immunology
The branch of biology and biomedicine concerned with the structure and function of the immune system, innate and acquired immunity, the bodily distinction of sself from nonself, and laboratory techniques involving the interaction of antigens with specific antibodies
immunogenicity
The property of being able to evoke an immune response within an organism; it depends partly on the size and complexity of the substance (antigen) in question and partly on how unlike the substance is in comparison to the host's molecules (self-antigens)
immune specificity
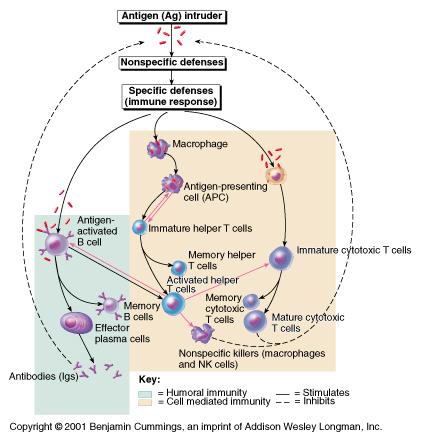
The central property of the immune system which is its ability to respond to a vast array of substances (antigens) individually by the production of responsive clones of activated and memory lymphocytes which generate the various defenses against the antigen; the key to individualized response is the combonation of a genetic library, the Major Histocompatibility Complex, capable of elaborating the array of cell surface markers which allow immune cells to recognize and cooperate with each other and to be able to distinguish foreign from self molecules. *NOTE- the ability of the immune system to respond to an antigen exists BEFORE it ever encounters that antigen
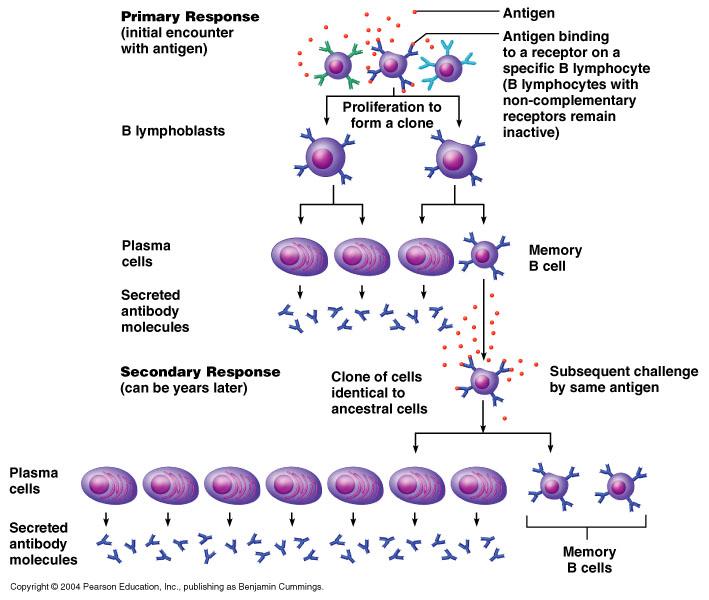
immunological memory
The property of the immune system which is its ability to respond to an antigen more rapidly and with greater efficiency in the second and subsequent encounters with the antigen; the memory response reflects the presence of a small population of T and B lymphocytes ("memory lymphocytes")which differentiate during the initial/primary response to the antigen; although the "memory" lymphocytees did not participate directly in the immune defenses in the primary response, they are present and capable of immediate response, includin proliferation and differentiation into active subclones of specific B and T lymphocytes in each subsequent encounter with the particular antigen
Diagram: immunological memory response
immunocompetence
The property of the immune system which is its normal capacity to develop a strong, effective immune response following exposure to an antigen
pathogen
Any living microorganism which has the potential to cause disease EX.viruses, bacteria, fungi, protozoans, and certain worms
resistance (to disease)/nonspecific resistance
The general term for all body defenses against injury and disease, which are non-specific in the sense of not being generated in response to specific foreign antigen(s)
List examples of nonspecific resistance
Ex. surface barriers (skin and mucous membranes)and their protective secretions (sweat, sebum, cerumen, tears, saliva, the acidity of urine, vaginal and gastric secreations), the processes of vomitting to expel toxins, inflammtions, phagocytosis, and fever, various antimicrobial proteins (lysozymes, complement, transferrins, interferons) and mediators of in flammation and fever (histamines, kinins, protaglandins, leukotrienes, etc.) and the action of Natural Killer (NK) lymphocytes
susceptability (to disease)
The property of an individual, an organ system, organ or tissue to be affected by diseasse; it is affected by envirnmental factors as well as genetic, developmental and nutritional factors which lowers one's resistance.
immunity
Inherited, acquired, or induced resistance to infection by a specific pathogen
abcess
A localized collection of pus in any internal part of the body (not on a surface such as the skin of a mucous membrane), formed by tissue disintegratin and surrounded by inflammed tissue, and perhaps walled off by scar tissue. AKA boil
ulcer
A crater-like lesion of the skin or mucous membrane, Ex. the linings of the respiratory, gastrointestional, and urogenitial systems, which is accompanied by formation of pus and necrosis and sloughing of surrounding tissue, usually resulting from inflammation or ischemia
metastasis
A secondary cancerous growth formed by transmission of cancerous cells from a primary growth (original site) to one or more sites elsewhere in the body, usually by way of the blood vessels or lymphatics; the potential for metastasis is a characteristic of almost all malignant cancers
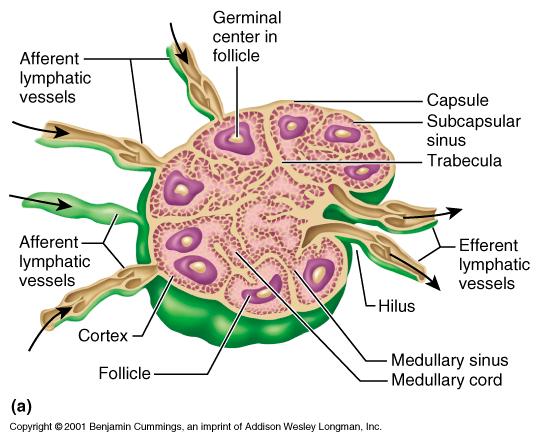
cortex
The outer layer of an organ or body structure, EX. the cerebrum, kidney, adrenal gland, or lymph node; the cortex of a lymph node contains many lymph follicles (dendritic cells surrounding germinal centers) which are separated by connective tissue trabeculae and the cortex contains a branching system of channels which route lymph from the afferent lymphatic vessels to the medulla; antigen-presenting macrophages and T and B lymphocytes in the cortex are involved in immune reactions to specific antigens
medulla
The inner core of an internal organ of body structure Ex. the cerebrum, kidney, adrenal gland, or lymph node; the medulla of a lymph node contains medullary cords (thin inward extensions of cortical lymphoid tissue) and lymph from the cortex to the efferent lmphatic vessels which carry lymph away from the lymph node at the hilus; the medulla also contains many macrophages
germinal center
The light staining interior of a lymph follicle which contains a few dendritic cells, some antigen-presenting macrophages and many activted proliferating T and B lymphocytes, particularly B lymphocytes, which are involved in immune reactions to specific antigens
medullary cord
A thin inward extension of cortical lymphoid tissue (T and B lymphocytes) which is bounded by lymph sinuses in the inner core (medulla) of a lymph node
afferent lymphatic vessel
Any of the delicate thin walled vascular tubes with valves which transport lymph from the tissue spaces into the interior of the cortex of a lymph node by passing the fluid through an opening in the capsule
efferent lymphatic vessel
Any of the delicate thin walled vascular tubes with valves which transport lymph from the interior (medulla) of a lymph node by exiting through an opening in the hilus and on through the lymphatic circulation
Diagram: Lymph Node
epidermis
The outer, pigmented, protective, innervated but nonvascular layer of keritinized stratified squamous epithelium covering the dermis; the epidermis gives rise to derivatives including hair, nails, sweat and sebaceous glands
mucous membranes
The general term for the specialized epithelial linings which produces a lubricating fluid containing the sticky protein mucin which traps microbes and dirt particles and protects and body structure which is continuous with the external environment except the skin itself
Examples of mucous membranes
Ex. the linings of the digestive, respiratory, and urogenital systems and the conjunctival lining of the eyes
mucous
The viscous, slippery substance which consists chiefly of the glycoprotein mucin, water, aloughed cells and leukocytes, and inorganic slats, and which is secreted, as a moistening and protective lubricant coating capable of trapping many microorganisms, by cells and glands of the mucous membranes of all the cavities which open externally
cilia
The minute hairlike processes, specilized membrane-bound microtubular cell organelles, only claerly observable in the electron microscope, which extend from the surface of a cell or unicellular organism; they are capable of rhythmical motion, and act in unison with other such structures to bring about movement of the cell or of the surrounding medium; in the human, they are found primarily on the cells lining the respiratory tree and the uterine tubes
lacrimal apparatus
Those accessory structures of the eye ehich function in the productin of tears including the lacrimal glands which synthesize the tears, and the drainage system for the tears, beginning with the openings, lacrimal puncts, to the lacrimal ducts, and the lacrimal sacs and nasolacrimal ducts; the tears moisten and lubricate the conjunctiva and contain protective compounds to inhibit microbes
saliva
The watery, slightly alkaline, mixture of secretions from the salivary and oral mucous glands which lubricates the oral cavity, tounge, and teeth, moistens the chewed food, and contains salivary amylase for initial starch digestion, lingual lipase for initial lipid digestion, and various immune defensive chemicals including IgA antibodies and lysozomes
sebum
The oily semifluid secretion of the sebaceous glands, consisting chiefly of lipids, keratin, and cellular material; with perspiration it moistens and protects the skin
lysozyme
A hydrolytic enzyme occuring in mucous secretions and in the lysosomes of phagocytic cells, capable of destroying the cells walls (peptigoglycan) of bacteria, particularly gram-positive species
hyaluronic acid
A gellike proteoglycan (glycoprotein) that is found in the connective tissue matrix, the synovial fluid of joints, and the vitreous humor of the eyes and acts as a binding, lubricating, and protective agent; it helps limit the spread of microorganisms in the tissue space
transferrins
A group of specific transport proteins for ferric irons, transport proteins found within the beta globulin group of plasma proteins; cells that require iron have surface receptors to bind these specific iron transport proteins to accomplish the transfer of iron into the cell; because iron ions in the plasma are bound to these specific carriers and not simply dissolved in the water of plasma, they are much less accessible for use by invading microorganisms while also require iron and, therfore, those specific iron transport proteins act as a form of resistance to infection
interferons
Any grooup of glycoproteins which are produced by different cell types, including leukocytes, in response to various stimuli, such as exposure to a virus, bacterium, parasite, or other antigen, and which prevent viral replication in newly infected cells and, in some cases, modulate specific cellular functions; others inhibit proliferation of normal and malignant cells, impede multiplication of intracellular parasites, augment the actions of Natural Killer (NK) lymphocytes, or play other locl regulatory roles in immune defenses; several subtypes and subcategories have been defined EX. alpha, beta, and gamma
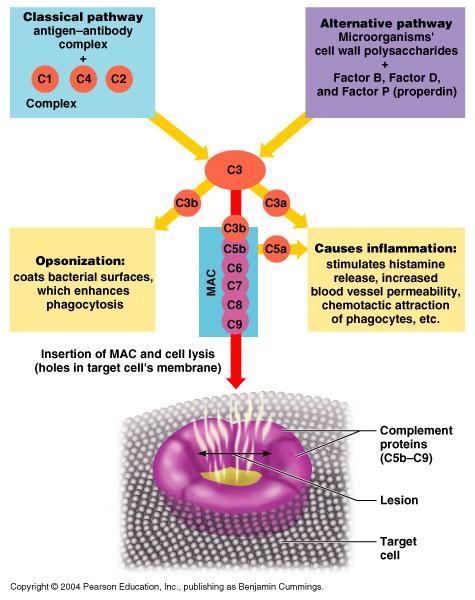
complement system
A system of 12 or more plasma proteins, designated C1, C2, etc., which react in an enzyme cascade to a cell displaying immune complexes or to foreign cell surfaces; these proteins act in various combonations to coat the cell and promote phagocytosis (opsonization), make holes in the cell membrane (cytolysis), attract leukocytes to the area (chemotaxis), and otherwise enhance the inflammatory response
Diagram: Complement response
6 mechanisms of innate/nonspecific resistance to disease and examples of each
1. surface barriers Ex. epidermis and mucous membranes (coughing, vomiting, diarrhea, and urination help cleanse mucous membranes)
2. inflammation Ex.3 stage process: vasodilation and increased vessel permeability, phagocyte migration, and tissue repair
3. phagocytosis Ex.4 stage process: chemotaxis, adherance, e.g.: opsinization, ingestion, digestion and killing. major phagocytes are polymorphonuclear neutrophils and monocytes/macrophages
4. fever Ex. endogenous pyrogens versus exogenous pyrogens
5. antimicrobial proteins Ex. lysozyme, hyaluronic acid, transferrins, interferons, complement system, etc.
6. Natural Killer (NK) lymphocytes Ex. major defenders against viral infection and tumor cells by means other than phagocytosis
List the bodies surface barriers and their chemical secretions which provide nonspecific resistance to disease.
1. skin; sebum's unsaturated fatty acids, NaCl, H+ ions, lysozyme
2. all mucous membranes; lysozymes, mucin protein for mucus
3. gastric lining and urinary tract; many H+ ions for strongly acidic pH
4. vaginal lining; some H+ ions for mildly acidic pH
5. dermis and other dense fibrous connective tissue internal barrier, Ex. fascia and joint and organ capsules; hyaluronic acid
List 4 specific types of cells that functions in nonspecific resistance to disease and their functions.
1. mast cell/"tissue basophil"; releases histamine and other vasoactive regulators to initiate inflammation and phagocyte chemotaxis
2. polymorphonuclear neutrophils; phagocytosis-1st responders
3. monocytes/macrophages; phagocytosis-slow responders
4. Natural Killer ("Null Killer") lymphocytes; destroy virally infected cells and tumor cells by means other than phagocytosis
List 4 categories of anitmicrobial substances/classes of antimicrobial molecules that function in nonspecific resistance to disease and the functions they perform.
1. electrolytes and other small molecules; salts , hydrogen ions and fatty acods create less favorable surface environments for microbial growth on skin and mucous membranes
2. enzymes; lysozyme (protein catalyst) degrades bacterial cell wall material
3. interferons; proteins which a. stimulate internal cellular defenses against viral infection and b. help stimulate and regulate inflammation and other immune defenses
4. complement proteins; plasma proteins which serve as a. opsonins for phagocyte adherence, b. chemotactic signal compounds, and c. lytic agents against cellular antigens
List 3 types of antimicrobial proteins and their functions.
1. enzymes; lysozyme (pprotein catalyst) degrades bacterial cell wall material
2. interferons; proteins which a. stimulate internal cellular defenses against viral infection and b. help stimulate and regulate inflammation and other immune defenses
3. complement proteins; plasma proteins which serve as a. opsonins for phagocyte adherence, b. chemotactic signal compounds, and c. lytic agents against cellular antigens
complement proteins
any of the proteins in the complement system, which a system of 12 or more plasma proteins, designated C1, C2, etc., which react in an enzyme cascade to a cell displaying immune complexes or to a foreign cell surfaces; these proteins act in various combonations to coat the cell and promote phagocytosis (opsinization), make holes in the cell membrane (cytolysis), attract leukocytes to the area (chemotaxis), and otherwise enhance the inflammatory response.
classical pathway
the primary or fundamental biochemical steps which activate the complement system, the complement proteins, which are triggered by the presence of an antigen-antibody complex; usually, the antibody is of the IgG or IgM class; the sequence of complement protein activation is C1, C2, C3, and C4 reacting to produce activated C3 which triggers the completion of the complement cascade
alternate pathway
an additional set of biochemical steps which can amplify the activation of the complement system, the complement proteins, which are triggered by the presence of activated C3 (C3B) on the surface of a cellular antigen (microbial polysaccharides); this additional sequence of complement protein activation is activated C3 which trggers the completion of the complement cascade
opsonization
to make bacteria or other cells more susceptible to phagocytosis (by neutrophils and monocytes/macrophages) by coating their cell membrane surfaces with various proteins, e.g., antibodies or elements of the complement system, e.g., activated C3 (C3B)
chemotactic agent
any chemical, usually a microbial protein or n immune regualtory substance, which induces the directed migration (but not the rate of movement) of leukocytes along its concentration gradient to the area(s) of higher concentration; histamine, various lymphokines, neutrophil products, and several of the activated complement proteins (C3a, C5a) serve this function
cytolysis
the rupture and destruction of cells by the breakdown of their lipid cell membrane/plasmalemmae; various immune molecules have this ability including the membrane attack complex of the complement cascade (activated C5, C6, C7, C8, and C9)
membrane attack complex
the series of protein molecules achieving the completion of the complement cascade using a common set of steps in which C5, C6, C7, C8, and C9 are activated in sequence, by either the classical or alternate pathways, to produce the molecular structure capable of cytolysis--one unit each of activated C5, C6, C7, and C8 (C5b678) will bind from 10-16 molecules of C9 to assemble a hydrophobic pore which crosses the cell membrane and lets ions, water, and other small molecules to pass in either direction, based upon concentration gradients; as a result, the attacked cell, which receives from hundreds to thousands of these pores from activation of the complement cascade, swells, ruptures, and dies
macrophage
any of the large long-lived phagocytic cells derived from monocytes comprising a major component of the diffuse immune system (sometimes called the reticuloendothelial system or, more recently, the mononuclear phagocytic system); these phagocytes from different sites in different organs and tissues have somewhat different properties; in addition to contributing to the killing of microorganisms and tumor cells; they release immune regulatory substances and play a vital role in antigen-presentation leading to the production of antibodies by B lymphocytes and the activation of T lymphocytes
dendritic cell
an activated antigen-presenting cell (monocyte-derived wandering macrophage) responsible for induction of the primary antigen-spevific immune response by their interactions with T and B lymphocytes; these wandering macrophages are usually found in the lymphoid organs such as the thymus, lymp nodes, and percent of mononuclear cells in the peripheral blood
neutriphil/polymorphonuclear leukocyte
the most abundant type of granulocytic white blood cell (60-70% of total WBCs) which is the rapid responder to sites of injury and inflemmation and is highly destructive of microorganisms, especially bacteria; its granules stain poorly and appear pale gray to lavender in typical blood stains; it is capable of phagocytosis and will participate in the removal of damaged tissues even in the absence of infection
monocyte
the largest tyoe of white blood cell (3-*% of total WBCs); a phagocytic agranulocyte, having a single well-defined, often kidney-bean shaped, nucleus and very fine granulation in the cytoplasm; they have long lifespans and when they emigrate into tissues they differentiate into various types of macrophages; they are slow responders to sites of injury and inflammation and are highly destructive of microorganisms
B lymphocyte/ B cell
a functional subclass of lymphocytes, orginating and maturing in the bone marrow; identified by the specific cell surface markers they express; they function in humoral immunity; they make antibodies/immunoglobulins, in a complex process requiring lymphokine stimulation and reaction with specific antigens, and usually the participation of antigen-presenting macrophages and T lymphocytes/Tcells; when actively involved in immune defense they may transform into plasma cells; any one B lymphocytes makes only one specific antibody
plasma cell
any of the antibody-secreting (immunoglobulin-secreting) cells found in lymphoid tissue, and in small numbers in blood, red bone marrow, and other connective tissues; they are derived form B lymphocytes/B cells in a complex process requiring lymphokine stimulation and reaction with a specific antigen, and usually the participation of antigen-presenting macrophages and T lymphocytes/T cells; they are larger than ordinary B lymphocytes, with more cytoplasm, an eccentric nucleus, and sometimes patvh of pale cytoplasm near the nucleus which presents a faintly visible enlarged and active Golgi apparatus where the antibodies are being packaged for storage and secretion
memory B lymphocyte/memory B cell
a functional subclass of B lymphocytes, which are produced after a B lymphocyte clone has become active in specific antibody/immunoglobulin production against a specific antigen; these cells are dormant during the initial response to antigen, but serve as rapid responders to any subsequent exposure of the individual to the specific antigen which was initially involved in their production; their presence insures that subsequent exposures to the specific antigen are met with a more rapid and powerful response; the majority of these cells will be found in the bone marrow and secodary lymphatic organs
T lymphocyte/T cell
a functional subclass of lymphocytes, originating in the bone marrow and maturing in the thymus; identified by the specific cell surface markers they express; (they do not make antibodies/immunoglobulins);they function in cellular immunity; they orchestrate and regulate meny of the immune system's responses; several functional subcategories are recognized including memory T cells, helper T cells, suppressor T cells, cytotoxic T cells, and delayed hypersensitivity T cells; the majority of these cells will be found in the bone marrow and the secondary lymphatic organs
helper T lymphocyte = helper T cell = Th cell
A functional subclass of T lymphocytes (identified by their CD4 markers), which are produced after an interaction with an antigen-presenting cell which has acquired and processed antigens; their activation causes them to release IL-2 and other signal molecules which provide "help," i.e., activate (cause proliferation and differentiation) of other lymphocytes (B, Tc, Ts, Tdh) capable of responding to the same antigen; they play the major role in coordinating antigen-specific immune responses; the majority of these cells will be found in the bone marrow and the secondary lymphatic organs.
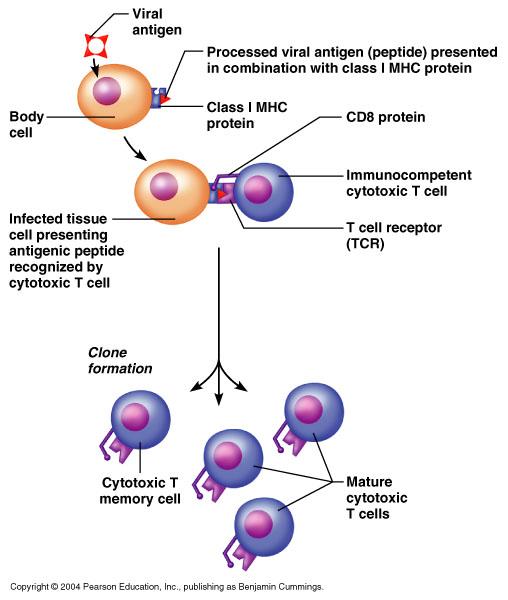
cytotoxic T lymphocyte = cytotoxic T cell = Tc cell
A functional subclass of T lymphocytes (identified by their CD8 markers), which are produced after an interaction with an antigen-presenting cell which has acquired antigens from a virally-infected host cell, a host cell infected by intracellular bacteria (e.g., mycoplasma) or from a tumor cell; their activation also requires IL-2 and other signals from a helper T cell; the activated Tc cells then migrate to the site of the infection or the tumor and secrete a variety of immune molecules, e.g., perforins, lymphotoxins, granzymes, and gamma interferon, which can lyse and kill or at least limit the growth of the targeted cells; these cells also play a major role in rejection of transplanted tissues and organs; the majority of these cells will be found in the bone marrow and the secondary lymphatic organs.
memory T lymphocyte = memory T cell
A functional subclass of T lymphocytes, which are produced after a T lymphocyte clone has become active in some specific cell-mediated response against a specific antigen; these cells are dormant during the initial response to antigen, but serve as rapid responders to any subsequent exposure of the individual to the specific antigen which was initially involved in their production; their presence insures that subsequent exposures to the specific antigen are met with a more rapid and powerful response; the majority of these cells will be found in the bone marrow and the secondary lymphatic organs.
natural killer cell = NK lymphocyte = NK cell
A functional subclass of lymphocytes, which are a resistance defense, i.e., not antigen-specific in their response; they are non-phagocytic cells which migrate to the vicinity of target cells (a host cell infected by a virus or an intracellular bacteria, e.g., mycoplasma, or a tumor cell), bind to the target cell and deliver a variety of potentially lethal chemicals; they may be assisted in identifying their target cells by the presence of antibodies bound to the target cell; these cells also play a major role in rejection of transplanted tissues and organs; the majority of these cells will be found in the bone marrow and the secondary lymphatic organs. [Note: these cells are sometimes referred to as "null" cells because they lack the CD markers which distinguish B and T lymphocytes.]
migration
The act of moving from one place to another; leukocytes are able to move from the red bone marrow, blood, lymph and lymphatic tissues, to any other tissues because they are capable of diapedesis (amoeboid movement); they often follow the concentration gradient of chemotactic signal molecules.
leukocytosis
An abnormally large increase in the number of white blood cells in the blood, often occurring during an acute infection or inflammation and also seen in many leukemias; generally a WBC > 11,000 cells/mm3 in adults, slightly higher in children.
List the types of disease against which cytotoxic T cells are most effective.
viral infections -- cancer (tumor cells)
[Note: they also play a role in graft rejection and are responsible for certain types of allergies]
Explain the differences between a natural killer (NK) lymphocyte and a cytotoxic T-Cell.
The natural killer (NK) lymphocyte is a component of non-antigen-specific defenses; the NK lymphocytes have the capacity to attack a wide variety of "foreign things," usually virally-infected cells and tumor cells, and NK lymphocytes do not require any specific antigen exposure or antigen presentation in order to become active.
The cytotoxic Tc lymphocyte is a component of antigen-specific defenses (within cell-mediated immunity); individual cytotoxic Tc lymphocytes have the capacity to attack a single specific "foreign thing," usually an antigenic determinant which is expressed as a cell membrane surface marker (or other cell membrane protein) on virally-infected cells and tumor cells, and cytotoxic Tc lymphocytes do require specific antigen exposure or antigen presentation in order to become active.
Diagram: The process of clonal selection and differentiation of B Cells when they become activated by exposure to endogenous and exogenous antigen.
1Explain the process of clonal selection and differentiation of B Cells when they become activated by exposure to endogenous and exogenous antigen.
B lymphocytes mature in bone marrow and mature inactive B lymphocytes distributed throughout the lymphatic tissues of the body (and some circulate in the blood stream). In a few instances, such as exposure to gram-negative bacteria, B lymphocytes can act directly in antigen processing and antigen presentation. In most instances, however, macrophages must ingest and process foreign antigens and then patrol the lymphatic tissues in order to identify (by matching of the MHC Class II marker and the antigenic determinant) suitable T and B lymphocytes for antigen presentation. In response to antigen-presentation, specific responsive B lymphocytes will be stimulated by regulatory substances (interleukins, cytokines, etc.). This activation triggers cell division in the specific responsive B lymphocytes producing an increasing population (clone) of identical antigen-specific B lymphocytes. The majority of the members of the clone begin antibody synthesis and secretion, transforming into plasma cells. A minority of the members of the clone remain relatively dormant as potentially responsive antigen-specific memory B lymphocytes. Later in the active response, plasma cells will differentiate into subclones which synthesize and secrete the different antibody classes, e.g., IgM, IgG, IgA, IgE, with all such antibodies still specific to the particular antigenic determinant.
In brief, "clonal selection" is the identification of the subset of B lymphocytes responsive to a specific ant
2Explain the process of clonal selection and differentiation of B Cells when they become activated by exposure to endogenous and exogenous antigen.
In brief, "differentiation" is the development of the subclones of active plasma cells and dormant memory B lymphocytes specific to a particular antigenic determinant.
1Explain the process of clonal selection and differentiation of T Cells when they become activated by exposure to endogenous and exogenous antigen.
T lymphocytes mature in the thymus and mature inactive T lymphocytes distributed throughout the lymphatic tissues of the body (and some circulate in the blood stream). In a few instances, such as exposure to virally-infected cells and tumor cells, T lymphocytes can respond directly to antigen presentation by the altered self cell. In most instances, however, macrophages must ingest and process foreign antigens and then patrol the lymphatic tissues in order to identify (by matching of the MHC Class II marker and the antigenic determinant) suitable T and B lymphocytes for antigen presentation. In response to antigen-presentation, specific responsive T lymphocytes will be stimulated by regulatory substances (interleukins, cytokines, etc.). This activation triggers cell division in the specific responsive T lymphocytes producing an increasing population (clones) of identical antigen-specific T lymphocytes. Some members of the clone differentiate into helper Th and suppressor Ts lymphocytes. A minority of the members of the clone remain relatively dormant as potentially responsive antigen-specific memory T lymphocytes. Other responsive cytotoxic Tc lymphocytes will also develop into active clones.
2Explain the process of clonal selection and differentiation of T Cells when they become activated by exposure to endogenous and exogenous antigen.
In brief, "clonal selection" is the identification of the subset of T lymphocytes responsive to a specific antigenic determinant through encounter with or antigen presentation with a particular antigenic determinant. In brief, "differentiation" is the development of the subclones of active classes of T lymphocytes and dormant memory T lymphocytes specific to a particular antigenic determinant.
Diagram: the process of clonal selection and differentiation of T Cells when they become activated by exposure to endogenous and exogenous antigen.
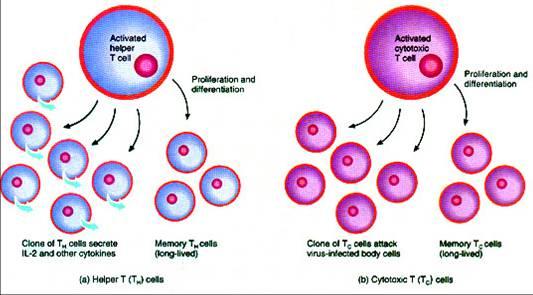
Diagram: the process of clonal selection and differentiation of T Cells when they become activated by exposure to endogenous and exogenous antigen.
inflammation
The body’s first response to any tissue irritation, injury, or infection; a localized protective reaction involving increased capillary blood flow and capillary permeability, triggered by histamine release from tissue mast cells, and characterized by pain, heat, redness, swelling, and sometimes loss of function.
vasodilation
Any increase in the diameter of blood vessels due to the relaxation of the smooth muscle in the vessel's walls; usually regulated by the autonomic NS and certain hormones.
semipermeability
The property of biological membranes which allows passage of some substances through the membrane while restricting the passage of other substances.
fever
rise in the temperature of the body above the normal range; frequently a symptom of infection; stimulated by various chemicals, some of which are present in microorganisms (exogenous pyrogens) while others are internal local hormones released by immune system cells (endogenous pyrogens).
phagocytosis
The process of engulfing and ingesting microorganisms (viruses, bacteria, fungi, protozoans) or other foreign bodies or the cellular debris formed after any injury or tissue necrosis by cells specialized for this function; the phagocytes include neutrophils, eosinophils, monocytes and monocyte-derived macrophages of various sorts; the process involves diapedesis (amoeboid movement), pseudopod formation, and endocytosis to form an internal membrane bound organelle, the phagosome, where the engulfed organisms or substances can be chemically attacked.
adherence
The property of sticking together; a variety of cells, including microbial pathogens and leukocytes and phagocytes have special cell membrane surface components specialized to facilitate their sticking to a surface; opsonins (e.g., antibodies and certain components of the complement system) are molecules which can adhere to cell surfaces to facilitate phagocytosis.
pus
A generally viscous, yellowish-white (to brown or green) opaque creamy fluid formed in infected tissue, consisting of living and dead microorganisims, living and dead white blood cells, cellular debris, and necrotic tissue.
List four accomplishments for the inflammatory response when a tissue is injured.
1. attracts WBCs/leukocytes to the area of injury
2. reduces the spread of harmful microbes or chemicals
3. removes injured or dead cells/tissues, harmful microbes or chemicals
4. increases the blood supply to the injury to provide oxygen and nutrients for WBCs/leukocytes and later for stem cells promoting tissue repair
List the five signs of inflammation.
heat - redness - swelling - pain - (usually some) loss of function
Describe the process of inflammation.
In brief: (1) injury (2) release of chemical regulators (3) histamine stimulates vasodilation and increased capillary permeability which cause increased blood flow to the area (4) chemotaxis of phagocytic leukocytes to the area of injury (5) possible fibrin clot formation (6) heat, redness, swelling, pain and (usually some) loss of function occur in the area (7) debris cleared by phagocytes (8) parenchymal repair or scar tissue formation begins.
Diagram the process of inflammation.
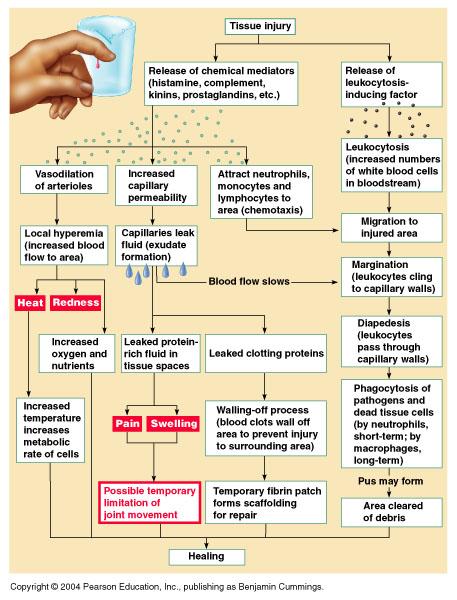
histamine
A physiologically active amine, C5H9N3, released from mast cells as part of the inflammatory process or in certain allergic reactions; it stimulates gastric acid secretion and causes dilation of capillaries, constriction of bronchial smooth muscle, and decreased blood pressure; it is derived from the amino acid histidine
kinins
A group of local hormones and immune regulatory substances with a peptide structure which are released by a variety of cells including lymphocytes which cause dilation of blood vessels and affect capillary permeability; e.g., cytokinin, bradykinin.
prostaglandins
A chemical class of local hormones and immune regulatory substances which are lipids, specifically unsaturated fatty acids derived from arachidonic acid, which are involved in the contraction of smooth muscle, the control of inflammation and body temperature, and many other physiological functions.
Diagram: prostaglandins

leukotrienes
A chemical class of local hormones and immune regulatory substances, related to prostaglandins and derived from arachidonic acid, which are produced by white blood cells in an immune response to antigens, and which contributes to allergic asthma and inflammatory reactions; they have potent actions on many tissues, including the CNS, GI tract, and immune system.
costimulator
Any set of local hormones and immune regulatory substances which cooperate to regulate a particular immune response, e.g., the set of cytokines, interleukins, etc., which are released during the initial maturation of lymphocytes or during the activation (proliferation and differentiation) of B and T lymphocyte clones after antigen-presentation by a macrophage or dendritic cell.
antigen
A substance that, when introduced into the body, stimulates the production of a specific antibody or a specific cell-mediated immune response; antigens include toxins, viruses, bacteria and other microorganisms, foreign blood cells, and the cells of transplanted organs and tissues; at the molecular level, antigens are large and complex molecules, usually proteins, less often carbohydrates or lipids, and only rarely nucleic acids.
antigenic determinant
A region on the surface of an antigen molecule to which a specific antibody or T lymphocyte receptor binds; at the molecular level, they are portions of the larger whole molecule, e.g., a cluster of adjacent amino acids on a protein or a cluster of monosaccharides (simple sugars) on a carbohydrate (polysaccharide).
antigen receptor
A specific molecule or complex of molecules on the surface of B and T lymphocytes which is capable of recognizing and non-covalently binding with a specific antigenic determinant; this binding is one of the necessary signals to begin activation of the lymphocytes; these binding sites are found as the variable regions of antibody molecules (immunoglobulins) and in the MHC Class II surface markers on T lymphocytes.
Diagram: antigen receptor
exogenous antigen
Any antigen which originated or is derived from outside the body; the vast majority of antigens to which the immune system responds because they are "foreign" to the individual, i.e., non-self.
endogenous antigen
Any antigen which originated or is derived from inside the body; this group includes ordinary self-antigens, including some which are unavailable for the lymphocyte-maturation process, e.g., sperm antigens which have not yet been produced at the time; it also includes some antigens which arise internally as a result of a disease process, e.g., the altered membrane lipids to which the reagin antibody forms in certain inflammatory processes including syphilis infection; it also includes many tumor antigens.
tumor antigen
Any antigen which originated or is derived from a cancer cell = tumor cell; while most such antigens are endogenous, a few are considered exogenous because the are derived from oncogenic viruses which have the capacity to transform host cells into tumor cells.
antibody-mediated immunity
The portion of the specific immune response which is due to the activation of B lymphocytes to differentiate and proliferate as clones of antibody-producing plasma cells and B memory cells. [Note: an older term for this process is humoral immunity.]
cell-mediated immunity
The portion of the specific immune response which is due to the activation of T lymphocytes to differentiate and proliferate as clones of helper, suppressor, and cytotoxic T cells and T memory cells. [Note: certain T lymphocytes (helpers and suppressors) also contribute to antibody-mediated immunity by their interactions with B lymphocytes.
List the two "arms" of adaptive (specific) immunity and the cells important in each.
Antibody-Mediated Immunity ("Humoral Immunity"):
1. major cellular defender
2.B lymphocytes which become active Ab-secreting plasma cells
3.additional significant participants
4.macrophages as antigen-presenting cells, helper Th lymphocytes, suppressor Ts lymphocytes and memory B lymphocytes
Cell-Mediated Immunity:
1.major cellular defenders
2.activated cytotoxic Tc cells and helper Th lymphocytes
3.additional significant participants
4.macrophages as antigen-presenting cells, suppressor Ts lymphocytes and various classes of memory T lymphocytes
List the differences between a first immune response and a second = memory response.
First Immune Response:
(1) The first response is the result of the individual's first encounter with the "foreign" antigen.
(2) The first response shows a delay or lag time, typically of 2 to 5 days duration, which represents the time necessary for antigen-processing, antigen-presentation, activation of specific clones of responsive T and B lymphocytes, and time for them to proliferate by repeated mitoses into relatively large populations adequate to deal with the "foreign" antigen.
(3) The strength of the first response is relatively low and somewhat limited. For example, often only IgM class antibodies are elaborated in the first response. At the end of the first response, circulating antibody levels drop back to negligible (though not zero) levels.
Second = Memory Response:
(1) The second = memory response is the result of the individual's second or any subsequent encounter, even decades later, with the same "foreign" antigen.
(2) The second = memory response shows a much reduced delay or lag time, typically from a few hours to a day or two in duration, which represents the time necessary for antigen-processing, antigen-presentation, activation of specific clones of responsive T and B memory lymphocytes, which already exist in relatively large numbers, though in a dormant state.
(3) The strength of the second = memory response is much greater and more elaborate. For example, not only will IgM class antibodies be elaborated, but also generally IgG class anti
Describe the difference between nonspecific resistance to disease and specific resistance to disease, i.e., immunity.
Nonspecific Resistance To Disease: Those body defenses which are already in place and fully functional before the body is exposed to the disease-causing entity. Examples include physical and physiological barriers (e.g., skin and mucous membranes), various chemical defenses (lysozyme, interferons, complement proteins, hyaluronic acid, fibrin, electrolytes, anti-bacterial fatty acids, etc.), and cells (granulocytic leukocytes, monocytes and monocyte-derived macrophages, and natural killer (NK) lymphocytes.
Specific Resistance To Disease, i.e., Immunity: Those body defenses which are already in place and but not fully functional before the body is exposed to the disease-causing entity and specific antigen presentation has occurred to activate the defenses. Examples include B lymphocytes and plasma cells in antibody-mediated immunity and the various classes of T lymphocytes (helper, cytotoxic, suppressor, etc.) in cell-mediated immunity.
Describe the two types of immune response (AMI versus CMI).
Antibody-Mediated Immunity ("Humoral Immunity"): Antibodies to specific antigenic determinants are secreted by plasma cells into the tissue fluid, lymphatic drainage, and blood circulation. These antibodies are then widely distributed through all tissues and some are added to mucous secretions as well. antibodies have a number of defensive functions. First, they adhere to the antigen and this adherence may inactivate the antigen. Secondly, they act as opsonins, encouraging phagocyte adherence and facilitating phagocytosis. Thirdly, certain classes of antibodies, e.g., IgM, can act as triggers to unleash the complement cascade against the antigen. Five classes of immunoglobulins are recognized, IgG, IgM, IgA, Igd, and IgE. Typically Antigen-presentation by a macrophage and Th lymphocyte "help" is required to initiate antibody production.
Cell-Mediated Immunity: Cell-mediated immunity is a more diverse set of specific defensive responses. Each response is provided by a different subset of T lymphocytes. (1) helper Th lymphocytes play a major managerial/regulatory role in the postive feedback control systems which activate B lymphocytes and cytotoxic Tc lymphocytes (usually in cooperation with antigen-presenting macrophages), working to establish complementary clones which are all responsive to the same antigenic determinant. (2) cytotoxic Tc lymphocytes direct non-phagocytic attacks against virally-infected cells, tumor cells, multicellular parasites, and transplant
Describe the difference between "self" and "foreign" antigens.
Self endogenous antigen - Any antigen which originated or is derived from inside the body; this group includes ordinary self-antigens, including some which are unavailable for the lymphocyte-maturation process, e.g., sperm antigens which have not yet been produced at the time; it also includes some antigens which arise internally as a result of a disease process, e.g., the altered membrane lipids to which the reagin antibody forms in certain inflammatory processes including syphilis infection; it also includes many tumor antigens.
Foreign exogenous antigen - Any antigen which originated or is derived from outside the body; the vast majority of antigens to which the immune system responds because they are "foreign" to the individual, i.e., non-self.
Sketch and Label: A diagram of the process of immunity.
immunoglobulin = antibody
Any of a group of large glycoproteins which are secreted by plasma cells in response to a specific antigen and which function in the immune response by binding with specific antigens; there are five classes of immunoglobulins: IgA, IgD, IgE, IgG, and IgM; these proteins carry a net positive charge at body fluid pH and are found in the gamma fraction of the plasma proteins; the molecule is composed of four polypeptide chains — two identical light chains and two identical heavy chains — joined by disulfide bridges; each type of chain has a constant and a variable portion that is different in each type of antibody and is the active portion of the molecule which binds with the specific antigen; the immune functions of different classes of antibodies are determined by properties of the constant regions of the heavy chain; immune functions include binding the antigen, neutralizing toxins, removing substances from circulation in body fluids; agglutinating cellular antigens; and activating complement (blood serum proteins which cause the destruction of invading cells).
antigen presenting cell
Those monocyte-derived wandering and fixed macrophages capable of partially digesting foreign matter and placing derived antigenic determinants on their cell surfaces in conjunction with MHC Class II surface markers in order to expose responsive B and T lymphocytes in order to activate them.
antigen processing
The part of the process of antigen presentation in which the macrophage has engulfed the foreign material, partially degraded it by enzymatic attack in the phagolysosome, and passed the mix of antigenic determinants to various MHC Class II markers which bind them and transport them to the cell surface of the macrophage so that it can expose responsive B and T lymphocytes in order to activate them.
antigen binding site (on antibody)
The subregion of the variable portion of the antibody molecule which is capable of specific noncovalent (reversible) binding to the antigenic determinant as a result of attraction and fit between the antigen binding site and a portion of he antigenic determinant; recognition and binding is due to compatible size, shape and surface charge characteristics.
antibody heavy chain
The larger longer pair of identical polypeptide chains which are covalently linked to each other and to the corresponding light chains by disulfide bridges; each heavy chain consists of three constant portions and a variable portion; the variable portion, along with the variable portion of the corresponding light chain form the antigen binding site which binds a specific antigenic determinant; components of the constant portions determine specific immune functions. e.g., complement fixation, secretion to mucous membranes, opsonization, phagocytosis, and are used in separating antibodies into five classes: IgA, IgD, IgE, IgG, and IgM.
antibody light chain
The smaller shorter pair of identical polypeptide chains which are covalently linked to the corresponding heavy chains by disulfide bridges; each light chain consists of a constant portion and a variable portion; the variable portion, along with the variable portion of the corresponding heavy chain form the antigen binding site which binds a specific antigenic determinant.
antibody constant regions
Those portions of the light and heavy chains of immunoglobulin molecules which are responsible for giving shape to the molecule in regions other than the antigen binding site; these portions of the heavy chain are responsible for determining specific immune functions and are used in separating antibodies into five classes: IgA, IgD, IgE, IgG, and IgM.
antibody variable regions
Those portions of the light and heavy chains of immunoglobulin molecules which are responsible for giving shape, surface charge, and functional (bonding) properties to the antibody molecule in the antigen binding site.
primary (immune) response
The initial response of the immune system to a first encounter with a foreign antigen in which there is a delay of several days (from one to three weeks) before any significant immune defenses are evident; the delay is due to the time required for macrophages to encounter, phagocytize, and process the foreign antigen, followed by the time required for the macrophages to locate suitable antigen-specific T and B lymphocytes for antigen-presentation, and followed by the time required for lymphocytes to become activated and to proliferate into functional clones capable of generating specific responses, e.g., antibody production, against the foreign antigen.
secondary (immune) response
The rapid response of the immune system to a second or subsequent encounter with a foreign antigen in which there is little delay (a few minutes to several hours to a few days before any significant immune defenses are evident; the lack of delay is due to the availability of T and B memory lymphocytes which can respond almost immediately to antigen-presenting macrophages, and the ability of these stimulated memory lymphocytes to become activated and to proliferate into functional clones capable of generating specific responses, e.g., antibody production, against the foreign antigen.
1/5 Sketch and label: The process of antigen processing and display. How does this process differ for endogenous versus exogenous antigens?

Endogenous antigen (from virally-infected cells or tumor cells) is processed by the self cell in conjunction with the participation of MHC Class I (HLA or tissue typing) self-cell surface markers. This combination of the MHC Class I marker and the "foreign" antigen helps the immune cells "understand" that a self cell will need to be attacked. A macrophage may not even be involved.
2/5 Sketch and label: The process of antigen processing and display. How does this process differ for endogenous versus exogenous antigens?
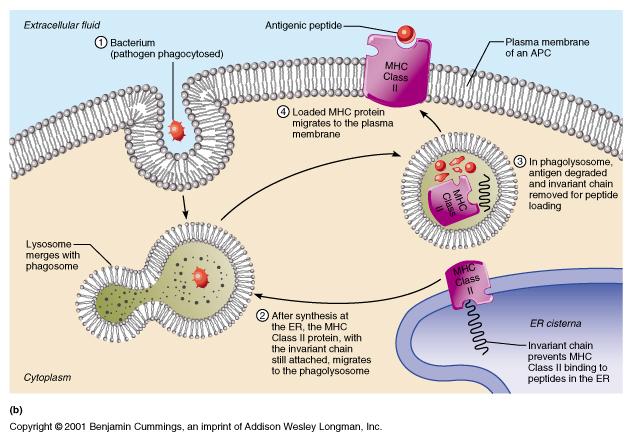
Exogenous antigen (foreign antigens, e.g., viruses, microorganisms, venoms, toxins, or drugs, etc.) is processed by a macrophage in conjunction with the participation of MHC Class II self-cell surface markers. MHC Class II markers, which have a limited distribution on macrophages, lymphocytes, and a few other cells, helps the specific immune cells (macrophages, B lymphocytes and T lymphocytes) recognize and cooperate with one another in developing specific defenses against the foreign antigen.
3/5 Sketch and label: The process of antigen processing and display. How does this process differ for endogenous versus exogenous antigens?
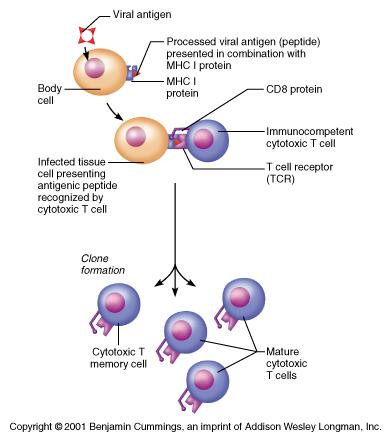
Once processed, the endogenous antigen is displayed on the self cell surface in conjunction with the MCH Class I marker in a complex. That complex is recognized by various immune cells, most often by antigen-specific cytotoxic Tc lymphocytes which will then release various immune defensive compounds in an effort to destroy the virally-infected cells or tumor cells.
4/5 Sketch and label: The process of antigen processing and display. How does this process differ for endogenous versus exogenous antigens?
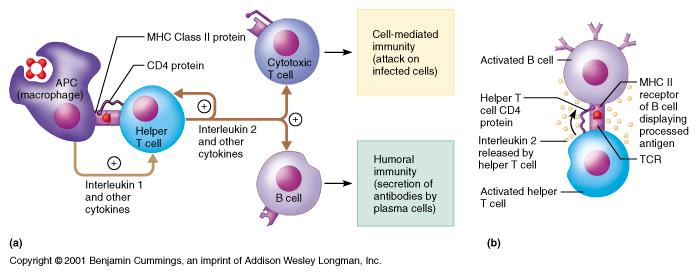
Once processed, the exogenous antigen is displayed on the macrophage surface in conjunction with the MCH Class II marker in a complex. That complex is recognized by various immune cells, most often by antigen-specific helper Th lymphocytes and B lymphocytes. The helper Th lymphocytes will then release various immune regulatory compounds (e.g., interleukins) which will serve to activate and cause proliferation of the antigen-specific cytotoxic Tc lymphocytes and B lymphocytes. The activated cytotoxic Tc lymphocytes will then seek out the foreign cellular antigen (e.g., viruses, microorganisms, parasites) and attempt to kill them. At the same time, the activated B lymphocytes become plasma cells which secrete specific antibodies which will bind with the foreign antigen (e.g., viruses, microorganisms, venoms, toxins, or drugs, etc.) and trigger the variety of antibody-mediated immune defenses against the foreign antigen.
5/5 Sketch and label: The process of antigen processing and display. How does this process differ for endogenous versus exogenous antigens?
How does this process differ for endogenous versus exogenous antigens? The two key differences are (1) endogenous antigen processing does not require the involvement of a macrophage while exogenous antigen processing does require a macrophage; and (2) endogenous antigen processing requires the recognition of specific MHC Class I (HLA or tissue typing) self-cell surface markers which are widely distributed (on most cell types other than erythrocytes) while exogenous antigen processing requires the recognition of specific MHC Class II cell surface markers which are narrowly distributed and found primarily on macrophages and lymphocytes.
anergy
A depression or lack of normal immunological function, either generalized or antigen-specific; typically the failure to react to an injected allergen or antigen, e.g., failure to respond to the tuberculin skin test by person with a prior history of TB.
clone
The propagation of genetically identical cells by mitosis and the resulting assemblage of the identical cells; in the immune system, the proliferation of stimulated antigen-specific B and T lymphocytes following exposure to the antigen into functional clones with various defensive functions.
self-recognition
The ability of the immune system to recognize the set of molecules and cells within the individual as "self," i.e., belonging to the body and, therefore, not being foreign; this immune function is centered in the maturation process of B and T lymphocytes in which any anti-self lymphocytes experience negative selection and are either destroyed = deleted or regulated into inactivity.
immunological tolerance
The failure of the immune system to respond to an antigen with any specific responses; it is not simply a failure to recognize an antigen as foreign, but is rather a particular form of active response in which immune defenses are not activated; it includes the "natural" failure to respond to self antigens and the "induced" tolerance to external foreign antigens which may be created by manipulating the immune system, e.g., with repeated allergy injections, or by the application of medications, e.g., the suppression of transplant rejection with corticosteroids and other drugs.
selection
In biological systems, a natural or artificial process which favors or induces survival and perpetuation of one kind of cell or organism over others that die or fail to produce offspring.
positive selection
In the immune system, those situations in which white blood cells are encouraged, i.e., regulated, to differentiate and proliferate; typically, it is the generation of active clones of B and T lymphocytes in response to antigen-presentation and stimulation by various lymphokines during active immune responses (memory lymphocytes clones will also be produced).
negative selection
In the immune system, those situations in which white blood cells are discouraged, i.e., regulated not to differentiate and proliferate; it includes the situation during the maturation process of B and T lymphocytes in which any anti-self lymphocytes are either destroyed = deleted or regulated into inactivity; it also includes the suppressive or negative feedback regulation which decreases the further proliferation and actions of active clones of B and T lymphocytes in response to certain lymphokines during the closing or ending phase of any active immune response when the body is returning to homeostasis.
deletion
In the immune system, those situations in which any anti-self B and T lymphocytes (clones) are destroyed during the maturation process in response to certain lymphokines and other local regulatory substances.
major histocompatibility complex (MHC) antigens
A group of widely distributed cell surface markers (membrane proteins), the histocompatibility antigens*, coded for by the genes of the Major Histocompatability Complex (MHC) (in humans, these genetic blueprints comprise the diverse set of alleles occurring at four loci on the short arm of chromosome 6); these cell surface markers (HLA* antigens) are subdivided into two functional classes, I & II.; these cell surface markers (antigens) permit leukocytes to recognize and distinguish self from non-self tissue cells (Class I) and to recognize and cooperate with other leukocytes and immune defense cells (Class II). [*Note: the histocompatibility antigens are also referred to as the human leukocyte antigens or HLA markers.]
MHC Class I antigens = MHC Class I surface markers
A group of widely distributed cell surface markers, the histocompatibility antigens*, coded for by the genes of the Major Histocompatability Complex (MHC) (in humans, these genetic blueprints comprise the diverse set of alleles occurring at four loci on the short arm of chromosome 6); these cell surface markers (antigens) are located on all nucleated body tissue cells; these cell surface markers (antigens) permit leukocytes to recognize and distinguish self from non-self tissue cells. [*Note: the histocompatibility antigens are also referred to as the human leukocyte antigens or HLA markers.]
MHC Class II antigens = MHC Class II surface markers
A group of widely distributed cell surface markers, coded for by the genes of the Major Histocompatability Complex (MHC) (in humans, these genetic blueprints comprise the diverse set of alleles occurring at several loci on the short arm of chromosome 6); these cell surface markers (antigens) are located on a limited number of immune cells, e.g., macrophages and T and B lymphocytes; these cell surface markers (antigens) permit these immune cells, e.g. macrophages and T and B lymphocytes, to recognize and cooperate with each other in antigen-presentation and in the generation of various antigen-specific immune defenses.
immunosurveillance = immunological surveillance
A normal continual monitoring process of the immune system which detects and destroys neoplastic = cancer cells and which tends to break down in immunosuppressed and immunocompromised individuals; it is one of the main functions of the NK = natural killer lymphocytes but also involves some macrophages and T and B lymphocytes.
allergy = hypersensitivty
An abnormally active and inappropriate immune response to certain common, ordinary, non-threatening antigens {"allergens"}(e.g., various chemicals, drugs, pollens, molds, foods, or microorganisms); reactions vary greatly in intensity; common symptoms may include sneezing, itching, and skin rashes; some allergens stimulate antibody-mediated responses while others stimulate cell-mediated responses.
Human Immunodeficiency Virus (HIV)
An RNA retrovirus which causes the generally fatal chronic illness, Acquired Immunodeficiency Syndrome (AIDS), by infecting helper T lymphocytes of the immune system; the virus attaches to the CD4 cell surface marker to penetrate the host cell and then uses the enzyme reverse transcriptase to introduce a DNA copy of its viral genome into the host cell's DNA, leading to a slow but steady reproduction of the virus inside the infected cell; the most common serotype, HIV-1, is distributed worldwide, while HIV-2 is primarily confined to West Africa.
Diagram of HIV
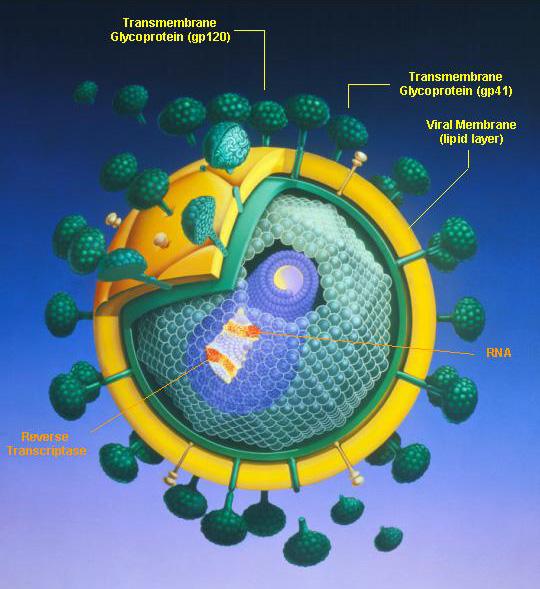
Acquired Immunodeficiency Syndrome (AIDS)
A severe immunological disorder caused by the RNA retrovirus HIV, characterized by increased susceptibility to opportunistic infections, e.g., Pneumocystis carinii pneumonia, TB and candidiasis, to certain cancers, especially Kaposi's sarcoma, and to neurological disorders; transmission is chiefly through blood or blood products which enter the body's bloodstream, esp. by sexual contact or contaminated hypodermic needles; other body fluids may also carry the virus.
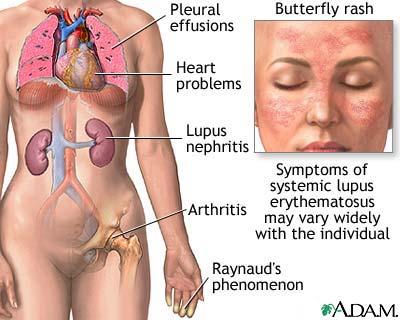
autoimmune disease
Any of a large group of diseases characterized by abnormal functioning of the immune system which causes it to produce specific anti-self antibodies or cell-mediated responses against one's own tissues; diseases of the immune system are currently treated by a variety of nonspecific immunosuppressive drugs and corticosteroids.
Systemic Lupus Erythematosus (SLE)
A chronic autoimmune inflammatory disease of the connective tissues, occurring mainly among middle-aged women, chiefly characterized by skin eruptions, joint pain, arthritis, fever, weakness, weight loss, anemia, enlargement of the spleen, and a characteristic butterfly-shaped skin rash on the face, recurrent pleurisy, and heart and kidney disease.
Diagram of SLE
Hodgkins disease
A malignant, progressive, sometimes fatal lymphoma of unknown cause, marked by progressive (but painless) enlargement of the lymph nodes, followed by enlargement of the spleen, and liver; bone marrow transplantation may be useful for selected patients who have relapsed following treatment with radiation and chemotherapy.
List seven autoimmune diseases and the organ(s) or tissue(s) attacked in each disease.
1. MS = Multiple Sclerosis: myelinated fiber tracts (white matter) of the brain and spinal cord (CNS) leading to a wide variety of neurological symptoms
2. Myasthenia Gravis: neuromuscular junction of skeletal muscle leading to progressive muscular weakness
3. Grave's Disease: TSH (thyroid stimulating hormone) receptor of thyroid follicular cells leading to hyperthyroidism
4. Type I ("juvenile") diabetes mellitus: pancreatic islet beta cells leading to insulin deficiency
5. SLE = Systemic Lupus Erythematosus: general attach on connective tissues; organ systems showing characteristic involvement and lesions include the dermis of the skin, the kidneys, the heart, and the lungs
6. Glomerulonephritis: capillary basement membrane of the nephrons of the kidney leading to progressive impairment of renal function
7. Rheumatoid Arthritis: self-antigen is patient's normal IgG class antibodies; the autoanti-IgG-antibody-IgG Ab-Ag complexes become deposited in various tissues including the joints and the glomerlular basement membrane of the nephrons of the kidney leading to chronic inflammatory changes and scar tissue formation
active immunity
Any immune response which develops as a result of an individual's exposure to a specific antigen in which the response is the product of the individual's own immune system becoming activated, generally through the generation of clones of antigen-specific B and T lymphocytes.
passive immunity
Any immune response which develops as a result of an individual receiving immune molecules (maternal antibodies crossing the placenta in utero or via colostrum or milk from the mammary glands or intravenous injections of gamma globulin) or immune cells (leukocyte transfusions or bone marrow transplants) transferred from another individual (who had had exposure to a specific antigen) and, therefore, the response is not the product of the individual's own immune system becoming activated.
natural immunity
Any immune response which develops as a result of an individual's exposure to a specific antigen encountered in the external environment without the intervention of medical therapy or practice.
artificial immunity
Any immune response which develops as a result of an individual's exposure to a specific antigen encountered due to the intervention of medical therapy or practice.
Natural active immunity
Natural active immunity occurs when a person develops immunity as a result of exposure to disease organisms or foreign toxins, venoms, allergens or drugs; generally, on initial exposure, the person develops the disease or has an initial negative response to the toxin or venom.
Passive active immunity
Passive active immunity occurs when a mother transmits her own antibodies to her fetus across the placenta or to her infant in her milk; such immunity is transient and relatively short-lived.
Artificial active immunity
Artificial active immunity occurs when a person develops immunity as a result of exposure to a vaccine designed to protect against disease organisms or foreign toxins, venoms, or allergens; generally, on initial exposure, the person does not develop symptoms of the disease or has only minimal response to the toxin or venom.
Passive artifticial immunity
Passive artifticial immunity occurs when an individual receives antibodies (injections of gamma globulin) or immune cells (leukocyte transfusions or bone marrow transplants) from another individual (who had had exposure to a specific antigen); such immunity may be transient and relatively short-lived (gamma globulin injections or leukocyte transfusions) or it may be permanent (bone marrow transplants).
List the difference between active and passive immunity.
Active Immunity: Any immune response which develops as a result of an individual's exposure to a specific antigen in which the response is the product of the individual's own immune system becoming activated, generally through the generation of clones of antigen-specific B and T lymphocytes.
Passive Immunity: Any immune response which develops as a result of an individual receiving immune molecules (injections of gamma globulin) or immune cells (leukocyte transfusions or bone marrow transplants) transferred from another individual (who had had exposure to a specific antigen) and, therefore, the response is not the product of the individual's own immune system becoming activated
List the difference between natural and artificial immunity.
Natural Immunity: Any immune response which develops as a result of an individual's exposure to a specific antigen encountered in the external environment without the intervention of medical therapy or practice.
Artificial Immunity: Any immune response which develops as a result of an individual's exposure to a specific antigen encountered due to the intervention of medical therapy or practice.
autograft
A tissue or organ grafted into a new position in or on the body of the same individual; the most desirable source for skin grafting in burns, if possible, because no rejection will occur.
isograft
A graft of tissue which is obtained from a donor genetically identical to the recipient for which no rejection will occur; only identical siblings (twins, triplets, etc.) can provide such tissue, a desirable source for transplantation, because no rejection will occur..
allograft = homograft
A graft of tissue which is obtained from a donor of the same species as, but with a different genetic make-up from, the recipient, as a tissue transplant between two humans (relatives or not); rejection of the tissue is likely unless immunosuppressive therapy is provided to the recipient.
xenograft = heterograft
A graft of tissue which is obtained from a donor of a different species from the recipient, e.g., when animal skin is used as a temporary transplant in cases of severe burns, or when pig heart valves are transplanted into humans; rapid rejection of the tissue is very likely unless potent immunosuppressive therapy is provided to the recipient.