what kind of tissue is blood?
connective tissue
what are the two components of blood
plasma and formed elements
what are the formed elements in blood
erythrocytes, leukocytes and thrombocytes
what are erythorocytes
red blood cells or RBC's
what are leukocytes
white blood cells or WBC's
what are thrombocytes
platelets
hematocrit
the percentage of blood volume that is red blood cells 47%(+ or -) for males and 42%(+ or -) for females
what are the physical characteristics of blood
sticky, opaque fluid
color is scarlet to dark red
pH is 7.35 to 7.45
38 degrees C
8 % of body weight
average vol 5-6 liters for males and 4-5 liters for females
one of the functions of blood is distribution explain
distributes oxygen and nutrients to body cels
distributes metabolic wastes to the lungs and kidneys for elimination
distributes hormones from the endocrine organs to target organs
one of the functions of blood is regulation explain
regulates body temperature by absorbing and distributing heat
regulates normal pH using buffers
regulates adequate fluid volume in the circulatory system
what is the most important regulatory function of the blood
regulating body temperature
one of the functions of blood is protection explain
protects against blood loss - plasma proteins and platelets initiate clot formation
protects against infection - antibodies, complement proteins and WBC's defend against forgien invaders
what is one area where blood doesnt go
cartilage
what is blood plasma composed of
90% water, proteins, nutrients, electrolytes, respiratory gases, hormones, and nitrogenous by products of metabolism
blood plasma - where are most of the proteins produced, what are the proteins,and what role do they play
mostly produced by the liver
60% albumin - main contributor of osmotic pressure (most important)
36% globulins - antibodies, transport proteins
4% fibrinogen - blood clotting proteins
what are the nitrogenous by products of metabolism in blood plasma
lactic acid, urea, creatine
what nutrients are found in blood plasma
glucose, carbohydrates, amino acids
what are the electrolytes found in blood plasma
Na K Ca Cl and HCO
respiratory gases found in blood
oxygen and carbon dioxide
which blood cells are the only complete blood cells and why
White blood cells - because they contain a nucleus
which blood cells contain no nuclei or organelles
red blood cells
platelets are considered what
cell fragments
how long do most formed elements survive in the blood stream
only a few days
where do most blood cells originate
bone marrow - and dont divide
describe an erythrocyte
red blood cell, biconcave discs, anucleate (no nucleus) essentially no organelles, filled with hemoglobin, are the major contributing factor to blood viscosity
why does a RBC have a biconcave shape
to give it a huge surface area relative to volume
an RBC has no mitochondia so how does it produce ATP
ATP production is anaerobic - which means no oxygen is used to generate ATP, and they are not consuming any of the oxygen that they are carrying
what fills a RBC
97% hemoglobin - for gas transport
where can you find spectrin and what is its function
on the cytoplasmic face of the plasma membrane - it gives the RCS the flexibility to change shape as necessary as it passes through capilaries and then to resume its biconcave shape.
what is the job of RBC's
to transport respiratory gases - oxygen and carbon dioxide
what is the job of hemoglobin and what is it made up of
to bind oxygen to the RBC (also what makes RBC's red)
made up of the protein globin, (which is made up of four polypeptide chains, two alpha chains and two beta chains) and the red pigment heme
oxygemoglobin
oxygen loading in the lungs - (ruby red)
deoxyhemoglobin
unloading of oxygen in the tissues - reduced hemoglobin (dark red)
carbminohemoglobin
carbon dioxide unloading in the tissues (carries 20% of carbon dioxide in the blood) occurs from tissues to lungs where carbondioxide is eliminated from the body
what is hematopoiesis
hema - blood poiesis - to produce
process in which blood cells are produced -occurs in the red bone marrow of the axial skeleton, girdles and proximal epiphyses of humerus and femur
where can 75% of bicarbonate be found
in the plasma
explain what hemocytoblasts are
stem cells, give rise to all formed elements
97% of oxgen is carried by the RBC's what happens to the rest of it
the rest is disolved as a gas in the blood
CO2 is converted to what? the rest is converted to what?
HCO3
carried as carbaminohemoglobin, and the rest is disolved as gas
what happens when carbondioxide binds to hemoglobin
it gets rid of the oxygen
what does the heme portion of the blood carry
iron
erythropoieses
the process of red blood cell production happens in the red bone marrow
explain the process of erythropoiesis
begins with the stem cell(hemocytoblast), hormones (erythropoitein EPO)circulating in the blood stream stimulate the cell to become a committed cell, the cell then beomes a proerythroblast at that time huge amounts of ribosomes are produced, next comes phase 1 (early erythroblast) ribosome sythesis occurs then phase 2 (late erythroblast) hemoglobin is sythesized and iron accumulates within the cell, it then becomes a normoblast, when most of the hemoglobin has accumulated the organelles are ejected. phase 3 the nuclear functions end and the nucleus degenerates and is ejectedwhich causes the cell to colapse giving it the biconcave shape resulting in a reticulocyte.
how long does the process of erythropoiesis take
about 15 days
what happens if you dont have enough RBC's
leads to tissue hypoxia - inadequate oxygen supply to the tissues
what happens if you have too many RBC's
an increase in blood viscosity
the balance between RBC production and destruction depends on what
hormonal controls and adequate supplies of iron, amino acids and B vitamins
describe the erythropoietin EPO process
1. stimulus - hypoxia(low blood O2 carrying ability) decreased RBC count, decreased hemoglobin, decreased availibility of oxygen
2.kidney (liver) releases EPO
3. EPO stimulates the red bone marrow
4. enhanced erythropoiesis increases RBC count
5.O2 carrying ability of blood increases
what is erythropoietin EPO
a glocoprotein hormone which directly stimulates erythropoiesis, which is released by the kidneys in response to hypoxia
what are causes of hypoxia
hemorrage or increased RBC destruction, insuficient hemoglobin (iron deficiency) and reduced availability of oxygen (high altitudes)
what are the effects of EPO
more rapid maturation of committe bone marrow cells
increased circulating reticulocyte count
what also enhances EPO production leading to higher RBC counts in males
testosterone
what is the hematocrit? what is its normal value
the percentage of blood that is occupied by erythrocytes - it is normally about 45%
list two protective funcions of blood
formation of clots - to prevent blood loss
prevent infection - because of antimicrobial proteins
are plasma proteins used as fuel for body cells - explain
no their presence in the blood is required to perform many key functions
Differentiate into macrophages
Monocyte
Form a temporary plug at the site of bleeding
Platelets
what are some of the, dietary requirements required for erythropoiesis
amino acids, lipids, and carbohydrates
iron and vitamin B12 and folic acid
Where / how is iron stored and transported
65% is stored in the hemoglobin,also in the liver, spleen, and bone marrow
it is stored in cells as ferritin and hemosiderin and transported by transferrin
what is Vitamin B12 and folic acid necessary for
DNA synthesis and cell division
what is the lifespan of a RBC
100 to 120 days
what is the life cycle of a red blood cell
1. low O2 levels in blood stimulate kidneys to produce EPO
2.EPO levels rise in blood
3. EPO and necessary raw materials in blood promote erythropoiesis in red bone marrow
4 new RBC's ente rthe blood stream and function for about 120 days
5. aged and damaged RBC's are engulfed by macropahges of liver, spleen, and bone marrow- the hemoglobin is broken down
6 raw amterials are made available in blood for erythrocyte synthesis
what happens to hemoglobin once it is broken down
the heme and the globin are seperated
iron is salvaged for reuse
heme is degraded to the yellow pigment billirubin
- liver secretes bilirubin (in bile) into the intestines
- degraded pigment leaves the body in feces as stercobilin
- globin is metabolized into amino acids
what are some erythrocyte disorders
anemia and polycythemia
what is anemia
when blood has abnormally low oxygen carrying capacity - its a sign rather than a disease, blood oxygen levels cant support normal metaboolism, accompanied by fatigue, paleness, shortness of breath and chills
what are some causes of anemia
1. insufficient erythrocytes
2. low hemoglobin content
3. abnormal hemoglobin
describe insufficient erythrocytes
1. hemorrhagic anemias
2. hemolytic anemias
3. aplastic anemias
describe hemorrhagic anemias
acute or chronic blood loss
describe hemolytic anemias
RBC's rupture prematurely
describe aplastic anemias
destruction or inhibition of red bone marrow
describe low hemoglobin content
1. iron deficiency anemia
2. prenicious anemia
describe iron deficiency anemia
secondary result of hemmorrhagic anemia or inadequate intake of iron-containing foods or impaired iron absorption
describe prenicious anemia
deficiency of vitamin B12
lack of intrinsic factor needed for absorption of B12
treated by intramuscular injection of B12 or application of nascobal
describe abnormal hemoglobin
1. thalassemias
2. sickle-cell anemia
describe thalassemias
absent or faulty globin chain
RBC's are thin, delicate, and deficient in hemoglobin
describe sickle-cell anemia
defective gene codes for abnormal hemoglobin (HbS)
causes RBC's to become sickle shaped in low-oxygen situations
aplastic
from the start
hemmorrhagic
older
how many molecules of oxygen can each hemoglobin molecule transport? what part of hemoglobin binds the oxygen?
each hemoglobin molecule can transport four O2
the heme portion of the hemoglobin binds the O2
patients with advanced kidney disease often have anemia - explain the connection
the kidneys synthesis of erythropoietin is compromised in advancded kidney disease
RBC production decreases causing anemia
what is polycythemia and what does it result from
an excess of RBC's that increases blood viscosity
polycythemia vera- bone marrow cancer
secondary polycythemia - when less oxygen is available (high altitudes) or when less EPO is produced
blood doping
what is blood doping
the practice of boosting the number of red blood cells (RBCs) in the bloodstream in order to enhance athletic performance.

red blood cell
description: biconcave, anucleate disc, salmon colored, diameter of 7-8 μm
cells/μL(mm3) of blood: 4-6 million
duration of development: about 15 days
life span: 100- 120 days
function: transport oxygen and carbon dioxide
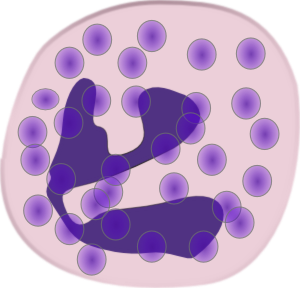
leukocytes
white blood cells
make up over 1% of total blood volume
spherical, nucleated cells
can leave capiliaries via diapedesis
diapedesis
The migration of blood cells (especially leucocytes) through the intact walls of blood vessels into the surrounding tissue
(powerpoint def- move through tissue spaces by ameboid motion and positive chemotaxis{positively moving out to tissue to get something it needs})
what is leukocytosis
when the WBC count is over 11,000/mm3 - normal response to a viral invasion
granulocytes
neutrophil
eosinophil
basophil
these cells are larger than RBS's and have shorter lives
contain a lobed nuclei
are phagocytic - bacteria slayers
formation of neutrophils
leukocytes arise from ancestral stem celss called hemocytoblats
committed cell stage: granular leukocytes develop via a sequence involving myeloblasts
developmental pathway: promyelocyte to neutrophilic myelocyte to neutrophilic band cells and finally as neutrophils
neutrophil
description: nucleus multilobed; contain fine granules that take up both acidic and basic dyes, give the cytopasm a lilac color, granules contain hydrolytic enzymes and defensins, diameter of 10-12 μm
cells/μL(mm3) of blood: 3000- 7000
duration of development: about 14 days
life span: 6 hours to a few days
function: phagocytize bacteria
formation of eosinophil
leukocytes arise from ancestral stem celss called hemocytoblats
committed cell stage: granular leukocytes develop via a sequence involving myeloblasts
developmental pathway: promyelocyte to eosinophilic myelocyte to eosinophilic band cells and finally as eosinophils

eosinophil
description:red staining bilobed nuclei, red to crimson(acidophillic) coarse, lysosome-like granules 10-12 μm
cells/μL(mm3) of blood: 100-400
duration of development: about 14 days
life span: 5 days
function: kill parasitic worms - complex role in alergy and asthma, modulators of the immune response
formation of basophil
leukocytes arise from ancestral stem celss called hemocytoblats
committed cell stage: granular leukocytes develop via a sequence involving myeloblasts
developmental pathway: promyelocyte to basophilic myelocyte to basophilic band cells and finally as basophils
basophil - rarest WBC
description: large puplish-black (basophilic) granules containing histamine 10-14 μm
cells/μL(mm3) of blood: 20-50
duration of development: about 1-7 days
life span: a few hours to a few days
function: release histamineand other mediatorsof inflammation, contain heperin (an anticoagulant) are functionally similar to mast cells
histamine
an inflammitory chemical that acts as a vasodilator and attracts other WBC's to inflammed sites
agranulocytes
lymphocytes and monocytes
lack visible cytoplasmic granule
have spherical or kidney shaped nuclei
lymphocyte formation
leukocytes arise from ancestral stem cells called hemocytoblats
committed cell stage:only lymphocytes arise via the lymphoid stem cell line lymphoid stem cell becomes lymphoblast
developmental pathway: the lymphoblast becomes a prolymphocyte then a lymphocyte some them become plasma cells
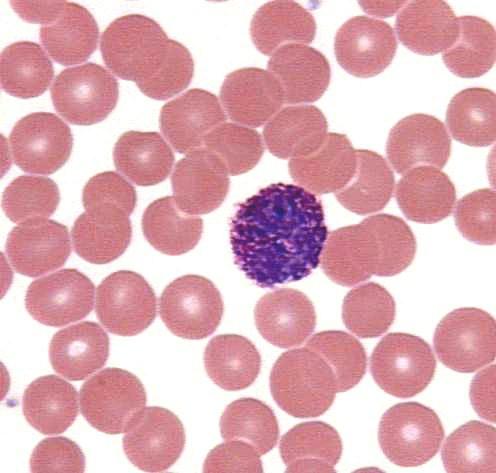
lymphocyte
description: large dark purple, circular nuclei with a thin rim of blue cytoplasmmostly in lymphoid tissue, few circulate in the blood 5-17 μm
cells/μL(mm3) of blood: 1500-3000
duration of development: days to weeks
life span:hours to years
function: mount immune response by direct cell attack or via antibodies
how many types of lymphocytes are there and what do they do
there are 2 types
T cells - act against virus infected cells and tumor cells
B cells - give rise to plasma cells, which produce antibodies
monocyte formation
leukocytes arise from ancestral stem celss called hemocytoblats
committed cell stage: monocytes like granular leukocytes, are progeny of the myeloid stem cell and share a common precursor with neutrophils
developmental pathway: promonocyte to monocytes - some become macrophages (tissue

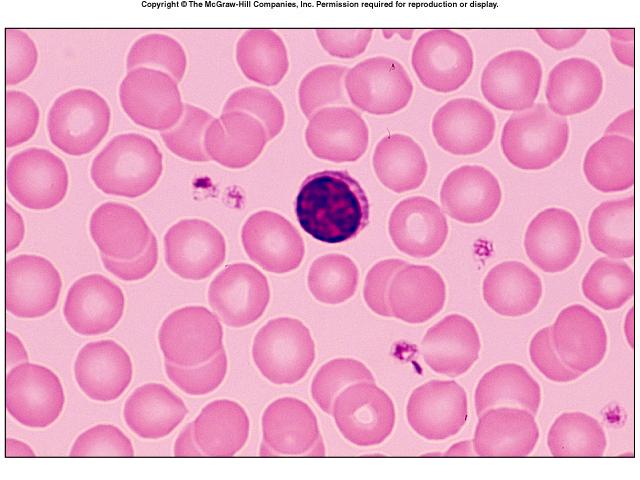
monocyte - the largest leukocyte
description: abundant pale blue cytoplasm, dark purple staining U or kidney shaped nuclei 14-24 μm
cells/μL(mm3) of blood: 100-700
duration of development: 2 to 3 days
life span: months
function: phagocytosis- crucial against viruses,intracellular bacterial parasites and chronic infections- activate lymphocytes to mount an immune response; leave circulation and develop into microphages in the tissues
leukopoiesis
production of white blood cells
stimulated by chemical messengers from bone marrow and mature white blood cells
interleukins - dictators
all leukocytes originate from hemocytoblasts
leukocyte disorders include what
leukopenia - abnormally low WBC count - drug induced
leukemia - cancerous condition involving WBC's (named so because of the abnormal WBC clone involved)
what sort of cells are involved in acute leukemia? who is primarily affected by this disease
blast type cells
children
leukemia
bone marrow totally occupied with cancerous leukocytes, immature nonfunctional WBC's in the bloodstream, death is caused by internal hemorrhage ans overwhelming infections, treatments include irradiation, antileukemic drugs, and stem cell transplants
cases of chronic leukemia more prevelant in what age group
older people
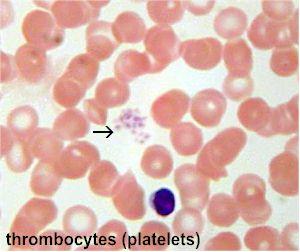
thrombocytes - platelets
description: small fragments of megakaryocytes formation of thrombopoietin, blue staining outer region, purple granules 2-4μm
cells/μL(mm3) of blood: 150,000- 400,000
duration of development: 4 to 5 days
life span: 5 to 10 days
function: seal small tears in blood vessels instrumental in blood clotting
circulating platelets are kept inactive and mobile by NO and prostacyclin from endothelial cells of blood vessels
which WBC's turn into macrophages in tissues? which other WBC is a voracious phagocyte?
noocytes become macrophages in tissues
neutrophils are also voracious phagocytes
platelets are called thrombocytes in other animals. which term that we have learned relates to its name? what does this term mean?
thrombopoietin is derived from the same word as thrombocyte
it is the hormone that promotes platelet formation
Amos has leukemia. even though his WBC count is abnormally high. Amos is prone to severe infections, bleeding, and anemia - explain.
his red bone marrow is spewing out many abnormal WBC's which are crowding out the production of normal bone marrow elements
the lack of normal WBC's allows the infections, the lack of platelets fails to stop bleeding and the lack of erythrocytes is anemia
thrombopoietin -
thrombocytes
formation of platelets
stem cell hemocytobalst
developmental pathway - megakaryoblast becomes promegakaryocyte which becomes magakaryocyte and developes into platelets
homestasis - stop bleeding
step 1 vascular spasm - smooth muscle contracts causing vasoconstriction
step 2 platelet plug formation - injury to lining of vessel exposes collagen fibers; platelets adhere (platelets release chemicals that make nearby platelets sticky - platelet plug forms
step 3 coagulation - fibrin forms a mesh that traps red blood cells and platelets forming a clot
what are the three phases of coagulation
1. prothrombin activator is formed when tissue is damaged A)intrinsic pathway- factors present within blood stimulate coagulation B) extrinsic coagulation- factors outside blood stimulate coagulation
2. prothrombin is converted into thrombin
3. thrombin catalyzes the joining of fibrinogen to form a fibrin mesh
thromboembolytic disorders
undesirable clot formation
bleeding disorders
abnormalities that prevent normal clot formation
thrombus
clot that developes and persists in an unbroken blood vessel - may block circulation, leading to tissue death
embolis
thrombus freely floating in the blood stream
pulmonary emboli impair the ability of the body to obtain oxygen
cerebral emboli can cause strokes
how can thromboembolytic conditions be prevented
aspirin- antiprostaglandin that inhibits thromboxane A2
heperin - anticoagulant used clinically for pre and postoperative cardiac care
warfarin - used for those prone to atrial fibrillation
disseminated intravascular coagulation
widespread clotting blocks intact blood vessels
severe bleeding occurs because residual blood unable to clot
most common in pregnancy, septicemia (blood infection) or incompatible blood transfusions
petechia
A petechia ( /pɨˈtiːkiə/; plural petechiae /pɨˈtiːkɪ.iː/) is a small (1-2mm) red or purple spot on the body, caused by a minor hemorrhage (broken capillary blood vessels).[1
thrombocytopenia
dificient number of circulating platelets
a. petechaae appear due to spontaneous widespread hemorrhage
b. due to suppression or destruction of bone marrow (malignancy- radiation)
c. platelet count under 50,000 mm3 is diagnostic
d. treated with transfusion of concentrated platelets
impaired liver function may also cause bleeding dsorders - explain
a. inability to synthesize procoagulants
b. causes include vitamin K deficiency (which is required for making clotting factors) hepatitis and cirrhosis
c. liver disease can also prevent the liver from producing bile, impairing fat and vitamin K (fat soluable molecule) absorption
hepatitis
Hepatitis is swelling and inflammation of the liver. It is not a condition, but is often used to refer to a viral infection of the liver
cirrhosis
Cirrhosis is scarring of the liver and poor liver function. It is the final phase of chronic liver disease.
hemophilias include several similar hereditary bleeding disorders describe A B and C
hemophilia A - most common type (77% of all cases) due to a deficiency of factor VIII
hemophilia B - defieciency of factor IX
hemophilia C - mild type defieciency of factor XI
one of the symptoms of hemophilia is prolonged bleeding, where does this occur
in the joint cavities
how are bleeding disorders treated
with plasma transfusions and injection of missing factor
what is a whole blood tranfusion
when blood loss is substantial
when are infusions of packed red cells
when whole blood from which most of the plasma has been removed is used to restore oxygen carrying capacity
what can occur if a transfusion of incompatible blood is given
it can be fatal
how many different varieties of naturally occuring Rbc antigens do humans have
30
what do antigens of the ABO and Rh blood groups cause
vigorous transfusion reactions
what are the blood types
A
B
AB
and O
antigen - agglutinogens
An antigen that stimulates the production of a particular agglutinin, such as an antibody. Also called agglutogen
antibodies - agglutinins
An antibody that causes particulate antigens such as bacteria or other cells to clump together.
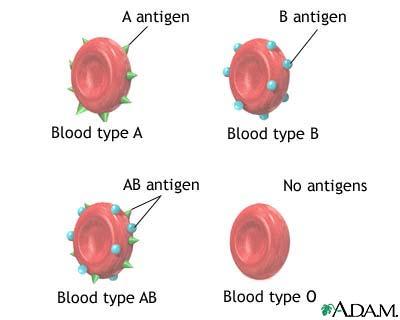
antigens photo
blood group AB
antigen (agglutinogens): A B
antibodies (agglutinins): none
blood that can be received: A, B, AB, and O - universal recipient
blood group B
antigen (agglutinogens): B
antibodies (agglutinins): A
blood that can be received: B and O
blood group B
antigen (agglutinogens) : A
antibodies (agglutinins): B
blood that can be received : A and O
blood group O
antigen (agglutinogens) : none
antibodies (agglutinins) A and B
blood that can be received: O universal donor
how many different Rh agglutinogens are there
45 different Rh agglutinogens (Rh factors)
C,D,and E being the most common
second exposure to Rh+ blood will result in a typical transfusion reaction
when do transfusion reactions occur
if mismatched blood is infused
when transfusion reactions occur what happens to the donors cells
they are attacked by the recipients plasma agglutinins, agglutinate and clog small vessels, rupture and release free hemoglobin into the bloodstream
when transfusion reactions occur what does it result in
diminished oxygen carrying capacity
hemoglobin in kidney tubules and rnal failure
what is erythroblast fetalis
hemolytic disease of the newborn the Rh- mother becomes sensitized when exposure to Rh+ blood occurs and causes her body to synthesize Rh antibodies which cross the placenta and destroy the RBC's of the Rh+ baby the baby can be treated with prebirth abd after birth transfusions - RhoGAM serum containing anto Rh can prevent the Rh- mother from becoming sensitized
what can result from low blood volume
death from shock
how can low blood volume be replaced immediately
a. with normal saline or multiple electrolyte solution that mimics plasma electrolyte composition
b. with plasma expanders (purified human serum albumin, hetastarch and dextran) - these would mimic the osmotic properties of albumin, its more expensive and may cause significant complications
diagnostic blod tests include what
1. hematocrit
2. blood glucose test
3. microscopic examination - reveals variations in size and shape of RBC's indications of anemias
4. differential WBC count
5. prothrombin time and platelet counts assess hemostasis
6 SMAC - a blood checmistry profile
7. complete blood count (CBC )