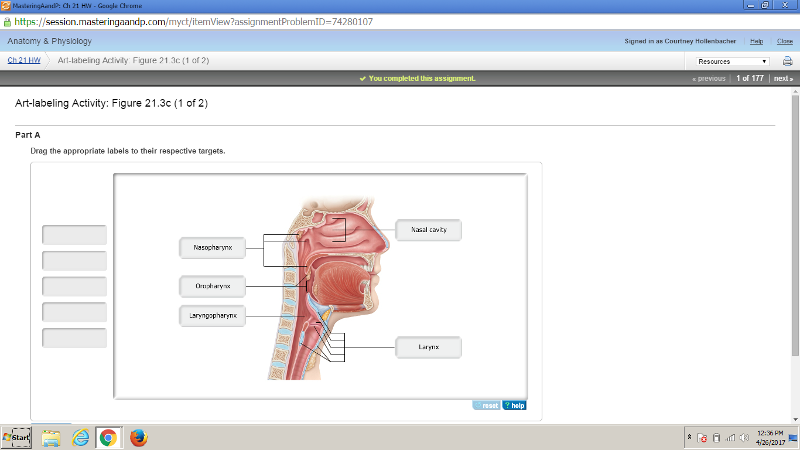
In which region are the palatine tonsils found?
oropharynx
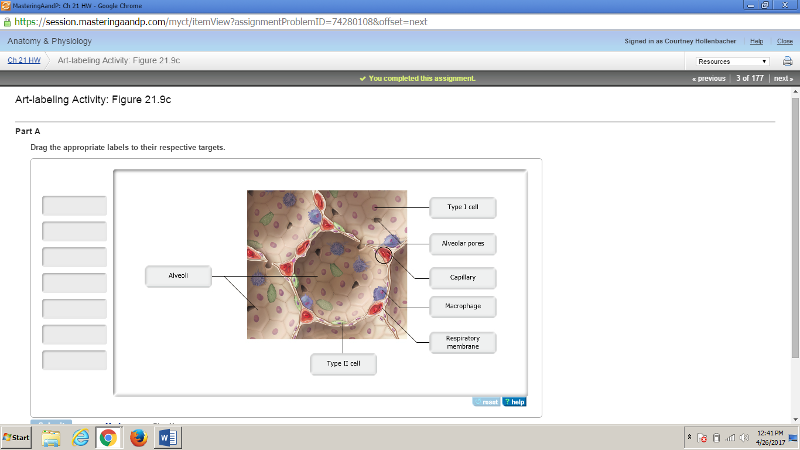
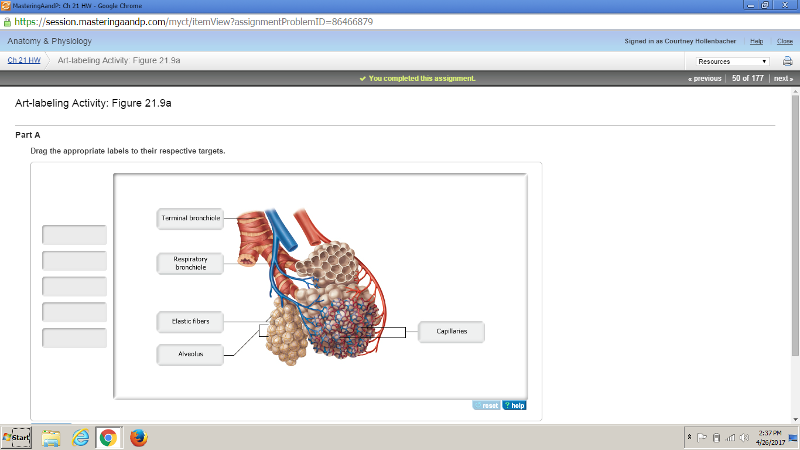
What type of epithelial tissue forms the walls of the alveoli?
simple squamous epithelium
Which of the following is NOT a physical factor that influences pulmonary ventilation?
partial pressure of oxygen in the air
What is the amount of air that can be exhaled with the greatest possible exhalation after the deepest inhalation called?
vital capacity
During inhalation,
the diaphragm and rib muscles contract.
From which structures do oxygen molecules move from the lungs to the blood?
Alveoli
Which statement is correct?
In the blood, oxygen is bound to hemoglobin, a protein found in red blood cells.
After blood becomes oxygenated,
it returns to the heart, and is then pumped to body cells.
Hemoglobin
is a protein that can bind four molecules of oxygen.
What is ventilation-perfusion coupling?
matching the amount of gas reaching the alveoli to the blood flow in pulmonary capillaries
Which of the following is the primary factor in oxygen attachment to, or release from, hemoglobin?
partial pressure of oxygen
What is the most powerful respiratory stimulant in a healthy person?
arterial blood carbon dioxide level
Patients with rhinitis often have "watery eyes" because ______.
the infection has caused inflammation of the nasolacrimal ducts
In pneumothorax, the lung collapses because ______.
intrapleural pressure is higher than intrapulmonary pressure
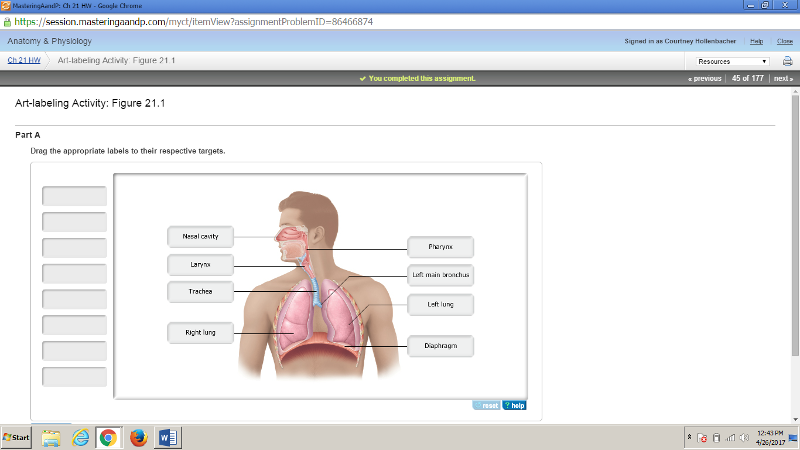
Which of the following processes are unique to the respiratory system?
pulmonary ventilation and external respiration
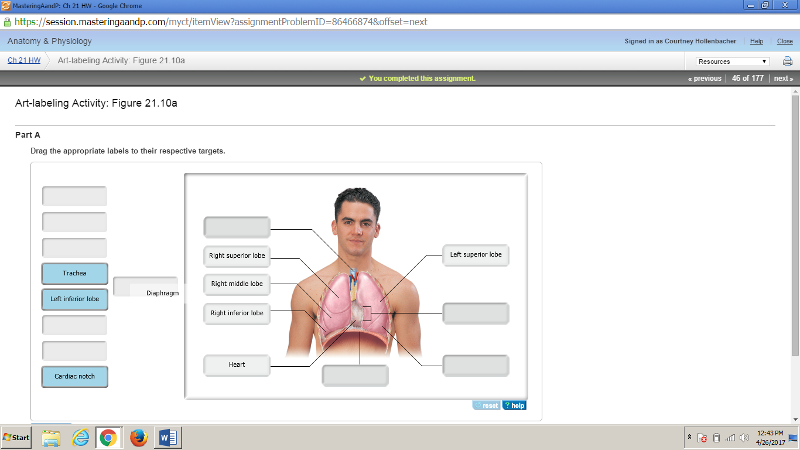
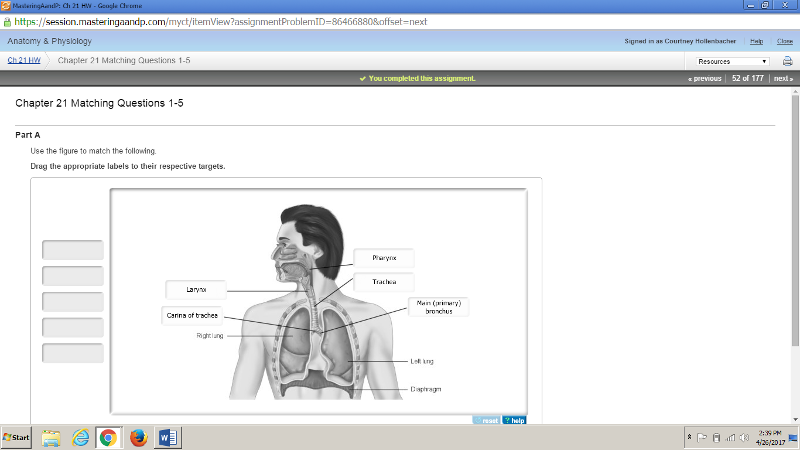
Which of the following features characterizes the right lung?
presence of a superior, middle, and inferior lobe
Which blood vessels supply oxygenated systemic blood to the lung tissue?
bronchial arteries
The indentation on the medial surface of each lung through which pulmonary and systemic blood vessels, bronchi, lymphatic vessels, and nerves enter and leave is called the ___________.
hilum
Which of the following is NOT a function of the nasal conchae?
routing air and food into proper channels
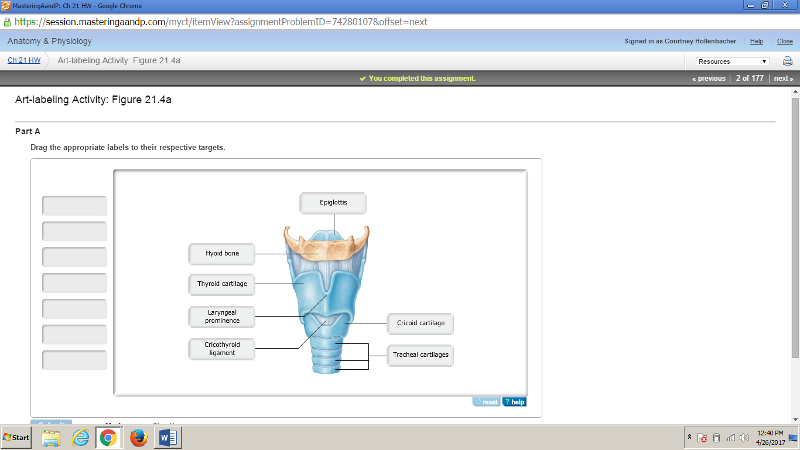
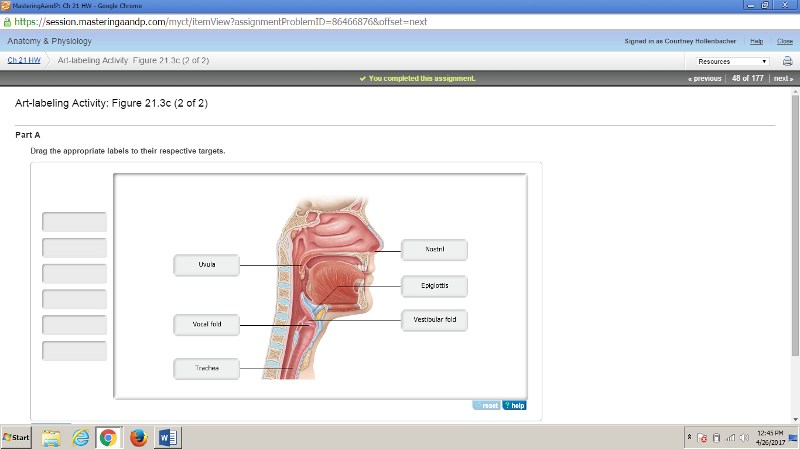
What part of the larynx covers the laryngeal inlet during swallowing to keep food out of the lower respiratory passages?
epiglottis
During the Valsalva's maneuver, what part of the larynx closes to increase intra-abdominal pressure, such as to help with defecation?
glottis
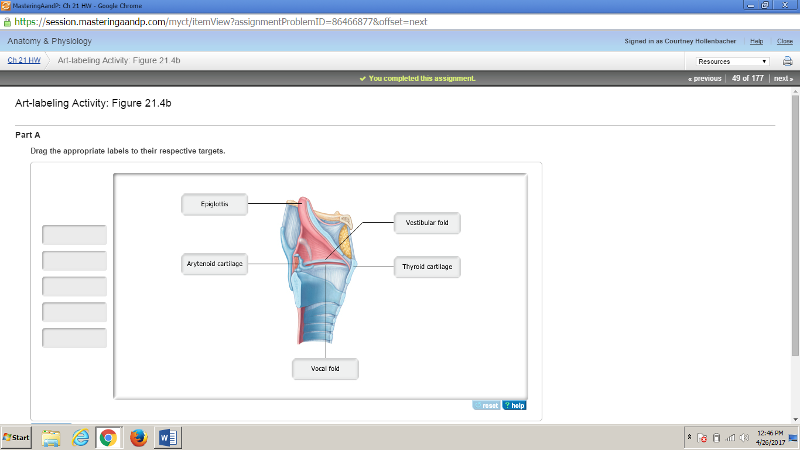
Which cartilage belonging to the larynx anchors the vocal cords?
arytenoid cartilages
Which of the following is NOT a function of the larynx?
serving as part of the respiratory zone
Since mucus-producing cells and cilia are sparse in the bronchioles and alveoli, how does the body remove microorganisms that make their way into the respiratory zone?
alveolar macrophages crawl freely along internal alveolar surfaces
Where does gas exchange occur in the respiratory system?
alveoli
Which of the following represents all of the processes involved in respiration in the correct order?
pulmonary ventilation; external respiration; transport of respiratory gases; internal respiration;
pulmonary ventilation; external respiration; transport of respiratory gases; internal respiration;
to destroy pathogens entering the nasopharynx
Which of the following respiratory structures is more commonly known as the "throat"?
pharynx
Which of the following is NOT a function of the larynx?
to assist in taste sensation
The __________ is also known as the "guardian of the airways."
epiglottis
The smallest subdivisions of the lung visible with the naked eye are the __________, which appear to be connected by black carbon in smokers.
lobules
Systemic venous blood that is to be oxygenated in the lungs is delivered by the __________, and the __________ provide oxygenated systemic blood to lung tissue.
pulmonary arteries; bronchial arteries
__________, the difference between the intrapulmonary and intrapleural pressures, prevents the lungs from collapsing.
Transpulmonary pressure
Quiet inspiration is __________, and quiet expiration is __________.
an active process; a passive process
The adenoids normally destroy pathogens because they contain ______.
lymphocytes
The tissue(s) and/or cells that may be affected during laryngitis ______.
is epithelial tissue
is connective tissue
are ciliated cells
All of the listed responses are correct.
Smoking inhibits cilia by inhibiting the movements of ______.
dynein molecules
Tracheal obstruction by a large piece of food typically involves obstruction of the ______.
larynx
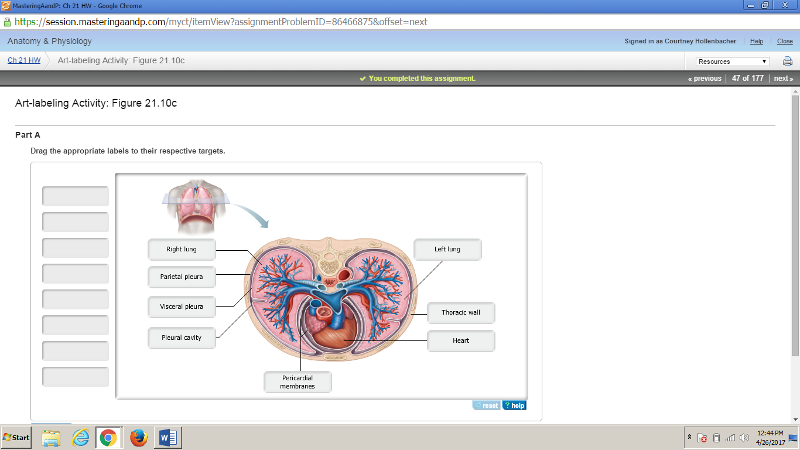
During pleurisy, the inflamed parietal pleura of one lung rubs against the inflamed ______.
visceral pleura of the same lung
Which parts of the respiratory system function as the main sites of gas exchange?
alveoli
Jane had been suffering through a severe cold and was complaining of a frontal headache and a dull, aching pain at the side of her face. What regions are likely to become sites of secondary infection following nasal infection?
The paranasal sinuses
The main site of gas exchange is the ________.
alveoli
The loudness of a person's voice depends on the ________.
force with which air rushes across the vocal folds
The walls of the alveoli are composed of two types of cells, type I and type II. The function of type II is to ________.
secrete surfactant
Select the correct statement about the pharynx.
The auditory tube drains into the nasopharynx.
The larynx contains ________.
the thyroid cartilage
Which of the choices below is not a role of the pleura?
aids in blood flow to and from the heart because the heart sits between the lungs
Which of the following provide the greatest surface area for gas exchange?
alveoli
The respiratory membrane is a combination of ________.
alveolar and capillary walls and their fused basement membranes
The nose serves all the following functions except ________.
as the direct initiator of the cough reflex
The factors responsible for holding the lungs to the thorax wall are ________.
surface tension from pleural fluid and negative pressure in the pleural cavity
Most inspired particles such as dust fail to reach the lungs because of the ________.
ciliated mucous lining in the nose
Which of the following maintains the patency (openness) of the trachea?
C-shaped cartilage rings
Which of the following descriptions accurately describes Boyle’s law?
The pressure of gas in your lungs is inversely proportional to the volume in your lungs.
Which muscles, when contracted, would increase the volume of air in the thoracic cavity?
diaphragm and external intercostals
Which pressure is the result of the natural tendency of the lungs to decrease their size (because of elasticity) and the opposing tendency of the thoracic wall to pull outward and enlarge the lungs?
intrapleural pressure
During an allergic reaction, which of the following would aid respiration?
epinephrine
If the transpulmonary pressure equals zero, what will happen to the lung?
lungs will collapse
Which of the following pressures rises and falls with the phases of breathing, but eventually equalizes with the atmospheric pressure?
intrapulmonary pressure
Which of the following pressures must remain negative to prevent lung collapse?
intrapleural pressure
Calculate the transpulmonary pressure if atmospheric pressure is 755 mm Hg.
4 mm Hg
Which of the following gives the relationship between the pressure and volume of a gas?
Boyle's law
Which of the following pressure relationships best illustrates when inspiration will occur?
Ppul < Patm
Which muscles are activated during normal quiet inspiration?
diaphragm and external intercostal muscles
What is the volume of the total amount of exchangeable air for a healthy, young adult male?
4800 ml
Which volumes are combined to provide the inspiratory capacity?
tidal volume (TV) + inspiratory reserve volume (IRV)
What is the tidal volume of an average adult male?
500 ml
Which form of hypoxia reflects poor O2 delivery resulting from too few RBCs or from RBCs that contain abnormal or too little hemoglobin?
anemic hypoxia
Which form of CO2 transport accounts for the least amount of CO2 transported in blood?
dissolved in plasma
If the compliance of the thoracic wall is decreased, ______.
the intrapleural pressure would not decrease normally during inhalation
Which of the following would NOT be involved in causing bronchiolar constriction during an asthma attack?
adrenal medulla
In babies born prematurely, pulmonary surfactant may not be present in adequate amounts ______.
due to insufficient exocytosis in the type II alveolar cells
What is the most immediate driving force behind pulmonary ventilation?
intrapulmonary pressure change
Surfactant helps to prevent the alveoli from collapsing by ________.
interfering with the cohesiveness of water molecules, thereby reducing the surface tension of alveolar fluid
Which of the choices below describes the forces that act to pull the lungs away from the thorax wall and thus collapse the lungs?
the natural tendency for the lungs to recoil and the surface tension of the alveolar fluid
The major nonelastic source of resistance to air flow in the respiratory passageways is ________.
friction
Which of the following determines lung compliance?
alveolar surface tension
Tidal volume is air ________.
exchanged during normal breathing
The lung volume that represents the total volume of exchangeable air is the ________.
vital capacity
The amount of air that can be inspired above the tidal volume is called ________.
inspiratory reserve
Which respiratory-associated muscles would contract if you were to blow up a balloon?
internal intercostals and abdominal muscles would contract
Complete the following statement using the choices below. Air moves out of the lungs when the pressure inside the lungs is
greater than the pressure in the atmosphere.
Inspiratory capacity is ________.
the total amount of air that can be inspired after a tidal expiration
Unlike inspiration, expiration is a passive act because no muscular contractions are involved. Expiration, however, depends on two factors. Which of the choices below lists those two factors?
the recoil of elastic fibers that were stretched during inspiration and the inward pull of surface tension due to the film of alveolar fluid
Which of the following is not possible?
Pressure gradient equals gas flow over resistance.
Select the correct statement about the physical factors influencing pulmonary ventilation.
As alveolar surface tension increases, additional muscle action will be required.
Intrapulmonary pressure is the ________.
pressure within the alveoli of the lungs
The relationship between gas pressure and gas volume is described by ________.
Boyle's law
Which of the following arterial blood levels is the most powerful respiratory stimulant?
rising CO2 levels
Which of the following structures would be the LEAST vulnerable to damage caused by oxygen toxicity?
costal cartilages
During pneumonia, the lungs become "waterlogged"; this means that within the alveoli there is an abnormal accumulation of ______.
interstitial fluid
Emphysema can result in an ______.
increased level of carbaminohemoglobin
increased level of deoxyhemoglobin
increased likelihood of the skin of Caucasians developing a slightly blue coloration
All of the listed responses are correct.
For gas exchange to be efficient, the respiratory membrane must be ________.
0.5 to 1 micrometer thick
The local matching of blood flow with ventilation is ________.
ventilation-perfusion coupling
Which of the following is not an event necessary to supply the body with O2 and dispose of CO2?
blood pH adjustment
Which of the choices below determines the direction of respiratory gas movement?
partial pressure gradient
Oxygen and carbon dioxide are exchanged in the lungs and through all cell membranes by ________.
diffusion
The statement, "in a mixture of gases, the total pressure is the sum of the individual partial pressures of gases in the mixture" paraphrases ________.
Dalton's law
Oxygen is unloaded where it is most needed when blood pH drops, this is a phenomenon known as ___________.
the Bohr effect
What is the most common method of carbon dioxide transport?
as bicarbonate ions in the plasma
Which of the following qualifies as a fully saturated hemoglobin molecule?
hemoglobin is transporting four oxygen molecules
Hypoxia can be caused by ______.
hyposecretion of erythropoietin
What is the primary form in which carbon dioxide is carried in blood?
as a bicarbonate ion in plasma
With the Bohr effect, more oxygen is released because a(n) ________.
decrease in pH (acidosis) weakens the hemoglobin-oxygen bond
In the plasma, the quantity of oxygen in solution is ________.
only about 1.5% of the oxygen carried in blood
Which of the following counteracts the movement of bicarbonate ions from the RBC?
chloride shifting
Possible causes of hypoxia include ________.
too little oxygen in the atmosphere
Which statement about CO2 is incorrect?
More CO2 dissolves in the blood plasma than is carried in the RBCs.
How is the bulk of carbon dioxide carried in blood?
as the bicarbonate ion in the plasma after first entering the red blood cells
Which of the following incorrectly describes mechanisms of CO2 transport?
attached to the heme part of hemoglobin
Which of the choices below is not a factor that promotes oxygen binding to and dissociation from hemoglobin?
number of red blood cells
Select the correct statement about oxygen transport in blood:
A 50% oxygen saturation level of blood returning to the lungs might indicate an activity level higher than normal.
Which of the following does not influence hemoglobin saturation?
nitric oxide
What area in the brain sets the respiratory rhythm?
ventral respiratory group (VRG)
Inspiratory neurons send information to the diaphragm via what nerve?
phrenic nerve
What directly stimulates the central chemoreceptors, thus increasing respiration?
H+ (hydrogen ions)
As a result of hyperventilation, what will happen to the partial pressures of CO2 (pCO2) and pH?
decreased pCO2 and increased pH
Which receptors inhibit inspiration during hyperinflation of the lungs?
pulmonary stretch receptors
What stimulates increased respiration at the beginning of exercise?
sensory input from receptors in joints, neural input from the motor cortex, and other factors
A homeostatic control mechanism controls respiration. What acts as the effector(s) in this system?
respiratory muscles
Which of the following initiates inspiration?
ventral respiratory group (VRG)
Which of the following respiratory rates illustrates eupnea for an average, healthy adult at rest?`
15 breaths per minute
Which of the following modifies and smoothes the respiratory pattern?
pontine respiratory centers
Which of the following stimuli is the most powerful respiratory stimulant to increase respiration?
rising carbon dioxide levels
Which of the following inhibits the respiration rate?
stimulation of stretch receptors in the lungs
Which of the following conditions or scenarios increases the respiratory rate?
acidosis
Hypocapnia causes ______.
hypoxia
What determines the respiratory rhythm in the body?
medullary respiratory centers
A patient was admitted to the hospital with chronic obstructive pulmonary disease. His PO2 was 55 and PCO2 was 65. A new resident orders 54% oxygen via the venturi mask. One hour later, after the oxygen was placed, the nurse finds the patient with no respiration or pulse. She calls for a Code Blue and begins cardiopulmonary resuscitation (CPR). Why did the patient stop breathing?
Oxygen dilates pulmonary arterioles, increasing perfusion and worsening an already poor ventilation-perfusion mismatch. In addition, oxygen drives more CO2 off of hemoglobin, dumping it into alveoli from which it cannot be removed.
How will the lungs compensate for an acute rise in the partial pressure of CO2 in arterial blood?
Respiratory rate will increase.
The most powerful respiratory stimulus for breathing in a healthy person is ________.
increase of carbon dioxide
Which of the following is not a stimulus for breathing?
rising blood pressure
Respiratory control centers are located in the ________.
medulla and pons
Factors that influence the rate and depth of breathing include ________.
voluntary cortical control
Gas emboli may occur because a ________.
diver holds his breath upon ascent
Which center is located in the pons?
pontine respirator group (PRG)
Select the correct statement about the neural mechanisms of respiratory control.
The pons is thought to be instrumental in the smooth transition from inspiration to expiration.
The erythrocyte count increases after a while when an individual goes from a low to a high altitude because the ________.
concentration of oxygen and/or total atmospheric pressure is lower at high altitudes
Why is a patient with tuberculosis often noncompliant with treatment?
Due to the time length of treatment, the patient may stop taking the medication when they start to feel better.
Which of the following is not a form of lung cancer?
Kaposi's sarcoma
Which of the disorders below is characterized by destruction of the walls of the alveoli producing abnormally large air spaces that remain filled with air during exhalation?
emphysema
The paired lungs occupy all of the thoracic cavity.
F
Smoking diminishes ciliary action and eventually destroys the cilia.
T
Tracheal obstruction is life threatening.
T
The parietal pleura lines the thoracic wall.
T
The olfactory mucosal lining of the nasal cavity contains the receptors for the sense of smell.
T
Nasal conchae mainly work on inhalation to warm and moisten air. They serve minor functions for exhalation.
F
The functions of the nasal conchae are to enhance the air turbulence in the cavity and to increase the mucosal surface area exposed to the air.
T
The lungs are perfused by two circulations: the pulmonary and the bronchial. The pulmonary circulation is for oxygenation of blood. The bronchial circulation supplies blood to the lung structures (tissue).
T
Valsalva's maneuver involves closing off the glottis (preventing expiration) while contracting the muscles of expiration, causing an increase in intra-abdominal pressure.
T
The average individual has 500 ml of residual volume in his lungs.
F
Atelectasis (lung collapse) renders the lung useless for ventilation.
T
Under certain conditions, the vocal folds act as a sphincter that prevents air passage.
T
Intrapleural pressure is normally about 4 mm Hg less than the pressure in the alveoli.
T
During normal quiet breathing, approximately 750 ml of air moves into and out of the lungs with each breath.
F
The alveolar ventilation rate is the best index of effective ventilation.
T
The structures within the respiratory system's conducting zone include the trachea and the paranasal sinuses.
T
Ventilation perfusion coupling means that more blood flows past functional alveoli than past nonfunctional alveoli.
T
Dalton's law states that the total pressure exerted by a mixture of gases is the sum of the pressures exerted independently by each gas in the mixture.
T
The alveoli are also known as alveolar sacs.
F
Dalton's law of partial pressures states that the total pressure exerted by a mixture of gases is the sum of the pressures exerted independently by each gas in the mixture.
T
The largest amount of carbon dioxide is transported in the bloodstream in the form of carbonic anhydrase.
F
Increased temperature results in decreased O2 unloading from hemoglobin.
F
As carbon dioxide enters systemic blood, it causes more oxygen to dissociate from hemoglobin (the Haldane effect), which in turn allows more CO2 to combine with hemoglobin and more bicarbonate ion to be generated (the Bohr effect).
F
Oxygenated hemoglobin releases oxygen more readily when the pH is more basic.
F
Changes in arterial pH can modify respiration rate and rhythm even when carbon dioxide and oxygen levels are normal.
T
Dalton's law of partial pressures states that when a gas is in contact with a liquid, that gas will dissolve in the liquid in proportion to its partial pressure.
F
The Hering-Breuer reflex is a potentially dangerous response that may cause overinflation of the lung.
F
Strong emotions and pain acting through the limbic system activate sympathetic centers in the hypothalamus, thus modulating respiratory rate and depth by sending signals to the respiratory centers.
T
Emphysema is distinguished by permanent shrinkage of the alveoli.
F
Although lung cancer is difficult to cure, it is highly preventable.
T
Labored breathing is termed dyspnea.
T
In chronic bronchitis, mucus production is decreased and this leads to the inflammation and fibrosis of the mucosal lining of the bronchial tree.
F
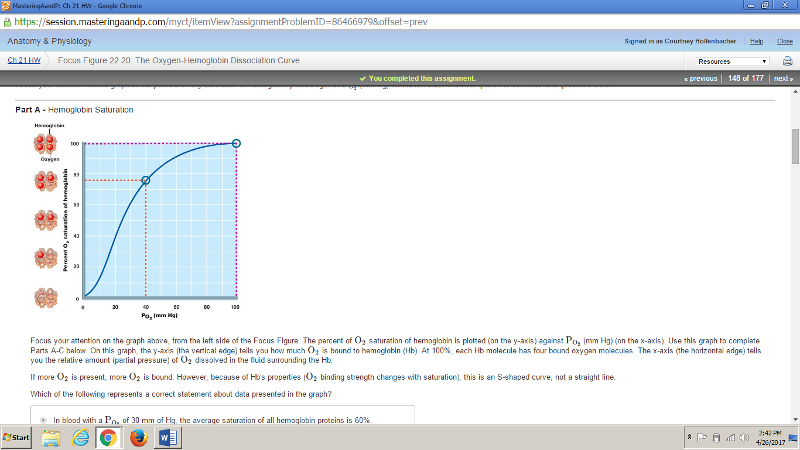
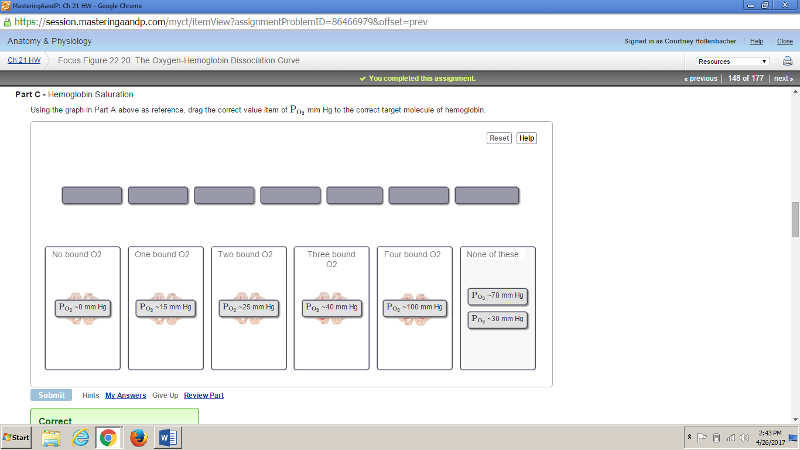
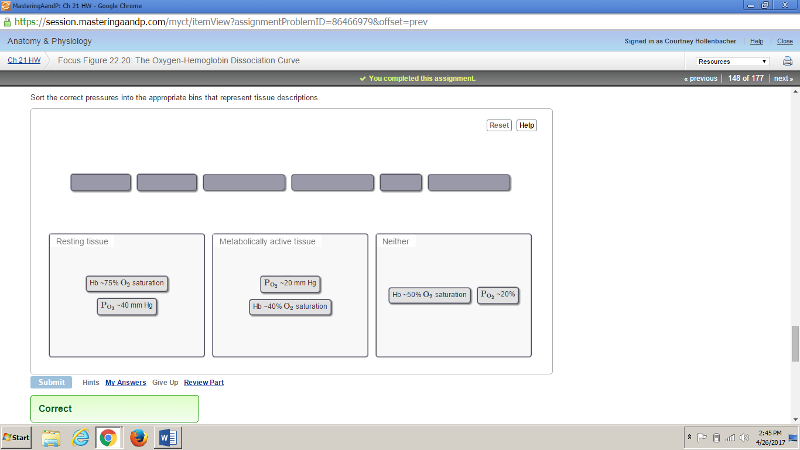
Using the same graph as in Part A above, what is the average number of oxygens bound to hemoglobin at a saturation of 50%?
2
...
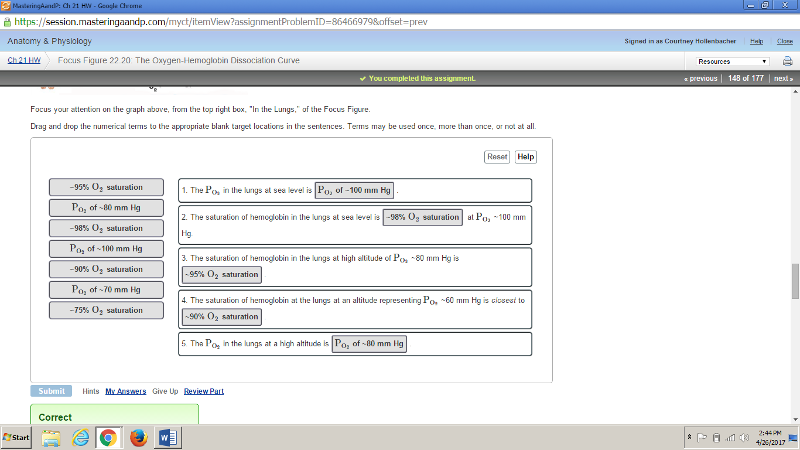
A fireman breathes in air normally as he enters a building following an explosion and fire. He has a meter that predicts the
The fireman's hemoglobin saturation will be about one oxygen per hemoglobin, and he will require an external air tank.