Physiology Integrative Chapters
look at specific neuron (efferent)
o Autonomic or somatic (always acting in an excitatory way)?
o Where is it happening? Spinal or cranial?
o Innate or learned?
o How many neurons? Mono (direct connection between efferent and afferent sides) or polysynaptic (almost all neurons)?
classification of neural reflexes
Key thing for mono – Direct synapse from sensory neuron onto efferent neuron
Poly uses a CNS interneuron which can get very complex, most common (all autonomic neurons)
• Convergence – Many sensory neurons feeding into few interneurons
• Divergence – Few interneurons feeding many efferent neurons
Contraction = excitation of efferent neuron
Relaxation = inhibition of efferent neuron
skeletal muscle reflexes
All are polysynaptic
At least one synapse between sensory & CNS & synapse between preganglionic w/postganglionic neurons
AKA visceral reflexes
All are polysynaptic
Many show tonic (continuous) activity
Can be integrated in spinal cord or brain
Limbic system = emotionally driven reflexes
Examples: Urination, breathing, eating, body temperature, blushing, getting goosebumps, etc.
autonomic reflexes
Proprioceptors -> CNS -> Alpha motor neurons (somatic motor neurons that innerve skeletal muscle fibers that contract) -> Extrafusal muscle fibers
o Proprioceptors – sensory receptors that monitor position in space, movement, etc.
o Proprioceptors include: joint receptors, muscle spindles & golgi tendon organs
o - Joint receptors – In capsules & ligaments to detect mechanical distortion around joints
Proprioceptors
- Sensory receptors that sense muscle length & changes in muscle length
Present in intrafusal muscle fibers
Stretch the whole length of the muscle tissue
Intrafusal muscle fibers have a muscle spindle in them and recognize the change in length of the spindle over time
Intrafusal fibers are contractile at the end but not in the middle (where muscle spindles lie)
Sustained contraction requires alpha-gamma coactivation and coactivation)
• Alpha motor neurons (somatic) innervate extrafusal fibers, Gamma innervate contractile portion of intrafusal fibers
muscle spindles (picture)
Respond to muscle tension during isometric contraction
Reflex response = relaxation
• Inhibiting muscle neurons causing them to not fire and causing relaxation
Prevents damage to tissue
Found in junction of muscle fibers and tendon
golgi tendon organs (picture)
• muscles are often arranged in antagonistic muscle groups. If you’re going to flex (contract) one muscle, you must extend (relax) its antagonist.
• Knee jerk example – very simple monosynaptic muscle reflex
• Sensory neuron branches in spinal cord:
o One part directly synapses with somatic motor neurons for quad muscle contraction and the Other part synapses on inhibitory neurons for hamstrings.
o Quad contracts, hamstring relaxes & your leg shoots out.
Inhibition of hamstring is part of the response
patellar tendon (knee jerk) reflex
• Reflex from stepping on something sharp or touching something hot (step-on-a-lego reflex)
• Polysynaptic muscle reflex
• Pulls body away from harmful stimuli
flexion reflex (step-on-a-lego reflex) (picture)
Multiple skeletal muscles signaling CNS that integrates signals and coordinates a response
All polysynaptic
Reflex movements
Voluntary movements
Rhythmic movements
body movement
• Stimulated by sensory receptors
• Simple, integrated in spinal cord or brain stem
• Rapid, inherent response
• Ex: knee jerk, cough
• Brain does receive sensory input to coordinate body-wide responses
reflex movements
• Stimulated by external stimuli or conscious thought
• Complex, integrated in CNS (usually brain)
• Learned movements
• Ex: playing the piano, swimming, riding a bike
• With practice, learned movements can become subconscious – muscle memory, more like a reflex
voluntary movement
• Start & stop are voluntary
• Intermediate complexity, integrated in spinal cord with higher level input
• Ex: Running, quiet breathing patterns
• Once started, CNS interneurons called central pattern generators maintain repetitive activity
• Ex: Take an animal that is paralyzed where the “start” signal for walking is blocked. If you support the animal on a treadmill and electrically stimulate the spinal central pattern generator for that movement, the legs will start walking.
rhythmic movement
3 levels of control:
• Spinal cord – spinal reflexes & has central pattern generators, reflex responses
• Brain stem & cerebellum – control postural reflexes & hand/eye movements, fine tunes movement
• Cerebral cortex & basal ganglia – voluntary movements, higher processing
neural control of movement (table)
o Picture yourself doing what you’re about to do
o Psychological process stimulates physiological process
o Presynaptic facilitation- Mental process in cerebral cortex stimulates signals in muscle groups
o Used is sports, any kind of performance, anxiety disorders, cancer treatment & pain management
visualization technique
o Has helped researchers understand how basal ganglia integrates signals
o Symptoms: abnormal movements (tremors), speech difficulty, lose facial expression, personality changes
o Dopamine activity is key
Give patients a precursor of dopamine, L-dopa, that can cross the blood-brain barrier.
parkinson's disease
o Mostly controlled by autonomic nervous system
o Hormones, in addition to neural cues, regulate contraction
o Skeletal muscle is attached to bone, smooth & cardiac are not.
o If you contract smooth or cardiac muscle, you change the shape of the organ
o Often very specific in the way that an organ is controlled, so we will cover that as we discuss those tissues.
visceral (autonomic muscle control)
o Body is constantly fighting to keep a relatively constant state
o Taking in water & ions, either need to use it or excrete it
Sweat, Urine, Feces, Ventilation
o Water and salt are two of the most important molecules to regulate
Ion concentrations in interstitial fluid used for transport
Mess up concentrations and neural function (and other functions) are messed up
Key for cell volume
homeostasis
osmolarity and tonicity
baroreceptor reflex
systemic integration (picture, response to low blood pressure or blood volume)
o Decrease in blood pressure past the point of vasoconstriction and reduces the blood flow into the glomerulus
o Kidneys can also adjust for differences in blood pressure
o Keeps GFR (glomerular filtration rate) constant over a wide range of pressures (80-180 mm Hg)
myogenic autoregulation
increase in blood causes and increase in the amount of fluid being pushed through the tubes
tubuloglomerular feedback (picture)
o Sympathetic control changes resistance in arterioles
o increase in NE causes either vasoconstriction or vasodilation in arterioles depending on the receptor present
kidneys are slower than cardiac for these changes
autonomic regulation
spreads through the blood for a widespread effect
in the kidneys: affects slits on podycytes that control regulation
hormonal regulation
1/3 water is extracellular, 2/3 water is intracellular
3L of plasma, the rest of water is in interstitial fluid
volume of water in= volume of water out
ccan be disrupted by excessive sweating or diarrhea
water balance
^ KNOW THIS
• happens mostly in the kidneys
• Adjust the GFR, adjust the amount of water that is lost
• Water cannot be replenished by the kidneys, just conserved
• Happens in:Renal medulla (significant amount of reabsorption), Distal tubule (small amount or reabsorption), Collecting duct (most of the regulation of reabsorption)
• Concentration of urine varies between 50 mOsM and 1200 mOsM(based on normal body osmolarity of 300 mOsM), trying to move water without moving solutes
water conservation (pictures)
• Peptide neurohormone synthesized in the hypothalamus
• Secreted by the posterior pituitary
• AKA antidiuretic hormone (ADH)
• Neurohormone is released into the blood
• Acts on collecting duct epithelium
• causes a slow change in the microtubule membrane composition (incorporates more aquaporins into the membrane)
• increases reabsorption (urine is concentrated), urine is diluted and more water is excreted in the absence of vasopressin
• Vasopressin binds to a receptor -> activates cAMP second messenger system -> inserts aquaporin into the apical membrane ->water is absorbed by osmosis into the blood
Vasopressin controlling water levels (picture)
Blood pressure
Blood volume
Plasma osmolarity* (more important)
• Receptors in the hypothalamus pick up on signals
• Threshold = 280 mOsM
o Release more vasopressin and increased water resorption if you exceed 280 mOsM
o Absorb more during the day than you do at night (Allows you to urinate less at night)
vasopressin regulation (picture)
Animals like whales that live in cold water need to circulate blood such that it conserves heat
• Puts blood vessels in close proximity conserves heat and conserve the energy that would be needed to heat the blood
•vasa recta
countercurrent exchange
Cross section of the renal medulla contains tons of ducts and tubes (vasa recta, loops of henle, collecting ducts, etc.)
Instead of transferring heat, transfers water and solutes
No loss to environment, kidney is a closed system
Countercurrent multiplier to make it more dilute than it could have been on its own
• each dot represents another loop, the image represents a whole tissue
• Picks up solutes as it is moved down the loop of henle (red down) due to concentration gradients and ending the blood
• Normal gradient pumps water in and leaved solute
• Start and end at the same concentration in the blood (300 mOsM) but change concentration within the loop
• interstitial fluid is more concentrated, more dilute levels leaving the loop of henle following the concentration gradient
• urea and salt act as solutes
vasa recta (countercurrent exchange) (picture)
o Addition of salt increases body osmolarity
o Without regulation would create a hypertonic ECF -> cell shrinking
o salt (solutes) increase osmolarity, leads to hypotonicity
o To combat the hypotonicity: Salt addition triggers vasopressin secretion and thirst
o Increased vasopressin triggers water conservation
o Thirst increases water intake
o Regulated only via kidneys
o Changes in blood volume are noticed due to the change in blood pressure
o Key hormone: aldosterone
sodium balance (picture)
o Fast response
Aldosterone secretion stimulated by:
Increased ECF K+ concentration or Decreased blood pressure Trigger the release of aldosterone
• No aquaporins in the membrane- move solutes without moving water
Aldosterone (picture)
Renin-angiotensin system (RAS) pathway
looks for changes in NaCl that passes through the loop of henle -> drop in NaCl levels= drop in blood pressure
renin is released in response the to the decrease in blood pressure
RAS pathway (picture)
from RAS pathways and aldosterone
o Angiotensin I
o Angiotensin II Effects (active molecule)
All effects increase blood pressure
• Increases vasopressin secretion (stimulates thirst)- increase in volume= increase in pressure since your body absorbs more water
• Vasoconstrictor
• Increases CVCC sympathetic output
• Increases proximal tubule reabsorption
Medication (ACE inhibitors) that blocks the production of Angiotensin II which will lower blood pressure but may have significant side effects
Angiotensin
• Key ion for excitable tissue (without proper regulation the concentration in the membranes will change dramatically)
• Hyperkalemia vs Hypokalemia
• Regulated by pH balance
• Kidney disease, improper eating, diarrhea, dehydration
Potassium regulation
• Hyperkalemia – too much K+
o Makes membrane more excitable and allows more solutes to pass through, cells cannot fully repolarize to “reset” the signal
• Hypokalemia – too little K+
o similar to hyperkalemia but opposite
o makes the membrane potential higher
weakened tissue and responses for both conditions
Hyperkalemia vs Hypokalemia
• drinking replaces fluid loss- reflex response to increased osmolarity, eating ice chips is effective
• salt appetite- animals lick the ground to increase salt content
• dehydration avoidance- mid afternoon nap helps you stay out of the sun during the hottest part of the day to avoid dehydration
• extreme sweating or blood loss- need to replace both the blood volume and the solutes
control of volume and osmolarity
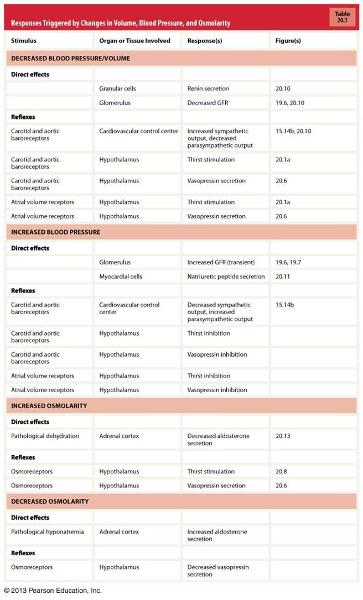
responses triggered by changes in volume, blood pressure, and osmolarity
o Body is normally slightly alkaline (pH = 7.40, Usually ECF & ICF pH are similar)
o Important because changes dramatically affect protein function (changes the structure of proteins which will change their function)
o Acidosis vs Alkalosis
o Related to K+ levels
o Source of pH changes (Comes from food & metabolism- biggest acid source, in all cells and plasma, bicarbonate and carbonic anhydrase which produces H+)
In general, your body takes on more acids than bases
Acid-base balance
o Acidosis
Too low pH
Neurons are less excitable = CNS depression -> coma -> death
o Alkalosis
Too high pH
Neurons are hyperexcitable = muscle twitches -> sustained contractions -> tetanus -> death
general Acidosis vs Alkalosis
Moderates but does not prevent changes in pH by interacting with H+
Proteins, phosphate ions, hemoglobin
Not a permanent fix
Reversible reaction
• Will increase levels of CO2
• Increased CO2 levels à increased ventilation
pH homeostasis mechanisms- buffers
Cover remaining 25% of regulation
• occurs in the kidneys
• Excrete or reabsorb H+ ions
• Excrete or reabsorb bicarbonate
• relatively slow
pH homeostasis mechanisms- renal regulation
buffers
renal regulation
ventilation
pH homeostasis mechanisms (types)
covers 75% of regulation
Respiratory acidosis
• Increased plasma CO2 due to hypoventilation
• Alcohol, drugs, asthma, fibrosis, dystrophy
• Need to excrete H+ and reabsorb bicarbonate in kidneys
pH homeostasis mechanisms- ventilation
Acidosis
• Dietary & metabolic input increases H+
o Lactic acidosis, ketoacidosis, aspirin, diarrhea
• Respiratory compensation à hyperventilation
alkalosis
• Decrease in H+ concentrations
• Excessive vomiting, excessive antacid consumption
• Respiratory compensation àhypoventilation
metabolic acidosis vs alkalosis
Respiratory acidosis
• Increased plasma CO2 due to hypoventilation
• Alcohol, drugs, asthma, fibrosis, dystrophy
• Need to excrete H+ and reabsorb bicarbonate in kidneys
respiratory acidosis vs alkalosis
ATP in muscle cells
Phosphocreatine (PCr) converting ADP into ATP
Lasts 10-15 seconds
energy sources for exercise
• Glycolytic metabolism
o Anaerobic
o 2.5 times faster
o 2 ATP/glucose
o Metabolic acidosis
• Citric acid cycle
o Aerobic
o Slower
o 30-32 ATP/glucose
o Both glucose & fatty acids with O2
store as glycogen. muscle and liveer glycogen stores provide 2000kcal worth of energy (20 miles of running). afterwards can use a combo of fatty acids and glucose for energy
manufacturing new ATP
• Glucagon, cortisol, growth hormone, epinephrine, and norepinephrine all increase during exercise
o Mobilize liver glycogen (turning it in to glucose) raising blood glucose levels
• Insulin decreases
o If blood sugar is up, why does insulin decrease?
Keeps glucose free for muscle fibers
Contracting muscle fibers do not need insulin for glucose uptake (GLUT4 transporter)
Transported to bring glucose from the blood to cells are independent of insulin
hormone regulation of energy production
• Oxidative phosphorylation uses up O2
• Can quantify intensity by measuring O2 use (VO2)
• VO2 max, athletes can have musch higher VO2 max than normal people
oxygen consumption during exercise
• Mitochondria
o Important for ATP generation (oxidative phosphorylation)
o Training increases number of mitochondria in muscle fiber
• Cardiovascular or pulmonary system?
o Which holds you back more?
o When cardiac output is 90% max, ventilation is only 65% max
limiting metabolic factors
As exercise begins
• Mechanoreceptors and proprioreceptors sense movement and signal motor cortex
• Motor cortex signals medulla oblongata to increase ventilation
• Central, carotid & aortic chemoreceptors monitor CO2, pH & O2
• Increase alveolar ventilation as needed
• Under moderate exercise, levels stay constant
ventilation response to exercise
• Cardiac output increases dramatically
o Resting = 5 L/min, Average person = 20 L/min, Trained athlete = 40 L/min
o Cardiac Output (CO)= heart rate x stroke volume
o CO= (SA node rate + autonomic nervous system input) x (venous return + force of contraction)
o Decrease parasympathetic activity -> rising heart rate
o Sympathetic takes over and stimulates heart
Increases contractility (more blood per beat)
Increases heart rate
o Sympathetic division triggers body-wide vasoconstriction
o Skeletal muscle vasodilates
Due to changes in microenvironment
• Temperature, CO2, O2, H+ concentration
• Overrides vasoconstriction signal
cardiac response to exercise
o Muscle gets about 1/4 of the blood (1.2L/min) at rest
o Exercise increases blood flow to muscles to almost 90%
o Trained athletes can increase blood flow to muscles to 22 L/min
blood flow during exercise
o Increases slightly
Skeletal muscle vasodilates
Cardiac output increases
o How does pressure stay increased?
New threshold?
Signal inhibition?
Muscle chemoreceptors?
blood pressure response to exercise
• As you exercise your body “wastes” energy in the form of heat during metabolism
• Body temperature can reach 104-108°F
• Two responses:
o Increased cutaneous blood flow
o Sweating
Lowers body temperature through evaporative cooling
Problems: Dehydration, Reduced blood volume
Disease: Hyperhidrosis, Hypohidrosis
temperature regulation during exercise