Which of the following respiratory structures is more commonly known as the "throat"?
a. Trachea
b. Pharynx
c. Esophagus
d. Larynx
b. Pharynx
What is the amount of air that can be exhaled with the greatest possible exhalation after the deepest inhalation called?
a. expiratory reserve volume
b. vital capacity
c. inspiratory reserve volume
d. tidal volume
b. vital capacity
What is the most powerful respiratory stimulant in a healthy person?
a. blood oxygen level
b. oxygen needs of cells
c. blood carbon dioxide level
d. blood pH
c. blood carbon dioxide level
Which of the following are the two main functions of the larynx.
a. To provide a patent airway; to act as a switching mechanism to route air and food into the proper channels.
b. Voice production; to provide a patent airway
c. Voice production; to act as a switching mechanism to route air and food into the proper channels.
d. Voice production; stimulation of the "cough" reflex
a. To provide a patent airway; to act as a switching mechanism to route air and food into the proper channels.
The _________________ is also known as the "guardian of the airways".
a. vestibular folds
b. epiglottis
c. larynx
d. glottis
b. epiglottis
The smallest subdivisions of the lung visible with the naked eye are the _____________, which appear to be connected by black carbon in smokers.
a. lobes
b. pleura
c. lobules
d. pulmonary hila
c. lobules
What is the amount of air that can be exhaled with the greatest possible exhalation after the deepest inhalation called?
a. vital capacity
b. tidal volume
c. inspiratory reserve volume
d. expiratory reserve volume
a. vital capacity
The descending limb of the loop of Henle is permeable to both solutes and water. T/F
False
Chemicals that enhance urinary output are called _______________.
a. countercurrent multipliers
b. reabsorbers
c. diuretics
d. countercurrent exchangers
c. diuretics
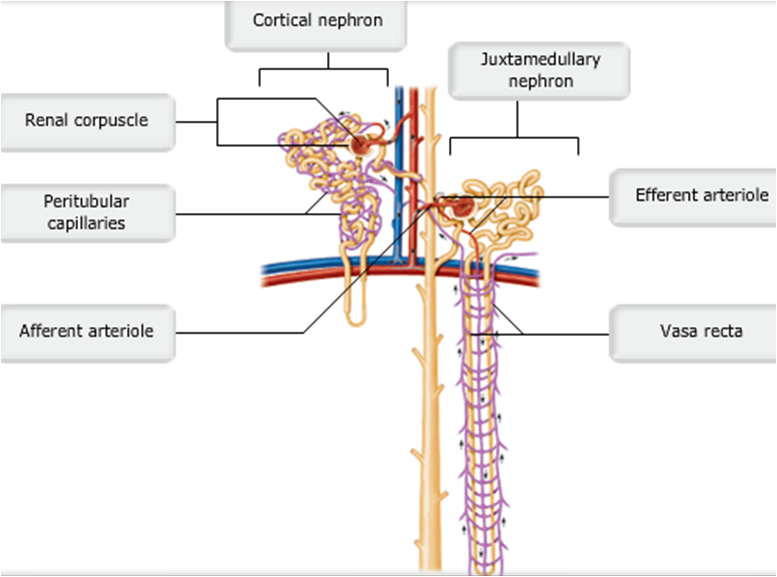
Cortical and Juxtamedullary Nephrons
pic
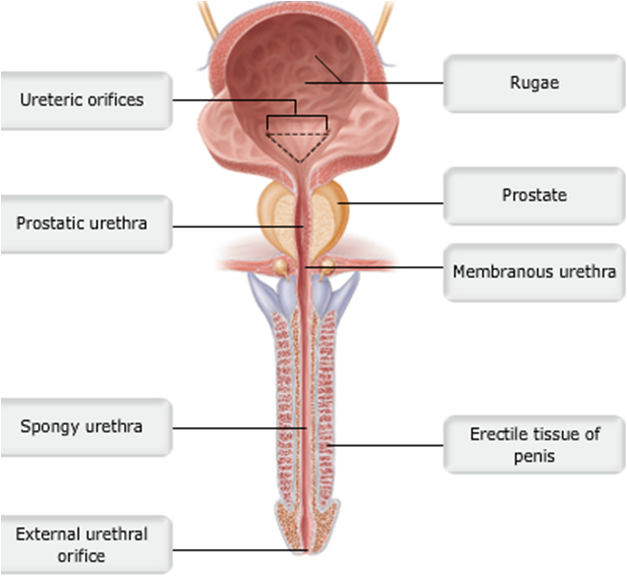
Male Urethra
pic
Which of the following is not one of the things that must happen for micturition to occur?
a. The extrusor muscle must relax
b. The internal urethral sphincter must open
c. The external urethral sphincter must open
d. The detrusor muscle must contract
a. The extrusor muscle must relax
...
Most solutes that are reabsorbed in the proximal convoluted tubule use which of the following pathways?
a. transcellular
b. paracellular
a. transcellular
**Yes, most substances are reabsorbed first through the luminal and then through the basolateral membranes of the proximal convoluted tubule.
During reabsorption of water in the proximal convoluted tubule, what causes water to diffuse from the lumen into the interstitial space?
a. active transport of water
b. an increase in the osmolarity of the interstitium
c. a decrease in the osmolarity of the interstitium
b. an increase in the osmolarity of the interstitium
**Yes, the increase in osmolarity causes the water to move into the interstitium.
The decreased intracellular concentration of sodium in tubular cells during active transport is caused by which of the following mechanisms?
a. sodium-glucose cotransporter
b. the sodium-potassium ATPase pump in the luminal membrane
c. the sodium-potassium ATPase pump in the basolateral membrane
d. passive sodium channels
c. the sodium-potassium ATPase pump in the basolateral membrane
**this pump moves sodium out of the cell into the interstitium, thus decreasing intracellular sodium.
The active transport of which ion out of proximal convoluted tubule cells causes the reabsorption of both water and solutes?
a. sodium
b. potassium
c. chloride
a. sodium
**the active transport of sodium out of the cell, across the basolateral membrane into the interstitium, provides the driving force for reabsorption of both water and solutes.
Which of the following transporters in the luminal membrane results in secretion?
a. glucose carrier transporter
b. Na+-glucose cotransporter
c. potassium ion channel
d. Na+-H+ countertransport
d. Na+-H+ countertransport
**because this is a countertransporter, Na+ is transported into the cell and H+ is transported out of the cell into the lumen.
What is the limiting factor for the reabsorption of most actively transported solutes in the proximal tubule?
a. number of transport carriers in the luminal membrane
b. number of transport carriers in the basolateral membrane
c. number of sodium-potassium ATPase pumps in the basolateral membrane
a. number of transport carriers in the luminal membrane
**the number of carriers is the rate-limiting factor. For example, in Diabetes Mellitus, plasma glucose levels are very high, and the sodium-glucose transporter cannot transport (reabsorb) all the glucose passing through the proximal tubule. Glucose is therefore found in the urine.
Which of the following substances is not normally found in filtrate?
a. blood cells and large particles
b. nitrogenous waste particles, such as urea
c. water and small solutes
d. ions, such as sodium and potassium
a. blood cells and large particles
**both blood cells and large particles, such as proteins, are not allowed to filter through a healthy glomerular membrane.
What is the primary driving force (pressure) that produces glomerular filtration?
a. colloid osmotic pressure of blood
b. hydrostatic pressure of blood (blood pressure)
c. gravity
b. hydrostatic pressure of blood (blood pressure)
**the hydrostatic pressure of blood forces fluid out of the glomerular capillaries.
Which of the following would only be found in the glomerular filtrate if the glomerular membrane were damaged?
a. creatinine
b. chloride
c. protein
d. glucose
c. protein
**large proteins are not normally filtered by a healthy glomerular membrane.
If the osmotic pressure in the glomerular capillaries increased from 28 mm Hg to 35 mm Hg, would net filtration increase or decrease?
a. net filtration would not be altered
b. net filtration would increase
c. net filtration would decrease
c. net filtration would decrease
**because osmotic pressure opposes filtration, increasing osmotic pressure would decrease net filtration.
Calculate the net filtration pressure if capillary hydrostatic pressure is 60 mm Hg, capillary osmotic pressure is 25 mm Hg, and capsular hydrostatic pressure is 10 mm Hg.
a. 60 mm Hg
b. 35 mm Hg
c. 50 mm Hg
d. 25 mm Hg
d. 25 mm Hg
**60 – (25 + 10) = 25 mm Hg. The two pressures that oppose filtration must be subtracted from the force favoring filtration.
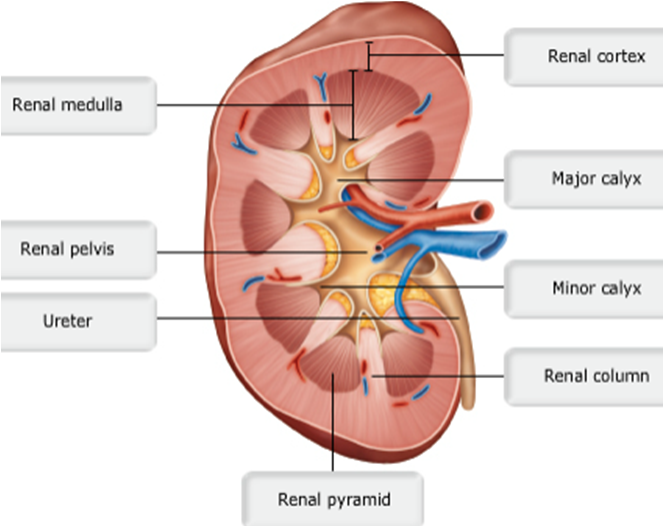
The _____________ collect(s) urine, which drains continuously from the papillae; the urine is then emptied into the ______________.
a. renal pyramids; renal pelvis
b. renal pelvis; calyces
c. renal pyramids; calyces
d. calyces; renal pelvis
d. calyces; renal pelvis
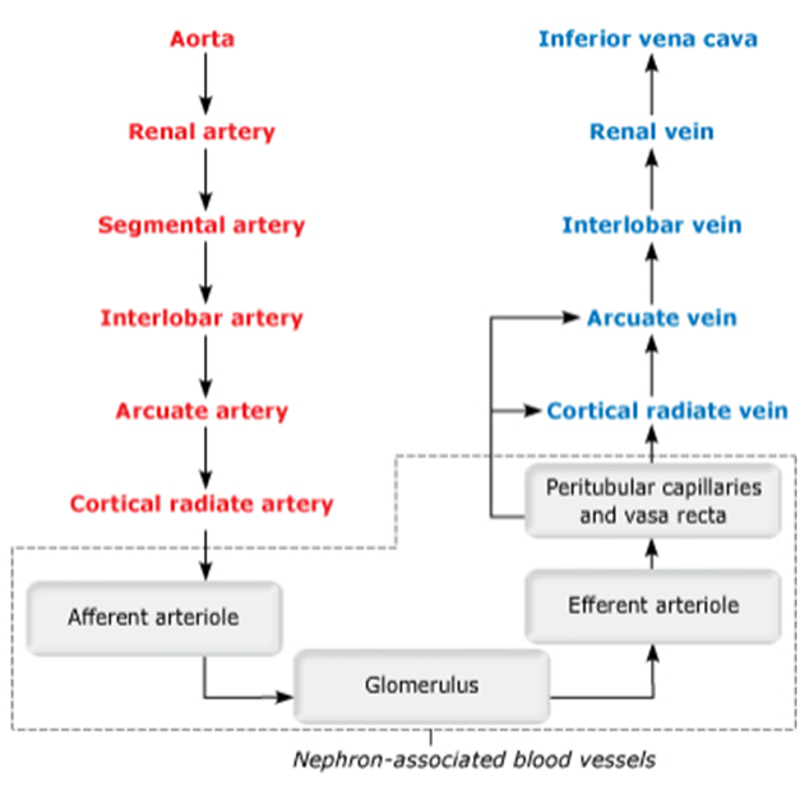
Blood flow path through renal bv
...
Approximately 80% of the energy used for active transport is devoted to the reabsorption of _______________.
a. water
b. sodium
c. glucose
d. potassium
b. sodium
What is the largest component of urine by weight, other than water?
a. creatine
b. phosphates
c. urea
d. salt
c. urea
Despite the fact that the kidney's intrinsic controls work to maintain a constant GFR, in some situations the body's extrinsic controls will work to override these intrinsic controls in order to maintain systemic blood pressure. T/F
True
In which part of the kidney is reabsorption (1) dependent upon the body's needs at the time, and (2) regulated by hormones?
a. Distal convoluted tubule
b. Ascending limb of the loop of Henle
c. Descending limb of the loop of Henle
d. Proximal convoluted tubule
a. Distal convoluted tubule
Which of the following is not a function of the kidneys?
a. Maintaining the proper balance between water and salts and between acids and bases
b. Producing the hormones melanin and oxytocin
c. Gluconeogenesis during prolonged fasting
d. Metabolizing vitamin D to its active form
b. Producing the hormones melanin and oxytocin
...
Which of the following best describes glomerular filtration rate (GFR)?
a. the volume of urine leaving the kidneys per minute
b. the volume of blood flowing through the glomerular capillaries per minute
c. the volume of filtrate created at the glomerulus per liter of blood flowing through the glomerular capillaries
d. the volume of filtrate created by the kidneys per minute
d. the volume of filtrate created by the kidneys per minute
**
Fluid and small solutes that leave the glomerulus are collectively termed filtrate. Glomerular filtration is driven by glomerular hydrostatic pressure (HPg) and produces ~125 ml of filtrate per minute.
GFR regulation mechanisms primarily affect which of the following?
a. blood osmotic pressure (OPg)
b. capsular hydrostatic pressure (HPc)
c. glomerular hydrostatic pressure (HPg)
d. capsular osmotic pressure (OPc)
SubmitHintsMy AnswersGive UpReview Part
Correct
c. glomerular hydrostatic pressure (HPg)
**Much like other capillaries in the body, hydrostatic pressure within the glomerular capillaries produces net outward movement of fluid. Unique to glomerular capillaries, HPg is consistently higher than other capillaries (~55 mm Hg), which ensures the one-way movement of fluid and solutes out of the glomerulus under normal conditions.
Which of the following are mechanisms of intrinsic control of glomerular filtration (renal autoregulation)?
a. myogenic mechanism and sympathetic nervous system control
b. sympathetic nervous system control and the renin-angiotensin mechanism
c. myogenic mechanism and tubuloglomerular feedback
d. tubuloglomerular feedback and the renin-angiotensin mechanism
c. myogenic mechanism and tubuloglomerular feedback
**Both of these mechanisms occur strictly within kidney (i.e., intrinsic controls). The myogenic mechanism is mediated by smooth muscle within the afferent arteriole. In contrast, tubuloglomerular feedback is mediated by macula densa cells of the juxtaglomerular apparatus (JGA).
Macula densa cells of the juxtaglomerular apparatus (JGA) regulate GFR through which intrinsic mechanism?
a. myogenic mechanism
b. renin-angiotensin mechanism
c. tubuloglomerular feedback
d. sympathetic nervous system control
c. tubuloglomerular feedback
**The JGA is a region of the nephron where the afferent arteriole and its associated tubule are closely apposed. This anatomical arrangement allows macula densa cells to adjust GFR according to the NaCl concentration in filtrate. This is called tubuloglomerular feedback because it allows the contents of the tubules (tubulo-) to affect the glomerular filtration rate.
The myogenic mechanism of renal autoregulation primarily involves smooth muscle in which blood vessels?
a. glomeruli
b. efferent arterioles
c. systemic arterioles
d. afferent arterioles
d. afferent arterioles
**By regulating afferent arteriole diameter, the myogenic mechanism affects HPg and therefore GFR. Under normal physiological conditions, this intrinsic control works to maintain GFR despite moderate changes in systemic blood pressure
What does a high concentration of NaCl in the renal tubule at the juxtaglomerular apparatus (JGA) most likely indicate?
a. excessive NaCl reabsorption due to high GFR
b. insufficient NaCl reabsorption due to high GFR
c. excessive NaCl reabsorption due to low GFR
d. insufficient NaCl reabsorption due to low GFR
b. insufficient NaCl reabsorption due to high GFR
**After glomerular filtration, NaCl is actively reabsorbed at many locations along the renal tubule. If the filtrate is moving through the tubule quickly, less reabsorption is possible, so more NaCl gets left behind. This means that at the JGA, the NaCl concentration within the filtrate will be high.
Through the tubuloglomerular feedback mechanism, how would an increase in filtrate NaCl concentration affect afferent arteriole diameter?
a. Afferent arteriole diameter would increase.
b. Afferent arteriole diameter would decrease.
c. Afferent arteriole diameter would stay about the same.
b. Afferent arteriole diameter would decrease.
**High NaCl concentration in the filtrate at the JGA indicates that GFR is too high. By decreasing the diameter of the arteriole delivering blood to the glomerulus, HPg is decreased, resulting in lower GFR.
Granular cells of the juxtaglomerular apparatus (JGA) regulate GFR through which mechanism?
a. renin-angiotensin mechanism
b. sympathetic nervous system controls
c. tubuloglomerular feedback mechanism
c. myogenic mechanism
a. renin-angiotensin mechanism
**When systemic blood pressure decreases, granular cells release renin which ultimately causes the formation of angiotensin II. Angiotensin II causes widespread vasoconstriction of systemic arterioles and the increase of blood volume due to aldosterone release.
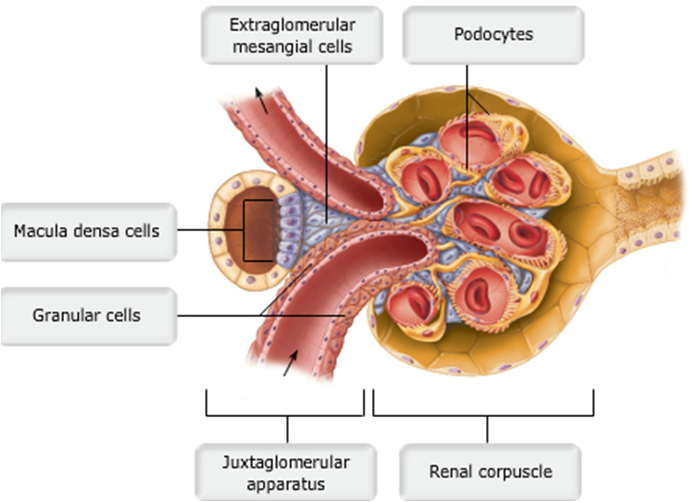
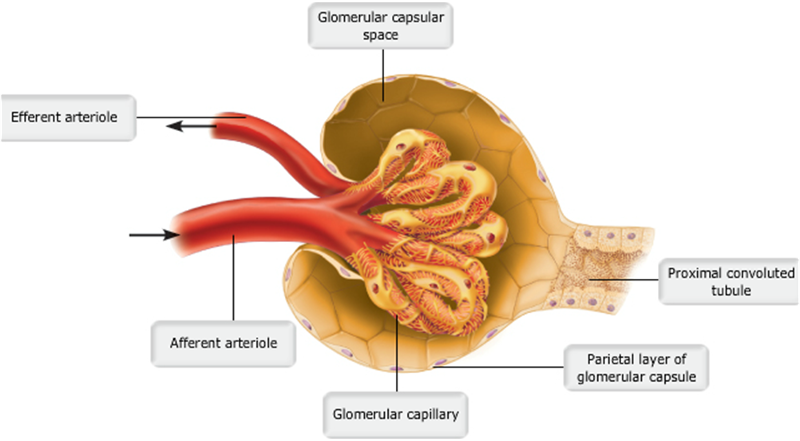
Juxtaglomerular complex of a nephron
...
The _______ keeps the urethra closed when urine is not being passed from the bladder, and prevents leaking between voiding.
a. internal urethral sphincter
b. prostatic urethra
c. external urethral sphincter
d. external urethral orifice
a. internal urethral sphincter
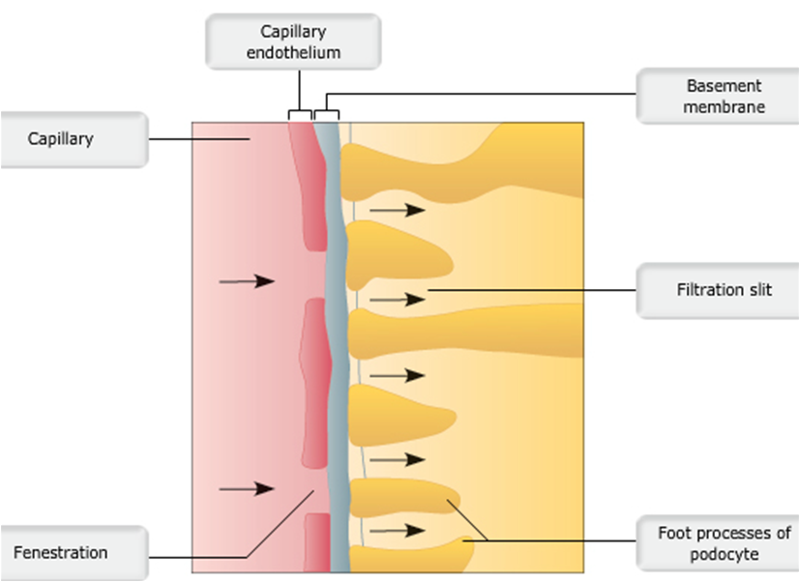
Layers of filtration membrane
...
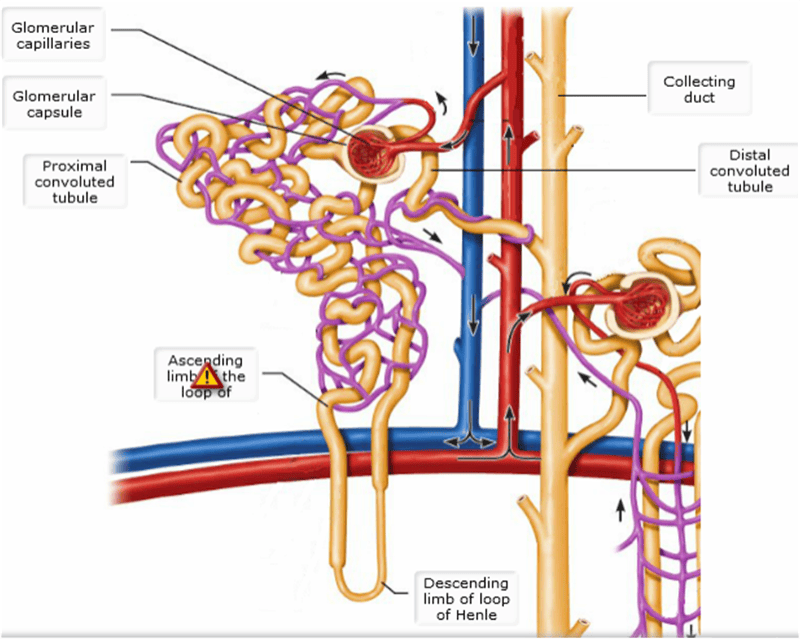
Cortical & juxtamedullary nephrons detailed
pic
Where does most solute reabsorption occur in the nephron?
a. Proximal convoluted tubule
b. Distal convoluted tubule
c. Collecting duct
d. Glomerulus
a. Proximal convoluted tubule
The _________ is an outer layer of dense fibrous connective tissue that anchors the kidney and the adrenal gland to surrounding structures. The _________ prevents infections in surrounding regions from spreading to the kidneys.
a. renal fascia; perirenal fat capsule
b. renal fascia; fibrous capsule
c. fibrous capsule; perirenal fat capsule
d. fibrous capsule; renal fascia
b. renal fascia; fibrous capsule
Under normal conditions, the large renal arteries deliver one-fourth of the total cardiac output (about 1200 ml) to the kidneys each minute. T/F
True
Glomerular hydrostatic pressure (HPg) is the chief force pushing water and solutes out of the blood and across the filtration membrane. T/F
True
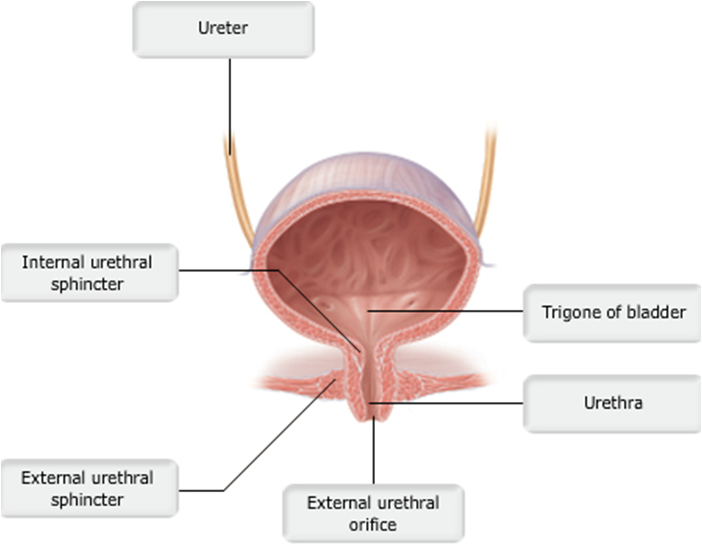
Urinary bladder (female)
pic
Each nephron consists of a _______________, which is a tuft of capillaries, and a ___________.
a. renal plexus; glomerulus
b. glomerulus; renal plexus
c. renal plexus; renal tubule
d. glomerulus; renal tubule
d. glomerulus; renal tubule
Which of the following congenital abnormalities of the urinary system is found in male infants only?
a. Hypospadias
b. Renal calculi
c. Polycystic kidney disease
d. Horseshoe kidney
a. Hypospadias
Under normal conditions, the proximal convoluted tubule reabsorbs all of the glucose, lactate, and amino acids in the filtrate and 65% of the Na+ and water. T/F
True
22 During inhalation,
a. the diaphragm relaxes.
b. air moves up the trachea.
c. oxygen molecules move into the lungs, and carbon dioxide molecules move out of the lungs.
d. the volume of the thoracic cavity decreases.
e. the diaphragm and rib muscles contract.
e. the diaphragm and rib muscles contract.
**The contraction of these muscles causes air to enter the lungs.
22 From which structures do oxygen molecules move from the lungs to the blood?
a. Bronchi
b. Bronchioles
c. Nose
d. Trachea
e. Alveoli
e. Alveoli
22 Which statement is correct?
a. As oxygen diffuses from the lungs into capillaries, blood becomes deoxygenated.
b. Carbon dioxide diffuses from the alveoli into surrounding capillaries.
c. Oxygen is released from the mitochondria as a product of cellular respiration.
d. In the blood, oxygen is bound to hemoglobin, a protein found in red blood cells.
e. Oxygen diffuses from large blood vessels into the body's cells.
d. In the blood, oxygen is bound to hemoglobin, a protein found in red blood cells.
**When oxygen diffuses from the alveoli to the surrounding capillaries, it enters a red blood cell and binds to hemoglobin.
After blood becomes oxygenated,
a. it does not return to the heart, but goes directly to the lungs.
b. it returns to the heart, and is then pumped to body cells.
c. it does not return to the heart, but goes to the nose and mouth.
e. it returns to the heart, and is then pumped to the lungs.
b. it returns to the heart, and is then pumped to body cells.
Hemoglobin
a. uses ATP to move oxygen from blood to body cells.
b. has five subunits.
c. is a protein that can bind four molecules of oxygen.
d. is found in blood plasma.
e. is the site of cellular respiration.
c. is a protein that can bind four molecules of oxygen.
Position of the kidneys against the posterior body wall
pic
m1 functional residual capacity
volume of air in lungs after normal tidal expiration
m1 inspiratory reserve
volume that can be forced in after a tidal inhalation
m1 tidal volume
about 500 ml
m1 total lung capacity
about 6000 ml in an average male
m1 vital capacity
maximum volume of air that can be exhaled after maximum inhalation
Air moves into the lungs because __________.
the gas pressure in the lungs becomes lower than the outside pressure as the diaphragm contracts
Boyle's law states that volume changes lead to pressure changes, and the pressure of a gas varies inversely with its volume.
Alveolar ventilation rate is __________.
the movement of air into and out of the alveoli during a particular time
AVR = breaths per minute × (TV - dead space)
Hemoglobin has a tendency to release oxygen where __________.
pH is more acidic
The Bohr effect states that CO2 loading and lower pH enhance O2 release
In the alveoli, the partial pressure of oxygen is __________.
about 104 mm Hg
The partial pressure of oxygen in the alveoli is ~104 mm Hg, which is about 35% less than that of the atmospheric PO2.
Most of the carbon dioxide transported by the blood is __________.
converted to bicarbonate ions and transported in plasma
Seventy percent of CO2 is converted to bicarbonate ions and transported in plasma
The elastic cartilage that shields the opening to the larynx during swallowing is the __________.
epiglottis
The movement of air into and out of the lungs is called __________.
pulmonary ventilation
Involuntary hyperventilation during an anxiety attack can cause the person to become faint because of __________.
lowered CO2 levels in the blood and consequent constriction of cerebral blood vessels
Which of the following terms describes the increase in depth and force of breathing that occurs during vigorous exercise?
hyperpnea
Approximately 20% of carbon dioxide is transported in the blood as __________.
carbaminohemoglobin
Which of the following controls the respiratory rate?
medulla
Which of the following is NOT a function of the trachealis muscle?
IT DOES NOT:
It prevents the trachea from collapsing and keeps it patent, despite the pressure changes that take place during breathing.
An example of an enzyme located in the lung capillary membrane that acts on material in the blood is __________.
angiotensin converting enzyme
Which of the following conditions would NOT cause atelectasis?
WOULD NOT CAUSE: loss of lung elasticity
One of the causes of atelectasis is plugging of the bronchioles
Airway resistance is insignificant in relationship to gas flow because __________.
the airways branch more as they get smaller, resulting in a huge total cross-sectional area
The transpulmonary pressure is the difference between the __________ and the __________ pressure.
intrapulmonary; intrapleural
Which of the following conditions would NOT decrease the total respiratory compliance
WOULD NOT: increase in lung compliance
**Deformity of the thorax would hinder thoracic expansion and lead to a decrease in the total respiratory compliance.
Which of the following nonrespiratory movements would ventilate all of the alveoli?
yawning
The dorsal respiratory group __________.
Is located dorsally at the root of cranial nerve IX
This is a characteristic of the ventral respiratory group.
The pontine respiratory group is responsible for all of the following functions, EXCEPT __________.
stimulating the contraction of the diaphragm
Which of the following would NOT be found in a "blue bloater"
weight loss
How is Na+ reabsorbed
by active transport using ATP
Micturition is __________.
a sacral reflex in infants
Micturition is a sacral reflex in infants. It is also called urination. Between ages 2 and 3, descending circuits from the brain have matured enough to begin to override reflexive urination.
The most important factor affecting the glomerular filtration rate is __________.
net filtration pressure
**GFR is directly proportional to NFP
When the concentration of ADH increases, __________.
less urine is produced
Which process results in increased blood pressure in response to hormone release?
renin-angiotensin-aldosterone mechanism
Arrange the following structures in the correct sequence in which urine passes through them to the external environment: (1) ureter, (2) renal pelvis, (3) calyx, (4) urinary bladder, (5) urethra.
3, 2, 1, 4, 5
If the efferent arteriole constricts while the afferent arteriole remains unchanged, the glomerular filtration rate __________.
increases
**If the efferent arteriole constricts while the afferent arteriole remains unchanged, the glomerular filtration rate increases. This will increase glomerular hydrostatic pressure.
The renal hilum lies on the __________ surface of the kidney.
medial
Renal ptosis may lead to __________.
hydronephrosis due to urine backup
All of the following are layers of the filtration membrane in the glomerular membrane, EXCEPT the __________.
renal capsule
Which of the following is NOT part of the filtration membrane?
extraglomerular mesangial cells
All of the following functions are carried out in the renal tubules, EXCEPT __________.
FILTRATION
All of the following would stimulate the release of renin from granular cells, EXCEPT __________.
inhibition by the macula densa cells
The energy needed for secondary active transport is provided by the __________.
concentration gradient established by Na
Which of the following is the countercurrent multiplier in the kidney?
the loop of Henle of a juxtamedullary nephron
Urea transport into the medullary collecting duct is enhanced by __________.
ADH
Which of the following substances is the standard substance used to measure the GFR?
inulin
Which of the following is NOT associated with primary nocturnal enuresis?
females over the age of 60 years