
Century
Louis Pasteur (1822-1895) developed pasteurization thru
his work with bacteria and proving the germ theory of infection
Robert Koch (1843-1910) receive the Nobel Prize in 1905 for his
discovery of a test for tuberculosis
Florence Nightingale
(1820-1910) developed the foundations for modern nursing
1895
Wilhelm Rontgen discovered x-rays medicine
o 20th Century saw
development of the scientific method throughout medicine
Sir
Alexander Fleming (1881-1955) discovered penicillin in 1928 which lead
to a better understanding of the immune system.
Increased use
of chemotherapy and a better understanding of the immune system
Human Genome Project started in 1953 which goals were to identify,
determine, store, improve, transfer, and address issues pertaining to
and around DNA
• Describe the discovery of the x-rays.
o
Wilhelm C. Röngten (Roentgen) (1845-1923)
began the field of
Radiology on November 8th, 1895.
Stumbled upon the X-Ray
working on cathode rays outside of their tubes
Barium
platinocyanide painted screen emitted light (fluorescing)
•
Became the first ever radiographic image
• Named “X-Ray” because
“X” was the symbol for UNKNOWN
• William Crookes (1832-1919)
produced x-rays around 1870 however did not grasp the significance of
the image
December 28th, 1895 Roentgen submitted his first
report, titled On a new Kind of Rays, to the Wurzburg Physico-Medical
Society
1901 Roentgen won the first Nobel Prize in Physics
80. What are some responsibilities of a radiographer?
- specialize in the use of x-rays to crate images
- diagnostic procedures - skeletal system, chest, and abdomen
- Administer contrast media to permit visualization of the GI tract
81. What are some key phrases a radiographer should use when conversing with a patient?
keep it simple and do not diagnosis
82. What is accreditation?
Accreditation – voluntary peer process through which an agency grants recognition to an institution for a program of study that meets specified criteria.
83. What is certification?
Certification - Voluntary process through which an agency grant recognition to an individual on demonstration, usually by examination, of specialized professional skills
84. Who is the examining body for the radiography profession?
Joint Review Committee (JRC)
85. What are some symptoms of stress?
repeated colds, ulcers, muscle stiffness, elevated cholesterol, excess sleeping, irritability, and headaches
86. What is the fight-or-flight response?
The physiologic reaction to a real or imagined threat arising from emotion of both fear and anger - internal - release of hormones to increase metabolism, increases in fats and sugars for energy, and increase sin heart rate and respiration.
87. What are some behaviors or thoughts that might increase the fight-or-flight response?
- "I'm stressed out!"
- home, school, daily life
88. What are some study techniques that enhance retention?
- Review the material soon after it is introduced
- use as many senses as possible
- plan a regular schedule of study
- study in a group
- attitude helps remembering
89. List the steps of successful test taking?
- Take the day off from study before a comprehensive test to relax and prepare both mentally and physically
- wear bright-colored clothes
- Avoid a diet full of carbohydrates
- get good nights sleep
- get to the test early
- scan the test
- review your test when completed
- put it behind you
90. What is critical thinking?
Creative action based on professional knowledge and experience involving sound judgement applied with high ethical standards and integrity
91. Why is critical thinking and problem solving important in radiologic sciences?
Not every case, patient, situation is the same.
92. What are the steps of problem solving?
- Identify the problem
- investigate the problem
- formulate viable solutions to the problem
- select the best solution
93. What is the purpose of clinical education?
The purpose of a clinical education is to provide an environment in which the student can transfer learning from the didactic and laboratory settings to real-world, patient-care experiences
94. Why is it important to adhere to major clinical education policies?
improved integration of the didactic, clinical and affctive aspects of the programs
Summarize the clinical education process.
didactic to introductions to "real world" experiences with mentorships and guidance given be RTs and clinical supervisors
96. Describe the structure of the administration of a hospital.
- Governance of a hospital begins with the board of directors or governing board.
- The President or Chief Executive Officer (CEO) is accountable to the hospital board.
- The hospital divisions and departments are accountable to the CEO.
97. Describe the structure of the radiology department.
- Varies depending on size and scope
- Often consists of sub-departments
- Requires support services
- Led by Administrative Director
98. How does the radiology department fit into the hospital?
Allied health - assist with diagnostic and treatment of the patients - same principles and focus as the hosptial
99. What is the role of the radiology administrator?
- managing resources and assets
- coaching and staff development
- analyzing opportunities
- strategic planning
100. Describe regulating agencies that affect radiology.
- The Joint Commission (TJC)
- Nuclear Regulatory Commission (NRC)
- Occupational Safety and Health Administration (OSHA)
- Food and Drug Administration (FDA)
- American College of Radiology (ACR)
- State Health Departments
- Internal agencies
- infection control
- radiation safety committee
- etc.
101. Describe the 3 major categories of image receptor systems used today in radiography.
- Film-screen (conventional) system - special film, manufactured to be particularly sensitive to x-radiation and certain colors of light radiation, is used to capture the energy message carried by the remnant beam and to convert it into an image. - Must be processed
- Digital Cassette Systemss - photostimulable phosphor systems, also know as computed radiography (CR) or cassette-based DR, PPS make use of the digital acquisition modality in chich PSP plates are used to produce radiographic images (imaging plates)
- Digital Cassette-less systems - the detectors are permanently enclosed in a rigid protective housing. Both direct capture DR and indirect capture DR detectors are used with these systems - x-ray photons are absorbed by the coating material and immediately converted into an electrical signal.
102. What is a latent image?
invisible image created after exposure but before processing
103. What is a manifest image?
the change on an x-ray film that becomes visible when the latent image undergoes appropriate chemical processing.
104. Identify the typical features of a radiographic system.
- x-ray tube
- collimator
- radiographic table
- control console
105. What is an R/F room used for?
radiography/fluoroscopy room (R/F)
106. Identify the units used to measure radiation exposure.
o Units of Measurement
The SI units (Système International
d’Unités, or International System of Units) were officially adopted in
1985.
Roentgen (Coulombs per Kilogram)
• Measures exposure
in air and is not used to express absorbed dose to individuals
•
A measure of ionization in air as a result of exposure to x-rays or
gamma rays
• Being phased out as a unit of exposure since
exposure may be expressed directly as coulombs per kilogram
Radiation absorbed dose (Gray)
• Expressed as rad
• Measures
the amount of energy absorbed in any medium, defined as 100 ergs of
energy absorbed in 1 g of absorbing material
• The rad has been
replaced by the gray (Gy) in the SI system.
o 1 Gy = 100
rad
• When we document patient dose in the medical chart we use
this unit – centigray (cGy)
Radiation equivalent man
(Sievert)
• Measured as rem
• Unit of dose
equivalence
• Accounts for different types of radiation and their
biologic effects
• rem has been replaced by the sievert
(Sv).
o 1 Sv = 100 rem
• Expressed as the product of the
absorbed dose in rad and a radiation quality factor
o rem = rad ×
QF
Curie (Becquerel)
• Measures the activity of a
radioactive material (radionuclide)
• Used in nuclear medicine
and radiation therapy
• The curie (Ci) is the unit of activity
equal to 3.7 × 1010 disintegrations per second (dps).
• SI unit
of activity is the becquerel (Bq).
o Defined as one
disintegration per second (1 dps)
o 1 Ci = 3.7 × 1010 Bq
107. Explain the ways in which ionizing radiation interacts with the body.
X-Ray Interactions with Matter
- Diagnostic Range of energies
- Classic coherent scattering
- Photoelectric interactions - diagnostic/complete absorption/electron leave atom creating a pair
- Compton scattering - diagnositc/ majority of occupational worker exposures/ incoming phoon collids with outer-shell creating a recoil
- Therapeutic Range of energies
- Pair production
- Photodisintegration
108. What are some methods to protect the patient from excessive radiation exposure?
- Time - minimize length of time patient remains in the path
- Distance - maximize the distance between the radiation source and the patient
- Shielding - shield reproductive areas as well as those not withing the interest area
109. What are some methods used to protect the occupational worker from excessive radiation exposure?
- Time - minimize length of time patient remains in the path to avoid scatter
- Distance - principle of the inverse square law
- Shielding - shielding garments
110. Explain the ethics of the radiologic sciences profession
"acts in the best interest of the patient"
111. Explain the four step problem-solving process of ethical analysis.
- identifying the problem - thoroughly look at the problem from every angle
- developing alternative solutions - exhaust all possible pathways to a resolution of the dilemma
- Selecting the best solution - based on moral and ethical resolve
- Defending the selection - you can explain the basis for your ethical decision in terms that you can justify to both colleagues and patients.
112. Identify moral dilemmas encountered in patient relationships.
faith, beliefs, and differences of behavior....
113. List key components of a patient’s medical record.
- patient identification data
- medical history
- examination findings
- diagnostic and therapeutic orders
- observations
- Reports and test
- consent forms
- Conclusions and follow up care
How does a patient’s medical record affect health care facilities and medical reimbursement?
Couple of different ways, treatment and billing
115 What does HIPAA stand for?
Health Insurance Portability and Accountability Act (HIPAA)
116 What is the purpose of HIPAA?
to improve the efficiency and effectiveness of the health care system by mandating confidentiality of health information - privacy, security, and the establishment of standards and requirements for the electronic transmission of certain health information
117. What is negligence?
- Failure to use such care as a reasonably prudent person would use under like or similar circumstances
118. What four things must be present for proof of medical negligence?
- For damages to be awarded, 4 elements must be proven
- Duty to the patient by the worker
- Breach of duty by an act or failure to do act
- Compensable injury
- Causal relation between injury and act
119. What is medical fraud?
A willful and intentional misrepresentation of facts that may cause harm to an individual or result in loss of an individual right of property
120. What is informed consent?
Person's agreement ot allow something to happen (such as surgery) that is based on a full disclosure of the facts needed to make the decision intelligently - risks, alternatives, benefits, etc