duration of pregnancy
Prenatal period: a time of physical and psychologic preparation for birth and parenthood
Duration of pregnancy: gestation
- spans 9 calender months, 10 lunar months.
- 40 weeks or 280 days
- trimesters
- first: weeks 1-13
- second: weeks 14-26
- third: weeks 27-40
Healthy People 2020 maternal goals
- Reduce the rate of fetal and infant deaths
- Reduce the rate of maternal mortality
- Reduce preterm births
- Reduce cesarean births among low risk women
Top three risk factors ob
- Hemorrhage—do pre-assessment, have blood ready
- HTN—does not get better until placenta is delivered ie. placenta causes the HTN—try to wait until 37 to 39 weeks to deliver
- Infection
Paternal adaptation to pregnancy
three phases
- Accepting the pregnancy
- uCouvade syndrome: has same symptoms as mom, nausea vomiting...so forth, weight gain
- uDevelopmental tasks experienced by the expectant
father
- uAnnouncement phase- accept to the fact of it
- uMoratorium phase- adjust tothe realityu
- uFocusing phase- becoming a good papa, active involvement in prego and being a dad
- uIdentifying with the father role
- uReordering personal relationships
- uEstablishing relationship with the fetus
- uPreparing for birth
Maternal Adaptation to pregnancy
three phases
uMaternal adaptation
- uAccepting the pregnancy
- uIdentifying with the mother role
- uReordering personal relationships
- uEstablishing relationship with fetus: attachment process of the
mother
- uPhase 1: She accepts the biologic fact of pregnancy
- uPhase 2: She accepts the growing fetus as distinct from herself
- uPhase 3: She prepares realistically for the birth and parenting of the child
- uPreparing for childbirth
- Ambivalence is normal, especially in first trimester
- May look into termination or adoption
3 parts to first prenatal visit
- Important components of the initial prenatal visit include detailed and carefully documented findings from the interview, a comprehensive physical examination, and selected laboratory tests.
Follow up visits
- Follow-up visits are shorter than the initial visit and are important for monitoring the health of the mother and fetus and providing anticipatory guidance as needed.
nnormal prenatal care timeline
Normal prenatal care = q month until 28 weeks, then q 2 months until 36 weeks, then every week until delivery.
iMMUNIZATIONS
Immunizations: MMR, TdAP (3rd trimester), flu, pneumovax, varicella
1.With regard to follow-up visits and the physical examination for women receiving prenatal care, nurses should be aware that:
a.The interview portions become more intensive as the visits become more frequent over the course of the pregnancy.
b.Monthly visits are scheduled for the first trimester, every 2 weeks for the second trimester, and weekly for the third trimester.
c.During the abdominal examination, the nurse should be alert for supine hypotension.
d.For pregnant women, a systolic blood pressure (BP) of 130 mm Hg and a diastolic BP of 80 mm Hg is sufficient to be considered hypertensive
C
What is supervena cavas syndrome
HOTN and less O2 to baby
How to care for a variety of women in pregnancy
- uCultural influences
- uMany cultural variations are found in prenatal care
- uCultural barriers to prenatal care: lack of money, lack of transportation, language barriers, modesty
- uEmotional response
- uPhysical activity and rest
- uClothing
- uSexual activity
- uDiet
- uAge differences
- uAdolescents
- uLess likely than older women to receive adequate prenatal care
- uWomen older than 35 years
- uMultifetal pregnancy
- uPuts the mother and fetuses at increased risk for adverse outcomes
- uMultifetal pregnancies are more likely to end in prematurity.
- uSpontaneous rupture of membranes before term is more common.
sex and pregooss
- Sex is okay. Lots of bleeding with sex and signs of preterm labor, must adjust.
- Sperm contains PG which can stimulate contractions, so may be advised it post-term
cAN I TRAVEL BY AIRPLANE
Travel beyond 34 – 35 weeks not condoned by airlines 2/2 risk of contractions from cabin pressure changes
What else to teach mom at visits
- uExpected maternal and fetal changes
- uNutrition
- uPersonal hygiene
- uPrevention of urinary tract infections
- uKegel exercises
- uPreparation for breastfeeding
- uDental health
- uPhysical activity
- Posture and body mechanics
- Rest and relaxation
- Employment
- Clothing
- Travel
- Medications and herbal preparations
- Immunizations
- uAlcohol, cigarette smoking, caffeine, drugs
- uNormal discomforts
- uRecognizing potential complications
- uRecognizing preterm labor—PROM, non BH contractions, etc, please come in.
- uSexual counseling
- uUsing the history
- uCountering misinformation
When would mom get ultrasound to estimate date of delivery
best at 1-13 weeks
1. Prenatal period definition:
2. Gestation definition:
3. Length of pregnancy/how many weeks in 1st 2nd and 3rd term?:
1. A time of physical and psychologic preparation for birth and parenthood
2. Duration of pregnancy:
3.
Spans 9 calendar months, 10 lunar months
40 weeks or 280 days
Trimesters
First: weeks 1-13
Second: weeks 14-26
Third: weeks 27-40
Signs and Symptoms of Pregnancy:
1. Presumptive
2. Probable
3. Positive
1. Suggested by the patient
- GI: Amenhorrea, nausea, vomiting, morning sickness
- Breast tenderness, need to pee, fatigue
- Quickening- feel the baby move at 16-20 weeks.
2. Probable: by examiner
- Pregnancy Test
- Uterine enlargement
- Braxton Hicks contractions
- Placental souffle
- Ballottement
3. Positive: Attributed to the FETUS
- Ultrasound
- Movement felt by someone else- third trimester
- Fetal heart beat distinct from mom
- Visualization of fetus
Estimated Date of Birth/Delivery: how to calculate? And who came up w/ this calculation?
Also, what is the gold standard for finding date of birth?
1. Take last menstural period
2. Substract 3 calender months
3. Add 7 days
4 This rule was founded by: Naegeles
5. Gold standard is ultrasound
Prenatal period:
1. Initial interview items
1.
Initial visit
- Prenatal interview:
- Reason for seeking care
- Current pregnancy
- Childbearing and female reproductive history
- Health history
- Nutritional history
- History of drug and herbal preparation use
- Family history
- Social, experiential, occupational history
- Prenatal interview (Cont.):
- History or risk of intimate partner violence
- Review of systems:
- Physical examination:
- Laboratory tests
- Urine, cervical, and blood samples
- Screening and diagnostic tests for infectious diseases and metabolic conditions
2. Physical assessment:
- Physical examination—teeth, thyroid, breast, breastfeeding, baby, abdomen size, vulva, vagina, cervix, pap, prenatal labs
- 3. Laboratory tests
- Urine, cervical, and blood samples
- Screening and diagnostic tests for infectious diseases and metabolic conditions
- Blood type, starting crit, hep, HIV, syph, asymptomatic bacteruria can cause preterm labor and ascend into kidney infxn, gonorrhea, chlamydia
Prenatal:
2. Follow up visits
Follow-up visits
- Interview
- Physical examination
- Fetal assessment
- Gestational age
- Fetal heart tones
- Health status
- Fundal height
- Laboratory/other tests
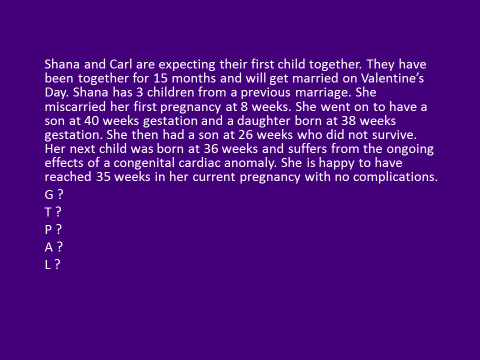
Terms:
1. Gravida
Gravida: women who is pregnant
2. Gravity
Gravity: the pregnancy
3. Mulitgravida
Multigravida- women with more than 2 pregnancies
Multipara
Multipara: women who has completed 2 or more pregnancies
Nulligravida
women who has never been pregnant
Parity
Parity : number of pregnancies in which fetus or fetuses have reached VIABILITY (20 wks), NOT the number of fetuses born
Nullipara
Nullipara : woman who has not completed pregnancy with a fetus or fetuses who have reached the stage of fetal viability
Primipara
Primipara : A woman who has completed one pregnancy with a fetus or fetuses who have reached 20 weeks of gestation
Multipara:
Multipara : A woman who has completed two or more pregnancies to 20 weeks of gestation or more
Preterm:
Preterm : a pregnancy that has reached 20 weeks of gestation but ends before completion of 37 weeks of gestation
Late preterm:
Late preterm : a pregnancy that has reached between 34 weeks 0 days and 36 weeks 6 days of gestation
Early Term:
Early term : a pregnancy that has reached between 37 weeks 0 days and 38 weeks 6 days of gestation
Full Term:
Full term : a pregnancy that has reached between 39 weeks 0 days and 40 weeks 6 days of gestation
Late term :
Late term : a pregnancy that has reached between 41 weeks 0 days and 41 weeks 6 days of gestation
Post term:
Post term : a pregnancy that has reached between 42 weeks 0 days and beyond of gestation
2 digit system used to identify the number of pregnancies
2 digit system: G__ P__
G – Gravida
P - Parity
5 digit system
5 digit system: G__ T__ P__ A__ L__
G – Gravida
T – Term birth
P – Preterm birth
A – Abortions and Miscarriages
L – Living children
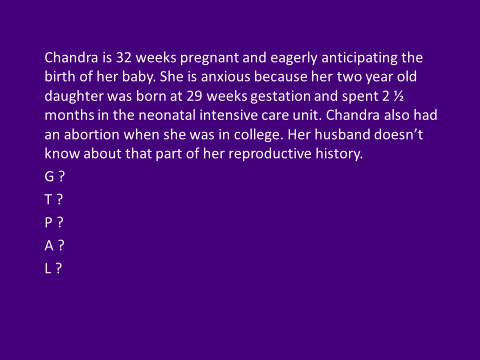
G- 3
T- 0
P-1
A- 1
L- 1
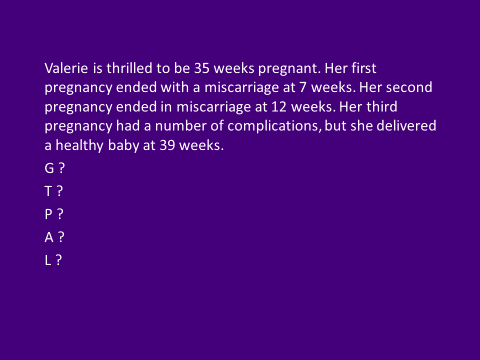
G- 4
T- 1
P- 0
A- 2
L-1
...
Uterus Changes in Pregnancy:
- What is hegar sign
- What are false contractions called
- What is bouncing of the baby in utero called
- what is quickening
- high levels of estrogen and progesterone stimulate growth in first tri.
-
- Due to increased vascularity, dilation of blood vessels, hyperplasia and hypertrophy and decidua.
- By 7 wk uterus = hen egg, 10=orange, 12= grapefruit.
- After third month growth due to fetus.
- 2nd trimester= uterine shape not pear anymore now globular. Then rises from pelvis to abdominal cavity. Start showing by 14-20 wks
- Uterus palpated above symphysis pubis 12-14 wk. at umbilicus at 22-24 wk, to xyphoid prcess at term. Then 38-40 wk, fundal height decreases and goes into pelvis (lightening).
- 6 wk= hegar sign, softening of the uterus and flexibility-press on wall of bladder= have to pee
- Braxton hicks contractions- false contractions.
- Uteroplacental blood flow: increases with size increase.
- More oxygen, uterine soufflé or bruit can be heard.
- Funic soufle is fetal blood moving through umbilical cord.
- Fetus changes:ballottment: passive movement of unengaged fetus- moving fetus up and down, bouncing gently and feeling rebound.
- Quickening-first fetal life recognition movement. 16-20 wks.
Cervical changes in pregnanyc:
what is chadwhick versus goodell sign
- Cervical:
- softening begins 6 wk.
- goodell sign = hypertrophy, vascularity, hyperplasia (red).
- Friability is increased= easily damaged tissue and bleeding.
- Chadwick sign: blue
Vagina and vulva
What is operculum
- Vagina and vulva:
- Operculum: mucosa thickens- mucus block to protect from infection. Ph is more acidic. 3.5-6.0. this makes her vulnerable to yeast infections though.
- connective tissue loosen, smooth muscle hypertrophy and vaginal vault to lengthen. Chadwick sign= more blood flow = bluish vaginal mucosa and cervis.
- Leukorrhea is white gray mucus and musty odor, white due to excess epithelial cells.
- Increased sensitivity due to vascularity of vagina. High degree of sexual interest and arousal.
- Edema and varicosities. External structures are enlarged due to more vascularity.
Breast changes
- fullness, sensitive, tingling, heaviness, pigmented nipples, hypertrophy of sebasious glands, Montgomery tubercles.
- Striae gravidarum.
- Colostrum-yellow fluid secreted during second trimester.
Cardiovascular changes
BP, blood flow, hr, coaguability?
Slight hypertrophy:bigger heart: moves and rotates due to the fetus
pushing.
Blood pressure: same, but decreases in third
trimester
Blood volume and composition: increases significantly
during pregnancy by approximately 30% to 45%
Cardiac output:
increases
Circulation and coagulation times
Pregnancy is
considered a hypercoagulable state : @ risk for DVT
Pulse: Apical impulse shifts. 20 weeks, audible splitting of s12 and 3. Maternal hr begins increasing at wk 5 but increases by 10-15 by 32 week.
Respiratory changes
- Pulmonary: ribs move due to estrogen relaxation. Upper resp is more vascular.
- become thoracic breathers
Renal
- urine, ureters
- Renal: renal pelvis and utereters dilate.
- Urine contains more nutrients and sugars= more at risk for urinary tract infection.
- Fetus pushing on bladder=Nocturia, bladder irritated, urinary urgency and frequencey.
- Integrementery:
malasma: darkened pigmentation- especially in dark skinned people
Linea nigra- from symphimas pubis to top of fundus.
Striae gravadrum. PUPPP: pruritic, uriticaric, plaques and papules of pregnancy. – red marks on ab.
muskuloskeletal
-Musckuloskletal: relaxin hormones +progesterone relaxes bones, ribs are relaxed so you can fit the baby.
Pelvis- relactin makes it loser. Hip pain joint pain, waddleing.
Posture changes- lower back change. Walk straight. Belly band.
Carpel Tunnel
GI changes
GI, mouth, appetite, liver
Gastrointestinal system
Appetite- decreased
Mouth- raised
red bumps sometimes
Esophagus, stomach, and intestines: decreased
GI motility= constipation
Gallbladder and liver- distended
gallbladder, decreased muscle tone, increasted emtying and thick bile=
can cause gallstones. Liver sometimes retains bile= itching and
jaundice sometimes
Abdominal discomfort: Pyrosis (heartburn) (due
to LES loosening), Ptyalism (excessive salivation)
Appendicitis
can be difficult to diagnose in pregnancy because the appendix is
displaced upward and laterally
Sonograms in pregnacy
- If woman is definite about their last menstrual period (ie first day of her last period), then you don’t need to go with a sonogram.
- Best time to date with a sonogram is first trimester, second trimester is a couple weeks off, third trimester is about three weeks off.
induction in wmoen with previous scars
- Don’t give induction medicines to women not in labor with a previous scar. Cervical massage is an acceptable alternative along with fetal testing to ensure placenta is still functioning well and baby is okay.
- Cook catheter great way for mechanical dilation for women who can’t get meds due to previous scars.
- Decreased muscle tone during pregnancy contributes to 3 things.
- Decreased muscle tone during pregnancy contributes to heartburn, reflux, and constipation.
- Dilation of renal pelves and ureters during pregnancy increases the risk of ______.
UTI
Change in hr in pregnancy
- Heart rate increases 10 to 15 beats/minute by 32 weeks of gestation and persists until term.
Anemia in pregnancy due to
- Physiologic anemia of pregnancy results from increase in plasma volume greater than the increase in red blood cells.
Common antepartum complications
- Gestational Diabetes
- Hyperemesis Gravidarum
- Hypertension
- Hemorrhagic Disorders
Diabetes Mellitis
- Diabetes mellitus (DM)
- Affects 4% to 14% of pregnant women
- Pregnancy complicated by diabetes is considered high risk
- Pathogenesis
- Group of metabolic diseases characterized by hyperglycemia resulting from defects in insulin secretion, insulin action, or both
- Body compensates for its inability to convert glucose into energy by burning muscle and fats
- Key to an optimal outcome is strict glycemic control
Diabetes Mellitis classifications and types
- Classification
- Type 1 diabetes
- Absolute insulin deficiency
- Type 2 diabetes
- Relative insulin deficiency
- Gestational diabetes mellitus (GDM)
- Pregestational diabetes mellitus
- Label given to type 1 or 2 diabetes that existed prior to pregnancy
- White’s classification system
- New ADA system (distinguishes with or without vascular complications)
Glucose changes in pregnnacy
- Metabolic changes associated with pregnancy
- Normal pregnancy is characterized by alterations in maternal glucose metabolism, insulin production, and metabolic homeostasis
- Glucose is the primary fuel for the fetus
- Glucose crosses the placenta, insulin does not
- Insulin needs increase during the first trimester
Gestational Diabetes
Complicates 3% to 9% of all pregnancies
Fetal risks
- No increase of birth defects if develop GDM after the first trimester
- At risk for macrosomia and associated birth trauma and neonatal hypoglycemia
Macrosemia vs. LGA
- Macrosomia is either greater than 8 lbs 13 oz or 9 lbs 15 oz
- LGA is weight, head circumference, or length greater than 90th or 97th percentile.
- Can be both
macrosmia causes risk for...
shoulder dystopia
Screening for gestational diabetes:
1. What makes them at high risk for GDM:
2. Screening
-screening:
1. High risk: obesity, corticosteroids, hx of gdm in previous pregnancies, races AA, NA Asian
2. Screen:
-1 hour glucose testing test, glucola, sweet orange juice- draw one bloodwork or finger gluocse to see level- if over 130= positive
-Do between 24 and 28- if positive do a longer test, a fasting, 1hr, 2hr and 3hr.
-if before 20 weeks evaluated probably diabetes not GDM
GDM care management: Antepartium
- Antepartum:
- Diet
- Exercise
- Self-monitoring of blood glucose:
- 4x a day!, fasting 1hr post prandial, 2hrs. Decrease to 2 or if stable to only fasting Pharmacologic therapy: glyburide
- Fetal surveillance
GDM Care: Intrapartum
- Intrapartum
- Blood glucose monitored hourly in labor
- Infusion of regular insulin
GDM care: postpartum
- Postpartum
- Will return to normal glucose levels after birth
- Likely to recur in future pregnancies
Key points for diabetes in pregnancy
- Poor glycemic control before and during pregnancy in women who have diabetes can lead to maternal and fetal complications.
- Careful glucose monitoring, medication administration when necessary, and dietary counseling are used to create a normal intrauterine environment for fetal growth and development in the pregnancy complicated by diabetes mellitus.
- Because GDM is asymptomatic in most cases, all women who are not known to have pregestational diabetes undergo routine screening by history, clinical risk factors, or laboratory assessment of blood glucose levels during pregnancy.
Hyperemesis Gravidarum
- Normal nausea and vomiting complicates 50% to 80% of all pregnancies, typically beginning at 4 to 10 weeks of gestation, usually resolving by 20 weeks of gestation
-
Hyperemesis gravidarum is
excessive, prolonged vomiting accompanied by the following:
- Weight loss
- Electrolyte imbalance
- Nutritional deficiencies
- Ketonuria
Assessment for HG
- Assessment
- Assess severity
- Weight, V/S, presence of ketonuria
- Psychosocial assessment: role of anxiety
Initial Care for HG: can be done outpatient!
- Intravenous (IV) therapy for correction of fluid and electrolyte imbalances
- Medications: Zofran can cause ceft palate, but they still give it, especially after 14 wks.
- Enteral or parenteral nutrition as a last resort
- Nursing interventions
Key points for managing HG
- The woman with hyperemesis gravidarum may have significant weight loss and dehydration. Management focuses on restoring fluid and electrolyte balance and preventing recurrence of nausea and vomiting.
Women with hyperemesis gravidarum:
a.Are a majority, because 80% of all pregnant women suffer from it at some time
b.Have vomiting severe and persistent enough to cause weight loss, dehydration, and electrolyte imbalance
c.Need IV fluid and nutrition for most of their pregnancy
d.Often inspire similar, milder symptoms in their male partners and mothers
B
Hypertensive Disorders: background and significance
- Common medical complication of pregnancy
- Hypertensive disorders are a major cause of perinatal morbidity and mortality worldwide due to the following:
- Uteroplacental insufficiency
- Premature birth
- Of maternal deaths worldwide, 10% to 15% can be attributed to preeclampsia and eclampsia.
- Preeclampsia accounts for more than 50,000 maternal deaths each year.
Morbidity and Mortality due to HTN Disorders
- Morbidity
- Renal failure
- Coagulopathy
- Cardiac or liver failure
- Placental abruption
- Seizures
- Stroke
- Mortality
- Pregnancy-related hypertension accounts for 10% to 15% of maternal deaths worldwide.
Types/Classification of HTN disorders
1. Gestational HTN
2. Preeclampsia
3. Eclampsia
4. Chronic HTN
5. Chronic HTN w/ superimposed preeclampsia
Gestational HTN:
- Onset of hypertension without proteinuria or other systemic findings diagnostic for preeclampsia after week 20 of pregnancy
- Systolic BP >140 or diastolic BP >90
Systolic over 140 or diastolic over 90 is ______________.
Systolic over 160 or diastolic over 110 is __________________.
1. hypertensive
2. very concerned
Preeclampsia definition
- Pregnancy-specific condition in which hypertension and proteinuria develop after 20 weeks of gestation in a previously normotensive woman
- In the absence of proteinuria,
preeclampsia may be defined as hypertension along with the
following:
- Thrombocytopenia
- Impaired liver function
- New development of renal insufficiency
- Pulmonary edema
- New-onset cerebral or visual disturbances
- THIS CONDITION DOES NOT GET BETTER UNTIL BABY IS BORN!
common feature of gest. htn and preecclampsia
What is a common feature of gestational HTN and preeclampsia?
Chronic HTN and
Chronic HTN w/ superimposed preeclampsia
- Chronic hypertension:
- Hypertension present before pregnancy or diagnosed before week 20 of gestation
- Chronic hypertension with superimposed preeclampsia:
- Women with chronic hypertension may acquire preeclampsia or eclampsia
- Can be difficult to diagnose
Preeclampsia etiology
- Etiology
- A condition unique to human pregnancy
- Common risk factors
- Primigravidity in woman <19 or >40 years of age
- First pregnancy with a new partner
- History of preeclampsia
- The cause of preeclampsia is unknown.
- Many theories
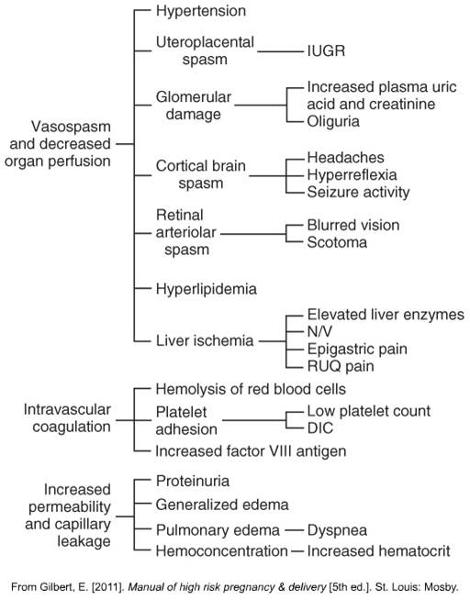
Preeclampsia pathophysiology
- Pathophysiology
- Progressive disorder with placenta as the root cause
- Begins to resolve after the placenta has been expelled
- Spiral arteries in the uterus normally become larger and thicker to handle increased blood volume.
- This vascular remodeling does not occur or only partially develops in women with preeclampsia and decreased placental perfusion and hypoxia result.
- DOES NOT RESOLVE UNTIL AFTER PLACENTA IS GONE!
Preeclampsia pathophysiology 2: what does this mean happens?
- lPathophysiology
- Placental ischemia → endothelial cell dysfunction
- Generalized vasospasm → poor tissue perfusion in all organ systems
- Increased peripheral resistance and blood pressure (BP)
- Increased endothelial cell permeability
- Reduced kidney perfusion
- Plasma colloid osmotic pressure decreases.
- Decreased liver perfusion
- Neurologic complications
labs for preeclampsia
- Kidney function
- Chem sevens
- Uric acid, BUN,
- Liver function tests to establish baseline, then recheck one week later.
What does Right upper gastric pain test in preeclampsia
-Upper gastric is liver backing up!
What does Headache, blurred vision, swelling mean in preeclampsia
retinal spasm and cortical brain spasm
edema where is most important
hands nad face
Chart on what happens in preeclampsia and s&sypmtoms
Corticobrain spasm causes what three things?
Identifying and preventing preeclampsia
- No reliable test or screening tool has been developed
- Low-dose aspirin (60 to 80 mg) may help certain high risk women
Assessment and Nurising Diagnoses for Preeclampsia
What is HELLP syndrome in preeclampsia
- Accurate measurement of BP
- Assessment of edema, although the presence of edema is no longer included in the definition of preeclampsia
- Deep tendon reflexes (DTRs)
- Assess for hyperactive reflexes (clonus) (uauLLY THIS OCCURS PRIOR TO SEIZURE)
- Proteinuria: ideally determined by evaluation of a 24-hour urine collection
- Evaluate for signs
and symptoms of severe preeclampsia:
- Headaches
- Epigastric pain
- Right upper quadrant abdominal pain
- Visual disturbances
- HELLP: hemolysis, elevated liver enzymes, and low platelet
Interventions Preeclampsia mild
- Mild gestational hypertension and preeclampsia without severe
features
- Goals of therapy are to ensure maternal safety and deliver a healthy newborn close to term.
- Home care
- Maternal and fetal assessment
- Activity restriction
- Diet
Interventions preeclampsia SEVERE
wHEN DO PREECLAMPSIA PT USUALLY HAVE THE BABY?
- Severe gestational hypertension and preeclampsia with severe
features
- Goals of care are to ensure maternal safety and formulate a plan for delivery.
- Intrapartum care
- Bed rest with siderails up
- Darkened environment
- Magnesium sulfate therapy
- Antihypertensive medications
- AT 37 WEEKS, THE RISKS OUTWEIGH THE BENEFITS OF KEEPING THE BABY IN. THEY WILL INDUCE
When is delivery usually called for before 39 weeks
Consistent 160/110, organ compromise, or consistent elevated labs call for delivery regardless of whether 39 weeks has been reached.
After 1st preeclampsia pregnancy will I have another, or HTN?
- Women with preeclampsia with severe features have a significantly increased risk of developing preeclampsia in a future pregnancy.
- These women have an increased risk of developing chronic hypertension and cardiovascular disease later in life.
- For now, women should be educated about lifestyle changes (maintaining a healthy weight, increasing physical activity, and avoiding smoking) that may decrease the risk for developing future health problems.
Key points preeclampsia
- Hypertensive disorders during pregnancy are a leading cause of maternal and perinatal morbidity and mortality worldwide.
- The cause of preeclampsia is unknown, and there are no known reliable tests for predicting women at risk for developing preeclampsia.
- Preeclampsia is a multisystem disease.
-
- Magnesium sulfate, the anticonvulsant of choice for preventing or controlling eclamptic seizures, requires careful monitoring of reflexes, respirations, renal function, and mental status.
- Women with preeclampsia (especially early-onset and preeclampsia with severe features) have an increased risk of developing chronic hypertension and cardiovascular disease later in life.
A client at 36 weeks of gestation presents to labor and delivery complaining of a constant headache for the past 2 days. She also states that her face “seems more swollen than usual.” What should be the nurse’s first action?
a.Obtain a urine sample.
b.Place the client on a fetal heart monitor.
c.Notify the physician of the client’s concerns.
d.Take the client’s blood pressure.
D
why do we want a babe to make it to 34 wks
what do we give then if required delivery
try to keep baby in for 34 weeks to allow for lung maturation and ensure baby will be able to breathe on its own once born.
Give betamethasone in case delivery before 34 weeks is required.
Antepartal Hemorragic Disorders: why are they a big deal and what are people at risk for?
- Bleeding in pregnancy jeopardizes maternal and fetal well-being.
- Maternal blood loss decreases oxygen-carrying capacity and increases risk for the following conditions:
- Hypovolemia
- Anemia
- Infection
- Preterm labor
- Impaired oxygen delivery to the fetus
Fetal risks from maternal hemmorage
- Fetal risks from maternal hemorrhage
- Blood loss, anemia
- Hypoxemia
- Hypoxia
- Anoxia
- Preterm birth
- Hemorrhagic disorders in pregnancy are medical emergencies.
- The incidence and type of bleeding vary by trimester.
Early Pregnancy Bleeding usually results in this
- Miscarriage (spontaneous abortion): a pregnancy that ends as a result of natural causes before 20 weeks of gestation
- Approximately 10% to 15% of pregnancies end in miscarriage.
- Types of miscarriages
- Threatened
- Inevitable
- Incomplete
- Complete
- Missed
- Recurrent
Types of miscarriages and what they mean
-Threatened: bleed a little, still viable. Do sonogram-check fetal heart
-Inevitable: mom bleeding heavier, expelling everything- provide supportive measures.
-Incomplete: tissue comes out, rather than formed fetus. Blood tissue clots- expel some of it, but some still stuck inside- intervene, send for scraping and vaccuuming.
-Complete- everything comes out. No more disconfort- severe cramping, getsrid of everything, uterus stops crampong.
-Missed- no bleeding, but no heart beat. Abortion. 3 fold treatment: expectant – let the body do it itself. 2nd is medical intervention = misoprostil- use for inducing missed miscarriage.
-Recurrent: probably need sto go to reproductive med. 3 is a lot of babys to lose. >35 needs to go to see a specialist.
-Recurrent-
Miscarriage Management
- Miscarriage care management
- Assessment and nursing diagnoses
- Initial care
- Depends on the classification of the miscarriage and on signs and symptoms
- Expectant management
- Medical management: misoprostol (Cytotec)
- Surgical management: dilation and curettage (D&C)
- Follow-up care
- Follow-up phone calls; support groups
What is an ectopic Pregnancy
incidence and etiology
clinical manifestations
- Ectopic pregnancy: the fertilized ovum is implanted outside the uterine cavity; also called “tubal pregnancies”
- Incidence and etiology
- Clinical manifestations
- Typically s/s occur 6 to 8 weeks after the last normal menstrual period
- The three most classic symptoms are the following:
1.Abdominal pain
2.Delayed menses
3.Abnormal vaginal bleeding (spotting)
More on ectopic pregnancies, what do you do
-ectopicà lifethreatening. Instead of imbedding into the uterus, it is imbedded into follopian tubes. May rupture! ED
- PAIN! One sided pain not general cramping.
-Ectopic severe pain on the tube side.
-Sonogram to determine where it is.
-Ectopicàgive meds to abort.
Late Pregnancy bleeding:
Placenta Previa
- Placenta previa
- Placenta implanted in lower uterine segment near or over internal cervical os
- Degree to which the internal cervical os is covered by placenta used to classify three types
- Complete placenta previa
- Marginal placenta previa
- Low-lying placenta
placenta previa
incidence
manifestations
maternal fetal outcomes
- Placenta previa (Cont.)
- Incidence and etiology
- 1 in 200 pregnancies
- Clinical manifestations
- Painless bright red vaginal bleeding during second or third trimester
- Maternal and fetal outcomes
- Major complication is hemorrhage
- Fetal death (caused by preterm birth)
- Stillbirth, malpresentation, fetal anemia, intrauterine growth restriction (IUGR)
placenta previa: diagnoses and care management
- Diagnosis
- Transabdominal ultrasound examination
- Care management
- Expectant management
- Home care
- Active management
Placental Abruption, premature
Risk factors?
- Premature separation of placenta (abruptio placentae) [placental abruption]
- Detachment of part or all of placenta from implantation site after 20 weeks of gestation
- Occurs in 1 in 75 to 1 in 226 pregnancies
Maternal hypertension is a primary risk factor
Placental Abruptions:
manifestations
diagnoses
- Premature separation of placenta (abruptio placentae) [placental abruption] (Cont.)
- Clinical manifestations
- Separation may be partial, complete, or only involve margin of placenta
- Vaginal bleeding, abdominal pain, and uterine tenderness and contractions
- Boardlike abdomen; Couvelaire uterus (discolered ab)
- Maternal and fetal outcomes
- Diagnosis
- Management
- Expectant
- Active
- WILL NEED CSECTION-
- See bright red bleeding= V/s and change position.
key points hemmoragic disorders
- Blood loss during pregnancy should always be regarded as a warning sign until the cause is determined.
- Some miscarriages occur for unknown reasons, but fetal or placental maldevelopment and maternal factors account for many others.
- The type of miscarriage and signs and symptoms direct care management.
-
- Ectopic pregnancy is a significant cause of maternal morbidity and mortality.
- Placenta previa and placental abruption are differentiated by type of bleeding, uterine tonicity, and presence or absence of pain.
- Management of late-pregnancy bleeding requires immediate evaluation; care is based on gestational age, amount of bleeding, and fetal condition.
What is the passenger during labor?
- what is important in the passenger
What is the presentation?
Passenger: fetus
Size of the fetal head
Bones in the fetal skull
Fontanels
Molding
Presentation of the fetus: the part of the fetus that enters the pelvic inlet first and leads through the birth canal during labor
Cephalic
Breech
Shoulder
More to do with the passenger:
What is the hardest part of passenger to come through? Why can this part come through okay?
When should they lie in a cephalic position by? and why?
What do they do if the baby is not cephalic?
What does cephalic mean?
What does breech mean?
What does scapula mean
Transverse??
Passenger: Hardest part is head, which needs to maneuver and come out first.
Majority come out head first.
Should be in cephalic position by 37 weeks (term) baby is big, and cant maneuver.
Will do an external rotation if not in cephalic at 37 weeks. Decreases csection rates.
Cephalic- head down
Breech- sacrum down
Scapula- shoulder
Transverese
Fetal head: not completely fused, even though they have bones- don’t fuse till 18 montsh of age. helps with birth because still moveable. Biparietal diameter is the largest piece to get through thte pelvis.
Fetal position means:
What is cephalic
Vertex?
ROA?
LOA?
Rot/Lot
Rop//Lot
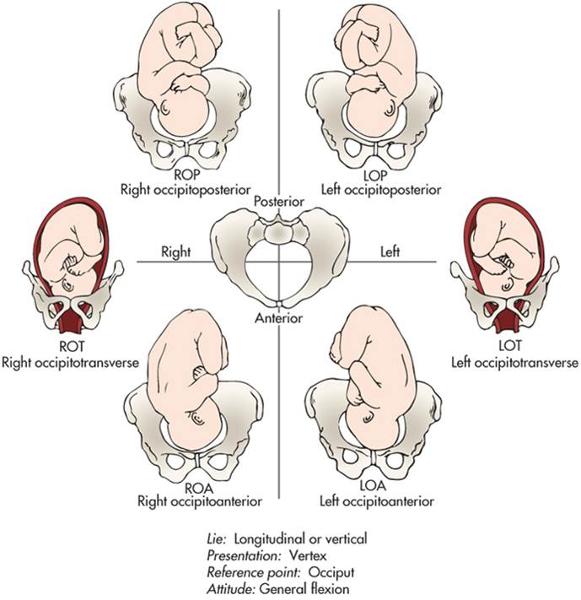
Fetal position : the relationship of a reference point on the presenting part to the four quadrants of the mother’s pelvis
Position is denoted by a three-part letter abbreviation
Vertex= cephalic/head first.
-Roa and loa are most common
-ROA- has to do with the bone.
-Put heart rate monitor on back .
-ROT-
-ROP, LOP- posterior.
-Transvere and posterior tak e a little longer and it is more uncomfortable.
Factors affecting the labor of the passenger:
Fetal lie
vs
Fetal attitude
Fetal lie : the relation of the long axis (spine) of the fetus to the long axis (spine) of the mother
Longitudinal/
Vertical
Fetal lie- in relation to long axis of spine in baby and mom
- longitudinal/vertical is straight up and down in relationship to mom spine
- transverse is horizontal
Fetal attitude : the relation of the fetal body parts to one another
General flexion
Fetal position
Fetal Station
Fetal Engagement
What landmark do we use to measure these?

Fetal position : the relationship of a reference point on the presenting part to the four quadrants of the mother’s pelvis
Position is denoted by a three-part letter abbreviation
Fetal station : a measure of the degree of descent of the presenting part of the fetus through the birth canal
Fetal engagement : usually corresponds to 0 station
*-Ischial spines is important landmark- most narrow diameter that baby needs to go through, talking about station that is the point of reference. O statioin is ischial spines. Anything above is negative. Anything below it is positive.
-+4 you usually can see the head.
What is the passageway
Passageway: Birth canal
- Bony pelvis
- Soft tissues
2 openings, goes into inlet, comes out the outlet (spines, tuberosities and arch)
Powers during labor:
primary vs secondary and what effects both of these powers
Powers
Primary powers: contractions
Frequency, duration, intensity
Effacement
Dilation
Secondary powers: bearing-down efforts
Valsalva maneuver
Laboring Down
Positition and psychologic state of pt affecting labor
Position of laboring woman
Discussed in depth in Chapter 19
Psychologic state of laboring woman
Discussed in depth in Chapter 19
The process of labor begins w/ something in the cervix happening? What comes first
Thinning-->dilation-->decent of fetus
How the fetus comes through in labor
Mechanism of labor
THIS ISIMPORTANT
Seven cardinal movements
Mechanism of labor
Turns and adjustments necessary in human birth process
Seven cardinal movements of mechanism of labor
1.Engagement
2.Descent
3.Flexion
4.Internal rotation
5.Extension
6.Restitution and external rotation
7.Expulsion
Each cardinal movement explained
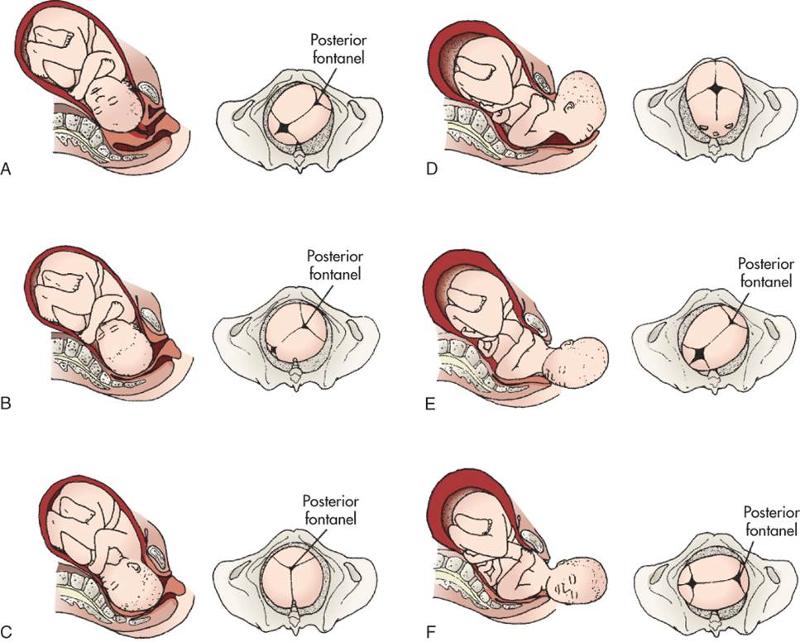
1.Engage: goes through internal inlet.
2.Descent – move down.
(0 station is engaged and descended
3. Pelvic muscle flexes neck
4. internally rotaiton of head to get out of bony pelvic outlet
5. Extension of head to say hell
6. Restitution and aligns head with shoulders, head moves back
7. expulsion- baby pops out.
cardinal again
- Engagement - the biparietal diameter of the head passes the pelvic inlet, the head is said to be engaged in the pelvic inlet.
- Descent - refers to the progress of the presenting part through the pelvis. descent depends on at least four forces: 1. pressure exerted by the amniotic fluid, 2. direct pressure exerted by the contracting fundus on the fetus, 3. force of the contraction of the maternal diaphragm and abdomnial muscles in the second stage of labor, and 4. extension and straightening of the fetal body. The degree of descent is measured by the station of the presenting part.
- Flexion - as soon as the descending head meets resistance from the cervix, pelvic wall, or pelvic floor, it normally flexes so that the chin is brough into closer contact with the fetal chest. flexion permits the smaller subooccipitobregmatic diamter rather than the larger diameters to present to outlet.
- Internal rotation - the maternal pelvic inlet is widest in the transverse diameter; therefore, the fetal head passes the inlet into the true pelvis in the occipitotransverse position. the outlet is widest is the anteroposterior diameter; for the fetus to exit, the head must rotate. The head is almost always rotated by the time it hits the pelvic floor. both the levator ani muscles and the bony pelvis are important for achieving anterior rotation. a previous childbirth injury or regional anesthesia may compromise the function of the levator sling.
- Extension - the fetal head reaches the perineum for birth, it is deflected anteriorly by the perineum.
- Restitution and external rotation - After the head is born it rotates briefly to the position it occupied when it was engaged in the inlet. this movement is referred to as restitiution.
- Expulsion - after birth of the shoulders, the head and shoulders are lifted up toward the mother’s pubic bone and the trunk of the baby is born by flexing it laterally in the direction of the symphysis pubis.
Four stages of labor: know these
The first stage of labor lasts from the time dilation begins to the time when the cervix is fully dilated.
The second stage of labor lasts from the time of full cervical dilation to the birth of the infant. (even if she is laboring down)
The third stage of labor lasts from the infant’s birth to the expulsion of the placenta.
The fourth stage of labor begins with the delivery of the placenta and includes at least the first 2 hours after birth. (q15 monitoring)
5 ps of pregnancy
Labor and birth are affected by the five Ps: passenger, passageway, powers, position of the woman, and psychologic response.
factors affecting pain response in laboring women
Physiologic factors
Culture
Anxiety
Previous experience
Gate-control theory of pain
Comfort
Support
Environment
Non pharmacologic pain measures
Childbirth preparation methods
Relaxing and breathing techniques
Focusing and relaxation
Breathing techniques
Effleurage and counterpressure
Touch and massage
Therapeutic touch
Application of heat and cold
non pharmaco pain methods
Acupressure and acupuncture
Transcutaneous electrical nerve stimulation
Water therapy (hydrotherapy)
Intradermal water block
Aromatherapy
Music
Hypnosis
Biofeedback
Pharm pain methods: anaelgesia vvs. anesthesia
Anesthesia encompasses analgesia, amnesia, and relaxation
Analgesia : the alleviation of the sensation of pain or the raising of the threshold for pain perception without loss of consciousness
The type of analgesic or anesthetic chosen is determined in part by the stage of labor of the woman and by the method of birth planned.
FENTANYL GREAT
Two types of anesthesia
Systemic analgesia
Nerve block analgesia and anesthesia
Epidural anesthesia or analgesia (block): currently the most effective pharmacologic pain relief method for labor
Combined spinal-epidural (CSE) analgesia: sometimes referred to as a “walking epidural,” although women often choose not to walk because of sedation and fatigue, abnormal sensations in and weakness of the legs, and a feeling of insecurity
Epidural and intrathecal (spinal) opioids
Nursing guidelines for pharm therapies
General informed consent
Informed consent for anesthesia
Timing of administration
Preparation for procedures
Administration of medication
Intravenous route
Intramuscular route
Regional (epidural or spinal) anesthesia
Safety and general care
When are sedatives a good idead?
What is narcan used for
Sedatives may be appropriate for women in prolonged early labor when there is a need to decrease anxiety or promote sleep or therapeutic rest.
Naloxone (Narcan) is an opioid (narcotic) antagonist that can reverse narcotic effects, especially respiratory depression.
Pharmacologic control of pain during labor requires collaboration among the health care providers and the laboring woman.
use of an epidural vs general
Epidural anesthesia and analgesia are the most effective available pharmacologic pain relief methods for labor.
General anesthesia is rarely used for vaginal birth but may be used for cesarean birth or whenever rapid anesthesia is needed in an emergency childbirth situation.
W/ anesthesia: what happens to moms bp, moms hr, and babies hr
bp down
hr up in mom
hr down in baby
Different fetal monitoring techniques
Intermittent auscultation :
Listening to fetal heart sounds at
periodic intervals to assess FHR
Easy to use, inexpensive, less
invasive than EFM
Difficult to perform on women who are
obese
Does not provide a permanent record
Electronic fetal
monitoring:
External monitoring
Ultrasound transducer
Toco transducer (tocodynamometer)
Electronic fetal monitoring techniques:
Electronic fetal monitoring (Cont.):
Internal
monitoring
Spiral electrode
Intrauterine pressure catheter
(IUPC) -->can insert fluid through this!
Display: displayed on
the monitor paper or computer screen, with the FHR in the upper
section and UA in the lower section
Fetal HR patterns:
What is baseline HR?
Baseline fetal heart rate
- Average rate during a 10-minute segment
- There must be at least 2 minutes of interpretable data
- Should be 110-160
What is variabilitiy
uVariability
uDescribed as irregular waves or fluctuations in the baseline FHR of two cycles per minute or greater
u4 possible categories of variability:
uAbsence
uMinimal
uModerate
uMarked
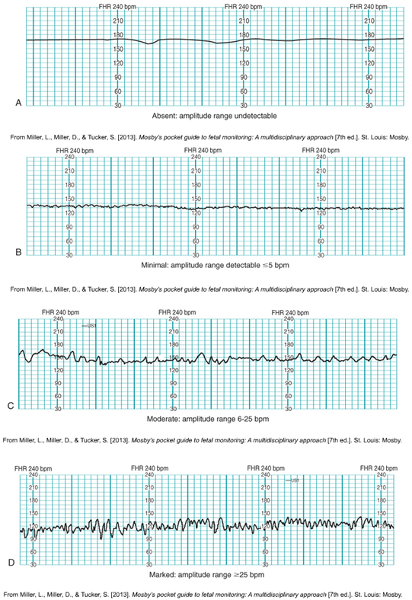
Variability patterns:
Normal baby- hr fluctuates.
A- absent fluctuations, CONCERNED!
B: minimal variability- less than 5 bpm change in fluctuation
C- 6-25 bpm fluctuations- moderate variability
D- Marked-active baby!
Dark blue lines a minute
Little squares are 10 seconds
Another rare finding

Rare event= IN TROUBLE . Fetal anemia- moms blood type doesn’t match, rh- and +
Fetaal tachycardia and bradycardia levels
Bradycardia= <110.
Tahy= >160
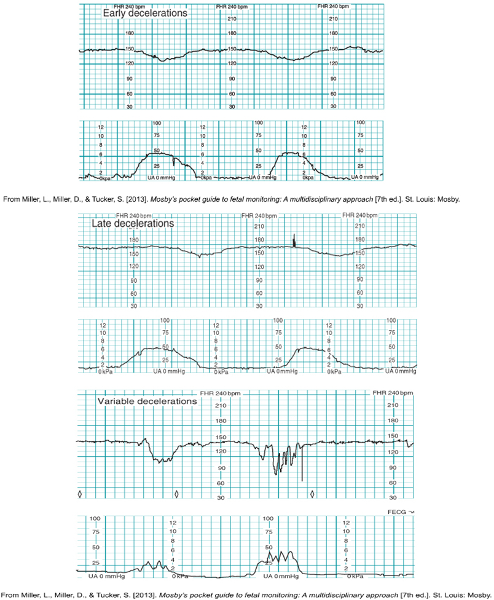
Change in fetal HR : what is a deceleration
Changes in FHR (Cont.):
Decelerations:
Early
decelerations in response to fetal head compression (mirrors
contractions, head is hitting pelvic floor, compressing cerebral blood
flow. NORMAL
Late decelerations due to
uteroplacental insufficiency-
WORRY- due to blood flow insufficiency: contraction happens, decel happens after the contraction.
Variable decelerations due to umbilical cord compression
NOT variability, is due to umbilical cord compression. No pattern to variable decels. V for variable- SHARP dip. Baby may be leaning on cord, need to turn mom off of that cord.
Prolonged decelerations:;
lasting longer, 2 minutes, 5 minutes,2-10min is polonnged, tryin to get her to move, get it to get back up.
what is acceleration
- Acceleration - is defined as a visually apparent abrupt (onset to peak less than 30 sec) increase in FHR above the baseline rate. the peak is at least 15 beats/minute above the baseline, and the acceleration lasts 15 seconds or more, with a return to baseline less than 2 minutes from the beginning of the acceleration. before 32 weeks of gestation the definition of an acceleration is a peak of 10 beats/minute or more above the baseline and a duration of at least 10 seconds. acceleration of the FHR for more than 10 minutes is considered a change in baseline rate.
- can be either periodic or episodic. Similar to moderate variability, accelerations are considered an indication of fetal well-being. their presence is highly predictive of a normal fetal acid-base balance.
Categories for fetal hr's
uCategory I: normal
uCategory II: indeterminate
uCategory III: abnormal
Category I
uBaseline FHR in the normal range of 110-160 beats/min
uBaseline fetal heart rate variability: moderate
uLate or variable decelerations: absent
uEarly decelerations: may be present or absent
uAccelerations: either present or absent
Category II
uBradycardia not accompanied by absence of baseline variability
uTachycardia
uMinimal or absence of baseline variability not accompanied by recurrent decelerations
uMarked baseline variability
uNo accelerations in response to fetal stimulation
uPeriodic or episodic decelerations
Category III
uNonreassuring FHR patterns associated with fetal hypoxemia
uHypoxemia can deteriorate to severe fetal hypoxia
uAbsence of baseline variability
uRecurrent or late decelerations
uBradycardia
uSinusoidal pattern
5 Essential parts to a fetal HR
The five essential components of the FHR tracing that must be evaluated regularly are baseline rate, baseline variability, accelerations, decelerations, and changes or trends over time.
Components of Intrauterine resuscitation
If any component is abnormal, corrective measures must be taken immediately to improve fetal oxygenation: intrauterine resuscitation
Supplemental oxygen
Maternal position changes
Increasing intravenous fluids
1.While evaluating an external monitor tracing of a woman in active labor whose labor is being induced, the nurse notes that the fetal heart rate (FHR) begins to decelerate at the onset of several contractions and returns to baseline before each contraction ends. The nurse should:
a.Change the woman’s position
b.Discontinue the oxytocin infusion
c.Insert an internal monitor
d.Document the finding in the client’s record
D, document
this is a normal finding!